ABSTRACT
The Asia–Pacific region is home to a large heterogeneous population whose respiratory health is influenced by diverse social, economic and environmental factors. Despite this variability, the most prevalent causes of respiratory morbidity and mortality are tobacco smoking, infection, and air pollution. This review aims to summarize current respiratory health issues in the region including smoking‐related diseases especially COPD, lung cancer and infectious problems such as pandemic influenza, the severe acute respiratory syndrome coronavirus, bacterial pneumonia and tuberculosis, as well as the contribution of air pollution to respiratory disease. Published data on trends in the epidemiology and management of respiratory diseases and are summarized; finally, the limitations of available data and projections for the future of respiratory health in the region are discussed.
Keywords: air pollution, Asia–Pacific, environmental and occupational health and epidemiology, tobacco, tuberculosis, viral infection
Author's Note:
In this review, the Asia–Pacific Region is defined as the countries and areas belonging to the Western Pacific Region of the World Health Organisation, plus Taiwan and Thailand.
This review was written on the basis of World Health Organisation data and a literature review using PubMed and Google Scholar and the search terms ‘respiratory’, ‘Asia–Pacific’, ‘Asia’, ‘Pacific’ concentrating on original publications and reviews from the last decade (since 2000). The references in papers of interest were also mined for studies that were not produced by the original search.
OVERVIEW
Respiratory diseases pose significant challenges to health systems worldwide and are major contributors to whole population morbidity and mortality. In the Asia–Pacific region there are a number of special considerations related to particular population characteristics. Infection (including tuberculosis (TB)) and tobacco smoking are the major causes of respiratory disease and death. Pandemic illnesses such as influenza and the severe acute respiratory syndrome (SARS) coronavirus bear special relevance to Asia as recent outbreaks have been traced to areas within the region, which has implications for disease control worldwide. Diseases resulting from air pollution and occupational exposures are of increasing importance as a result of the increasing industrialization of previously under‐developed economies in this region.
In this, and subsequent issues of 2011, Respirology has commissioned a series of review articles focusing on particular aspects of respiratory health in the Asia–Pacific region. This article provides an overview on the key features of respiratory problems in the region, and will serve as a platform for the Asia–Pacific respiratory health review series.
The Asia–Pacific region (here defined as the WHO ‘Western Pacific’ plus Taiwan and Thailand) accounted for 1.7 billion of the world's population in 2004 1 (see Table 1). This includes the large, economically ascendant Chinese population, a number of smaller low to middle income countries (see Table 1) and several relatively developed nations of which the largest are Japan, Australia and New Zealand. The Asia–Pacific therefore comprises a heterogeneous group of populations whose respiratory health and health in general are influenced by diverse factors including economic wealth, population density and urbanization, climate, air pollution and industrialization, tobacco smoking, occupational exposures to toxic substances, and the availability and affordability of medical treatment. Within the region there are also a number of indigenous populations whose particular health problems are often difficult to address at a population level due to a paucity of data. 2 In general, indigenous health is particularly adversely affected by relative poverty, overcrowding and environmental contamination with the movement from traditional societies to urban environments, high prevalence of infection and smoking, and inadequate access to health care. 2 In discussing the Asia–Pacific region as a whole, many of these issues that also affect the general population will be addressed. The particular effects on localized and disadvantaged groups, while important, are beyond the scope of this review.
Table 1.
Countries of the Asia–Pacific region
| High‐income countries | Australia, Brunei Darussalam, Japan, New Zealand, Republic of Korea, Singapore |
| Low to middle income countries | Cambodia, China, Cook Islands, Fiji, Kiribati, Lao People's Democratic Republic, Malaysia, Marshall Islands, Micronesia, Mongolia, Nauru, Niue, Palau, Papua New Guinea, the Philippines, Samoa, Solomon Islands, Taiwan, Thailand, Tonga, Tuvalu, Vanuatu, Vietnam |
MORTALITY
There were an estimated 12 million deaths in the Asia–Pacific region in 2004, of which approximately one quarter (2.8 million) were attributable to respiratory causes 1 , 3 (see Table 2). Together, COPD and lung cancer accounted for 70% of all deaths attributable to respiratory disease in this region in 2004. Infections comprised the other major cause of death, with pneumonia (475 000, 16.8%) and TB (305 000 deaths, 10.8% of respiratory deaths) the major contributors 3 (please refer also to the recent TB review series in Respirology).
Table 2.
Causes of respiratory mortality
| n | % of Asia–Pacific respiratory † | % of Asia–Pacific all cause ‡ | |
|---|---|---|---|
| Tuberculosis | 305 000 | 10.8% | 2.5% |
| Respiratory infections | 475 000 | 16.8% | 3.9% |
| COPD | 1 508 000 | 52.2% | 12.4% |
| Asthma | 48 000 | 1.7% | 0.4% |
| Lung cancer | 495 000 | 17.5% | 4.1% |
| Total respiratory (Asia–Pacific) | 2 832 000 | 98% | 23.2% |
| Total deaths Asia–Pacific (all cause) | 12 191 000 | ||
| Total deaths Worldwide (all cause) | 57 772 000 |
Adapted from: WHO Global Burden 2004 Update. 1
Percentage contribution of each disease to total mortality in the Asia–Pacific from respiratory causes.
Percentage contribution of each disease to total mortality in the Asia–Pacific region from all causes.
INFECTIOUS/COMMUNICABLE DISEASES
Influenza and viral pandemics
Respiratory viral illnesses such as influenza A and the SARS coronavirus have become important global health problems in recent years, attracting significant attention from both the media and disease control agencies. With the increasing ease of international travel, an outbreak of a highly pathogenic virus in one country or region can rapidly become a worldwide health problem, raising the importance of preparedness in both source countries and distant nations. 4 In some subtropical areas in Asia, influenza is endemic, producing a perennial pool of infectious patients rather than the seasonal peaks observed in temperate regions. 5
In the recent past there have been outbreaks of Influenza A H5N1 (‘avian flu’) 4 and H1N1 (‘swine flu’) 6 as well as a novel coronavirus causing the illness known as SARS. 7 Influenza A H5N1 was first isolated in birds in Hong Kong in 1997 and the few reported human cases had an extremely high mortality (6 deaths from 18 cases), which were all related to the handling of live or recently killed birds; 6 later, the worldwide spread resulted in significant human illness and efforts to prevent further spread among both animals and humans. Novel Influenza A H1N1 originated in pigs in Mexico in 2009 but as of early 2010 has spread to humans worldwide including in South East Asia. 8 The SARS coronavirus was first isolated in Guangdong province in China and produced a small (in absolute terms), short‐lived pandemic in early 2003 with approximately 8000 reported cases yet with a high case‐mortality of 9.6%. 9
Further viral pandemics are inevitable, and the population of the Asia–Pacific region will inevitably be involved, whether or not the region is the source of initial spread. Urban overcrowding, poverty and close contact with infected animals including birds undoubtedly predispose to outbreaks, and these factors are present in many areas of East and South‐East Asia. 6 , 10 , 11 The Asia–Pacific region is therefore a potential source of the next pandemic, and international cooperation within the region will be needed to prevent and control highly pathogenic viruses. Although the high‐income countries, e.g. Australia, are able to access additional resources in the event of a pandemic, 12 whether they have dealt with the recent H1N1 outbreak effectively continues to be debated. 13 Low‐ and middle‐income countries are less well equipped despite the likelihood that they would be at the epicentre of an outbreak. 6 , 10
Pandemic preparedness
Efforts at preparation for influenza outbreaks face a number of difficulties; fundamentally, this is because past outbreaks are imperfect models for future outbreaks. A number of factors contribute to this difficulty including antigenic drift (i.e. different strains), variable disease severity, levels of population immunity to different strains, the capacity of hospitals and other health‐care facilities, supply of vaccines and antiviral medications, and the efficacy of both vaccines and medications.
In the Asia–Pacific region as elsewhere, there are four main approaches to the prevention and control of influenza outbreaks: (i) social measures to reduce transmission via person‐to‐person contact in the general population; (ii) isolation and treatment of proven or suspected cases; (iii) vaccination; and (iv) antiviral medications. 4 , 10 , 14 , 15 National and international plans use each of these approaches to varying degrees. Developing countries tend to use social measures where health system capacity and economic factors limit the availability of other approaches. The use of vaccination and antiviral medications may be widespread or confined to at‐risk groups; given the costs and logistics involved, recent research efforts have been directed at determining an optimal strategy for the use of these agents, although this may vary from country to country and from outbreak to outbreak. 15
Neuraminidase inhibitors have attracted attention as potential antiviral agents to control influenza; however, there is renewed scrutiny 16 of the effectiveness and indications for the use of these medications, especially as stockpiling of these agents imposes significant financial costs. At present there is insufficient evidence to support a role for neuraminidase inhibitors in the prevention of serious complications of influenza although there is some evidence that they shorten the duration of illness. 17
Influenza vaccination
Vaccination either before an outbreak or at its inception remains a powerful method of preventing the spread of influenza and associated morbidity and mortality; 18 , 19 safe and effective vaccines now exist for all prevalent influenza A subtypes, including H5N1. 20 However, there are multiple complexities surrounding the use of influenza vaccines apart from safety and efficacy. At the level of the virus, the rapid evolution of viral antigens requires that new vaccines be developed annually and that countries use an appropriate vaccine for current viral strains 21 although there is a degree of cross‐reactivity. 22 At the human and national levels, new viral subtypes combined with logistic delays in the hasty production of new vaccines may create difficulties in their use in the control of a new outbreak. 15 In addition, there are problems of supply, cost and availability which necessitate the use of vaccines primarily for at‐risk groups only (i.e. children, the elderly, those with comorbidities and health professionals), a strategy that has been validated by modelling in Asia. 18 , 19 Finally, concerns about vaccine side‐effects (real or perceived) can limit the uptake of vaccines even when they are widely available. 23
The control of influenza is a complex issue of particular public health concern in the Asia–Pacific region. A large body of evidence exists to inform public policy, although the interpretation and implementation of this evidence are expected to vary from country to country.
Tuberculosis
The Asia–Pacific region accounts for about one‐fifth of worldwide TB incidence. 1 , 24 , 25 Rates of TB within the region vary widely (Fig. 2): from 10 per 100 000 population in low‐prevalence countries like Australia to over 500 per 100 000 in high‐prevalence countries like Cambodia. 24 With its large population, China accounts for approximately two‐thirds of reported cases within the region. 24 In developed countries with an aging population, most cases occur in older adults and the elderly, whose comorbidities or frailty may result in a higher case fatality rate (see the recent review by Schaaf et al. which also discusses TB in infants 26 ). For example, in Japan, over 60% of reported TB cases are in those aged over 65 years, whereas in China over 80% occur in those aged less than 65 years and in Papua New Guinea (whose overall rate is high at 250 per 100 000), over 80% occur in those under 45 years. 24
Figure 2.
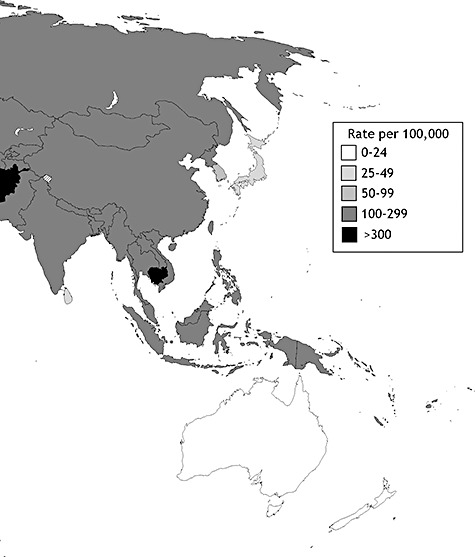
TB incidence rates (all forms) per 98 000 (Asia–Pacific and surrounding countries). Adapted from Anderson et al. and WHO data (WHO. Global tuberculosis control—surveillance, planning, financing. [online]http://www.who.int/tb/publications/global_report/2004/en/
In developed nations, a sharp decline in rates of the disease during the 20th century has produced a degree of complacency among health professionals and the public. In the developing world, TB is a major health concern. Its importance is made all the more pressing by the emergence of multi‐drug‐resistant (MDR) and extensively drug‐resistant (XDR) strains, as well as co‐infection with the HIV, all of which carry significant risk of death and make the management of TB infection more challenging than ever before.
(1)
[ Countries of the Asia–Pacific region. ]
Around 1% of TB patients in the Asia–Pacific region are co‐infected with HIV. The rate of HIV/TB co‐infection is highest in rural Cambodia (in some regions up to 38% of TB patients are HIV positive 27 ), southern Vietnam (up to 9.3% 28 ), and Papua New Guinea 29 (9.7% 28 ). Infection with HIV predisposes to the activation of latent TB, and active TB in HIV‐seropositive patients carries a high risk of death. 28 The specific management challenges of this combination of infections are beyond the scope of this review (please refer to the recent TB review series in Respirology), but it clearly requires efforts both at international and at individual patient levels to combat its spread. Onozaki and Raviglione have summarized the current goals and strategies pertaining to the region in a recent issue of this journal. 30
Drug resistance in Mycobacterium tuberculosis is a significant problem in the Asia–Pacific region and has been discussed in detail by Chiang et al. in a recent review. 31 MDR TB is defined as in vitro resistance to at least isoniazid and rifampicin, while XDR TB is resistant to these agents as well as fluoroquinolones and injectable second‐line drugs. 28 Areas of China, Vietnam, Thailand, Korea and the Philippines are noted to have high rates of MDR and XDR TB. 32 Previous unsupervised ineffective treatment is the strongest predictor of drug resistance, 25 while poverty and HIV co‐infection also increase the risk. 33
In the last two decades, short‐course directly observed therapy (DOTS) has become the standard of care in the Asia–Pacific region and worldwide. 25 , 28 This strategy requires significant investment in health‐care networks, laboratories, drug availability and affordability, sufficient record keeping and analysis, as well as a sustained political commitment underwriting the continuity of the service. DOTS has been shown to be associated with improved patient compliance and treatment outcomes in resource‐poor areas. 34
The recent TB review series in Respirology discussed many relevant topics in detail, including the relationship between chronic TB and airflow limitation, 35 treatment of latent TB, 35 recent advances in the immunology 36 and chemotherapy 37 of TB, genetic susceptibility to TB, 38 and advances in TB diagnosis. 39
Tuberculosis vaccination
Vaccination against TB with the Mycobacterium bovis bacillus Calmette‐Guerin (BCG) is the most widely used vaccine in the world, and remains an important disease prevention measure in infants in endemic regions of the Asia–Pacific region. 40 , 41 The vaccine has been shown to be highly effective and cost‐effective in reducing severe childhood TB, especially military TB and tuberculous meningitis 42 and provides a degree of cross‐protection for other mycobacteria, other bacteria and some protozoal infections; 40 it is less effective in preventing adult pulmonary TB. 41 , 43 Expansion of neonatal vaccination programmes is expected to decrease TB incidence by up to 50% by 2050 44 and considerable research efforts are being directed towards improved vaccines, especially for possible use in adults, although none is yet in the advanced testing phase. 40 , 44
Pneumonia
Community‐ and hospital‐acquired pneumonias are important causes of morbidity and mortality worldwide. Apart from the variable incidence of TB, which may present as community‐acquired pneumonia, 45 , 46 or as a pleural effusion (see the recent review by Professor Light 47 ), and the pandemic viral causes—both of which have been discussed above—the aetiology of pneumonia in the Asia–Pacific region varies little from country to country. One exotic pathogen, Burkholderia pseudomallei, is endemic in rural South‐East Asia and in northern Australia, and is an important consideration in patients with pneumonia from these areas. 45 Nevertheless, the most important aspects of the treatment of pneumonia in all countries are accurate diagnosis, knowledge of local antibiotic resistance patterns and appropriate antibiotic therapy.
Streptococcus pneumoniae is the major cause of community‐acquired pneumonia, and recent studies have shown a high prevalence of antibiotic resistance to first‐line agents in this organism in Asia 48 although so far this has not produced an increased mortality from treatment‐resistant infections. 45 Antibiotics are widely available over the counter in many Asia–Pacific countries and this availability been shown to contribute to the level of resistance of common bacterial pathogens. 48 , 49 A recent study has shown that a single course of antibiotics in the primary care setting is sufficient to induce resistance in common pathogens for up to 12 months. 50 Just as the emergence of drug resistance in TB has necessitated more stringent use of first‐line therapy, antibiotic therapy for pneumonia may warrant a similar approach.
In recent years, Asia–Pacific countries have seen significant natural disasters, including major tsunamis, earthquakes and bushfires. Respiratory infections are common secondary complications in survivors, and this topic will be included in the Asia–Pacific respiratory health series in subsequent issues of Respirology.
SMOKING‐RELATED DISEASES
Tobacco smoking is a significant contributor to respiratory ill‐health and death in the Asia–Pacific region as it is worldwide. Lung cancer kills more people than any other cancer 1 , 3 and smoking is the most important cause in the majority of cases. 51 Smoking also contributes to airway diseases (COPD and asthma) as well as to non‐respiratory health problems such as cardiovascular disease and other cancers. World‐leading legislative and health promotion efforts in Australia and New Zealand have resulted in a significant decline in the rate of smoking in these countries. Yet in many countries in the region, there has been an alarming increase in tobacco smoking, which is likely to produce a further increase in smoking‐related morbidity and mortality in the future. 51
Lung cancer
Lung cancer (including cancers of the trachea, bronchus and lung parenchyma) is the single biggest contributor to cancer‐related mortality in the Asia–Pacific region and worldwide. 3 Over half a million cases are diagnosed each year in the region and the incidence is increasing. 1 Tobacco smoking is the cause of an overwhelming majority of lung cancers worldwide, and is the likely cause of the increasing rate among Asian men, 52 although other factors (discussed below) contribute to the incidence of the disease including indoor 53 and outdoor 54 air pollution, and exposure to occupational carcinogens. 55
Mortality from lung cancer in Asian women is increasing despite a low rate of smoking among women that in many countries has not significantly increased. While some non‐smoking women are exposed to environmental tobacco smoke, that is, from a husband who smokes (odds ratio 1.2 for lung cancer in a non‐smoking woman exposed to smoke at home by meta‐analysis 56 ), there are thought to be other contributory factors. 57 These factors vary by locality. The use of coal fires with poor ventilation for domestic heating has been shown to be associated with lung cancer, particularly in rural China. 53 , 58 , 59 In the last two decades, some areas have replaced unvented fires with stoves fitted with chimneys, which has been a successful intervention in attempts to bring about a reduction of the incidence of the disease. 60 , 61
In many areas in Asia, women in particular are also exposed to high temperature cooking oil vapours that have also been associated with lung cancer. Studies in China 62 , 63 and Taiwan 64 have shown relative risks of 1.4–3.8 for lung cancer in housewives so exposed in the domestic setting. At least one study 64 has shown that the use of fume extractors diminishes risk, suggesting a dose–response relationship.
A variety of infectious agents have been linked with lung cancer in the region although the nature of any causal relationship remains unclear. 60 Examples include TB infection, 65 the human papillomavirus, 66 , 67 and, in areas of rural Thailand, the fungus Microsporum canis. 68 Further work is needed to clarify or refute the existence of causal pathways linking infection with lung cancer.
The tyrosine kinase inhibitors erlotinib and gefitinib are novel agents for the treatment of lung cancer that bear particular relevance to the Asian population. These drugs have been shown to be particularly effective in adenocarcinomas of the lung, in never smokers, in patients of Asian ethnicity, especially women, and in those with proven endothelial growth factor receptor mutations. 57 , 69 This topic will be further discussed in the Asia–Pacific respiratory health series by Professor T Mok. 70
COPD
COPD is comprised of a heterogeneous group of disorders that includes chronic bronchitis (cough with sputum production), intrinsic airway narrowing (as in asthma) or loss of elastic pulmonary recoil (emphysema). 71 The GOLD criteria (Global initiative for Chronic Obstructive Lung Disease 72 ) has arbitrarily standardized the diagnosis of COPD, defining the disorder by a reduction in the ratio of FEV1 to FVC and progressing in stages of severity by the degree fall in FEV1 expressed as a percentage of the predicted normal value.
COPD by GOLD criteria begins at an arbitrary cut‐off of FEV1/FVC <70%, which has made accurate diagnosis difficult in groups such as the elderly for whom an FEV1/FVC at such a level may be ‘normal’ as assessed by published predicted normal values. Use of appropriate predicted FEV1 figures adjusted for the ethnicity of the population being studied is also important 73 : for example, the normal value for an Asian male subject of a given height is known to be less than that of an equivalent European Australian male subject 73 , 74 and the same is true of other ethnic groups including indigenous Australians. 75 Furthermore, spirometric measures for COPD diagnosis should be recorded after bronchodilator administration to separate asthma (i.e. reversible airflow obstruction) from of COPD (i.e. irreversible obstruction). 71 Later in the Asia–Pacific respiratory health series, Professor Ip will discuss in detail the problems of lack of appropriate reference lung function values for Asian populations and the lack of suitable facilities in certain Asian sectors limits obtaining accurate spirometric values in all patients. 76
Mortality and morbidity statistics for COPD often underestimate its contribution to ill health and death because it is frequently not diagnosed in people with mild disease or recorded as an underlying condition death certificates even in people with diagnosed disease 77 , 78 (for example in patients who die from pneumonia but whose pre‐morbid spirometry is unknown or not recorded). In general, COPD morbidity and mortality increase with age and with pack‐years of tobacco smoking and decrease according to years since smoking cessation. The increase with age may be partly an artefact of the definition.
COPD prevalence in the Asia–Pacific region as a whole is estimated to be 10.6% of adults. 79 The major aetiological contributors to the development of COPD in the Asia–Pacific region are tobacco smoking, air pollution and occupational exposures. 78 , 80
In developed nations such as Australia and New Zealand, the population mortality from COPD has been steadily declining over recent decades in line with a reduction in smoking rates 77 although rates of chronic respiratory disease remain much higher in indigenous populations. 2 By contrast, among Asian men in low to middle income countries, the rates of smoking and COPD mortality and hospitalization are rising. 78 Lower morbidity and mortality in women reflect the fact that smoking is much more common in Asian men than in Asian women. 78
Estimates of current smoking rates in countries within the region vary widely (Table 3). In many parts of the region, smoking rates among men are as high as in China, where 45–75% of men are current smokers, whereas only 1–21% of women smoke, 51 and 10% of the population identifying themselves as former smokers. 81 As a result of an entrenched cultural acceptance of smoking and marketing by the tobacco industry with little restriction, up to 60% of Chinese men who smoke have never considered quitting. 81
Table 3.
Estimates of current smoking rates in the Asia–Pacific region
| Country | Men | Women | Number of studies | ||
|---|---|---|---|---|---|
| Low | High | Low | High | ||
| Australia | 7% | 30% | 7% | 21% | 7 |
| China | 45% | 75% | 1% | 21% | 8 |
| Hong Kong | 29% | — | 11% | — | 1 |
| Japan | 51% | 76% | 2% | 17% | 10 |
| New Zealand | 26% | — | 18% | — | 1 |
| Singapore | 35% | 41% | 3% | 3% | 2 |
| South Korea | 58% | — | 0% | — | 1 |
| Taiwan | 48% | 50% | 2% | 5% | 2 |
Adapted from Barzi et al. 51
The dose–response relationships of smoking to total and respiratory mortality are stronger in Australia and New Zealand than in mainland Asia. 51 Barzi et al. 51 conclude that the most likely explanation for this observation is the relative maturity of the smoking epidemic in Australia and New Zealand compared with the relatively recent uptake among Asian populations. This means that the full impact of smoking‐related disease in Asia has yet to be realized and is not likely to peak for some years to come, although there is already data to support smoking cessation as a means of reducing mortality in Asia. 82
The World Health Organisation predicts that the disease burden of COPD is likely to increase from the 13th to the fifth biggest contributor to worldwide disability‐adjusted life years (DALY), and the Asia–Pacific region is already at the epicentre of this epidemic of morbidity, with COPD ranked third for DALY in the region for 2004. 1 This trend reflects two features of the region: first, the increase in economic prosperity that has resulted in less morbidity from infectious diseases due to better treatment; second, the high rates of tobacco smoking within the region. Despite the rising trend in morbidity and mortality for COPD, lung cancer and other smoking‐related diseases, smoking rates are likely to continue at similar levels or increase further unless effective measures are taken to reduce tobacco smoking by the prevention of smoking uptake and the encouragement of smoking cessation.
ASTHMA, AIR POLLUTION AND OCCUPATIONAL LUNG DISEASE
Asthma
Asthma is a heterogeneous airway disorder characterized by wheeze and variable reversible airflow obstruction. It is typically diagnosed in childhood and both its symptoms and severity may vary between individuals and in one person with asthma over their lifetime.
The prevalence of asthma in developed countries rose markedly in the second half of the 20th century and generally remained low in the developing world, consistent with the ‘hygiene hypothesis’. 83 More recent reports suggest that this trend has stabilized or perhaps slightly reversed 84 and Australia and New Zealand are typical of this tendency. In contrast, international studies of asthma have shown that rates are increasing in developing nations including those of the Asia–Pacific region. 85 , 86 , 87
Despite the increasing prevalence of asthma in Asia, a study of eight Asia–pacific countries showed low levels of asthma control and suboptimal levels of ‘controller’ medications such as inhaled corticosteroids (used by less than 20% of those with severe persistent asthma). 11 In the same study, only one‐third of patients with a diagnosis of asthma had undergone lung function testing, and in general there appeared to be a poor correlation between the severity of asthma and medical management. This was reflected by the fact that nearly half (43.6%) of patients with asthma had attended an emergency department or made unscheduled emergency visits to other health‐care providers in the previous year. These observations may reflect the lower availability of effective asthma medications and medical supervision in communities with lower socioeconomic status.
Air pollution and respiratory health
Outdoor air pollution (in the form of small diameter particulate matter or nanoparticles as well as noxious gases such as ozone, nitrogen dioxide and sulfur dioxide) has been associated with increased respiratory and all‐cause mortality. 88 , 89 Industrial development, a paucity of industrial emission controls, high population density and vehicle emissions in many parts of the Asia–Pacific region contribute to high levels of exposure to air pollution. The World Health Organisation's global burden of disease project 54 examined the public health implications of previous findings and estimated that 800 000 excess deaths were attributable to air pollution worldwide in the year 2000. Developing nations in the Asia–Pacific region accounted for 39% of years of life lost due to air pollution (when the definition of Asia was expanded to include the Indian subcontinent, Asia accounted for 65% of the total burden). 54 Worldwide, outdoor air pollution was estimated to be responsible for 1% of mortality in children age <5 years due to deaths from respiratory infection, 5% of lung and airway cancers in adults, and 3% of total adult cardiopulmonary disease mortality. 54 The same study estimated that, taken together, all exposures to pollution (outdoor and indoor air pollution, water pollution) account for even more disease burden than smoking by perhaps 50%! 54
In Hong Kong, Wong et al. 90 showed that high daily levels of outdoor air pollution produced a significant increase in hospital admissions for respiratory as well as cardiovascular disease with strong effects for both airway diseases (asthma and COPD) and infection (influenza and pneumonia) for various pollutants in the 3 days following high levels. The highest effect sizes for overall respiratory admission in the Hong Kong study were for particulate matter (1.6% increase in relative risk) and ozone (2.2%). 90
Indoor air pollution from the use of solid fuels (such as wood and coal) has been shown to be a major risk factor for respiratory disease including COPD, lung cancer and TB in China 91 and can be anticipated to have similar effects elsewhere. A reduction in these exposures would be expected to significantly reduce mortality and disease burden; 91 without intervention, mortality from COPD and lung cancer in China are predicted to double in the coming decades. 91 , 92
The impact of air pollution particles on respiratory health, especially during bush fires in Asia and Australia, will be further discussed in the Asia–Pacific respiratory health series by Dennekamp et al. 93
The burden of disease from air pollution imposes significant financial costs 94 and health burdens on societies and individuals that are likely to increase with the frenetic pace of development, which continues in many parts of the Asia–Pacific region.
Occupational lung disease
Occupational lung disease represents a significant proportion of respiratory morbidity and mortality in the Asia–Pacific region. The respiratory health consequences of occupational exposure to irritants and carcinogens can include lung cancer, 55 malignant mesothelioma, 95 COPD, 80 asthma, 96 interstitial lung disease 95 , 97 and an increased risk of TB. 97
Taking lung cancer as an example, occupational exposures are estimated to account for 6% of the incidence of lung cancer in developed nations of the Asia–Pacific, and 10% in developing nations; 55 the attributable risks are higher in men (8% in developed and 12% in developing nations), compared with women (3% and 7%, respectively), reflecting the fact that men work more often in occupations with higher carcinogen exposures.
Asbestos production and its use have declined, especially in developed nations, and the removal of existing asbestos (i.e. in buildings) is carefully controlled. 95 However, due to the long lag time (sometimes of more than 20 years) between exposure and the development of both benign (i.e. fibrosis and pleural plaques) and malignant disease (i.e. lung cancer and mesothelioma) due to asbestos exposure has resulted in high rates in areas where asbestos mining has long ceased such as Western Australia. 98 Accurate data on asbestos exposure and related disease are often difficult to obtain in the developing world; however, the production of asbestos continues in countries of the region (including China, the world's second largest producer 99 ), exposures in occupations such as construction may be high, and rates of asbestos‐related disease are likely to peak in the future. 95
LIMITATIONS
This review of respiratory health issues in the Asia–Pacific region faces limitations due to incomplete data in many areas. While mortality data are improving, the majority of South‐East Asian countries have no population level death registration data, and these data are often incomplete. 3 Data on indigenous groups are often limited, although improving in many areas. 2 Figures for infections such as TB rely on notification, which may be incomplete, especially in isolated or impoverished areas. 24 , 100 Although there is increasing use of diagnostic and management guidelines for airways diseases such as Asthma and COPD, diagnostic strategies vary and these diseases are under‐reported in different degrees in different areas. 77 Finally, even where incidence and mortality figures are accurate, the causes and population attributable risks for common respiratory diseases may vary by country and area, and these data are not widely available, meaning that it is often necessary to rely on estimates derived from other populations. 1
CONCLUSIONS
Prominent respiratory health issues in the Asia–Pacific region include smoking‐related diseases, respiratory viruses including influenza, TB, air pollution and occupational lung diseases. While these diseases are significant problems worldwide, they pose particular problems in the region due to increasing smoking rates in some areas, recent viral outbreaks that have spread from the region around the world, variable rates of TB (with or without HIV) and antibiotic resistance of bacterial organisms, and also socioeconomic factors that have produced rising levels of air pollution, often in areas that are the most impoverished. While smoking‐related disease, asthma and TB have stabilized or declined in developed countries, they still require significant medical intervention, and are creating increasing challenges in developing nations. In contrast, influenza outbreaks and air pollution are significant problems throughout the region, which bears a significant proportion of worldwide disease burden for both. Increasingly, nations within the Asia–Pacific are able to look to scientific data to guide medical and strategic approaches to these issues, all of which will continue to be significant health issues in the future.
The Authors: Dr Euzebiusz (Zeb) Jamrozik is a resident medical officer and basic physician trainee at Sir Charles Gairdner Hospital in Perth, Western Australia. He has research interests in clinical and genetic epidemiology, international health, philosophy and ethics. Clinical Professor AW (Bill) Musk has been a respiratory physician at Sir Charles Gairdner Hospital since 1978 and a clinical professor in the School of Population Health at the University of Western Australia since 1988. He graduated in medicine at UWA and has postgraduate degrees from UNSW (MD) and Harvard School of Population Health (MSc: Occupational Medicine). With training in clinical and occupational respiratory medicine, epidemiology and public health, his research interests have been in clinical and epidemiological aspects of lung disease (particularly occupational and environmental lung diseases). He is Chairperson of the Busselton Population Medical Research Foundation and the WA Mesothelioma Registry and has been recognized internationally for his work on asbestos‐related disease and smoking control.
REFERENCES
- 1. WHO . Global Burden of Disease Report: 2004 Update. World Health Organisation, Geneva, 2008. [Google Scholar]
- 2. Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet 2009; 374: 65–75. [DOI] [PubMed] [Google Scholar]
- 3. Mathers CD, Boerma T, Fat DM. Global and regional causes of death. Br. Med. Bull. 2009; 92: 7–32. [DOI] [PubMed] [Google Scholar]
- 4. Sellwood C, Asgari‐Jirhandeh N, Salimee S. Bird flu: if or when? Planning for the next pandemic. Postgrad. Med. J. 2007; 83: 445–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tam JS, Capeding MR, Lum LC et al Efficacy and safety of a live attenuated, cold‐adapted influenza vaccine, trivalent against culture‐confirmed influenza in young children in Asia. Pediatr. Infect. Dis. J. 2007; 26: 619–28. [DOI] [PubMed] [Google Scholar]
- 6. Park AW, Glass K. Dynamic patterns of avian and human influenza in east and southeast Asia. Lancet Infect. Dis. 2007; 7: 543–8. [DOI] [PubMed] [Google Scholar]
- 7. Webster RG. Wet markets—a continuing source of severe acute respiratory syndrome and influenza? Lancet 2004; 363: 234–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO . Pandemic (H1N1) 2009—Update 100 (May). World Health Organisation, Geneva, 2010. [Google Scholar]
- 9. Emanuel EJ. The lessons of SARS. Ann. Intern. Med. 2003; 139: 589–91. [DOI] [PubMed] [Google Scholar]
- 10. Coker R, Mounier‐Jack S. Pandemic influenza preparedness in the Asia‐Pacific region. Lancet 2006; 368: 886–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lai CK, De Guia TS, Kim YY et al Asthma control in the Asia‐Pacific region: the Asthma Insights and Reality in Asia‐Pacific Study. J. Allergy Clin. Immunol. 2003; 111: 263–8. [DOI] [PubMed] [Google Scholar]
- 12. Bishop JF, Murnane MP, Owen R. Australia's winter with the 2009 pandemic influenza A (H1N1) virus. N. Engl. J. Med. 2009; 361: 2591–4. [DOI] [PubMed] [Google Scholar]
- 13. Waterer GW, Hui DS, Jenkins CR. Public health management of pandemic (H1N1) 2009 infection in Australia: a failure! Respirology 2010; 15: 51–6. [DOI] [PubMed] [Google Scholar]
- 14. Zhong N‐S, Zeng G‐Q. Pandemic planning in China: applying lessons from severe acute respiratory syndrome. Respirology 2008; 13: S33–S35. [DOI] [PubMed] [Google Scholar]
- 15. Ferguson NM, Cummings DAT, Cauchemez S et al Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature 2005; 437: 209–14. [DOI] [PubMed] [Google Scholar]
- 16. Cohen D, Carter P. WHO and the pandemic flu ‘conspiracies’. BMJ 2010; 340: 1274–9. [DOI] [PubMed] [Google Scholar]
- 17. Doshi P. Neuraminidase inhibitors: the story behind the Cochrane review. BMJ 2009; 339: 1348–54. [DOI] [PubMed] [Google Scholar]
- 18. Katz MA, Tharmaphornpilas P, Chantra S et al Who gets hospitalized for influenza pneumonia in Thailand? Implications for vaccine policy. Vaccine 2007; 25: 3827–33. [DOI] [PubMed] [Google Scholar]
- 19. Mylius SD, Hagenaars TJ, Lugner AK et al Optimal allocation of pandemic influenza vaccine depends on age, risk and timing. Vaccine 2008; 26: 3742–9. [DOI] [PubMed] [Google Scholar]
- 20. Prieto‐Lara E, Llanos‐Mendez A. Safety and immunogenicity of prepandemic H5N1 influenza vaccines: a systematic review of the literature. Vaccine 2010; 28: 4328–34. [DOI] [PubMed] [Google Scholar]
- 21. Russell CA, Jones TC, Barr IG et al Influenza vaccine strain selection and recent studies on the global migration of seasonal influenza viruses. Vaccine 2008; 26 (Suppl. 4): D31–4. [DOI] [PubMed] [Google Scholar]
- 22. Leroux‐Roels I, Borkowski A, Vanwolleghem T et al Antigen sparing and cross‐reactive immunity with an adjuvanted rH5N1 prototype pandemic influenza vaccine: a randomised controlled trial. Lancet 2007; 370: 580–9. [DOI] [PubMed] [Google Scholar]
- 23. Streefland PH, Chowdhury AM, Ramos‐Jimenez P. Quality of vaccination services and social demand for vaccinations in Africa and Asia. Bull. World Health Organ. 1999; 77: 722–30. [PMC free article] [PubMed] [Google Scholar]
- 24. Mori T. Tuberculosis epidemiology in the Asia‐Pacific region. Respirology 2008; 13 (s3): S56–S64. [Google Scholar]
- 25. Shimouchi A. Tuberculosis problems in the Asia‐Pacific region. Respirology 2001; 6: 75–8. [DOI] [PubMed] [Google Scholar]
- 26. Schaaf HS, Collins A, Bekker A et al Tuberculosis at extremes of age. Respirology 2010; 15: 747–63. [DOI] [PubMed] [Google Scholar]
- 27. Cain KP, Kanara N, Laserson KF et al The epidemiology of HIV‐associated tuberculosis in rural Cambodia. Int. J. Tuberc. Lung Dis. 2007; 11: 1008–13. [PubMed] [Google Scholar]
- 28. Yew WW, Leung CC. Management of multidrug‐resistant tuberculosis: update 2007. Respirology 2008; 13: 21–46. [DOI] [PubMed] [Google Scholar]
- 29. Wardlow H. Men's extramarital sexuality in rural Papua New Guinea. Am. J. Public Health 2007; 97: 1006–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Onozaki I, Raviglione MC. Stopping tuberculosis in the 21st century: goals and strategies. Respirology 2010; 15: 32–43. [DOI] [PubMed] [Google Scholar]
- 31. Chiang C‐Y, Centis R, Migliori GB. Drug‐resistant tuberculosis: past, present, future. Respirology 2010; 15: 413–32. [DOI] [PubMed] [Google Scholar]
- 32. Zignol M, Hosseini MS, Wright A et al Global incidence of multidrug‐resistant tuberculosis. J. Infect. Dis. 2006; 194: 479–85. [DOI] [PubMed] [Google Scholar]
- 33. Espinal MA, Laserson K, Camacho M et al Determinants of drug‐resistant tuberculosis: analysis of 11 countries. Int. J. Tuberc. Lung Dis. 2001; 5: 887–93. [PubMed] [Google Scholar]
- 34. Thiam S, LeFevre AM, Hane F et al Effectiveness of a strategy to improve adherence to tuberculosis treatment in a resource‐poor setting: a cluster randomized controlled trial. JAMA 2007; 297: 380–6. [DOI] [PubMed] [Google Scholar]
- 35. Lobue P, Menzies D. Treatment of latent tuberculosis infection: an update. Respirology 2010; 15: 603–22. [DOI] [PubMed] [Google Scholar]
- 36. Dheda K, Schwander SK, Zhu B et al The immunology of tuberculosis: from bench to bedside. Respirology 2010; 15: 433–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nuermberger EL, Spigelman MK, Yew WW. Current development and future prospects in chemotherapy of tuberculosis. Respirology 2010; 15: 764–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yim J‐J, Selvaraj P. Genetic susceptibility in tuberculosis. Respirology 2010; 15: 241–56. [DOI] [PubMed] [Google Scholar]
- 39. Lange C, Mori T. Advances in the diagnosis of tuberculosis. Respirology 2010; 15: 220–40. [DOI] [PubMed] [Google Scholar]
- 40. Shann F. BCG vaccination in developing countries. BMJ 2010; 340: c809. [DOI] [PubMed] [Google Scholar]
- 41. Andersen P. Tuberculosis vaccines—an update. Nat. Rev. Microbiol. 2007; 5: 484–7. [DOI] [PubMed] [Google Scholar]
- 42. Trunz BB, Fine P, Dye C. Effect of BCG vaccination on childhood tuberculous meningitis and miliary tuberculosis worldwide: a meta‐analysis and assessment of cost‐effectiveness. Lancet 2006; 367: 1173–80. [DOI] [PubMed] [Google Scholar]
- 43. Andersen P, Doherty TM. The success and failure of BCG—implications for a novel tuberculosis vaccine. Nat. Rev. Microbiol. 2005; 3: 656–62. [DOI] [PubMed] [Google Scholar]
- 44. Abu‐Raddad LJ, Sabatelli L, Achterberg JT et al Epidemiological benefits of more‐effective tuberculosis vaccines, drugs, and diagnostics. Proc. Natl Acad. Sci. USA 2009; 106: 13980–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liam CK, Pang YK, Poosparajah S et al Community‐acquired pneumonia: an Asia Pacific perspective. Respirology 2007; 12: 162–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Liam CK, Pang YK, Poosparajah S. Pulmonary tuberculosis presenting as community‐acquired penumonia. Respirology 2006; 11: 786–92. [DOI] [PubMed] [Google Scholar]
- 47. Light RW. Update on tuberculous pleural effusion. Respirology 2010; 15: 451–8. [DOI] [PubMed] [Google Scholar]
- 48. Song JH, Jung SI, Ko KS et al High prevalence of antimicrobial resistance among clinical Streptococcus pneumoniae isolates in Asia (an ANSORP study). Antimicrob. Agents Chemother. 2004; 48: 2101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nys S, Okeke IN, Kariuki S et al Antibiotic resistance of faecal Escherichia coli from healthy volunteers from eight developing countries. J. Antimicrob. Chemother. 2004; 54: 952–5. [DOI] [PubMed] [Google Scholar]
- 50. Costelloe C, Metcalfe C, Lovering A et al Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta‐analysis. BMJ 2010; 340: c2096. [DOI] [PubMed] [Google Scholar]
- 51. Barzi F, Huxley R, Jamrozik K et al Association of smoking and smoking cessation with major causes of mortality in the Asia Pacific Region: the Asia Pacific Cohort Studies Collaboration. Tob. Control 2008; 17: 166–72. [DOI] [PubMed] [Google Scholar]
- 52. Parkin DM, Bray F, Ferlay J et al Global cancer statistics, 2002. CA Cancer J. Clin. 2005; 55: 74–108. [DOI] [PubMed] [Google Scholar]
- 53. Mumford JL, He XZ, Chapman RS et al Lung cancer and indoor air pollution in Xuan Wei, China. Science 1987; 235: 217–20. [DOI] [PubMed] [Google Scholar]
- 54. Cohen AJ, Anderson HR, Ostra B et al The global burden of disease due to outdoor air pollution. J. Toxicol. Eniron. Health 2005; 68: 1–7. [DOI] [PubMed] [Google Scholar]
- 55. Driscoll T, Nelson DI, Steenland K et al The global burden of disease due to occupational carcinogens. Am. J. Ind. Med. 2005; 48: 419–31. [DOI] [PubMed] [Google Scholar]
- 56. Zhong L, Goldberg MS, Parent ME et al Exposure to environmental tobacco smoke and the risk of lung cancer: a meta‐aalysis. Lung Cancer 2000; 12: 797–802. [DOI] [PubMed] [Google Scholar]
- 57. Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers—a different disease. Nat. Rev. Cancer 2007; 7: 778–90. [DOI] [PubMed] [Google Scholar]
- 58. Xu ZY, Blot WJ, Xiao HP et al Smoking, air pollution, and the high rates of lung cancer in Shenyang, China. J. Natl. Cancer Inst. 1989; 81: 1800–6. [DOI] [PubMed] [Google Scholar]
- 59. Wu‐Williams AH, Dai XD, Blot W et al Lung cancer among women in north‐east China. Br. J. Cancer 1990; 62: 982–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lam WK. Lung cancer in Asian women‐the environment and genes. Respirology 2005; 10: 408–17. [DOI] [PubMed] [Google Scholar]
- 61. Lan Q, Chapman RS, Schreinemachers DM et al Household stove improvement and risk of lung cancer in Xuanwei, China. J. Natl. Cancer Inst. 2002; 94: 826–35. [DOI] [PubMed] [Google Scholar]
- 62. Metayer C, Wang Z, Kleinerman RA et al Cooking oil fumes and risk of lung cancer in women in rural Gansu, China. Lung Cancer 2002; 35: 111–7. [DOI] [PubMed] [Google Scholar]
- 63. Wang TJ, Zhou BS, Shi JP. Lung cancer in nonsmoking Chinese women: a case‐control study. Lung Cancer 1996; 14 (Suppl. 1): S93–8. [DOI] [PubMed] [Google Scholar]
- 64. Ko YC, Cheng LS, Lee CH et al Chinese food cooking and lung cancer in women nonsmokers. Am. J. Epidemiol. 2000; 151: 140–7. [DOI] [PubMed] [Google Scholar]
- 65. Gao YT, Zheng W, Jin F. Retrospective cohort study on the association of lung cancer with pulmonary tuberculosis. J. Epidemiol. 1992; 2: S82–8. [Google Scholar]
- 66. Hirayasu T, Iwamasa T, Kamada Y et al Human papillomavirus DNA in squamous cell carcinoma of the lung. J. Clin. Pathol. 1996; 51: 741–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cheng YW, Chiou HL, Sheu GT et al The association of human papillomavirus 16/18 infection with lung cancer among nonsmoking Taiwanese women. Cancer Res. 2001; 61: 2799–803. [PubMed] [Google Scholar]
- 68. Nakachi K, Limtrakul P, Sonklin P et al Risk factors for lung cancer among Northern Thai women: epidemiological, nutritional, serological, and bacteriological surveys of residents in high‐ and low‐incidence areas. Jpn. J. Cancer Res. 1999; 90: 1187–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tsao MS, Sakurada A, Cutz JC et al Erlotinib in lung cancer—molecular and clinical predictors of outcome. N. Engl. J. Med. 2005; 353: 133–44. [DOI] [PubMed] [Google Scholar]
- 70. Lam K‐C, Mok TS. Targeted therapy: an evolving world of lung cancer. Respirology 2011; DOI: 10.1111/j.1440‐1843.2010.01821.x [DOI] [PubMed] [Google Scholar]
- 71. Fletcher C, Peto R, Tinker C et al The Natural History of Chronic Bronchitis and Emphysema: An Eight Year Study of Early Chronic Obstructive Lung Disease in Working Men in London. Oxford University Press, Oxford, 1976. [Google Scholar]
- 72. Global Initiative for Chronic Obstructive Lung Disease strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: an Asia‐Pacific perspective. Respirology 2005; 10: 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Cotes JE, Chinn DJ, Miller MR. Lung Function, 6th edn. Blackwell; Carlton, Australia, 2006. [Google Scholar]
- 74. Woo J, Pang J. Spirometry in healthy elderly Chinese. Thorax 1988; 43: 617–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Bremner PR, de Klerk NH, Ryan GF et al Respiratory symptoms and lung function in aborigines from tropical Western Australia. Am. J. Respir. Crit. Care Med. 1998; 158: 1724–9. [DOI] [PubMed] [Google Scholar]
- 76. Ip MSM. Lung function testing in health and disease–issues pertaining to Asian‐Pacific populations. Respirology 2011; DOI: 10.1111/j.1440‐1843.2010.01850.x [DOI] [PubMed] [Google Scholar]
- 77. Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet 2007; 370: 765–73. [DOI] [PubMed] [Google Scholar]
- 78. Tan WC et al Trends in COPD mortality and hospitalizations in countries and regions of Asia‐Pacific. Respirology 2009; 14: 90–7. [DOI] [PubMed] [Google Scholar]
- 79. Halbert RJ, Natoli JL, Gano A et al Global burden of COPD: systematic review and meta‐analysis. Eur. Respir. J. 2006; 28: 523–32. [DOI] [PubMed] [Google Scholar]
- 80. Blanc PD, Toren K. Occupation in chronic obstructive pulmonary disease and chronic bronchitis: an update. Int. J. Tuberc. Lung Dis. 2007; 11: 251–7. [PubMed] [Google Scholar]
- 81. Yang G, Ma J, Chen A et al Smoking cessation in China: findings from the 1996 national prevalence survey. Tob. Control 2001; 10: 170–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Huxley R, Jamrozik K, Lam TH et al Impact of smoking and smoking cessation on lung cancer mortality in the Asia‐Pacific region. Am. J. Epidemiol. 2007; 165: 1280–6. [DOI] [PubMed] [Google Scholar]
- 83. Ramsey CD, Celedon JC. The hygeine hypothesis and asthma. Curr. Opin. Pulm. Med. 2005; 11: 14–20. [DOI] [PubMed] [Google Scholar]
- 84. Platts‐Mills TAE, Erwin E, Heymann P et al Is the hygiene hypothesis still a viable explanation for the increased prevalence of asthma? Allergy 2005; 60 (s79): 25–31. [DOI] [PubMed] [Google Scholar]
- 85. Braman SS. The global burden of asthma. Chest 2006; 130 (1 Suppl.): 4S–12S. [DOI] [PubMed] [Google Scholar]
- 86. Fok AO, Wong GW. What have we learnt from ISAAC phase III in the Asia‐Pacific rim? Curr. Opin. Allergy Clin. Immunol. 2009; 9: 116–22. [DOI] [PubMed] [Google Scholar]
- 87. Wong GW, Leung TF, Fok TF. ISAAC and risk factors for asthma in the Asia‐Pacific. Paediatr. Respir. Rev. 2004; 5 (Suppl. A): S163–9. [DOI] [PubMed] [Google Scholar]
- 88. Bell ML, Dominici F, Samet JM. A meta‐analysis of time‐series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology 2005; 16: 436–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Stieb DM, Judek S, Burnett RT. Meta‐analysis of time‐series studies of air pollution and mortality: effects of gases and particles and the influence of cause of death, age, and season. J. Air Waste Manag. Assoc. 2002; 52: 470–84. [DOI] [PubMed] [Google Scholar]
- 90. Wong TW, Lau TS, Yu TS et al Air pollution and hospital admissions for respiratory and cardiovascular diseases in Hong Kong. Occup. Environ. Med. 1999; 56: 679–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Lin HH, Murray M, Cohen T et al Effects of smoking and solid‐fuel use on COPD, lung cancer, and tuberculosis in China: a time‐based, multiple risk factor, modelling study. Lancet 2008; 372: 1473–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006; 3: e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Dennekamp M, Abramson MJ. The effects of bushfire smoke on respiratory health. Respirology. 2011; DOI: 10.1111/j.1440‐1843.2010.01868.x [DOI] [PubMed] [Google Scholar]
- 94. Quah E, Boon TL. The economic cost of particulate air pollution on health in Singapore. J. Asian Econ. 2003; 14: 73–90. [Google Scholar]
- 95. Becklake MR, Bagatin E, Neder JA. Asbestos‐related diseases of the lungs and pleura: uses, trends and management over the last century. Int. J. Tuberc. Lung Dis. 2007; 11: 356–69. [PubMed] [Google Scholar]
- 96. Jeebhay MF, Quirce S. Occupational asthma in the developing and industrialised world: a review. Int. J. Tuberc. Lung Dis. 2007; 11: 122–33. [PubMed] [Google Scholar]
- 97. Rees D, Murray J. Silica, silicosis and tuberculosis. Int. J. Tuberc. Lung Dis. 2007; 11: 474–84. [PubMed] [Google Scholar]
- 98. de Klerk NH, Musk AW. Epidemiology of mesothelioma In: Robinson BWS, Chahinian P. (eds) Mesothelioma. Martin Dunitz, London, 2002; 339–49. [Google Scholar]
- 99. Virta R. Minerals Yearbook 2008: Asbestos. United States Geological Survey, Reston, Virginia, 2009. [Google Scholar]
- 100. Cohen T, Colijn C, Wright A et al Challenges in estimating the total burden of drug‐resistant tuberculosis. Am. J. Respir. Crit. Care Med. 2008; 177: 1302–6. [DOI] [PMC free article] [PubMed] [Google Scholar]



