Abstract
Background
Guidelines and clinical practice for the prevention of complications associated with central venous catheters (CVC) around the world vary greatly. Most institutions recommend the use of heparin to prevent occlusion; there is debate, however, regarding the need for heparin and evidence to suggest normal saline (0.9% sodium chloride) may be as effective. The use of heparin is not without risk, may be unnecessary and is also associated with increased cost. This is an update of the review published in 2015.
Objectives
To assess the clinical effects (benefits and harms) of intermittent flushing of normal saline versus heparin to prevent occlusion in long‐term central venous catheters in infants and children.
Search methods
The Cochrane Vascular Information Specialist searched the Cochrane Vascular Specialised Register, CENTRAL, MEDLINE, Embase and CINAHL databases; World Health Organization International Clinical Trials Registry Platform and ClinicalTrials.gov trials register to 9 April 2019. We also undertook reference checking, citation searching and contact with study authors to identify additional studies.
Selection criteria
We included randomised controlled trials (RCTs) that compared the efficacy of intermittent flushing with normal saline versus heparin to prevent occlusion of long‐term CVCs in infants and children aged up to 18 years of age. We excluded temporary CVCs and peripherally inserted central catheters (PICC).
Data collection and analysis
Two review authors independently assessed trial inclusion criteria, trial quality and extracted data. We assessed study quality with the Cochrane 'Risk of bias' tool. For dichotomous outcomes, we calculated the rate ratio (RR) and corresponding 95% confidence interval (CI). We pooled data using a random‐effects model; and we used GRADE to assess the overall certainty of the evidence supporting the outcomes assessed in this review.
Main results
We identified one new study for this update, bringing the total number of included studies to four (255 participants). The four trials directly compared the use of normal saline and heparin; the studies all used different protocols for the intervention and control arms, however, and all used different concentrations of heparin. Different frequencies of flushes were also reported between studies. In addition, not all studies reported on all outcomes. The certainty of the evidence ranged from moderate to very low because there was no blinding; heterogeneity and inconsistency between studies was high; and the CIs were wide. CVC occlusion was assessed in all four trials. We were able to pool the results of two trials for the outcomes of CVC occlusion and CVC‐associated blood stream infection. The estimated RR for CVC occlusion per 1000 catheter days between the normal saline and heparin groups was 0.75 (95% CI 0.10 to 5.51; 2 studies, 229 participants; very low certainty evidence). The estimated RR for CVC‐associated blood stream infection was 1.48 (95% CI 0.24 to 9.37; 2 studies, 231 participants; low‐certainty evidence). The duration of catheter placement was reported to be similar for the two study arms in one study (203 participants; moderate‐certainty evidence), and not reported in the remaining studies.
Authors' conclusions
The review found that there was not enough evidence to determine the effects of intermittent flushing with normal saline versus heparin to prevent occlusion in long‐term central venous catheters in infants and children. It remains unclear whether heparin is necessary to prevent occlusion, CVC‐associated blood stream infection or effects duration of catheter placement. Lack of agreement between institutions around the world regarding the appropriate care and maintenance of these devices remains.
Plain language summary
Replacing heparin flushing with saline flushing to prevent complications in long‐term central venous catheters in children
Background
A central venous catheter (CVC) is a long, thin, flexible tube which is inserted into a large central vein. This enables access to the blood stream for people with serious medical conditions to receive medications and fluids, as well as the collection of blood specimens. Long‐term CVCs are used to access the blood system in children with complex medical conditions like cancer. To stop the catheter from becoming blocked it is usual to use heparin, a drug that prevents clots forming, to flush the catheter. However, some studies have shown that heparin is not necessary, and that normal saline (a sterile salt water solution) can be safely used instead. Heparin may be associated with complications, such as bleeding and infection, along with higher costs for healthcare providers. While the complications such as infections and occlusions are uncommon, practices vary around the world and there are many inconsistencies regarding the best flush solution to use to prevent complications in long‐term catheters.
Study characteristics and key results
This review included randomised controlled trials (clinical studies where people were randomly assigned into one of two or more treatment groups) that compared the use of saline and heparin to prevent blockage, and other complications related to long‐term catheters. The evidence is current to 9 April 2019. Two review authors independently reviewed the studies. We included four studies with a total of 255 participants in the review. The four trials were all undertaken in large teaching (tertiary) hospitals, and directly compared the use of saline and heparin. The studies were, however, very different in the way they compared saline and heparin, with different concentrations of heparin and different frequencies of flushes reported. We were able to combine the results of two studies: the analysis showed imprecise results for the blocking of catheters and blood stream infections for normal saline versus heparin. One study reported the duration of catheter placement to be similar between the two study arms.
Certainty of the evidence
The overall certainty of the evidence ranged from moderate to very low. There was high risk of bias for blinding, there were differences between the studies methods and interventions, inconsistent results between the studies, and not all studies reported all outcomes of interest. We found there was not enough evidence to determine which solution, saline or heparin, is more effective for reducing complications. Further research is required and is likely to have an important impact in this area. This review is an update of a review first published in 2015.
Summary of findings
Summary of findings 1. Does normal saline flushing in long‐term central venous catheters (CVC) prevent occlusion compared to heparin flushing in infants and children?
| Normal saline versus heparin flushing for prevention of occlusion in long‐term CVC in infants and children | ||||||
| Patient or population: infants and children with a long‐term CVC Settings: tertiary hospitals Intervention: normal saline flush Control: heparin flush | ||||||
| Outcomes | Anticipated absolute effects * (95% CI) | Relative effect (95% CI) | No. of participants (RCTs) | Certainty of the evidence (GRADE) | Comments | |
| Risk with heparin flush | Risk with normal saline flush | |||||
|
CVC occlusion rate per 1000 catheter days: ability to infuse solution through CVC Follow‐up: 3029 to 115,991 at‐risk days |
Study population | Rate ratio 0.75 (0.10 to 5.51) | 229 (2 RCTs) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 551 per 1000 | 507 per 1000 (99 to 1000) | |||||
|
CVC‐associated blood stream infection rate per 1000 catheter days: incidence of positive blood culture Follow‐up: 3029 to 115,991 at‐risk days |
Study population | Rate ratio 1.48 (0.24 to 9.37) | 231 (2 RCTs) | ⊕⊕⊝⊝ low1,3,4,5 | ||
| 93 per 1000 | 209 per 1000 (103 to 425) | |||||
|
Duration of CVC placement (days) Follow up: median 360 days |
See comment | 203 (1 RCT) |
⊕⊕⊕⊝ moderate1,4 | Cesaro 2009 reported this in terms of survival, not in days. Mean survival was reported as 77% (95% CI 66% to 84%) in the normal saline group and 69% (95% CI 53% to 80%) in the heparin group. No differences were found in cause or frequency of premature removal of catheter between study arms. The remaining studies did not report on this outcome. | ||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; CVC: Central venous catheter; RCTs: Randomised controlled trial | ||||||
|
GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1No blinding in either study. Performance and detection bias is high in both studies 2Heterogeneity and inconsistency between studies is high 3Confidence intervals were wide and included the null hypothesis 4Results could be attributed to other factors associated with the use of heparin 5The outcomes could also be attributed to the use of positive pressure cap in the Cesaro 2009 study
Background
Description of the condition
A central venous catheter (CVC) is a long, thin, flexible tube which is inserted into a large central vein, with the tip of the catheter ideally placed within the superior vena cava (Schuster 2000). This enables the administration of medications and fluids, as well as the collection of blood specimens, and avoids multiple venipunctures. CVCs are commonly known as 'central lines' or by their brand name including Broviac, Hickman, and Port‐a‐Cath. The use of long‐term CVCs for the management of chronic medical conditions in infants and children has greatly improved the quality and safety of care provision. Long‐term CVCs are typically inserted when the administration of intravenous medication or nutritional support is required over a considerable time period. Hypertonic medications such as vesicant chemotherapy drugs, certain antibiotics, other supportive drugs and parenteral nutrition cannot be safely administered through peripheral venous catheters. For children with cancer and other chronic medical conditions who require such medications, this safety issue is overcome by the insertion of a CVC which commonly remains in place for the duration of treatment (Gonzalez 2012). There are three types of long‐term CVCs: tunnelled catheters; totally implanted catheters; and peripherally inserted central catheters (PICC). A tunnelled CVC is surgically inserted under the skin, with the catheter lumen(s) typically exiting from the chest or neck. A totally implanted catheter is also surgically inserted, but is placed entirely under the skin and commonly referred to as a 'port'. The port reservoir is accessed with a needle through the skin. A PICC line is inserted into a central vein through the arm and thus is a narrower catheter.
Adverse events associated with CVCs may cause complications in up to 46% of children (Athale 2012). Adverse events in the scope of this review include mechanical failure, catheter fracture, infections and intravascular thrombosis, all of which can affect patient morbidity and mortality (Baskin 2009; Fratino 2005; Stocco 2012; Wong 2012). Mechanical failure is often attributed to catheter occlusion. Over time, it is common for a fibrin sheath to develop at the tip of the catheter. The fibrin sheath may prevent aspiration of blood from the catheter and cause resistance when infusing fluids. An intraluminal clot can also occur, which can totally occlude the catheter. Intraluminal clots may occur as a result of precipitate from medications, which would not be prevented by use of heparin; or from blood refluxing into the catheter lumen and forming a clot. Occlusion can result in the need for the catheter to be removed (and replaced), interrupting and delaying treatment of the underlying disease (Shah 2007). Occlusions of CVCs are estimated to occur in 14% to 36% of patients within one to two years of catheter insertion (Fratino 2005); or at an incidence rate of 1.35 per 1000 catheter days (95% confidence interval (CI) 1.10 to 1.63) (Revel‐Vilk 2010). Incidence rates of central‐line‐associated blood stream infection differ depending upon the type of catheter, with rates reported between 1.40 per 1000 catheter days (95% CI 1.06 to 1.82) and 0.46 per 1000 catheter days (95% CI 0.29 to 0.69). Intravascular thrombosis is the rarest adverse event reported in children, with a lower incidence rate of 0.08 per 1000 catheter days (95% CI 0.04 to 0.16), and can only be diagnosed by radiographic methods (Fratino 2005). Intravascular thrombosis may or may not occur concurrently with other complications.
Description of the intervention
A flush refers to a solution of 0.9% sodium chloride (normal saline) injected to clear or 'rinse' the catheter of blood or fibrin build‐up. This is commonly used when the catheter is accessed, between administration of medications, or before and after collection of blood specimens. A lock is used to instil fluid into the catheter when the catheter will not be accessed for a period of time. A positive pressure lock refers to the technique used to ensure blood does not flow back into the catheter after it is flushed, which may otherwise clot and cause occlusion. Tunnelled CVCs and PICC lines are typically flushed and locked weekly, while implanted ports are flushed and locked every 4 to 6 weeks. A typical lock solution for tunnelled catheters in children is to use between 1 mL to 3 mL (depending on the volume of the catheter) of 10 units/mL of heparin for a 24‐hour to 7‐day lock. For implanted ports, 5 mL of 100 units/mL is typically used as a lock solution for a 30‐day lock (Davis 2013). There is debate, however, regarding the effectiveness of heparin to prevent occlusion over such time periods, given its short half‐life (Young 2008). The evidence to support the use of heparin to prevent occlusion in adult CVCs is inconclusive and there is growing evidence to support the use of normal saline to lock CVCs, particularly in the paediatric population (Bertoglio 2012; Lee 2005). In paediatrics, there is an additional risk of bleeding due to overdose of heparin from frequent flushing or incorrect dilution.
How the intervention might work
Heparin is used to prevent occlusion because of its anticoagulant properties which are believed to prevent thrombus forming in the catheter. Alternatively normal saline, when used with pulsatile (push‒pause rather than continuous) flushing techniques and a positive pressure lock or positive displacement device, may be as effective in preventing thrombus formation in catheters—eliminating the need for heparin to be used (Bertoglio 2012).
Why it is important to do this review
Catheter maintenance practices vary among institutions because of the lack of evidence regarding best practice to prevent occlusion of CVCs. Variations include the quantity of flush and lock solutions, the proportional volume of heparin lock solution, the concentration of heparin, and the frequency of flushes and locks. The use of heparin is not risk free and in certain instances may actually cause harm, including infection (Shanks 2005), and heparin‐induced thrombocytopenia (HIT) (Barclay 2012). The mechanism of haemostasis in children is different when compared to adults, particularly in infants and very young children; and the evidence suggests algorithms used in adults are unlikely to be valid in children (Monagle 2010). Additionally, treatments for diseases such as cancer involve the use of medications which can affect coagulation. In the absence of specific data related to paediatrics, using evidence based on adults may be inappropriate and there is a need for paediatric‐specific studies (Monagle 2010). For these reasons the use of heparin to prevent CVC occlusion should be judicious and evidence based. While the risks of adverse effects from the use of heparin may be regarded as less than those which might arise from occlusion of a catheter and subsequent replacement, it is important to ensure interventions are based on evidence.
In the adult population, there have been several trials investigating heparin versus normal saline to prevent occlusions in CVCs, six of which are summarised in a Cochrane Review (Lopez‐Briz 2018). As evidence from adult studies is not directly transferable to paediatrics, systematic reviews focused on infants and children are required. A review published in 2014 that did relate specifically to paediatrics did not identify all relevant studies and made recommendations based on the current practice of several institutions (Conway 2014). These recommendations were not evidence based, and are contrary to the practice of many other institutions. It is important, therefore, to systematically appraise the evidence for the use of normal saline compared with heparin to prevent occlusion of CVCs. This is an update of a previously published systematic review (Bradford 2015).
Objectives
To assess the clinical effects (benefits and harms) of intermittent flushing of normal saline versus heparin to prevent occlusion in long‐term central venous catheters in infants and children.
Methods
Criteria for considering studies for this review
Types of studies
We considered all randomised controlled trials (RCTs) that compared the efficacy of normal saline with heparin for the prevention of occlusion of central venous catheters (CVCs). Due to potential bias, we excluded studies that used alternative methods (quasi‐randomised) to allocate participants to an intervention or control group.
Types of participants
We included study populations comprising infants and children aged 0 to 18 years, who had a CVC (tunnelled catheter or totally implanted catheter) inserted for long‐term venous access. Because midline catheters are not placed in the same position as a CVC (superior or inferior vena cava), and PICC have narrow lumens which require specific care, studies of infants or children with midline catheters or PICCs were beyond the scope of this review and we excluded them. We placed no restrictions on the insertion site, or catheter tip placement site (superior or inferior vena cava). We placed no restrictions on the healthcare setting in which the study was conducted, for example tertiary hospital or community setting. Where studies had a mixed population that included infants, children and adults, we included data from infants and children only. If information was not presented in the article, we contacted the study authors to attempt to obtain age‐stratified results. If we were unable to contact the study authors, and children and infants comprised a proportion greater than 20% of the study population, we included the appropriate proportion of participants to represent the paediatric component. If we were unable to obtain any information regarding the proportion of infants and children in the study population, we excluded the study from the review.
Types of interventions
We included studies where the intervention of interest was the intermittent (any time frequency) flushing of normal saline (alone, or in combination with pulsatile flushing techniques, positive displacement devices or positive pressure lock) compared with intermittent flushing with heparin (any dose or concentration) delivered with the intention to prevent occlusion of the CVC.
Types of outcome measures
We did not consider outcome measures to be a part of eligibility criteria.
Primary outcomes
Occlusion of the CVC, determined by the inability to infuse fluids through the catheter
CVC‐associated blood stream infection or colonisation of the catheter (as defined by studies)
Duration in days of catheter placement
Secondary outcomes
Inability to withdraw blood from the CVC
Any use of urokinase or recombinant tissue plasminogen such as alteplase
Incidence of removal/re‐insertion of the catheter
CVC‐related thrombosis
Other CVC‐related complication (e.g. dislocation of CVCs, tunnel or site infection, allergic reaction, haemorrhage, heparin‐induced thrombocytopenia, elevated hepatic enzymes)
Search methods for identification of studies
Electronic searches
The Cochrane Vascular Information Specialist conducted systematic searches of the following databases for randomised controlled trials and controlled clinical trials without language, publication year or publication status restrictions.
Cochrane Vascular Specialised Register via the Cochrane Register of Studies (CRS Web searched on 9 April 2019)
Cochrane Central Register of Controlled Trials (CENTRAL) Cochrane Register of Studies Online (CRSO 2019, 3)
MEDLINE (Ovid MEDLINE® Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE®) (searched from 1 January 2017 to 9 April 2019)
Embase Ovid (searched from 1 January 2017 to 9 April 2019)
CINAHL EBSCO (searched from 1 January 2017 to 9 April 2019)
AMED Ovid (searched from 1 January 2017 to 9 April 2019)
The Information Specialist modelled search strategies for other databases on the search strategy designed for CENTRAL. Where appropriate, they were combined with adaptations of the Highly Sensitive Search Strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions, Chapter 6, Lefebvre 2011). Search strategies for major databases are provided in Appendix 1.
The Information Specialist searched the following trials registries on 9 April 2019.
World Health Organization (WHO) International Clinical Trials Registry Platform (who.int/trialsearch)
ClinicalTrials.gov
Searching other resources
Two review authors (NB, RE) screened the reference lists of retrieved articles for additional studies. We attempted to contact authors of any studies identified in unpublished literature to obtain further data.
Data collection and analysis
Selection of studies
Two review authors (NB, RE) independently reviewed all titles and abstracts of retrieved articles using Covidence software (Covidence), to assess eligibility against inclusion criteria. When disagreement arose regarding the inclusion of a study, the third author (RC) acted as arbitrator. We obtained the full text of all potentially eligible studies and contacted authors of primary studies to clarify data if necessary. We used a flowchart based upon the PRISMA statement to document results (Moher 2009). We recorded data on the results of all searches undertaken including database searched, date, limiters, and number of results. We recorded the reasons for exclusion of studies.
Data extraction and management
Two review authors (NB, RC) extracted the data independently using the Cochrane Vascular Group forms for dichotomous and continuous data. In the updated review, we also used Covidence to extract data (Covidence). Where available, we collected data regarding the:
lead author and year of study;
country where the study was undertaken;
participant inclusion criteria;
participant age and gender;
study design;
description of interventions;
setting of study;
number of participants in each arm;
attrition or losses to follow‐up;
variables associated with catheter maintenance (e.g. preparation of injectables (pre‐filled or not), caregiver level of education);
outcome measures.
We resolved any disagreement regarding data extraction by discussion between all review authors (NB, RE, RC).
Assessment of risk of bias in included studies
We assessed bias within studies using the tool described in the Cochrane Handbook for Systematic Reviews of Interventions and reported on the following domains: sequence generation; allocation concealment; blinding; incomplete data; selective outcome reporting; and other biases (Higgins 2011b). If necessary, primary authors were contacted to clarify any information. Two review authors (NB, RC) independently undertook the risk of bias assessment. We resolved disagreement regarding the assessment of bias by discussion between review authors (NB, RC).
Measures of treatment effect
As dichotomous outcomes such as occlusion or central‐line‐associated blood stream infection could occur more than once for individual participants (e.g. once in each lumen of a double lumen CVC), we calculated count data per time at risk of outcome (per 1000 catheter days) and reported rate ratios (RR) with 95% confidence intervals (CI). Using section 9.4.8 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011), we also calculated the formula for the log of the standard error (SE) for each RR. We used descriptive statistics, including mean differences (MD) with 95% CI, for any continuous data. We planned to report time‐to‐event data as hazard ratios (HR) with 95% CI. We analysed data with Review Manager software (RevMan Web 2019).
Unit of analysis issues
We identified the unit of analysis in each study at either the patient or the catheter level. We planned to analyse studies separately for different units of analysis. Where results were reported from cluster RCTs, cross‐over trials or repeated measurements of the same outcome, we took the appropriate design effect into consideration to avoid unit of analysis error.
Dealing with missing data
We contacted primary authors of studies to attempt to obtain any missing data. We assessed all data for potential mislabelling and made no assumptions regarding missing data in order to include these in the analysis. Where data were missing and proved to be irretrievable, we excluded them from the analysis.
Assessment of heterogeneity
Where feasible, we assessed heterogeneity between effect sizes of included studies by visual inspection of forest plots and the Chi² test (P value < 0.05). We planned to describe inconsistency between trials by assessing the I² statistic and the variability between the effect estimates (Higgins 2003), with an I² value of 50% considered to represent substantial heterogeneity (Higgins 2011a). Additionally we considered the clinical heterogeneity of studies where the frequency of interventions or catheter type differed between studies.
Assessment of reporting biases
Where appropriate, we planned to assess publication bias using funnel plots and Egger's test (Egger 1997; Sterne 2011). Additionally, we reduced possible reporting bias by searching multiple electronic databases, proceedings of conferences and scientific meetings, and trial registries. We excluded duplicates of the same trial to avoid duplicate publication bias.
Data synthesis
The primary author (NB) entered data into RevMan Web (RevMan Web 2019), and undertook analysis according to recommended guidelines (Deeks 2011). We planned to combine effect sizes across studies using a fixed‐effect model and CI limits set at 95%. Where substantial heterogeneity existed, we pooled data using the random‐effects model. Where it was not appropriate to combine results, we presented a narrative review descriptively summarising the results.
Subgroup analysis and investigation of heterogeneity
We planned to conduct subgroup analysis where appropriate with:
type of CVC (tunnelled catheter or implanted port);
insertion site or catheter tip placement site, or both;
age group;
oncology or other diagnosis;
use of systemic heparin.
We were unable to do this as data were not available.
Sensitivity analysis
We planned to undertake sensitivity analyses to examine the effects of different trials and their methodology including: number of participants (≥ 50 vs < 50 participants); concentration of heparin; and duration of follow‐up. We were unable to do this as data were not available.
Summary of findings and assessment of the certainty of the evidence
We present the main findings of the review results concerning the certainty of evidence, the magnitude of effect of the interventions examined, the sum of available data for the primary outcomes CVC occlusion rate, and CVC‐associated blood stream infection and duration in days of catheter placement in Table 1, according to Schünemann 2011 and Atkins 2004. We used GRADEprofiler (GRADEpro) software to assist in the preparation of the 'Summary of findings' table (GRADEpro GDT).
Results
Description of studies
Results of the search
See Figure 1.
1.
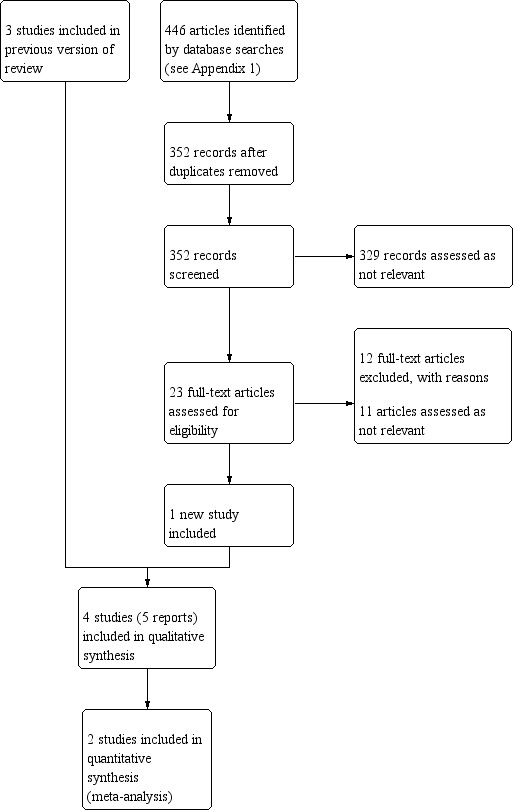
Study flow diagram.
We identified one new study for this update (da Silva 2018); and included three studies from the previous version (Cesaro 2009; Goossens 2013; Smith 1991). We excluded 12 new studies (Arauj 2011; Arnts 2011; Brito 2018; Heidari Gorji 2015; Klein 2017; Klein 2018; NCT01343680; NCT00001518; NCT02354118; NCT02923830; Reichardt 2002; Schallom 2012).
Included studies
Based on the review of full texts, four studies met eligibility criteria and we have included them in the final updated review (Cesaro 2009; da Silva 2018; Goossens 2013; Smith 1991) (see Table: Characteristics of included studies). The studies undertaken by Cesaro 2009 and Goossens 2013 were of medium duration (25 and 23 months respectively) and included follow‐up periods of 14 and six months respectively. The Smith 1991 study was a cross‐over study of two time periods, each of three‐and‐a‐half months (total duration seven months) and did not include a follow‐up period. We were not able to ascertain if this study was analysed as paired data or not, and no information was available regarding the first cross‐over period. The da Silva 2018 study was a dissertation thesis and was undertaken over a period of 180 days without a follow‐up period. All studies had obtained ethical approval from their relevant institutions.
Population
The four included trials involved a total of 255 participants, with the majority of participants (203) coming from Cesaro 2009. Of the other three studies, Goossens 2013 contributed 28 participants, Smith 1991 contributed 14 participants and da Silva 2018 10 participants. Goossens 2013 and da Silva 2018 were not trials specific to children; Goossens 2013 had more participants in the control arm (n = 17) compared to the intervention arm (n = 11); and child participant numbers were balanced between the intervention and control arms in da Silva 2018. All participants had a long‐term central venous catheter (CVC), and were undergoing treatment for haematology or oncology conditions, or undergoing stem cell transplantation. Cesaro 2009 was undertaken in Italy, Goossens 2013 in Belgium, Smith 1991 in Canada and da Silva 2018 in Brazil. Participants in Smith 1991 and Cesaro 2009 had Broviac tunnelled CVCs inserted, da Silva 2018 participants all had Hickman catheters inserted, whereas all participants in Goossens 2013 had totally inserted catheters (ports) placed. All studies were undertaken in developed nations in tertiary referral centres, i.e. large hospitals that provide specialist health care after referral from the providers of primary care and secondary care. Both Cesaro 2009 and Goossens 2013 undertook power size calculations to obtain sample sizes; it is important to note, however, that children comprised only 3.5% of the Goossens 2013 study population, thus this study was not powered to analyse the results of children separately. Smith 1991 was a small study with only 14 participants. da Silva 2018 recruited only 17 of a planned 100 participants, of which 10 were children aged less than 18 years.
Intervention
Participants in all four included studies received standard care except where stated as follows.
All included studies involved an intervention arm where normal saline solution was used in place of heparinised saline when the CVC was not being used. As well as changing the type of solution used to flush the CVC, Smith 1991 increased the duration between flushes in the intervention arm. Participants in the control arm received standard care with CVCs flushed twice daily. In the intervention arm, the duration between flushes was increased to weekly. Similarly, Cesaro 2009 increased the duration between flushes in the intervention arm compared to standard care from twice per week to weekly. Cesaro 2009 also introduced a positive pressure cap into the intervention arm. These changes confound the interventions so it is not possible to associate outcomes with the use of the solution alone. Goossens 2013 and da Silva 2018 were the only two studies included in this review where the only difference between the intervention and control arm was the use of normal saline (intervention) or heparin (control) solution to flush the CVC under positive pressure. In da Silva 2018, it was not clear when participants received either solution; participants were inpatients and four syringes were prepared daily with either normal saline or heparin. However there is no information about when these syringes were administered, or if all four were administered each day. The intervention arm in da Silva 2018 may have received up to four catheter locks of normal saline each day. These catheter locks were administered whenever a catheter was not used.
Control
In all studies, participants randomised to the control arm received various concentrations of heparinised saline to flush their CVC. Participants in Smith 1991 received 5 mL of 10 units/mL heparinised saline (i.e. 50 units of heparin) twice daily. Participants in Cesaro 2009 received 3 mL of 200 units/mL heparinised saline (i.e. 600 units of heparin) twice weekly. In Goossens 2013, participants in the control arm received maintenance care (normal saline pulsatile flushes after infusions, blood sampling, etc.), and their CVC was flushed with 3 mL of 100 units/mL heparin (i.e. 300 units of heparin) under positive pressure at least every eight weeks when the CVC was not in use. In da Silva 2018, the control arm received up to four syringes daily of 3 mL containing 50 units of heparin per mL (150 units of heparin per syringe).
Outcomes
The primary outcome of interest, occlusion of CVC, was measured in all four studies included in this review. In Smith 1991, occlusion was defined as blockage of the catheter and measured by both echocardiogram to determine thrombus formation and inability to infuse fluids. Smith 1991 also recorded CVC‐associated blood stream and exit site infections. Blood stream infections were defined by Smith 1991 as the presence of systemic infection and positive blood cultures, and exit site infections were defined as the presence of infection and positive culture from the exit site. Cesaro 2009 defined CVC occlusion as the inability to withdraw blood or infuse fluids, or both. Cesaro 2009 also measured CVC‐associated blood stream infection, CVC mechanical issues and CVC‐related thrombosis. CVC‐associated blood stream infection was defined by Cesaro 2009 as one or more positive blood cultures obtained through the CVC in patients with signs of infection. CVC mechanical issues included dislodgement of the CVC tip or cuff, fracture or accidental CVC self‐removal by the patient; these outcomes were evaluated by visual inspection and chest X‐ray. CVC‐related thrombosis was measured where clinically indicated by ultrasound, computed tomography or magnetic resonance imaging. Goossens 2013 measured CVC occlusion as a secondary end point, their primary outcome was partial occlusion defined by easy infusion, difficulty withdrawing from CVC. Other secondary outcome measures in Goossens 2013 were CVC‐associated blood stream infection and other CVC mechanical issues. CVC‐associated blood stream infection was defined by Goossens 2013 as positive blood cultures from the CVC and peripheral veins, and fever or chills in the absence of other infection sources. CVC mechanical issues encompassed all other functional problems encountered with each access. da Silva 2018 measured CVC occlusion daily on both lumens of the CVC, defined as the inability to aspirate fluids/blood. If no fluids/blood could be withdrawn following repositioning, normal saline was injected. If there was resistance or pressure present, the CVC was noted as having a partial occlusion. If no fluids could be infused, the CVC was deemed to have a 'complete occlusion' and the lumen involved was then finished in the study. As the lumens of Hickman catheters are independent, the other lumen could remain in the study until it too occluded, or the study ended. As participants could experience outcomes more than once, all studies except da Silva 2018 reported the number of catheter days that participants in either study arm were at risk of experiencing an outcome.
Excluded studies
For this update, 12 studies were excluded as they did not meet the eligibility criteria (Arauj 2011; Arnts 2011; Brito 2018; Heidari Gorji 2015; Klein 2017; Klein 2018; NCT00001518; NCT01343680; NCT02354118; NCT02923830; Reichardt 2002; Schallom 2012). Six studies were excluded from the previous version (De Neef 2002; Geritz 1992; Kaneko 2004; Pumarola 2007; Rabe 2002; Schultz 2002), making a total of 18 excluded studies. Most studies were excluded because they were adult studies with no children (Arauj 2011; Arnts 2011; Heidari Gorji 2015; Kaneko 2004; Klein 2017; Klein 2018; NCT00001518; NCT01343680; NCT02354118; NCT02923830; Rabe 2002; Reichardt 2002; Schallom 2012). One study was not a RCT (Brito 2018); and one study was terminated after recruiting only two participants (NCT01343680). Geritz 1992 and Schultz 2002 reported trials investigating peripheral catheters; De Neef 2002 and Kaneko 2004 investigated arterial catheters; and Pumarola 2007 and Rabe 2002 investigated temporary central venous catheters. See Characteristics of excluded studies.
Risk of bias in included studies
See Figure 2, Figure 3 and Characteristics of included studies.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
There was low risk of selection bias in the Cesaro 2009, Goossens 2013 and da Silva 2018 studies; these investigators reported using computerised random sequencing and concealing allocation until participants had been recruited and provided consent. Smith 1991 did not provide any details regarding how participants were randomised and we therefore judged it to be of unclear risk of selection bias.
Blinding
da Silva 2018 was the only study that reported blinding participants, clinicians and researchers to which arm the participant was allocated and we deemed it to have low risk for performance bias and detection bias. Goossens 2013 stated blinding was not possible for logistical reasons. All outcomes were objectively measured, but in Cesaro 2009, Goossens 2013 and Smith 1991 there is the possibility clinicians may have modified their technique depending on the arm to which the participant had been allocated. We therefore assessed these three studies at high risk of both performance and detection bias.
Incomplete outcome data
All four studies included in this review reported full results for all participants who were randomised. A flowchart of participant progress through the study was provided by Goossens 2013. There were no protocol violations reported by Goossens 2013 or Cesaro 2009. In Goossens 2013 there was a 4.9% dropout rate which was not statistically different between the two groups and all analysis was based on intention to treat. This dropout rate relates to the adult participants and not the children included in this review. In Cesaro 2009, 22% (n = 44) of CVCs required premature removal; there were, however, no statistical differences between study arms. Attrition of two participants due to death also occurred in this study but no losses to follow‐up occurred. Smith 1991 and da Silva 2018 reported no losses to follow‐up. We assigned Cesaro 2009, da Silva 2018 and Smith 1991 a low risk of attrition bias, and Goossens 2013 an unclear risk.
Selective reporting
All studies reported on their primary and secondary outcome measures. There was a study protocol for da Silva 2018; we therefore deemed risk of reporting bias for this study to be low. Neither Cesaro 2009 nor Goossens 2013 had a published protocol and so we deemed them at unclear risk. Smith 1991 reported data in a basic format with no results from statistical tests. It is not clear if paired analysis was undertaken; we assessed this study as being at high risk for reporting bias.
Other potential sources of bias
In both the Cesaro 2009 and Smith 1991 studies, there is a high concern for confounding of results. Both these studies altered the frequency between flushes for the intervention arm as well as the concentration of the heparin solution. Additionally, the intervention arm included the use of a positive pressure cap in Cesaro 2009. It is not possible therefore to attribute the outcome to the use of the solution alone: the outcome could plausibly also be attributed to the frequency of flushes or the use of a positive pressure cap. It may therefore be more appropriate to view the intervention as a component of a bundle of care. Further bias may exist in the subset of unpublished data of paediatric participants provided by Goossens 2013; we were not able to determine if the characteristics of this subset of participants were subject to other biases. As it is a cross‐over study, there may have been a carry‐over effect of the intervention from one arm to the other in Smith 1991. It is not clear if the study authors considered this. da Silva 2018 recruited only 17 of a planned 100 participants: this small sample size reduced precision of the findings. Additionally it was not clear how long participants remained in the study. These other potential sources of bias across all four studies are substantial and they are all at high risk of bias for this domain.
Effects of interventions
See: Table 1
See Table 1 for the three primary outcomes: CVC occlusion; CVC‐associated blood stream infection or colonisation; and duration in days of catheter placement. See Additional Table 2 for summary of outcome rates per 1000 catheter days.
1. Rate per 1000 catheter days for primary and secondary outcomes.
| Smith 1991 | Cesaro 2009 | Goossens 2013 | ||||
| Outcome | Normal saline | Heparin | Normal saline | Heparin | Normal saline | Heparin |
| CVC occlusion rate per 1000 catheter days | 1.32 | 0.66 | 2.16 | 1.11 | 2.62 | 10.35 |
| CVC‐associated blood stream infection rate per 1000 catheter days | 1.32 | 0.66 | 0.62 | 0.24 | 0.32 | 1.04 |
| Inability to withdraw blood | Not reported | Not reported | Not reported | Not reported | 3.42 | 10.60 |
| CVC dislodgement | 0.33 | 1.65 | 0.47 | 0.54 | Not reported | Not reported |
| CVC site infection | 2.31 | 0.33 | 0.26 | 0.38 | Not reported | Not reported |
| CVC‐related thrombosis | 0.66 | 0.66 | 0.30 | 0.30 | Not reported | Not reported |
CVC: Central venous catheter
da Silva 2018 not included in table as rate per 1000 catheter days not able to be calculated
We were not able to ascertain if Smith 1991 analysed data as paired data or not, and no information was available regarding the first cross‐over period. We were not able to obtain data regarding the child participants in da Silva 2018, or information regarding the number of catheter days. We therefore did not pool results from these two studies with the others.
Primary outcomes
CVC occlusion
CVC occlusion was reported in all four included trials (253 participants; Goossens 2013 provided data for 26 of 28 participants for CVC occlusion). Smith 1991 and Cesaro 2009 provided information regarding the number of catheter days for each arm of their study. Goossens 2013 provided the mean catheter days for each arm of the total population in their study (i.e. including both the child and adult participants). Goossens 2013 provided data specific to children; this did not, however, include disaggregate data regarding the number of mean catheter days. We assumed that the mean number of catheter days for the child participants in each study arm was comparable to that of the adult participants. Based on this information, we calculated the occlusion rate ratio (RR) for the intervention arm (normal saline) versus the control arm (heparin) for each study per 1000 catheter days. In Smith 1991, Cesaro 2009 and da Silva 2018, there were more CVC occlusions in the intervention (normal saline) arm. The RR of CVC occlusion in Smith 1991 was 2.0 (95% CI 0.18 to 21.85), and in Cesaro 2009 the RR was 1.95 (95% CI 1.34 to 2.83). Because of absent data regarding the first period in the cross‐over study design used in Smith 1991, we did not pool results from this study.
We were unable to calculate a RR for da Silva 2018 as there was no information about number of catheter days. We therefore could not pool data for analysis. This study reported survival analysis for each lumen and reported fewer occlusions in the control arm (heparin) compared to the intervention arm (normal saline); in the white lumen for all participants, both children and adults, the mean number of days until occlusion for normal saline was 52 (95% CI 42.92 to 61.07) versus for heparin 13.46 (95% CI 8.16 to 18.77; P < 0.001); and in red lumen for normal saline 35.29 (95% CI 25.59 to 44.98) versus for heparin 22.3 (95% CI 12.42 to 32.18; P = 0.03). In children less than 18 years of age, in the intervention group (normal saline, n = 5) all participants experienced an occlusion in at least one lumen compared to the control group (heparin, n = 5) where only one child experienced occlusion in one lumen. These results for child participants were reported by da Silva 2018 but were not formally assessed.
Goossens 2013 found there were fewer CVC occlusions in the intervention (normal saline) arm; the RR was 0.25 (95% CI 0.09 to 0.73).
When we pooled the results from the Cesaro 2009 and Goossens 2013 studies, the heterogeneity was substantial (I² = 92%); we therefore chose a random‐effects model to estimate the combined effect. Combined analysis suggested there was no clear benefit in the outcome of CVC occlusion between flushing with heparin or normal saline (RR 0.75, 95% CI 0.10 to 5.51; 2 studies, 229 participants; P = 0.78). Heterogeneity between studies indicates this result may be due to differences between the studies. See Analysis 1.1. We downgraded the certainty of the evidence to very low (see Table 1).
1.1. Analysis.

Comparison 1: Normal saline versus heparin flushing, Outcome 1: CVC occlusion rate per 1000 catheter days
CVC‐associated blood stream infection or colonisation
Incidence of CVC‐associated blood stream infection was reported in three included trials (245 participants) (Cesaro 2009; Goossens 2013; Smith 1991). As described above, we calculated RR for each study based upon 1000 catheter days. There were more CVC‐associated blood stream infections in the intervention (normal saline) arm in both Smith 1991 and Cesaro 2009. The RR in Smith 1991 was 2.00 (95% CI 0.18 to 21.85); in Cesaro 2009 the RR was 2.58 (95% CI 1.20 to 5.54). In Goossens 2013, there were no incidences of infection in the intervention (normal saline) arm; therefore to calculate the log of the standard error for the rate ratio, as per section 9.4.8 of the Cochrane Handbook for Systematic Reviews of Interventions, we added 0.5 to each arm of the study (Deeks 2011). The resulting calculation in Goossens 2013 was a RR of 0.30 (95% CI 0.01 to 6.26). Because of absent data regarding the first period in the cross‐over study design used in Smith 1991, we did not pool results from this study. We pooled the results of Cesaro 2009 and Goossens 2013. The heterogeneity between studies was I² = 45%. Because the I² statistic approached 50% and there was also evidence of clinical heterogeneity between the studies, (e.g. difference in frequency of flushing, implanted catheters and tunnelled catheters, use of positive pressure cap) we used the random‐effects model. See Analysis 1.2. There is no clear difference between the use of saline to flush CVCs and the incidence of CVC‐associated blood stream infection (RR 1.48, 95% CI 0.24 to 9.37; 2 studies, 231 participants; P = 0.67). We downgraded the certainty of the evidence to low (see Table 1).
1.2. Analysis.

Comparison 1: Normal saline versus heparin flushing, Outcome 2: CVC‐associated blood stream infection rate per 1000 catheter days
Duration of CVC placement (days)
Duration of CVC placement was not reported in Smith 1991, Goossens 2013, and da Silva 2018. Cesaro 2009 reported survival data rather than duration of CVC placement in days. We report the survival data below.
After a median follow‐up of 360 days, Cesaro 2009 reported that CVC survival was similar between the two study arms (203 participants). In the intervention (normal saline) arm mean survival was reported as 77% (95% CI 66% to 84%); and in the control (heparin) arm mean survival was reported as 69% (95% CI 53% to 80%). We downgraded the certainty of evidence to moderate (see Table 1).
Secondary outcomes
Inability to withdraw blood from the CVC
Goossens 2013 reported on the inability to withdraw blood from the CVC (26 participants). Compared to the intervention (normal saline) group, there was a decreased inability to withdraw blood from the CVC in the heparin group (RR 0.32, 95% CI 0.14 to 0.88). Cesaro 2009, Smith 1991 and da Silva 2018 did not report on the inability to withdraw blood from the CVC.
Any use of urokinase or recombinant tissue plasminogen
Urokinase was used in 116 of 124 (94%) episodes of CVC occlusion in the Cesaro 2009 study of 203 patients, and patency was restored in 107 out of 116 (92%). No specific information was available regarding which treatment arm urokinase was used in and the subsequent result; it is noted, however, that 83 CVCs occluded in the normal saline group and 41 in the heparin group. Five of the CVCs were occluded in only one lumen and so were left in situ while the remaining four were unable to have patency restored in either lumen and were prematurely removed. There was no information available regarding the use of urokinase or other drugs to restore patency in Smith 1991, Goossens 2013 and da Silva 2018.
Incidence of removal/re‐insertion of the catheter
Cesaro 2009 reported premature removal of a CVC was required in 44 participants, 22% of the total study population of 203 patients. Premature removal was comparable between the two study arms — 21 in the saline arm and 23 in the heparin arm — and was generally indicated because of dislocation of the catheter or infection, rather than CVC occlusion. There was no information regarding this outcome from Smith 1991, Goossens 2013 and da Silva 2018.
CVC‐related thrombosis
CVC‐related thrombosis was reported in two out of 203 (1%) of the study population in Cesaro 2009 with no differences between study arms (RR 1.00, 95% CI 0.06 to 15.86). In Smith 1991, CVC‐related thrombosis was reported in two out of 14 (14%) of the population; again there was no difference between study arms (RR 1.00, 95% CI 0.06 to 15.86).
Other CVC‐related complications
Dislodgment of the CVC occurred in 38 out of 203 (19%) of the total study population in Cesaro 2009. There were no differences between study arms (RR 0.87, 95% CI 0.46 to 1.63). In Smith 1991, dislodgement occurred in two out of 14 (14%) of the study population. There was no difference between study arms (RR 0.20, 95% CI 0.01 to 4.81). There was no information regarding this outcome available from Goossens 2013 or da Silva 2018.
CVC site infection was reported in 24 out of 203 (12%) in Cesaro 2009 with no differences between study arms (RR 0.68, 95% CI 0.30 to 1.52). In Smith 1991, CVC site infection was reported in six out of 28 (21%) of the study population; again there was no difference between study arms (RR 7.00, 95% CI 0.37 to 132.40).
There were no data available from Goossens 2013 regarding other CVC complications in the paediatric population of 28 patients, or from da Silva 2018.
Subgroup analysis
As there were only four studies included in this review, we were not able to undertake any subgroup analysis.
Sensitivity analysis
Due to the limited number of studies in this review, it was not appropriate to undertake a sensitivity analysis.
Discussion
Summary of main results
This updated systematic review compared the use of 0.9% sodium chloride (normal saline) locks with heparin locks and includes four studies with inconsistent results. The outcomes of interest were: central venous catheter (CVC) occlusion; CVC‐associated blood stream infection; duration in days of catheter placement; inability to withdraw blood from the CVC; use of urokinase or recombinant tissue plasminogen; incidence of removal or re‐insertion of the CVC, or both; thrombosis associated with CVC; other CVC‐related complications such as dislocation of the CVC, other CVC infection, allergic reaction, haemorrhage, heparin‐induced thrombocytopenia, and elevated hepatic enzymes. We calculated rate ratios for outcome measures to estimate the probability of each event occurring in each treatment arm. See Table 1 for details on the primary outcomes 'CVC occlusion', 'CVC‐associated blood stream infection' and 'Duration in days of catheter placement'. The quantity of available evidence was small: for this updated review we found only one small additional study, and it did not change the original conclusions. We found that there is insufficient data to determine the effects of intermittent flushing of normal saline versus heparin to prevent CVC occlusion or CVC‐associated blood stream infection in infants and children. The use of a positive pressure cap in Cesaro 2009 may have biased the results of this study regarding the outcome of CVC‐associated blood stream infection: there is evidence of an association between the use of a positive pressure cap and CVC‐associated blood stream infection in other studies (Jacobs 2004; Jarvis 2009; Marschall 2008). The certainty and strength of the evidence for the use of normal saline instead of heparin for the routine management of CVC is moderate to very low and further well‐designed studies are required.
Overall completeness and applicability of evidence
The trials included in the review directly compared the use of normal saline and heparin in long‐term CVCs in children in community and acute settings, and we were able to undertake two meta‐analyses. All studies included participants representative of those usually found in the clinical setting. Between studies, however, all used different protocols for the intervention and control arms with different concentrations of heparin and different frequencies of flushes reported. Additionally, within studies, Smith 1991 and Cesaro 2009 changed not only the solution being used, but also the frequency of flushes. Any difference seen could therefore be plausibly attributed to either the solution or the frequency of flushes; changing the frequency of flushes may actually confound the results towards the null hypothesis.
The four included studies employed a pragmatic approach to assess the effectiveness of saline in routine care (Cesaro 2009; da Silva 2018; Goossens 2013; Smith 1991). While this approach is desirable to inform policy and routine practice, greater emphasis is required to minimise bias and confounding in the study design to ensure generalisibility. As there are concerns with the internal validity of all studies, the generalisibility (external validity) of results from the studies included in the review is poor.
Quality of the evidence
Study methodology
There was a high level of clinical heterogeneity between all four studies. We summarised the assessment of bias for all studies using Cochrane's 'Risk of bias' tool (Figure 2 and Figure 3) and indicated methodological weaknesses in all studies. Because of the nature of the outcomes (occlusion, infection, duration of catheter days), a lack of blinding may have impacted the outcome assessment. It could be argued that, if the frequency of flushes had been kept consistent between the intervention and control arms, greater care could have been taken to blind the intervention from both participants and clinicians. As clinicians could potentially modify their technique when assessing for occlusion, blinding allocation to the intervention reduces risk. The da Silva 2018 study was the only one to undertake blinding of the intervention. Other concerns across all studies included the potential for selection bias, selective reporting bias, imprecision and possible confounding of results.
Smith 1991 in particular is subject to high levels of uncertainty regarding its precision. This study was undertaken many years ago and is reported with minimal detail. It is unclear how the data were analysed (i.e. paired or un‐paired), or if individual participants experienced more than one outcome. Following this study, the institution where the study was conducted changed its practice, replacing heparin with normal saline locks. Recent communication with this institution confirmed that the facility continues to routinely use normal saline locks for long‐term CVCs in children over 12 months of age, providing strong support for the study's findings (HHSC 2014 [pers comm]). Therefore despite the bias evident in this study, it is important to consider the clinical implications of the experience of the efficacy of normal saline locks in long‐term CVCs over two decades.
In Cesaro 2009, the randomisation process is well reported and the study is methodologically sound. However there are concerns regarding the potential for outcomes to be attributed to the positive pressure cap, or the frequency of flushes (or a combination of both) and so it is unclear what role the flushing solution plays.
Goossens 2013 did not intend for the subset of paediatric data to be analysed separately; their study included a large number of adults and only a small proportion of children (28/802, 3.5%). As a consequence, not all the information required to make an assessment of the quality of the study was available.
da Silva 2018 is a dissertation, undertaken by one investigator, and while the study protocol is reported, the study did not recruit as many participants as was intended, and results are reported with minimal analysis. Ten of the 17 recruited participants were children; we were unable, however, to obtain data about these participants or the number of catheter days. The small number of participants reduced the precision of the study findings.
Heterogeneity, inconsistency and imprecision of results
When we combined two studies to assess the effect of normal saline on CVC occlusion, the statistical heterogeneity was high (Cesaro 2009; Goossens 2013). The combined results of both CVC occlusion and CVC‐associated blood stream infection revealed wide confidence intervals which included the null hypothesis (Analysis 1.1; Analysis 1.2). The studies do not appear to provide consistent information and we were unable to determine the precision of the studies. The small sample sizes and the few events in the two studies are likely the cause of this heterogeneity.
Overall certainty
We assessed the overall certainty of the evidence as very low to low using the GRADE assessment tool; there was a high risk of performance and detection bias in the majority of the studies as well as a high risk of other bias related to differences in frequency of flushes between heparin and saline groups in Cesaro 2009 and Smith 1991. We also assumed a high risk of other bias for the subset of unpublished paediatric data provided for Goossens 2013. In addition we identified heterogeneity, imprecision and inconsistency of the effect estimates (Table 1). Consequently, the results of these meta‐analyses should be interpreted with caution. Further research is likely to improve the confidence in the estimate of these effects if undertaken with greater attention to methodology.
Potential biases in the review process
None of the review authors were investigators in any of the studies included in this review. The literature review was thorough and the methodology transparent and can be reproduced. None of the review authors have any conflicts of interest to declare. While we attempted to minimise bias in this review as described above, we are aware that there are differing practices worldwide and there may be unpublished studies which we did not include in this review. The review authors made assumptions with the paediatric data provided in the Goossens 2013 study that the subset of paediatric patients had the same catheter days at risk as reported in the larger study; these assumptions may have introduced bias in the review process. We originally defined the study population as children and infants aged 1 to 18 years. The included studies had recruited children from age 0 to 20 years: accordingly we changed our study population to include these ages as there were not enough data available to exclude children aged under 1 year in Cesaro 2009 or over 18 years in Smith 1991; we made the assumption this was unlikely to affect the results.
Agreements and disagreements with other studies or reviews
A recent systematic review concurred with our findings that there is insufficient evidence to support the use of normal saline to prevent CVC occlusion (Conway 2014). This review included studies related to the adult population and also peripherally inserted CVCs. Conway 2014 concluded with recommendations for daily flushing with heparin based on the practices of selected facilities. There is insufficient evidence to make this recommendation, however, and it may lead to higher amounts of heparin being used than is necessary, introducing avoidable costs and risks associated with the use of heparin in this patient group. Peripherally inserted CVCs have a much narrower lumen and require different care and thus were excluded from this Cochrane Review.
Evidence is emerging to support the use of ethanol locks in children to prevent blood stream infection associated with tunnelled CVC; a randomised trial of 307 children found ethanol locks were safe and had a 50% statistically significant reduction in infection compared to heparin (Schoot 2015). Ethanol was, however, associated with transient symptoms of nausea, taste alterations, dizziness and blushing.
A RCT in adults was undertaken by Dal Molin 2015 and included 430 participants with totally implanted venous access devices. This large study failed to demonstrate heparin was superior to normal saline and concluded that the use of heparin continues to be controversial. Similarly, in a smaller trial of 30 adults with tunnelled CVCs normal saline was reported to be safe and effective, and using heparin provided no additional benefit (Klein 2018). The updated Cochrane Review for adults, Lopez‐Briz 2018, also found no clear evidence to support the use of heparin to prevent occlusions; while there were fewer occlusions with heparin, the evidence was of very low quality. There was no evidence to suggest heparin was superior to normal saline for CVC‐related sepsis, mortality, haemorrhage, or heparin‐induced thrombocytopenia.
There are numerous observational studies that investigate this issue (Bowers 2008; Brito 2018; Fratino 2005). Many of these studies support the use of normal saline for routine flushing of long‐term CVCs (Abate 2013; Kelly 2008), or found no difference between groups (Brito 2018); and institutions report the practice of using normal saline in their clinical practice guidelines (Nelson 2008).
Despite the literature suggesting that heparin may not be required to maintain patency of CVCs, more RCTs are required to determine the ideal flush solution, concentration, and the frequency of flushes (Baskin 2009). Without strong evidence to support the use of either solution, debate will continue and inconsistencies in practice will prevail. In an area where patients are already vulnerable as a result of their disease state, there should be greater understanding of this relatively simple question and practice should be standardised.
Authors' conclusions
Implications for practice.
There is insufficient evidence to determine the effects of intermittent flushing with normal saline versus heparin to prevent occlusion in long‐term central venous catheters in infants and children. It remains unclear whether heparin is necessary to prevent occlusion, CVC‐associated blood stream infection or the effects of prolonged catheter placement. Lack of agreement remains between institutions around the world regarding the appropriate care and maintenance of these devices.
Implications for research.
Given the results of this review, there is a need for healthcare organisations to consider undertaking further research in this area to contribute to the evidence base. Ultimately this would facilitate the development of evidence‐based clinical practice guidelines and consistency of practice. Careful attention to study design is required, including blinding and proper sample size calculations to detect clinically meaningful differences, and ensuring only one aspect of the intervention is changed in the intervention arm (flushing frequency, concentration of heparin or use of normal saline). Additionally, reporting on variables that may influence outcomes, such as catheter maintenance processes, infection control processes and packaging of flush solutions, would assist with evaluation. Such studies would generate evidence and ensure results could be appraised and generalised to address the current gaps in knowledge. Consistency of outcome reporting would aid interpretation of results. No studies measured the costs associated with the intervention or control arms. If efficacy is similar between both normal saline and heparin, then the use of heparin incurs costs to health systems with no advantages; cost analysis would be a useful addition to future studies. Alternatively, decision models could be used to ascertain what differences in complication rates would make a meaningful difference in costs or outcomes.
What's new
| Date | Event | Description |
|---|---|---|
| 12 September 2019 | New search has been performed | Search updated. One new study included and 12 new studies excluded. One new ongoing study identified. |
| 12 September 2019 | New citation required but conclusions have not changed | Search updated. One new study included and 12 new studies excluded. One new ongoing study identified. Text amended to reflect current Cochrane standards. No change to conclusions. |
History
Protocol first published: Issue 2, 2014 Review first published: Issue 11, 2015
Acknowledgements
We wish to acknowledge the support provided by Cochrane Vascular in developing the search strategy and guidance with developing this protocol and review. We also wish to thank Cochrane for providing accessible training and education for undertaking Cochrane Reviews. In this updated review, we wish to acknowledge Diane Gal and Juliana Martins for their assistance with translating studies from Portuguese to English.
The authors, and the Cochrane Vascular Editorial base, are grateful to the following peer reviewers for their time and comments.
Eduardo López‐Briz PharmD, Department of Pharmacy. University Hospital La Fe, Valencia, Spain
Prof Christoph Male, Department of Paediatrics, Medical University of Vienna, Austria
Ahmed HS Ibrahim, Egypt
Lynne Suprock, USA
Appendices
Appendix 1. Database search strategies
| Source | Search strategy | Hits retrieved |
| CENTRAL | #1 MESH DESCRIPTOR Heparin EXPLODE ALL TREES 4434 #2 (hep* or UH or UFH or LMWH):TI,AB,KY 54652 #3 #1 OR #2 54929 #4 MESH DESCRIPTOR Sodium Chloride 2178 #5 MESH DESCRIPTOR Saline Solution, Hypertonic 474 #6 saline:TI,AB,KY 28913 #7 sodium*:TI,AB,KY 35702 #8 NaCl:TI,AB,KY 2205 #9 #4 OR #5 OR #6 OR #7 OR #8 59497 #10 MESH DESCRIPTOR Catheterization, Central Venous 757 #11 MESH DESCRIPTOR Catheterization 1543 #12 MESH DESCRIPTOR Catheters, Indwelling 963 #13 MESH DESCRIPTOR Vascular Access Devices 89 #14 MESH DESCRIPTOR Central Venous Catheters 100 #15 catheter*:TI,AB,KY 25956 #16 cannula*:TI,AB,KY 4305 #17 (venous near3 access):TI,AB,KY 734 #18 (CVC* or PICC):TI,AB,KY 945 #19 #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 29593 #20 #3 AND #9 AND #19 309 |
162 |
| ClinicalTrials.gov | heparan OR heparin | catheter OR Catheterisation OR catherization OR Vascular Access Device OR cannula | Start date on or after 01/01/2015 | Last update posted on or before 04/09/2019 | 56 |
| ICTRP Search Portal | heparan OR heparin AND Catheter* OR Vascular Access Device* OR cannula* | 11 |
| MEDLINE (Ovid MEDLINE® Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE®) 1946 to present (2017, 2018 and 2019 only) |
1 exp HEPARIN/ 2 (hep* or UH or UFH or LMWH).ti,ab. 3 heparin.ti,ab. 4 alpha‐Heparin.ti,ab. 5 heparan.ti,ab. 6 1 or 2 or 3 or 4 or 5 7 Sodium Chloride/ 8 Saline Solution, Hypertonic/ 9 saline.ti,ab. 10 sodium*.ti,ab. 11 NaCl.ti,ab. 12 7 or 8 or 9 or 10 or 11 13 6 and 12 14 Catheterization, Central Venous/ 15 CATHETERIZATION/ 16 Catheters, Indwelling/ 17 Vascular Access Devices/ 18 Central Venous Catheters/ 19 catheter*.ti,ab. 20 cannula*.ti,ab. 21 (CVC* or PICC).ti,ab. 22 (venous adj3 access).ti,ab. 23 or/14‐22 24 13 and 23 25 randomized controlled trial.pt. 26 controlled clinical trial.pt. 27 randomized.ab. 28 placebo.ab. 29 drug therapy.fs. 30 randomly.ab. 31 trial.ab. 32 groups.ab. 33 or/25‐32 34 exp animals/ not humans.sh. 35 33 not 34 36 24 and 35 |
40 |
| Embase 1974 to present (2017, 2018 and 2019 only) | 1 exp heparin/ 2 (hep* or UH or UFH or LMWH).ti,ab. 3 heparin.ti,ab. 4 heparan.ti,ab. 5 alpha‐Heparin.ti,ab. 6 1 or 2 or 3 or 4 or 5 7 sodium chloride/ 8 saline.ti,ab. 9 sodium*.ti,ab. 10 NaCl.ti,ab. 11 7 or 8 or 9 or 10 12 6 and 11 13 central venous catheterization/ 14 catheterization/ 15 indwelling catheter/ 16 vascular access device/ 17 central venous catheter/ 18 catheter*.ti,ab. 19 cannula*.ti,ab. 20 (CVC* or PICC).ti,ab. 21 (venous adj3 access).ti,ab. 22 or/13‐21 23 12 and 22 24 randomized controlled trial/ 25 controlled clinical trial/ 26 random$.ti,ab. 27 randomization/ 28 intermethod comparison/ 29 placebo.ti,ab. 30 (compare or compared or comparison).ti. 31 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 32 (open adj label).ti,ab. 33 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 34 double blind procedure/ 35 parallel group$1.ti,ab. 36 (crossover or cross over).ti,ab. 37 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 38 (assigned or allocated).ti,ab. 39 (controlled adj7 (study or design or trial)).ti,ab. 40 (volunteer or volunteers).ti,ab. 41 trial.ti. 42 or/24‐41 43 23 and 42 |
141 |
| CINAHL (2017, 2018 and 2019 only) | S39 S23 AND S38 S38 S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 S37 MH "Random Assignment" S36 MH "Triple‐Blind Studies" S35 MH "Double‐Blind Studies" S34 MH "Single‐Blind Studies" S33 MH "Crossover Design" S32 MH "Factorial Design" S31 MH "Placebos" S30 MH "Clinical Trials" S29 TX "multi‐centre study" OR "multi‐center study" OR "multicentre study" OR "multicenter study" OR "multi‐site study" S28 TX crossover OR "cross‐over" S27 AB placebo* S26 TX random* S25 TX trial* S24 TX "latin square" S23 S13 AND S22 S22 S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 S21 TX venous n3 access S20 TX CVC* or PICC S19 TX cannula* S18 TX catheter* S17 (MH "Central Venous Catheters") S16 (MH "Vascular Access Devices") S15 (MH "Catheterization") S14 (MH "Catheterization, Central Venous") S13 S6 AND S12 S12 S7 OR S8 OR S9 OR S10 S11 TX NaCl S10 TX sodium* S9 TX saline S8 (MH "Saline Solution, Hypertonic") S7 (MH "Sodium Chloride") S6 S1 OR S2 OR S3 OR S4 OR S5 S5 TX heparan S4 TX alpha‐Heparin S3 TX heparin S2 TX hep* or UH or UFH or LMWH S1 (MH "Heparin+") |
10 |
| AMED (Allied and Complementary Medicine) 1985 to July (2017, 2018 and 2019 only) | 1 exp HEPARIN/ 2 (hep* or UH or UFH or LMWH).ti,ab. 3 heparin.ti,ab. 4 alpha‐Heparin.ti,ab. 5 heparan.ti,ab. 6 1 or 2 or 3 or 4 or 5 7 Sodium Chloride/ 8 Saline Solution, Hypertonic/ 9 saline.ti,ab. 10 sodium*.ti,ab. 11 NaCl.ti,ab. 12 7 or 8 or 9 or 10 or 11 13 6 and 12 14 CATHETERIZATION/ 15 catheter*.ti,ab. 16 cannula*.ti,ab. 17 (CVC* or PICC).ti,ab. 18 (venous adj3 access).b,ab. 19 14 or 15 or 16 or 17 or 18 20 13 and 19 |
0 |
Data and analyses
Comparison 1. Normal saline versus heparin flushing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 CVC occlusion rate per 1000 catheter days | 2 | 229 | Rate Ratio (IV, Random, 95% CI) | 0.75 [0.10, 5.51] |
| 1.2 CVC‐associated blood stream infection rate per 1000 catheter days | 2 | 231 | Rate Ratio (IV, Random, 95% CI) | 1.48 [0.24, 9.37] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cesaro 2009.
| Study characteristics | ||
| Methods |
Study design: prospective parallel RCT, at a single tertiary referral centre, during a 25‐month study period Method of randomisation: computer generated Allocation concealment: sealed envelopes |
|
| Participants |
Country: Italy Setting: single tertiary referral centre Numbers: 203 paediatric haematology or oncology patients with tunnelled Broviac CVC. 101 participants randomised to intervention arm and 102 participants randomised to control arm Age: 0 to 17 years; age < 5 years = 39, age > 5 years = 62 in intervention arm; age < 5 years = 41, age > 5 years = 61 in control arm Gender: 60 male, 41 female in intervention arm; 60 male, 42 female in control arm Catheter days at risk: total of 75,249 catheter days. Mean of 381 days per person (range 11 to 1072) in the intervention arm; 351 days per person (range 4 to 1073) in the control arm Inclusion criteria: paediatric patient (0 to 17 years of age, with malignant or non‐malignant haematologic or oncologic disease with a Broviac‐Hickman‐type CVC i.e. tunnelled, partially inserted, open‐ended, inserted for the purpose of chemotherapy of haematopoietic stem cell transplantation Exclusion criteria: not stated |
|
| Interventions |
Intervention arm: flushing with normal saline at least weekly via a positive pressure cap Control arm: flushing with 3 mL of normal saline with 200 units heparin twice weekly via a standard CVC cap |
|
| Outcomes |
|
|
| Notes | Potential confounding of results due to outcomes being attributable to positive pressure cap or frequency between flushes rather than the flushing solution used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer generated randomisation lists were drawn up by a statistician not involved in patient management" |
| Allocation concealment (selection bias) | Low risk | Quote: "Stored by sequentially numbered sealed envelopes. Permuted blocks of four were used for treatment allocation. Information concealed to investigators until completion of recruitment" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no blinding of participants or personnel. Different caps were used in the different arms of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: due to nature of interventions, not possible to blind assessment of outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: low attrition rate; follow‐up for median of 360 days; results from all enrolled participants were reported |
| Selective reporting (reporting bias) | Unclear risk | Comment: all nominated outcome data were reported. No study protocol available |
| Other bias | High risk | Comment: outcomes could also be attributed to different caps, or frequency of flushing, not only to use of different solutions |
da Silva 2018.
| Study characteristics | ||
| Methods |
Study design: prospective parallel RCT, at a single tertiary referral centre, during a 180‐day study period Method of randomisation: computer generated in blocks of 6, 3 each to the control and intervention arm Allocation concealment: sequentially numbered, placed in opaque envelopes located in a separate area |
|
| Participants |
Country: Brazil Setting: public teaching hospital with a Bone Marrow Transplant service Numbers: 17 individuals with an oncology or haematology condition, who had a Hickman® CVC inserted. Of participants aged under 18 years, 5 were randomised to the intervention arm, and 5 to the control arm. No further details are available for the paediatric subset of data. Age: 10 (71.4%) individuals were aged under 18 years, and 7 (28.6%) aged over 18 years. We were not able to obtain further data from the investigator for participants aged under 18 years. Gender: 3 (30%) female in the intervention arm, 2 (28.6%) female in the control arms. Further details not available for paediatric subset. Catheter days at risk: no information was available for catheter days at risk Inclusion criteria: being hospitalised in the research unit; have a Hickman® CVC inserted; first hospitalisation for stem cell transplantation Exclusion criteria: patients on anti‐coagulant therapy by any route of administration; on fibrinolytic therapy; allergy to heparin components; bleeding during the period of data collection; refractory to platelet transfusion; previous hospitalisation in the research unit |
|
| Interventions |
Intervention arm: daily pulsatile flushing with normal saline and then locking with positive pressure Control arm: daily pulsatile flushing with normal saline and then heparin (50 units/mL), locking with positive pressure |
|
| Outcomes |
|
|
| Notes | No data were available for the paediatric subset only. Not all variables available; there may be some systematic differences in the characteristics of children in the subset of data; the study was not powered to analyse this subset of data separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A list was created on a computer to randomly allocate intervention or control solutions. These were coded and kept in sealed, opaque envelopes. Randomisation was undertaken in blocks of 6: 3 intervention and 3 controls at a time. The sequence was generated at random by a computer program by a person outside of the research team. These were placed in sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Triple‐blinded sealed envelopes contained coded groups, so investigators, nursing staff and participants did not know which group they belonged to |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Researchers, nursing staff and participants were blinded to which group had the intervention or control |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Nursing staff were blinded to which group participants were allocated to when assessing CVCs for occlusion |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low numbers of patients lost to follow‐up from both groups, therefore a low risk of bias resulting from difference in outcomes due to incomplete follow‐up |
| Selective reporting (reporting bias) | Low risk | Reported on the main outcome of occlusion |
| Other bias | High risk | Due to resources available, a convenience sample of consecutive patients that were eligible to participate were recruited. Small numbers reduce precision of findings |
Goossens 2013.
| Study characteristics | ||
| Methods |
Study design: prospective parallel RCT, at a single tertiary referral centre, during a 23‐month study period Method of randomisation: computer generated Allocation of concealment: sequentially numbered cards located in a separate area |
|
| Participants |
Country: Belgium Setting: single tertiary referral centre Numbers: 802 individuals with an oncology or haematology condition, who had a totally implantable intravenous catheter inserted. A subset of unpublished data was obtained from the investigators for 28 (3.5%) participants, aged 1 to 18 years; 11 participants were randomised to intervention arm and 17 were randomised to control arm. No further details available for paediatric subset of data Age: 1 to 71 years, mean age 57.9 years (SD 14.8) in the intervention arm; mean age 54.9 years (SD 16.6) in the control arm. Further details not available for paediatric subset Gender: 261 (64.6%) female in the intervention arm, 263 (66.1%) female in the control arm. Further details not available paediatric subset Catheter days at risk: total catheter days 115,991: 58,197 in the intervention arm (mean 152.4 days per patient); 57,794 in the control arm (mean 150.9 days per patient). We assumed that the mean catheter days was equivalent in the paediatric population Inclusion criteria: patients older than 1 year, scheduled for insertion of a totally implantable CVC for the first time, with a haematology or oncology condition and expected to survive for the planned follow‐up of 180 days Exclusion criteria: patients (or caregivers in the case of children) unable to provide informed consent, unable to stand for a post‐operative chest X‐ray, patients with therapeutic intravenous heparin administration, a history of HIT or abnormal clotting tests, or coincident participation in other clinical trials |
|
| Interventions |
Intervention arm: pulsatile flushing with 10 mL of normal saline and then locking with positive pressure Control arm: pulsatile flushing with 10 mL of normal saline, followed by 3 mL heparin (100 units/mL) and locking with positive pressure |
|
| Outcomes |
|
|
| Notes | Subset of paediatric data (unpublished) was obtained to assess outcomes for children only: 26 out of 28 children contributed data. Not all variables available, there may be some systematic differences in the characteristics of children in the subset of data, the study was not powered to analyse this subset of data separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We randomly assigned patients in a 1:1 ratio using computerised random numbers to two groups" |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence was concealed from researchers who enrolled patients according to sequentially numbered patient cards stored in a separate room." Patients were assigned to groups after providing consent to participate |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no blinding of participants or personnel |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: due to nature of interventions, it was not possible to blind the assessment of outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: attrition occurred with adult participants; however analysis was based on CVC access rate rather than individual patient data. Unsure if paediatric data was complete |
| Selective reporting (reporting bias) | Unclear risk | Comment: all nominated outcome data were reported. No study protocol available |
| Other bias | High risk | Comment: subset of paediatric data was unpublished, provided by the study author; there may be systematic differences of participant characteristics in this subset of data |
Smith 1991.
| Study characteristics | ||
| Methods |
Study design: prospective cross‐over RCT, at a single tertiary referral centre, during a 7‐month study period Method of randomisation: no information available Allocation of concealment: no information available |
|
| Participants |
Country: Canada Setting: single tertiary referral centre Numbers: 14 participants with tunnelled Broviac CVC Age: 21 months to 20 years of age (median 5.4). As a cross‐over design, the same participants were in both the intervention and the control arms Gender: no information available Mean duration of catheter days at risk: total catheter days 3029: 1515 catheter days (mean 108 days per person) in the intervention arm and 1514 (mean 108 days per person) in the control arm Inclusion criteria: none stated. All patients had CVCs placed prior to entering study Exclusion criteria: none stated |
|
| Interventions |
Intervention arm: once per week flush with 9 mL normal saline Control arm: twice daily flushes with 5 mL heparinised normal saline (10 units/mL heparin) |
|
| Outcomes |
|
|
| Notes | Older study, not reported using contemporary standards. Potential for confounding of results due to outcomes being attributable to frequency between flushes rather than solution used. No information available for first cross‐over period results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk |
Comment: no information provided regarding sequence generation for randomisation; cross‐over design but no information regarding how participants were selected Quote: "patients were randomised to one of two methods of catheter care and then crossed over at the end of a three and a half month period to the opposite arm for an additional three and a half month period" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided regarding allocation concealment; however as a cross‐over design all participants were their own controls |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no blinding of participants or personnel |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: due to nature of intervention, not possible to blind assessment of outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no attrition in study; results from all enrolled participants reported |
| Selective reporting (reporting bias) | High risk | Comment: all nominated outcome data reported in basic format; no results from statistical tests reported. It is not clear if paired analysis was undertaken. No study protocol available |
| Other bias | High risk | Comment: unable to establish if authors considered carry‐over effect of the interventions from 1 arm to the other; possible selection bias. Outcomes could also be attributed to alterations between the frequency of flushes |
CVC: central venous catheter HIT: heparin‐induced thrombocytopenia RCT: randomised controlled study SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Arauj 2011 | Wrong population group: PICC catheter |
| Arnts 2011 | Wrong population: peripheral cannula |
| Brito 2018 | Wrong study type: retrospective study |
| De Neef 2002 | Type of catheter not relevant |
| Geritz 1992 | Type of catheter not relevant |
| Heidari Gorji 2015 | Wrong population: adults |
| Kaneko 2004 | Population not relevant: adults aged over 18 years |
| Klein 2017 | Wrong population: adults |
| Klein 2018 | Wrong population: adults |
| NCT00001518 | Wrong population: adults |
| NCT01343680 | Study terminated due to poor patient accrual (total of 2 participants enrolled) |
| NCT02354118 | Wrong population: adults |
| NCT02923830 | Wrong population: adults |
| Pumarola 2007 | Type of catheter not relevant |
| Rabe 2002 | Type of catheter not relevant and population aged over 18 years |
| Reichardt 2002 | Wrong population: adults |
| Schallom 2012 | Wrong population: adults |
| Schultz 2002 | Type of catheter not relevant |
PICC: peripherally inserted central catheter
Differences between protocol and review
The duration of catheter placement was changed from "number of weeks" in the protocol, to "number of days" in the review as per the reported outcomes in the included studies' reported outcomes.
A secondary outcome measure of dislocation of CVCs was included in the review as it was deemed an important clinical variable.
We originally planned to use odds ratios or risk ratios in the published protocol; however outcome measures were not reported consistently in studies. As all included studies reported the number of catheter days for each study population, we were able to calculate rate ratios as a common metric to compare and report outcomes.
We originally defined the study population as children and infants aged 1 to 18 years. The included studies had recruited children from age 0 to 20 years; accordingly we changed our study population to include these ages as there was not enough data available to exclude children aged under one year in Cesaro 2009 or over 18 years in Smith 1991; we made the assumption this was unlikely to affect the results.
We have included a 'Summary of findings' table and GRADE assessment of the evidence according to current Cochrane guidelines.
Contributions of authors
All authors contributed to the design and development of the Cochrane Review protocol and review, and participated in the review update.
NB: contributed to study selection, appraisal, data extraction, data analysis and the writing of the review RE: contributed to study selection and appraisal, and editing drafts of the review RC: contributed to study appraisal, data extraction, data analysis and editing drafts of the review
Sources of support
Internal sources
-
Children's Health Queensland Hospital and Health Service, Australia
Royal Children's Hospital provided salary and facilities for RE to conduct this systematic review
-
Queensland University of Technology, Australia
Queensland University of Technology provided salary and facilities to support NB and RC to undertake this systematic review
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK
The Cochrane Vascular editorial base is supported by the Chief Scientist Office
Declarations of interest
NB: none known RE: none known RC: none known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Cesaro 2009 {published data only}
- Cesaro S, Tridello G, Cavaliere M, Magagna L, Gavin P, Cusinato R, et al. Prospective, randomized trial of two different modalities of flushing central venous catheters in pediatric patients with cancer. Journal of Clinical Oncology 2009;27(12):2059-65. [DOI] [PubMed] [Google Scholar]
da Silva 2018 {published data only (unpublished sought but not used)}
- da Silva RS. Effect of heparin to prevent obstruction of the Hickman catheter [Efetividade da solucao de heparina na prevencao de oclusao do cateter de kickman: ensaio clinico randomizado]. [Thesis dissertation] acervodigital.ufpr.br/handle/1884/56046 2018 (accessed 13 September 2019).
Goossens 2013 {published and unpublished data}
- Goosens GA, Jerome M, Janssens C, Peetermans WE, Fieuws S, Moons P, et al. Comparing normal saline versus diluted heparin to lock non-valved totally implantable venous access devices in cancer patients: a randomised, non-inferiority, open trial. Annals of Oncology 2013;24(7):1892-9. [DOI] [PubMed] [Google Scholar]
- Goossens GA, Jerome M, Janssens C, Peetermans WE, Fieuws S, Moons P, et al. Heparin versus normal saline as locking solution in totally implantable venous ports: A randomized controlled trial in cancer patients. Supportive Care in Cancer 2013;21:S28. [Google Scholar]
Smith 1991 {published data only (unpublished sought but not used)}
- Smith S, Dawson S, Hennessey R, Andrew M. Maintenance of the patency of indwelling central venous catheters: is heparin necessary? American Journal of Pediatric Hematology/oncology 1991;13(2):141-3. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Arauj 2011 {published data only}
- Araujo O, Araujo M, Silva J, Barros M, . Intermittent heparin is not effective at preventing the occlusion of peripherally inserted central venous catheters in preterm and term neonates. Revista Brasileira de Terapia Intensiva 2011;23(3):335-40. [PubMed] [Google Scholar]
Arnts 2011 {published data only}
- Arnts IJ, Heijnen JA, Wilbers HT, Wilt GJ, Groenewoud JM, Liem KD, . Effectiveness of heparin solution versus normal saline in maintaining patency of intravenous locks in neonates: a double blind randomized controlled study. Journal of Advanced Nursing 2011;67(12):2677-85. [DOI] [PubMed] [Google Scholar]
Brito 2018 {published data only}
- Brito ARO, Nishinari K, Saad PF, Saad KR, Pereira MAT, Emidio SCD, et al. Comparison between saline solution containing heparin versus saline solution in the lock of totally implantable catheters. Annals of Vascular Surgery 2018;47:85-9. [DOI] [PubMed] [Google Scholar]
De Neef 2002 {published data only}
- De Neef M, Heijboer H, Van Woensel JB, De Haan RJ. The efficacy of heparinization in prolonging patency of arterial and central venous catheters in children: a randomized double-blind trial. Pediatric Hematology and Oncology 2002;19(8):553-60. [DOI] [PubMed] [Google Scholar]
Geritz 1992 {published data only}
- Geritz MA. Saline versus heparin in intermittent infuser patency maintenance. Western Journal of Nursing Research 1992;14(2):131-7. [DOI] [PubMed] [Google Scholar]
Heidari Gorji 2015 {published data only}
- Heidari Gorji MA, Rezaei F, Jafari H, Yazdani Cherati J. Comparison of the effects of heparin and 0.9% sodium chloride solutions in maintenance of patency of central venous catheters. Anesthesiology and Pain Medicine 2015;5(2):e22595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaneko 2004 {published data only}
- Kaneko Y, Iwano M, Yoshida H, Kosuge M, Ito S, Narita I, et al. Natural saline-flush is sufficient to maintain patency of immobilized-urokinase double-lumen catheter used to provide temporary blood access for hemodialysis. Blood Purification 2004;22(5):473-9. [DOI] [PubMed] [Google Scholar]
Klein 2017 {published data only}
- Klein J, Patterson A, Jepsen A, Badgero K, Moore M, Warrell WA, Thornton K. Effectiveness of heparin versus saline flushing for managing central venous catheters (CVCs) in the blood and marrow transplant (BMT) patients: a pilot study. Biology of Blood and Marrow Transplantation 2017;23(3):S386. [Google Scholar]
Klein 2018 {published data only}
- Klein J, Jepsen A, Patterson A, Reich RR, Mason TM. Heparin versus normal saline: flushing effectiveness in managing central venous catheters in patients undergoing blood and marrow transplantation. Clinical Journal of Oncology Nursing 2018;22(2):1-5. [DOI] [PubMed] [Google Scholar]
NCT00001518 {published data only}
- NCT00001518. A randomized evaluation of the effect of routine normal saline flush versus heparinized saline solution in Groshong and Groshong PICC catheters. clinicaltrials.gov/ct2/show/NCT00001518 (first posted December 10 2002).
NCT01343680 {unpublished data only}
- NCT01343680. Trial of two central venous catheter (CVC) flushing schemes in pediatric hematology and oncology patients. https://clinicaltrials.gov/show/NCT01343680 (first posted 28 April 2011).
NCT02354118 {published data only}
- NCT02354118. Maintaining patency in implanted port catheters. https://clinicaltrials.gov/ct2/show/NCT02354118 (first posted 3 February 2015).
NCT02923830 {published data only}
- NCT02923830. Maintaining patency in BioFlo implanted port catheters with saline only flushes. https://clinicaltrials.gov/ct2/show/NCT02923830 (first posted 5 October 2016).
Pumarola 2007 {published data only}
- Pumarola C, Casademont Mercader R, Colomer Plana M, Cordon Bueno C, Sabench Casellas S, Felez Vidal M, et al. Comparative study of maintenance of patency of triple lumen central venous catheter [Estudio comparativo del mantenimiento de la permeabilidad de los cateteres venosos centrales de tres luces]. Enfermeria Intensiva 2007;18(1):25-35. [DOI] [PubMed] [Google Scholar]
Rabe 2002 {published data only}
- Rabe C, Gramann T, Sons X, Berna M, Gonzalez-Carmona MA, Klehr HU, et al. Keeping central venous lines open: a prospective comparison of heparin, vitamin C and sodium chloride sealing solutions in medical patients. Intensive Care Medicine 2002;28(8):1172-6. [DOI] [PubMed] [Google Scholar]
Reichardt 2002 {published data only}
- Reichardt P, Kretzschmar A, Biakhov M, Irwin D, Slabber C, Miller L, et al. A phase III randomized, double-blind, placebo-controlled study evaluating the efficacy and safety of daily low-molecular-weight heparin (dalteparin sodium, fragmin) in preventing catheter-related complications (CRCs) in cancer patients with central venous catheters (CVCs). Journal of Clinical Oncology 2002;21:1474. [Google Scholar]
Schallom 2012 {published data only}
- Schallom ME, Prentice D, Sona C, Micek ST, Skrupky LP. Heparin or 0.9% sodium chloride to maintain central venous catheter patency: a randomized trial. Critical Care Medicine 2012;40(6):1820-26. [DOI] [PubMed] [Google Scholar]
Schultz 2002 {published data only}
- Schultz AA, Drew D, Hewitt H. Comparison of normal saline and heparinized saline for patency of IV locks in neonates. Applied Nursing Research 2002;15(1):28-34. [DOI] [PubMed] [Google Scholar]
Additional references
Abate 2013
- Abate ME, Escobosa-Sanchez O, Boschi R, Raspanti C, Loro L, Affinito D, et al. Analysis of risk factors for central venous catheters related complications: a prospective observational study in pediatric patients with bone sarcomas. Cancer Nursing 2013;37(4):292-8. [DOI] [PubMed] [Google Scholar]
Athale 2012
- Athale UH, Siciliano S, Cheng J, Thabane L, Chan AK. Central venous line dysfunction is an independent predictor of poor survival in children with cancer. Journal of Pediatric Hematology/oncology 2012;34(3):188-93. [DOI] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al, GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barclay 2012
- Barclay CA, Vonderhaar KJ, Clark EA. The development of evidence-based care recommendations to improve the safe use of anticoagulants in children. Journal of Pediatric Pharmacology and Therapeutics 2012;17(2):155-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baskin 2009
- Baskin JL, Pui C-H, Reiss U, Wilimas JA, Metzger ML, Ribeiro RC, et al. Management of occlusion and thrombosis associated with long-term indwelling central venous catheters. Lancet 2009;374(9684):159-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bertoglio 2012
- Bertoglio S, Solari N, Meszaros P, Vassallo F, Bonvento M, Pastorino S, et al. Efficacy of normal saline versus heparinized saline solution for locking catheters of totally implantable long-term central vascular access devices in adult cancer patients. Cancer Nursing 2012;35(4):E35-42. [DOI] [PubMed] [Google Scholar]
Bowers 2008
- Bowers L, Gabel Speroni K, Jones L, Atherton M. Comparison of occlusion rates by flushing solutions for peripherally inserted central venous catheters with positive pressure Luer-activated devices. Journal of Infusion Nursing 2008;31(1):22-7. [DOI] [PubMed] [Google Scholar]
Conway 2014
- Conway MA, McCollom C, Bannon C. Central venous catheter flushing recommendations: a systematic evidenced-based practice review. Journal of Pediatric Oncology Nursing 2014;31(4):185-90. [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation Covidence. Version accessed 10 April 2019. Melbourne, Australia: Veritas Health Innovation.Available at covidence.org.
Dal Molin 2015
- Dal Molin A, Clerico M, Baccini M, Guerretta L, Sartorello B, Rasero L. Normal saline versus heparin solution to lock totally implanted venous access devices: results from a multicentred randomized trial. European Journal of Oncology Nursing 2015;19(6):638-43. [DOI] [PubMed] [Google Scholar]
Davis 2013
- Davis MB. Pediatric central venous catheter management: a review of current practice. Journal of the Association for Vascular Access 2013;18(2):93-8. [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG editor(s). Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S editor(s).Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fratino 2005
- Fratino G, Molinari AC, Parodi S, Longo S, Saracco P, Castagnola E, et al. Central venous catheter-related complications in children with oncological/hematological diseases: an observational study of 418 devices. Annals of Oncology 2005;16(4):648-54. [DOI] [PubMed] [Google Scholar]
Gonzalez 2012
- Gonzalez G, Davidoff AM, Howard SC, Pui CH, Rao BN, Shenep JL, et al. Safety of central venous catheter placement at diagnosis of acute lymphoblastic leukemia in children. Pediatric Blood & Cancer 2012;58(4):498-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 13 September 2019. Hamilton (ON): McMaster University (developed by Evidence Prime).Available at www.gradepro.org.
HHSC 2014 [pers comm]
- Education Department McMaster Children's Hospital. Protocol for CVC maintenance [personal communication]. Email to: HHS-education@HHSC.CA 29 May 2014.
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Altman DG, Sterne JAC editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jacobs 2004
- Jacobs BR, Schilling S, Doellman D, Hutchinson N, Rickey M, Nelson S. Central venous catheter occlusion: a prospective controlled trial examining the impact of a positive pressure valve device. Journal of Parenteral and Enteral Nutrition 2004;28(2):113-8. [DOI] [PubMed] [Google Scholar]
Jarvis 2009
- Jarvis WR, Murphy C, Hall KK, Fogle PJ, Karchmer TB, Harrington G, et al. Health care-associated bloodstream infections associated with negative- or positive-pressure or displacement mechanical valve needleless connectors. Clinical Infectious Diseases 2009;49(12):1821-7. [DOI] [PubMed] [Google Scholar]
Kelly 2008
- Kelly L. The care of vascular access devices in community care. British Journal of Community Nursing 2008;13(5):198-205. [DOI] [PubMed] [Google Scholar]
Lee 2005
- Lee OK, Johnston L. A systematic review for effective management of central venous catheters and catheter sites in acute care paediatric patients. Worldviews on Evidence-based Nursing / Sigma Theta Tau International, Honor Society of Nursing 2005;2(1):4-13, discussion 14-5. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. Available from handbook.cochrane.org 2011.
Lopez‐Briz 2018
- Lopez-Briz E, Ruiz Garcia V, Cabelle JB, Bort-Marti S, Carbonell Sanchis R, Burls A. Heparin versus 0.9% sodium chloride locking for prevention of occlusion in central venous catheters in adults. Cochrane Database of Systematic Reviews 2018, Issue 7. [DOI: 10.1002/14651858.CD008462.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marschall 2008
- Marschall J, Mermel LA, Classen D, Arias KM, Podgorny K, Anderson D, et al. Strategies to prevent central-line associated infections in acute care hospitals. Strategies 2008;29(S1):S22-S30. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tezlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 2009;151(4):264-9. [DOI] [PubMed] [Google Scholar]
Monagle 2010
- Monagle P, Ignjatovic V, Savoia H. Hemostasis in neonates and children: pitfalls and dilemmas. Blood Reviews 2010;24(2):63-8. [DOI] [PubMed] [Google Scholar]
Nelson 2008
- Nelson S, Armes S, Austin A, Clark N, Hicks G, Johnston J, et al. Care and maintenance to reduce vascular access complications. Registered Nurse's Association of Ontario International Affairs and Best Practice Guidelines Programs Guidelines Supplement 2008:1-7.
Revel‐Vilk 2010
- Revel-Vilk S, Yacobovich J, Tamary H, Goldstein G, Nemet S, Weintraub M, et al. Risk factors for central venous catheter thrombotic complications in children and adolescents with cancer. Cancer 2010;116(17):4197-205. [DOI] [PubMed] [Google Scholar]
RevMan Web 2019 [Computer program]
- The Cochrane Collaboration Review Manager Web (RevMan Web). The Cochrane Collaboration, 2019.Available at: revman.cochrane.org.
Schoot 2015
- Schoot RA, Ommen CH, Stijnen T, Tissing WJE, Michiels E, Abbink FCH, et al. Prevention of central venous catheter-associated bloodstream infections in paediatric oncology patients using 70% ethanol locks: a randomised controlled multi-centre trial. European Journal of Cancer 2015;51(14):2031-8. [DOI] [PubMed] [Google Scholar]
Schuster 2000
- Schuster M, Nave H, Piepenbrock S, Pabst R, Panning B. The carina as a landmark in central venous catheter placement. British Journal of Anaesthesia 2000;85(2):192-4. [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JP, Green S editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Shah 2007
- Shah PS, Kalyn A, Satodia P, Dunn MS, Parvez B, Daneman A, et al. A randomized, controlled trial of heparin versus placebo infusion to prolong the usability of peripherally placed percutaneous central venous catheters (PCVCs) in neonates: the HIP (Heparin Infusion for PCVC) study. Pediatrics 2007;119(1):e284-e91. [DOI] [PubMed] [Google Scholar]
Shanks 2005
- Shanks RM, Donegan NP, Graber ML, Buckingham SE, Zegans ME, Cheung AL, et al. Heparin stimulates Staphylococcus aureus biofilm formation. Infection and Immunity 2005;73(8):4596-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D editor(s). Chapter 10: Addressing reporting biases. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Intervention. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Stocco 2012
- Stocco JGD, Crozeta K, Taminato M, Reichembach-Danski MT, Meier MJ. Evaluation of the mortality of neonates and children related to the use of central venous catheters: a systematic review. Acta Paulista de Enfermagem 2012;25(1):90-5. [Google Scholar]
Wong 2012
- Wong T, Clifford V, McCallum Z, Shalley H, Peterkin M, Paxton G, et al. Central venous catheter thrombosis associated with 70% ethanol locks in pediatric intestinal failure patients on home parenteral nutrition. A case series. Journal of Parenteral and Enteral Nutrition 2012;36(3):358-60. [DOI] [PubMed] [Google Scholar]
Young 2008
- Young G. New anticoagulants in children. ASH Education Program Book 2008;1:245-50. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bradford 2014
- Bradford NK, Edwards RM, Chan RJ. Heparin versus 0.9% sodium chloride intermittent flushing for the prevention of occlusion in long term central venous catheters in infants and children. Cochrane Database of Systematic Reviews 2014, Issue 2. [DOI: 10.1002/14651858.CD010996] [DOI] [PubMed] [Google Scholar]
Bradford 2015
- Bradford NK, Edwards RM, Chan RJ. Heparin versus 0.9% sodium chloride intermittent flushing for the prevention of occlusion in long term central venous catheters in infants and children. Cochrane Database of Systematic Reviews 2015, Issue 11. [DOI: 10.1002/14651858.CD010996.pub2] [DOI] [PubMed] [Google Scholar]


