Highlights
-
•
We first described the epidemiological characteristics of patients with SARS-CoV-2 in Hunan and these patients were early mild cases.
-
•
The clinical symptoms, laboratory results, and imaging reports of patients with COVID-19 in the Hunan area were different from Wuhan area.
-
•
For non-Wuhan epidemic areas, more attention should be paid to the nucleic acid test results of throat swabs and stools.
-
•
Reduced whole blood lymph count can be used as an adjuvant diagnosis of early SARS-CoV-2 infection.
-
•
Attention should be paid to asymptomatic carriers, and this is of great significance for the control of the global epidemic.
Keywords: COVID-19, SARS-CoV-2, Hunan, China, Clinical features
Abstract
Background
In December 2019, coronavirus Disease 2019 (COVID-19) occurred in Wuhan, Hubei Province, China. The disease has rapidly spread from Wuhan to other regions.
Objectives
To describe the clinical manifestations and epidemiological characteristics of patients with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in Hunan Province in 2020.
Study design
From January 19 to February 7, 2020, 33 patients with positive in nucleic acid test of pharyngeal swab were retrospectively collected and analyzed.
Results
There are 33 COVID-19 patients (16 male, 17 female), and the median age was 46 years. Nineteen patients (48 %) were associated with a family cluster outbreak. Seventeen patients (52 %) had traveled or lived in Hubei Province. These patients are early mild cases, most common symptoms are fever [23 (70 %)] and cough [13 (39 %)]. Most patients' white blood cell counts are normal, while they manifest as significant reduction in lymphocytes [17/28 (61 %)]. The levels of c-reactive protein and erythrocyte sedimentation rate suggest a typical viral infection. Procalcitonin did not increase and D-dimer increased slightly. Lactate dehydrogenase (LDH) levels have elevated in most patients. CT images of these patients showed bilateral multiple plaques or nodular ground-glass opacities (68.4 %). Fecal nucleic acid results were positive in eight COVID-19 patients accompanied with diarrhea. Tear nucleic acid results were negative in six COVID-19 patients. And four asymptomatic patients were infected with SARS-CoV-2.
Conclusions
The clinical symptoms, laboratory results and imaging reports of patients with COVID-19 in Hunan area are significantly different from those in Wuhan area. For non-Wuhan epidemic areas, more attention should be paid to nucleic acid test results of throat swabs and stools, and it is not easily to diagnose based on clinical symptoms and CT results. Reduced whole blood lymph count can be used as an adjuvant diagnosis of early SARS-CoV-2 infection. Attention should be paid to asymptomatic carriers, which is of great significance for the control of the global epidemic.
1. Background
In December 2019, a series of acute respiratory diseases occurred in Wuhan, Hubei Province, China, now are called Coronavirus Disease 2019 (COVID-19) [1]. The disease has rapidly spread from Wuhan to other regions. As of February 25, 2020, a total of 77,785 COVID-19 cases have been confirmed in China. A new type of coronavirus (SARS-CoV-2) was identified in a bronchial alveolar lavage fluid sample from a patient in Wuhan City, and then it confirmed as the pathogen of COVID-19 /A new type of coronavirus (SARS-CoV-2), which was identified in a bronchial alveolar lavage fluid sample from a patient in Wuhan City, was confirmed as the cause of COVID-192. Now the virus is renamed SARS-CoV-2 by WHO [3]. Whole-genome sequencing and phylogenetic analysis indicate that SARS-CoV-2 is a unique clade of β -coronal viruses associated with human severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) [2]. Like other β coronaviruses’, the genome of SARS-CoV-2 has a long ORF1ab polyprotein at the 5′ end, followed by four major structural proteins, including the spike surface glycoprotein, small envelope protein, matrix protein, and nucleocapsid protein [4]. SARS-CoV-2 is very similar to coronavirus in bats, which are presumed to be the main source [5]. Although the origin of SARS-CoV-2 is still under investigation, current evidence suggests that it spread to humans through wild animals sold illegally in the South China.
Huang et al. first reported 41 COVID-19 cases, most of whom had a history of exposure to the South China Seafood Wholesale Market. The patient's clinical manifestations include fever, dry cough, dyspnea, myalgia, fatigue, normal or decreased white blood cell count, and imaging evidence of pneumonia [7]. However, no difference in clinical characteristics have been reported between Wuhan and other cities in China. Case reports confirm human-to-human transmission of SARS-CoV-2 [8]. Currently, there is no effective First Screening and diagnosis Guide for COVID-19 in Non-Wuhan areas. Therefore, if the Hunan hospital adopts clinical COVID-19 diagnosis measures similar to Hubei area, it will often lead to a higher misdiagnosis rate because of the lighter early clinical symptoms, slighter respiratory damage and the lower positive rate of imaging results.
2. Objectives
The purpose of this case series is to describe the clinical manifestations and epidemiological characteristics of patients with SARS-CoV-2 infection in Hunan, China, then compared with Wuhan’s.
3. Study design
3.1. Sample collection
This study was approved by the Hospital Ethics Committee, and all study participants were informed. The study population consisted of 33 COVID-19 patients at the Second Xiangya Hospital of Central South University, Hunan province, China, between to January to February 2020, aged 20–70 years. All the patients were diagnosed by two experienced doctors. We only show the patients who are positive for in viral nucleotide testing. The samples from the participants were obtained before clinical intensive treatment. Participants received preoperative radiotherapy or chemotherapy were excluded. Respiratory and stool samples were collected with the consent of all patients. Unless otherwise stated, patients were sampled without gender or age bias. Swabs and stool were stored at −20℃ until use.
3.2. RNA extraction and qRT-PCR
Whenever a commercial kit is used, the manufacturer's instructions should be followed without modification. Nucleic acids were extracted by SSNP-2000A Automatic Nucleic Acid Extraction Instrument and nucleic acid extraction kits (Sansure biotech, China). 20 μL extracted nucleic acid sample was added into a PCR amplification tube which contains 30 μL of the prepared PCR-mixed solution, detected through fluorescence quantitative PCR using a fluorescent PCR instrument. Amplification was performed as follows: 50℃ for 30 min, 95℃ for 60 s, and then 40 cycles, including 95℃ for 15 s, 60℃ for 30 s.
The primer and probe sequences [9]:
ORF1b gene
5’-TGGGGYTTTACRGGTAACCT-3’ (Forward)
5’-AACRCGCTTAACAAAGCACTC-3’ (Reverse)
N gene
5′-TAATCAGACAAGGAACTGATTA-3′ (Forward)
5′-CGAAGGTGTGACTTCCATG-3′ (Reverse)
3.3. Data collection
We reviewed the care records, laboratory test results, and chest X-rays and CT reports of laboratory-confirmed SARS-CoV-2 infected patients. Admission data for these patients were from January 9, 2020 to February 9, 2020. The two researchers also independently reviewed data collection forms to confirm repeatedly.
3.4. Statistical analysis
Continuous variables are expressed as median (IQR) and compared using the Mann-Whitney U test Categorical variables are expressed as numbers (%) and compared by chi-square test or Fisher's exact test. A two-sided α of less than 0.05 was considered statistically significant. SPSS version 25.0 Software (SPSS, Inc., Chicago, IL, USA) was used to analyse the datas.
4. Results
By Feb 9, 2020, 33 admitted hospital patients were identified as laboratory-confirmed SARS-CoV-2 infection in Hunan. The patients infected with SARS-CoV-2 were aged from 27 to 78, and the median age of the patients was 46 years (IQR 31.5−65). As of Feb 9, in our cohort of 33 patients no child was infected and no gender distribution in infected patients (Table 1 ).
Table 1.
Comparison of the demographic characteristics and clinical symptoms of SARS-CoV-2 in Hunan and Wuhan [7].
| Area | Hunan | Wuhan | P |
|---|---|---|---|
| All patients | 33 | 41 | |
| characteristics | |||
| Age, years | 46(31.5−65) | 49.0 (41.0–58.0) | |
| Sex | |||
| Men | 16 (48 %) | 30 (73 %) | 0.034 |
| Women | 17 (52 %) | 11 (27 %) | 0.034 |
| Hubei travel or residence history | 19 (58 %) | —— | —— |
| Hubei personnel contact history | 14 (42 %) | —— | —— |
| Signs and symptoms | |||
| Fever | 23 (70 %) | 40 (98 %) | 0.001 |
| Highest temperature (℃) | |||
| <37.3 | 10 (30 %) | 1 (2%) | 0.002 |
| 37.3−39.0 | 21 (64 %) | 26 (64 %) | 1.000 |
| >39.0 | 2 (6%) | 14(34 %) | 0.004 |
| Cough | 13 (39 %) | 31 (76 %) | 0.002 |
| Myalgia or fatigue | 14 (30 %) | 18 (44 %) | 0.898 |
| Sputum production | 5 (15 %) | 11/39 (28 %) | 0.573 |
| Headache | 2 (6%) | 3/38 (8%) | 0.831 |
| Diarrhea | 5 (15 %) | 1/38 (3%) | 0.059 |
| Dyspnea | 0 (0%) | 22/40 (55 %) | 0.001 |
| Chest tightness | 5 (15 %) | —— | —— |
| Shortness of breath | 6 (18 %) | —— | —— |
The clinical and laboratory data of patients in the Wuhan area originated from the article of Huang, C et al [7]. Data are median (IQR), n (%), or n/N (%), where N is the total number of patients with available data. p values comparing Hunan and Wuhan are from χ² test, Fisher’s exact test, or Mann-Whitney U test
The clinical and laboratory data of patients in Wuhan area originated from the article of Huang, C et al. [7]. 19 (58 %) patients had Hubei travel or residence history, while 14 (42 %) patients had contacted Hubei personnel. The most common symptoms at onset of illness were fever [23 (70 %) of 33 patients], cough [13 (39 %)], and myalgia or fatigue [14 (30 %)]; less common symptoms were sputum production [5 (15 %) of 33], headache [2 (6%) of 33], and diarrhoea [5 (15 %) of 33]. Most of patients had chest tightness [5 (15 %)] or Shortness of breath [6 (18 %)]. However, few patients [0 (0%) of 33] developed dyspnoea. By comparing the Hunan’s data with Wuhan’s (the area with the most severe outbreak of COVID-19 in China), we found that the clinical symptoms of patients with SARS-CoV-2 infection in Hunan were significantly different from those in Wuhan. The fever rate of newly diagnosed patients in Hunan area is lower and the temperature of most patients is below 39 ℃ (94 %). Most patients with SARS-CoV-2 did not cough in the early stages of infection. It is worth noting that patients with SARS-CoV-2 in Hunan rarely have difficulty breathing at first diagnosis, only with slight shortness of breath or chest tightness. However, more than half of patients (55 %) in Wuhan suffer from dyspnea (Table 2 and Fig. 1 ).
Table 2.
Comparison of the demographic characteristics and clinical symptoms of SARS-CoV-2 in Hunan and Wuhan [7].
| Area | Hu nan | Wu han | p | reference interval |
|---|---|---|---|---|
| All patients | 28 | 41 | ||
| White blood cell count, × 10⁹ /L | 5.23 (1.95−26.68) | 6·2 (4.1–10.5) | 3.50−9.50*109/L | |
| <4 | 10/28 (35 %) | 10/40 (25 %) | 0.421 | |
| 4–10 | 14/28 (50 %) | 18/40 (45 %) | 0.806 | |
| >10 | 4/28 (15 %) | 12/40 (30 %) | 0.158 | |
| Neutrophil count, × 10⁹ /L | 3.5 (2.70−4.76) | 5.0 (3.3–8.9) | 1.80−6.30*109/L | |
| Lymphocyte count, × 10⁹/L | 0.98 (0.68−1.43) | 0.8 (0.6–1.1) | 1.10−3.20*109/L | |
| <1·1 | 17/28 (61 %) | 26/41 (63 %) | 0.509 | |
| ≥1·1 | 11/28 (39 %) | 15/41 (37 %) | 0.509 | |
| Hemoglobin, g/L | 142 (124.5−155.5) | 126.0 (118.0–140.0) | 130−175 g/L | |
| Platelet count, × 10⁹/L | 186 (157−212.75) | 164.5 (131.5–263.0) | 125−350*109/L | |
| <100 | 3/28 (11 %) | 2/40 (5%) | 0.333 | |
| ≥100 | 25/28 (89 %) | 38/40 (95 %) | 0.333 | |
| Electron spin resonance mm/h | 10 (6−18) | —— | ≤20 mm/h | |
| D-dimer, μg/mL | 0.92 (0.8−1.11) | 0.5 (0.3–1.3) | 0−0.55 μg/mL | |
| Albumin, g/L | 44.4 (42.28−46.68) | 31.4 (28.9–36.0) | 40.0−55.0 g/L | |
| Alanine amino transferase, U/L | 28.85 (22.68−41.25) | 32.0 (21.0–50.0) | 9.0−50.0 U/L | |
| Aspartate amino transferase, U/L | 30.95 (22.7−42.53) | 34.0 (26.0–48.0) | 15.0−40.0 U/L | |
| ≤40 | 11/16 (69 %) | 26/41 (63 %) | 0.478 | |
| >40 | 5/16 (31 %) | 15/41 (37 %) | 0.478 | |
| Total bilirubin, umol/L | 73.15 (72.22−79.18) | 11.7 (9.5–13.9) | 3.4−17.1 umol/L | |
| Potassium, mmol/L | 3.97 (3.65−4.31) | 4.2 (3.8–4.8) | 3.50−5.30 mmol/L | |
| Creatinine, μmol/L | 80.6 (56.5−93) | 74.2 (57.5–85.7) | 44.0−133.0 μmol/L | |
| ≤133 | 14/15 (50 %) | 37/41 (90 %) | 0.594 | |
| >133 | 1/15 (50 %) | 4/41 (10 %) | 0.594 | |
| Uric acid, umol/L | 348.9 (268.8−459.6) | —— | 208.0−428.0 μmol/L | |
| Blood Urea Nitrogen, mol/L | 4.13 (3.1−4.98) | —— | 2.90−7.14 mmol/L | |
| Creatine kinase, U/L | 120.5 (82.1−165.75) | 132.5 (62.0–219.0) | 50.0−310.0 U/L | |
| ≤185 | 14/17 (93 %) | 27/40 (68 %) | 0.209 | |
| >185 | 3/17 (7%) | 13/40 (33 %) | 0.209 | |
| Lactate dehydrogenase, U/L | 254.3 (218.25−315.8) | 286.0 (242.0–408.0) | 120.0−250.0 U/L | |
| ≤245 | 6/13 (46 %) | 11/40 (28 %) | 0.400 | |
| >245 | 7/13 (54 %) | 29/40 (73 %) | 0.400 | |
| Procalcitonin, ng/mL | 0.074 (0.044−0.090) | 0.1 (0.1–0.4) | 0−0.050 ng/mL | |
| C-reactive protein mg/L | 5.23 (1.95−26.68) | —— | ≤10.00 mg/L | |
| Respiratory tract(Ct) | 32.77 (26.3–36.9) | 32.2 (31.0–34.5) | ≤37 | |
| Rtool(Ct) | 34.64 (28.59–36.0) | —— | ≤37 | |
| Mycoplasma pneumoniae IgM | negative | —— | negative |
The clinical and laboratory data of patients in the Wuhan area originated from the article of Huang, C et al [7]. Data are median (IQR), n (%), or n/N (%), where N is the total number of patients with available data. p values comparing Hunan and Wuhan are from χ² test, Fisher’s exact test, or Mann-Whitney U test
Fig. 1.
The clinical data and laboratory data of patients in Wuhan area originated from the article of Huang, C et al [7]. Data are median (IQR). Comparison of laboratory results of patients with SARS-CoV-2 infection at admission in Hunan and Wuhan [7].
The blood counts of patients on admission showed lymphopenia (lymphocyte count less than 1 × 10⁹/L; 17 (61 %) of 28 patients), while the white blood cell count was usually normal (5.23 × 10⁹/L (1.95−26.68)). The level of D-dimer in Hunan’s [median D-dimer level 0.92 mg/L (0.8−1.11)] was higher than that in Wuhan’s [median D-dimer level 0.5 mg/L (0.3–1.3)]. Levels of alanine amino transferase [28.85 U/L (22.68−41.25)] and aspartate amino transferase [30.95 U/L (22.7−42.53)] in Hunan showed no statistical significance with Wuhan’s. Total bilirubin [73.15 mmol/L (72.22−79.18)] was increased substantially in Hunan patients. Uric acid [348.9 mmol/L (268.8−459.6)] and blood urea nitrogen [4.13 mol/L (3.1−4.98)] were dramatically changed in different patients. The creatine kinase of Hunan patients [120.5U/L (82.1−165.75)] manifested a smaller change compared to Wuhan [132.5 U/L (62.0–219.0)], and lactate dehydrogenase [254.3 U/L (218.25−315.8) was increased in the most patients. These reminded the function of liver, heart and kidney will be slightly damaged. The serum levels of procalcitonin on admission of most patients is normal [0.074 ng/mL (0.0445−0.09025)]. However, patients usually manifested higher C-reactive protein [5.23 mg/L (1.95−26.68)]. Mycoplasma pneumoniae IgM did not rise in all patients and we also did not find cases of co-infection between Influenza A/B virus and SARS-CoV-2. Cycle threshold of respiratory tract [Ct = 32.77 (26.3–36.9)] and stool [Ct = 34.64 (28.59–36.0)] were below the reference value (Ct = 37) (Table 2).
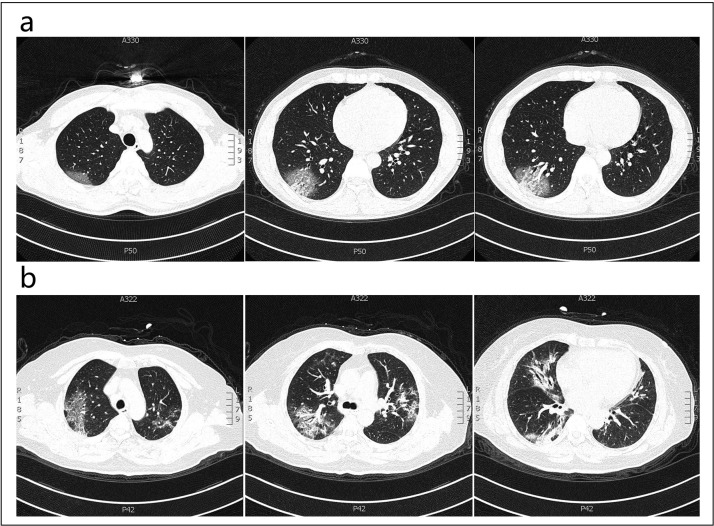
On admission, abnormalities in chest CT images were detected among most patients. The Report of CT results of COVID-19 patients in Wuhan area originated from Pan, Y et al. [10]. Of the 19 patients in Hunan, 6 (31.6 %) did not show obvious abnormalities. The typical findings of chest CT images of patients [6 (31.6 %)] were patchy/punctate ground glass opacities (Fig. 2 b). Only two patient’s CT images performed ground glass opacity, patchy consolidation and fibrous stripes (10.5 %) (Fig. 2a). Compared with patients in Wuhan, the pathological changes in the lungs of Hunan patients were milder in CT (69.4 %) and chest radiographs (62.5 %) (Table 3 ).
Fig. 2.
(a) Transverse chest CT images from a 40-year-old man showing bilateral ground-glass opacity. (b) Transverse chest CT images from a 53-year-old woman showing patchy/punctate ground glass opacities。.
Table 3.
Comparison of CT and chest radiographs features of patients on admission with SARS-CoV-2 infection in Hunan and Wuhan [10].
| Area | Hu nan | Wu han | p |
|---|---|---|---|
| All patients | 19 | 63 | |
| No obvious abnormalities | 6 (31.6 %) | 0 (00.0 %) | 0.001 |
| Ground glass opacity | 2 (10.5 %) | 14 (22.2 %) | 0.218 |
| Patchy/punctate ground glass opacities | 6 (31.6 %) | 54 (85.7 %) | 0.001 |
| Patchy consolidation | 2 (10.5 %) | 12 (19.0 %) | 0.315 |
| Fibrous stripes | 2 (10.5 %) | 11 (17.5 %) | 0.373 |
| Irregular solid nodules | 1 (5.3 %) | 8 (12.7 %) | 0.004 |
| Chest radiographs | 10/16 (62.5 %) | 40/41 (98 %) | 0.001 |
Report of CT results of COVID-19 patients in the Wuhan area originated from Pan, Y et al [10]. Data are median (IQR), n (%), or n/N (%), where N is the total number of patients with available data. p values comparing Hunan and Wuhan are from χ² test, Fisher’s exact test, or Mann-Whitney U test
Many patients with COVID-19 in Hunan region showed significant symptoms of diarrhea. By testing nucleic acid levels in stool of these patients, we found that the virus was present in both the respiratory tract and the stool of eight patients. Of these patients, there is no statistical difference between cycle threshold of respiratory tract and stool (p = 0.893). The expression amount of Nucleic acid is not related to diarrhea (p = 0.285) (Table 4 ). However, by testing nucleic acid levels in tears, we found the virus in 6 patients’ respiratory tract while their tears were negative (Table 5 ).
Table 4.
Nucleic acid test results of respiratory and fecal specimens of 8 patients with SARS-CoV-2 infection at admission.
| Number | Age | Sex | Fever | Cough | Diarrhea | Cycle threshold of respiratory tract | Cycle threshold of stool |
|---|---|---|---|---|---|---|---|
| 1 | 40 | Men | Positive | negative | Positive | 37.78 | 36.08 |
| 2 | 41 | Women | Positive | Positive | Positive | 31.17 | 25.81 |
| 3 | 70 | Women | Positive | Positive | Positive | 38.75 | 34.55 |
| 4 | 54 | Men | Positive | Positive | Positive | 24.65 | 26.96 |
| 5 | 66 | Men | Positive | Positive | Positive | 25.42 | 33.47 |
| 6 | 72 | Men | negative | negative | negative | 38.69 | 38.99 |
| 7 | 37 | Men | Positive | Positive | negative | 30.2 | 35.75 |
| 8 | 51 | Women | Positive | negative | negative | 32.98 | 33.53 |
8 patients were tested for nucleic acid levels in stool and respiratory tract, and stool both carried virus. CT results <37.
Table 5.
Nucleic acid test results of respiratory and tear specimens of 6 patients with SARS-CoV-2 infection at admission.
| Number | Age | Sex | Fever | Cough | Diarrhea | Cycle threshold of respiratory tract | Cycle threshold of tear |
|---|---|---|---|---|---|---|---|
| 1 | 29 | Men | Positive | negative | negative | 34.22 | >40 |
| 2 | 31 | Men | Positive | negative | negative | 24.69 | >40 |
| 3 | 45 | Men | negative | negative | negative | 25.23 | >40 |
| 4 | 40 | Women | Positive | negative | negative | 34.02 | >40 |
| 5 | 32 | Women | negative | Positive | negative | 25.22 | >40 |
| 6 | 37 | Men | Positive | negative | negative | 21.76 | >40 |
6 patients were tested for nucleic acid levels in tear and respiratory tract, and tear both did not carry virus. CT results>40.
5. Discussion
Within weeks after the outbreak of the COVID-19, China quickly developed a nucleic acid detection protocol for this virus. This is the first time we have proposed a preliminary screening program for COVID-19 patients in Hunan. We detected SARS-CoV-2 in oral swabs and stools, because infected patients may release this pathogen through the respiratory tract, feces or body fluids.
The white blood cell counts of most newly diagnosed patients with COVID-19 in Hunan area were normal. Even so he will be accompanied by significant decrease in lymphocyte counts and electrolyte disturbances. Some patients have impaired in cardiac, renal and liver functions. Diagnostic value of X-ray and CT for patients in Hunan was lower, on account of no significant pathological changes in the lungs of most early COVID-19 patients [10]. Most patients presented with fever, but hardly accompanied with dyspnea/Most patients are accompanied by fever instead of the symptoms of dyspnea, which is significantly different from the clinical symptoms of patients in Wuhan. This may be rare related to the second-generation infection of the virus outside Wuhan. In an early report in Wuhan, China, 2–10 % of COVID-19 patients developed symptoms of diarrhea. Such patients are more likely to be admitted to the intensive care unit (ICU). And there are related studies showing that transmission of SARS-CoV-2 may be faecal-oral. In our study, it was found that patients outside Hubei may have up to 15 % of their first symptoms as diarrhea. It is worth mentioning that more patients in Hunan suffer from the diarrhea, and the stool nucleic acid positive rate is higher. All of the above phenomenon may be related to regional differences. Therefore, every doctor needs to be alert to such a phenomenon, whether to perform SARS-CoV-2 nucleic acid detection on diarrhea patients instead of only those patients with flu symptoms. Such findings have more positive significance for the global prevention and control of COVID-19.
All COVID-19 patients are negative in Influenza A/B virus nucleic acid, and this phenomenon suggesting there may be interference between viruses. When two viruses infect the same cell or body, the phenomenon that one virus inhibits the replication of another virus is called interference [11], and the specific mechanism needs further research.
Due to various factors such as specimen type, collection method, transportation, and performance limitations of the kit, the positive rate of RT-PCR screening for new coronary pneumonia is not ideal. The total positive rate of pharyngeal swab nucleic acid detection is about 60 %, which sometimes cannot meet the clinical requirements. However, the specificity of chest CT diagnosis of COVID-19 is only 25 %. As the disease progresses, the specificity of CT will be lower, and it is difficult to distinguish COVID-19 from general pneumonia. The rate of missed diagnosis of nucleic acid detection is high, and there are many patients in Wuhan, at this point, CT screening showed its advantages. It can help detect patients as soon as possible, and then the patients will be isolated and treated as soon as possible. It is affordable to combining CT screening and nucleic acid detection because of the fewer patients in Hunan and other places.
During the initial screening process, a comprehensive analysis of the patient's epidemiological history, symptoms, and laboratory tests is required. If necessary, further chest CT or combination with nucleic acid testing is performed. The laboratory nucleic acid test is a crucial tool for detecting viral pneumonia anytime. If the Hunan area hospitals adopt clinical COVID-19 diagnosis measures similar to Hubei area, it will often lead to a higher misdiagnosis rate. During the epidemic period, the lower lymphocyte count of the test results is more suggestive. Pharyngeal swabs and stool simultaneous nucleic acid testing are still the first choices for early diagnosis of patients with SARS-CoV-2 in Hunan.
Interestingly, we also found that four patients were diagnosed with COVID-19 without clinical symptoms. All of them have a history of Wuhan sojourn or contact with relevant people. Therefore, suspected-infected patients without clinical symptoms still need to be excluded via nucleic acid testing. Screening of crowd who contacts of confirmed COVID-19 patients is currently recommended, what’s more systematic screening of crowd outside of health care facilities and avoiding cluster activities should be encouraged [12].
Author contributions
Sheng Yin and Yizhi Peng have the same contribution. Min Wang and Wenlong Wang have the same contribution and are corresponding authors. All authors have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; and have been involved in drafting the manuscript or revising it critically for important intellectual content; and have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and have agreed to be accountable for all aspects of the work.
Declaration of Competing Interest
All the authors have no conflict of interest.
Acknowledgments
This work was supported by grants from the Hunan Scientific and Technological Department Special Project under the COVID-19 Emergency (Grant No. 2020SK3018), the Hunan Provincial Natural Science Foundation of China (Grant No. 2019JJ40426), the Hunan Provincial Natural Science Foundation of China (Grant No. 2019JJ40418), the Hunan Provincial Clinical Medical Technology Innovation Guide Project (Grant No. 2017SK50122), the Fundamental Research Funds for the Central Universities of Central South University (Grant NO. 2019zzts806).
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jcv.2020.104397.
Contributor Information
Min Wang, Email: wangmin0000@csu.edu.cn.
Wenlong Wang, Email: wangwenlong@csu.edu.cn.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan X., Chen D., Xia Y. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phan T. Genetic diversity and evolution of SARS-CoV-2. Infect. Genet. Evol. 2020 doi: 10.1016/j.meegid.2020.104260. 104260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang N., Li S.Y., Yang X.L. Serological evidence of bat SARS-related coronavirus infection in humans, China. Virol. Sin. 2018;33(1):104–107. doi: 10.1007/s12250-018-0012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson R. Pandemic potential of 2019-nCoV. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chu D.K.W., Pan Y., Cheng S.M.S. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin. Chem. 2020 doi: 10.1093/clinchem/hvaa029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan Y., Guan H., Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur. Radiol. 2020 doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar N., Sharma S., Barua S., Tripathi B.N., Rouse B.T. Virological and immunological outcomes of coinfections. Clin. Microbiol. Rev. 2018;31(4) doi: 10.1128/CMR.00111-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant R., Malik M.R., Elkholy A., Van Kerkhove M.D. A review of asymptomatic and sub-clinical middle east respiratory syndrome coronavirus infections. Epidemiol. Rev. 2019 doi: 10.1093/epirev/mxz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.