Abstract
Background
In the novel coronavirus disease 2019 (COVID-19) pandemic, social distancing has been necessary to help prevent disease transmission. As a result, medical practices have limited access to in-person visits. This poses a challenge to maintain appropriate patient care while preventing a substantial backlog of patients once stay-at-home restrictions are lifted. In practices that are naïve to telehealth as an alternative option, providers and staff are experiencing challenges with telemedicine implementation. We aim to provide a comprehensive guide on how to rapidly integrate telemedicine into practice during a pandemic.
Methods
We built a toolkit that details the following 8 essential components to successful implementation of a telemedicine platform: provider and staff training, patient education, an existing electronic medical record system, patient and provider investment in hardware, billing and coding integration, information technology support, audiovisual platforms, and patient and caregiver participation.
Results
Rapid integration of telemedicine in our practice was required to be compliant with our institution’s COVID-19 task force. Within 3 days of this declaration, our large specialty-care clinic converted to a telemedicine platform and we completed 638 visits within the first month of implementation.
Conclusions
Effective and efficient integration of a telemedicine program requires extensive staff and patient education, accessory platforms to facilitate video and audio communication, and adoption of new billing codes that are outlined in this toolkit.
Telemedicine was previously touted as an opportunity to expand healthcare access to rural1 , 2 and underserved populations,3 but has urgently been adopted as a safer means of providing medical care during the novel coronavirus disease 2019 (COVID-19) pandemic.4 The Centers for Medicare and Medicaid Services rapidly facilitated this change through the 1135 Waiver, allowing clinicians to provide telemedicine services in broader circumstances.4 , 5
In addition to reducing the potential risk of infectious disease transmission, telemedicine visits have achieved similar health outcomes compared with in-person patient visits in several primary care studies,6 and have ancillary benefits of reducing travel costs and time away from work.7 Subspecialists across multiple disciplines have also used telemedicine to increase access for patients seen in rural clinics. This has been associated with high levels of satisfaction among both patients and their primary care physicians.7 In a study from the Department of Veterans Affairs, patients seeking care in the Greater Los Angeles area rated their satisfaction as “very good” to “excellent” in 95% of cases.8 On average, patients saved 277 miles driven, $67 in travel-related expenses, and $126 in missed opportunity costs per telemedicine appointment.8 This approach affords potential benefits to the environment and the economic well-being of patients, many of whom might have reduced earning potential in the wake of a pandemic. Medical specialties have recognized the growing need and potential of telemedicine for use in the outpatient setting, telesurgery, and telerounding. Although some specialties have initiated telehealth visits successfully,10, 11, 12, 13, 14, 8, 9 the issue of reimbursement has been noted to be the major barrier to implementation for many.15 Amidst the COVID-19 pandemic, however, facilitating healthcare access in a safe setting became a priority as cities promoted social distancing. Telemedicine regulatory restrictions have been eased in the US in an effort to promote safety for patients, their family members, and healthcare professionals, and to avoid healthcare service delays that might compromise future health. As a result, many practices are now finding themselves forced to acclimate to the sudden and broad implementation of telemedicine platforms, and the learning process can frustrate patients, providers, support staff, and the healthcare system.
In this article, we offer an implementation guide to share the resources that have allowed us to rapidly integrate telemedicine across all of our divisions in an academic specialty practice through the use of Epic electronic medical record (EMR) system, the MyChart (powered by Epic) application, and video-calling services, such as FaceTime (Apple Inc); Google Duo (Google LLC), Doximity, and Skype (Microsoft). It can serve as an effective resource for staff and provider training.
Telehealth Program Implementation
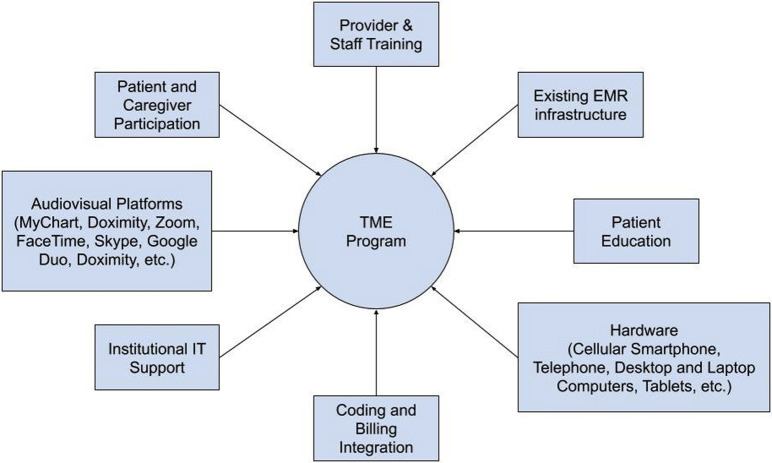
The following 8 elements are necessary for telemedicine integration: an existing EMR system infrastructure, audiovisual platforms, institutional information technology support, provider and patient investment in hardware, provider and staff training, patient education, patient and caregiver participation, and coding/billing integration (Fig. 1 ).
Figure 1.
Elements of a telemedicine (TME) program. EMR, electronic medical record; IT, information technology.
Existing electronic medical record infrastructure
At our institution, the Epic EMR platform has been in use since 2012. Epic is used in more than 250 healthcare organizations in the US, and 45% of the population has at least some of their medical records in an Epic system.16 Epic is particularly dominant in larger hospitals and health organizations, and in 2018 had a 28% market share of the 5,447 acute care hospitals in the US.17 MyChart is a Health Insurance Portability and Accountability Act (HIPAA)-protected patient access portal that is included in Epic. It allows patients to access their charts to view medical records, laboratory, and imaging results, share their records with other providers, update their conditions, schedule appointments, and message providers.18 Patients can access this portal with their personal Apple or Android devices, tablets, desktop, or laptop computer, and is free of charge. Having access to this portal is essential for both e-visits and video visits to be properly conducted. If this or a similar portal is not available, however, alternative audiovisual platforms can be used to meet the requirements for a video telemedicine visit.
Alternative audiovisual platforms
As HIPAA violation penalties against healthcare workers have been waived temporarily, widely available video-calling services, such as FaceTime, Skype, Doximity, WhatsApp, and Google Duo are alternative options.19 If an institution has not integrated audiovisual capabilities into the existing EMR system, these platforms are attractive options for conducting telemedicine visits. If MyChart video visit capability is incorporated into your Epic EMR system, the commercially available videoconferencing software should be used as a last resort. Initiation of video calls using these platforms from personal devices, however, might disclose personal numbers and addresses. Doximity, an online networking service for medical professionals, has a feature (Doximity Dialer) that permits substitution of whatever telephone number is needed, such as the provider’s general clinic, to appear on the recipient’s device (https://www.doximity.com/download/general?c=web_mast_logged_out&pid=internal_marketing). A new video feature was recently added to their application. It is free for Doximity users and enables communication between Apple and Android devices. Through this application, a text message is sent to any smartphone device and contains a video link that permits easy video connectivity. In our experience, this is the easiest way to connect with patients outside of approved portals and is especially useful if patients are enrolled in programs, such as MyChart, so they can receive printed after-visit instructions.
Institutional information technology support
System overload is a common problem when using HIPAA-protected EMR services, such as MyChart. It is necessary to have information technology support to ensure adequate bandwidth and a secure connection to allow for proper operation of this system.
Provider and patient investment in hardware
Beginning a telehealth practice requires some investment in hardware. Most offices are equipped with desktop computers, laptops, and smartphones. For telehealth visits, older computers might need external webcams or speakers. In the US, 81% of the adult population own a smartphone and 13% own a mobile phone without smartphone capabilities.20 Approximately 89% of US households have computers.21 With such widespread accessibility, we have found that a large majority of our patients already have access to the necessary hardware.
Provider and staff training
In our experience, it takes at least 1 hour of in-person provider and staff training to learn how to implement telehealth visits. We created educational handouts and then conducted a group trial run of a mock telemedicine encounter. This was very helpful to demonstrate the myriad of potential obstacles and solutions to video visits through the patient portal. Although telemedicine is currently built as a physician platform, we included our front desk and nursing staff within our telemedicine model to mimic a standard in-person encounter. For the first week, we limited the scheduling of all telemedicine visits to 30 minutes for both new and return patient visits. Once familiarity and competence was demonstrated, providers could then choose to increase their templates to accommodate a larger number of patients per day.
Patient education and participation
Patient education is a resource-intensive yet critical component of telemedicine success, especially if HIPAA-approved systems such as MyChart are used. There is an initial investment of office staff time to effectively present the option of a telemedicine visit and then coach the patient through the necessary software for the first encounter. The patients are also advised of the potential advantages of the telemedicine visit, such as not postponing their healthcare needs while staying safely at home, having the ability to save travel and waiting times, and avoiding the expenses associated with transportation and parking. The nursing staff calls patients approximately 1 week ahead of their appointment to confirm their preferred method of audiovisual connection. Depending on the device, our staff will send instructions on how to download the necessary applications and access MyChart.com (see eDocument 1). Fifteen minutes before the telemedicine appointment time, a member of our nursing staff calls the patient to confirm connectivity and then completes a review of patient history, medications, and allergies. This information is entered into the chart exactly as during an in-person encounter. The provider is then fully equipped to initiate an efficient telemedicine visit at the scheduled appointment time.
Eligibility, coding, and billing integration
Telehealth implementation requires a comprehensive understanding of eligibility, terminology, and billing. Eligibility and documentation requirements differ for telemedicine visits according to their classification, and familiarity is essential for compliance with coding and billing. Virtual services include telehealth visits, virtual check-ins, and e-visits. The list below describes the visit type, eligibility requirements, and billing codes. These are organized from lowest to highest time and complexity and correlate to the revenue value unit potential (Table 1 ).
-
1.
E-visits are secure, digital evaluation and management (E/M) services that patients initiate through an EMR. The patient must be established, enrolled, and active in the patient portal and have had an appointment in the past 1 year. These visits are not permitted to relay test results or schedule appointments. Billing is according to cumulative time accrued during a 7-day period: 99421 (5 to 10 minutes); 99422 (11 to 20 minutes); and 99423 (more than 21 minutes).
-
2.
G2010: This is a remote evaluation of recorded video and/or images submitted by an established patient that includes interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days or leading to an E/M service or procedure within the next 24 hours or soonest available appointment.
-
3.
G2012: Virtual check-in is a brief (minimum of 5 minutes) established patient telephone check-in with a physician or advanced practice provider to decide whether an office visit or other service is needed. For example, a patient calls with complaints of an acute urinary tract infection. The provider empirically sends treatment to pharmacy and verbally advises the patient to schedule an appointment if symptoms do not respond in 48 hours. The origin for the virtual check-in visit cannot be from a E/M service within the previous 7 days, and cannot lead to an E/M service or procedure within the next 24 hours or soonest available appointment, and this has to be documented for each virtual check-in encounter. Additional documentation requirements include consent for the visit, confirmation of patient identity and established patient status, details of encounter to establish medical necessity, and total amount of time. One can only submit G2012 if a minimum of 5 minutes of direct communication was achieved.
-
4.
Clinician phone visits are scheduled telephone-based encounters between patient and provider not originating from a related E/M service provided within the previous 7 days or leading to an E/M service or procedure within the next 24 hours or soonest available appointment, and are billed according to time spent in direct physician-to-patient telephone contact (Table 1). A very recent change permitted new and established patients to use this telehealth option and it is not necessary to be enrolled in the patient portal. For example, a patient requests a clinician phone appointment to discuss recurrent urinary tract infection symptoms. The provider calls to obtain the history, reviews the medical history and earlier culture results, and makes a decision about treatment. The total time documented was 15 minutes. After appropriate documentation of consent and all of the other elements detailed above, a 99442 code could be entered.
-
5.
Telemedicine visits (also called “video visits”) allow clinicians and patients to interact through the necessary elements of both live interactive audio and video to avoid the need for an in-person appointment. This encounter can be used for both new and established patients as well as consults. Billing code selection is based on the same criteria and documentation requirements as for in-person encounters. Non-HIPAA-compliant communications platforms are allowed during the COVID-19 pandemic as long as they are not public facing, such as Facebook.
Table 1.
Classification of Virtual Services
| Virtual service, patient type, visit length | Billing code | Relative value unit |
|---|---|---|
| e-Visit, established | ||
| 5–10 min | 99421 | 0 |
| 11–20 min | 99422 | 0 |
| > 21 min | 99423 | 0 |
| Remote evaluation of image/video, established | ||
| NA | G2010 | 0.18 |
| Virtual check-in, established | ||
| 5 min | G2012 | 0.25 |
| Phone visit, new or established | ||
| 5–10 min | 99441 | 0.25 |
| 11–20 min | 99442 | 0.5 |
| 21–30 min | 99443 | 0.75 |
| Telehealth (video) | ||
| New | ||
| 10 min | 99201 | 0.48 |
| 20 min | 99202 | 0.93 |
| 30 min | 99203 | 1.42 |
| 45 min | 99204 | 2.43 |
| 60 min | 99205 | 3.17 |
| Established | ||
| 5 min | 99211 | 0.18 |
| 10 min | 99212 | 0.48 |
| 15 min | 99213 | 0.97 |
| 25 min | 99214 | 1.5 |
| 45 min | 99215 | 2.11 |
NA, not applicable.
Consent is required before initiation of all telehealth visits and documentation is required within each note. The US government has also waived the requirement of a patient co-payment during the COVID pandemic. Telehealth (video) visits can be billed by time or complexity. We recommend setting up an easily insertable smartphrase (eDocument 2) that will document the mode of communication used as well as time spent. A modifier 95 is applied for telehealth visits. Some payers might have considerations for GT and GQ modifiers as well.
New and established patient office visits can be reported with the same in-person billing codes regardless of location as long as the visit is conducted using live audio and visual connection. Billing is entered according to face-to-face time or, for established patients, the same elements that are used for in-person encounters (see eTable 1).
Nonphysician staff telehealth encounters
Any nonphysician healthcare professional (physical and occupational therapists, speech pathologists, clinical psychologists) might interact with established patients through a patient portal or through secure, encrypted email as directed using the codes outlined in Table 2 .4
Table 2.
Classification and Billing Codes for Nurse Telehealth Visits
| Visit type | Code |
|---|---|
| Review of video or image, with interpretation and report | G2010 |
| e-Visit | G2012 |
| Nursing or staff online assessment of an established patient for up to 7 d, cumulative time 5–10 min | G2061 |
| Nursing or staff online assessment of an established patient for up to 7 d, cumulative time 11–20 min | G2062 |
| Nursing or staff online assessment of an established patient for up to 7 d, cumulative time 21 min or more | G2063 |
Discussion
This toolkit facilitated provider and staff training and resulted in rapid implementation of a successful telemedicine program across all divisions within our subspecialty program during the course of 3 days. Within 1 month, we successfully completed 638 telemedicine visits, which permitted continuation of outpatient services with minimal requirements for appointment cancellation. Access to healthcare services was preserved with the ability to discriminate more accurately which patients required an in-person visit. In addition, involvement of our nursing and office staff within the telemedicine visit structure was instrumental in maintaining 75% of employment hours for our staff. As staff members interface with patients on the telephone to convert in-person visits to telemedicine, they served as important ambassadors for programmatic success.
Although this rapid change has disrupted our normal workflow considerably, it has generally been very well received by patients and office staff. We are currently in the process of objectively determining patient-specific barriers to telemedicine appointments, as well as patient satisfaction using a validated telemedicine survey questionnaire.22 Our anecdotal experience is that patients who are older and less educated require significantly more nursing or office staff instruction on how to connect via telemedicine, and the recruitment of a younger family member can be very helpful. Flexibility in video connection options has been paramount, although the majority have been able to successfully connect via a simple link sent through the Doximity video application function. Review of our Press Ganey scores have remained consistently high during this time, especially with regard to patient satisfaction with ease of scheduling appointments, concern of nursing staff toward the patient’s problem, satisfaction with his or her provider, and likelihood of recommending our practice to others. We attribute this success in large part to having a comprehensive toolkit that eased the transition for our staff.
In addition, our providers have expressed satisfaction with telemedicine, as it has allowed us to continue to serve patients with nonemergent health symptomes and plan future operations. For many surgical sub-specialties, a comprehensive history and review of referral records and available diagnostic data, including imaging, are enough to be able to schedule an operation while delaying physical examination to a preoperative visit. For example, an audit of new patients seen by a provider in female pelvic health (CAM) demonstrated a 20% to 25% conversion rate of new telemedicine visits to incontinence and pelvic organ prolapse operations posted within the next 3 months.
A valid concern that patients, physicians, and the healthcare systems might have when using commercially available videoconferencing software is cybersecurity, which could compromise sensitive patient information. During this pandemic, we have seen this issue with the popular service, Zoom, which became the victim of hacking, interrupting educational sessions.23 Although these services are convenient, we recommend they be used as a last resort. We advocate for the use of a secure patient portal, such as MyChart, to conduct telemedicine visits that will be less vulnerable to cyber attacks, and sensitive patient information will be stored on a secure server.
With telemedicine projected to be a $48.8 billion industry by 2023,24 many startup companies are developing platforms to gain market share by promoting convenience and cost savings from the comforts of their own home compared with an in-person visit.25 Especially with men’s and women's health, these companies are linking patients with on-demand telehealth physicians (usually family and internal medicine physicians and gynecologists), and prescribing medication, such as erectile dysfunction medication, testosterone replacement, contraception, and male pattern baldness treatment, through their online pharmacies. With no state or federal oversight of these prescription drug companies, they are not required to comply with the same standards as drug distributors.25 In addition, with only a brief intake questionnaire, no physical examination, and very little, if any, follow-up, critical assessments of associated conditions and potentially dangerous side effects (eg cardiovascular disease associated with erectile dysfunction and polycythemia as a side effect of testosterone replacement) can compromise patient care.25 By instituting telemedicine into brick-and-mortar practices, patients can receive appropriate care and follow-up, and develop a relationship with a qualified provider, especially during a pandemic.
Conclusions
Rapid adoption of telemedicine ensures access to, and continuity of, patient care while limiting unnecessary exposure to infectious illnesses, such as COVID-19. This toolkit provides the necessary guide for provider and patient education to successfully implement a telehealth program and comply with billing documentation and coding requirements. As this is mostly unchartered territory for most practices, this practical guide should facilitate an easier transition to a telemedicine program.
Author Contributions
Study conception and design: Smith, Terlecki, Kelly, Matthews
Acquisition of data: Smith, Atala, Terlecki, Kelly, Matthews
Analysis and interpretation of data: Smith, Terlecki, Matthews
Drafting of manuscript: Smith, Terlecki, Matthews
Critical revision: Terlecki, Kelly, Matthews
Footnotes
Disclosure Information: Nothing to disclose.
Disclosures outside the scope of this work: Dr Matthews receives fees for expert testimony fromJohnson & Johnson, and Dr Matthews and Dr Terlecki’s institution receives grant funding from Neomedic,Boston Scientific, and theDepartment of Defense.
eDocument 1. Smartphrase Documentation
Today’s visit was completed via a real-time telehealth (see specific modality noted below). A telehealth visit was used in order to decrease the patient's potential exposure to COVID-19 vs an in-person visit. The patient/authorized person provided oral consent at the time of the visit to engaging in a telemedicine encounter with the present provider at [hospital or clinic name]. The patient/authorized person was informed of the potential benefits, limitations, and risks of telemedicine. The patient/authorized person expressed understanding that the laws that protect confidentiality also apply to telemedicine. The patient/authorized person acknowledged understanding that telemedicine does not provide emergency services and that he or she would need to call 9-1-1 or proceed to the nearest hospital for help if such a need arose.
Total time spent in the clinical discussion ∗∗∗ minutes.
Telehealth Modality: {Modality: # (39305 = Audio; 39306 = Audio and Visual)
Application Download and Mychart Access Instructions
Please NOTE: If you are using a mobile device, you must download the ExtendedCare Virtual Care Room mobile app BEFORE starting your virtual visit.
Begin these steps at least 30 minutes before your scheduled appointment time.
From mobile phone/tablet:
-
1.
Ensure mobile device is connected to WiFi. Cellular data is not recommended.
-
2.
Open the App Store or Google Play Store.
-
3.
Download the "ExtendedCare Virtual Care Room" app (Telehealth Video Solution by STA Group, LLC)
-
4.
Open/Download "MyChart" app by Epic. If this is your first time using the MyChart app, select "Wake Forest Baptist Health" as your healthcare provider.
-
5.
In the MyChart app, click on the Appointments icon.
-
6.
Select the appropriate appointment.
-
7.
Click "Begin Visit." The ExtendedCare Virtual Care Room app will launch.
eTable 1.
Elements Needed for Visit CPT CodeVisit type, CPT code History
Examination MDM Total encounter time, min HPI ROS FSH Outpatient consultation∗ 99241 1 NA NA 1 OS SF 15 99242 1 1 NA 2–7 OS SF 30 99243 4 2 1 D Low 40 99244 4 10+ 3 8 OS Moderate 60 99245 4 10+ 3 8 OS High 80 New patient visit∗ 99201 1 NA NA 1 OS SF 10 99202 1 1 NA 2–7 OS SF 20 99203 4 2 1 D Low 30 99204 4 10+ 3 8 OS Moderate 45 99205 4 10+ 3 8 OS High 60 Established patient visit† 99211 NA NA NA NA NA 5 99212 1 NA NA 1 OS SF 10 99213 1 1 NA 2–7 OS Low 15 99214 4 2 1 D Moderate 25 99215 4 10+ 2 of 3 8 OS High 40 D, detailed examination (requires at least 2 findings for at least 2 organ systems/body areas); FSH, family and social history; HPI, history of present illness; MDM, medical decision making; NA, not applicable; OS, organ system; ROS, review of systems; SF, straightforward.∗Must address 3 of 3 history/examination/MDM.†Must address 2 of 3 history/examination/MDM.
References
- 1.Nesbitt T.S., Marcin J.P., Daschbach M.M. Perceptions of local health care quality in 7 rural communities with telemedicine. J Rural Health. 2005;21 doi: 10.1111/j.1748-0361.2005.tb00066.x. [DOI] [PubMed] [Google Scholar]
- 2.Davis A.M., Sampilo M., Gallagher K.S. Treating rural paediatric obesity through telemedicine vs. telephone: outcomes from a cluster randomized controlled trial. J Telemed Telecare. 2016;22:86–95. doi: 10.1177/1357633X15586642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Atabaki S., Hatcliffe R., Ledda M. Improving access to pediatric sub-specialty care using DTC telemedicine by addressing barriers. GW Research Days. https://hsrc.himmelfarb.gwu.edu/gw_research_days/2018/SMHS/13 Available at:
- 4.Centers for Medicare and Medicaid Services Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Available at:
- 5.Centers for Medicare and Medicaid Services telehealth benefits in Medicare are a lifeline for patients during coronavirus outbreak. https://www.cms.gov/newsroom/press-releases/telehealth-benefits-medicare-are-lifeline-patients-during-coronavirus-outbreak Available at:
- 6.Flodgren G., Rachas A., Farmer A.J. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;Sep 7;(9):CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nesbitt T.S., Hilty D.M., Kuenneth C.A. Development of a telemedicine program: a review of 1,000 videoconferencing consultations. West J Med. 2000;173:169–174. doi: 10.1136/ewjm.173.3.169-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu S., Boxer R., Madison P. Veterans Affairs telemedicine: bringing urologic care to remote clinics. Urology. 2015;86:255–260. doi: 10.1016/j.urology.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 9.Glassman D.T., Puri A.K., Weingarten S. Initial experience with telemedicine at a single institution. Urol Pract. 2018;5:367–371. doi: 10.1016/j.urpr.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Thelen-Perry S., Ved R., Ellimoottil C. Evaluating the patient experience with urological video visits at an academic medical center. Mhealth. 2018;4:54. doi: 10.21037/mhealth.2018.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cremades M., Ferret G., Parés D. Telemedicine to follow patients in a general surgery department. A randomized controlled trial. Am J Surg. 2020 doi: 10.1016/j.amjsurg.2020.03.023. 2020 Mar 26 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Haimi M., Brammli-Greenberg S., Baron-Epel O. Assessing patient safety in a pediatric telemedicine setting: a multi-methods study. BMC Med Inform Decis Mak. 2020;20:63. doi: 10.1186/s12911-020-1074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sohn G.K., Wong D.J., Yu S.S. A review of the use of telemedicine in dermatologic surgery. Dermatol Surg. 2020;46:501–507. doi: 10.1097/DSS.0000000000002230. [DOI] [PubMed] [Google Scholar]
- 14.Wang R.F., Trinidad J., Lawrence J. Improved patient access and outcomes with the integration of an eConsult program (teledermatology) within a large academic medical center. J Am Acad Dermatol. 2019 October 31 doi: 10.1016/j.jaad.2019.10.053. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Badalato G.M., Kaag M., Lee R. Role of telemedicine in urology: contemporary practice patterns and future directions. Urol Pract. 2020;7:122–126. doi: 10.1097/UPJ.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 16.Day J.A. Why Epic. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/epic/why_epic/ Available at:
- 17.HealthLeaders In EMR Market Share Wars, Epic and Cerner Triumph Yet Again. https://www.healthleadersmedia.com/innovation/emr-market-share-wars-epic-and-cerner-triumph-yet-again Available at:
- 18.MyChart What you can do with MyChart. https://www.mychart.com/Features Available at:
- 19.US Department of Health and Human Services HIPAA, Civil Rights, and COVID-19. https://www.hhs.gov/hipaa/for-professionals/special-topics/hipaa-covid19/index.html?language=es Available at:
- 20.Silver L. Smartphone ownership is growing rapidly around the world, but not always equally. Pew Research Center. Global Attitudes and Trends. https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/ Available at:
- 21.US Census Bureau Computer and internet use in the United States: 2016. https://www.census.gov/library/publications/2018/acs/acs-39.html Available at:
- 22.Parmanto B., Lewis A.N., Jr., Graham K.M. Development of the Telehealth Usability Questionnaire (TUQ) Int J Telerehabil. 2016;8:3–10. doi: 10.5195/ijt.2016.6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hakim D., Singer N. New York Attorney General looks into Zoom’s privacy practices. https://www.nytimes.com/2020/03/30/technology/new-york-attorney-general-zoom-privacy.html Available at:
- 24.Telemedicine Market to Generate Revenue Worth $48.8 Billion by 2023. https://www.psmarketresearch.com/press-release/global-telemedicine-market Available at: Published June 2018. Accessed April 7, 2020.
- 25.Houman J.J., Eleswarapu S.V., Mills J.N. Current and future trends in men’s health clinics. Transl Androl Urol. 2020;9:S116. doi: 10.21037/tau.2019.08.33. [DOI] [PMC free article] [PubMed] [Google Scholar]