Abstract
Objectives:
Reconstruction of wide lower lip defects is still a challenging subject in terms of obtaining functional and aesthetically acceptable results. Lower lip reconstruction with depressor anguli oris muscle was first described by Tobin in 1983. Since the sensory innervation of this composite muscle flap is provided by the mental nerve, it has been advocated that the mental nerve should be preserve during flap elevation. However, no further study has been conducted about this subject since then.
Methods:
Sixteen patients with lower lip mass have undergone excisional biopsy. The resultant defects were higher than 30% of the total lower lip. All the defects were reconstructed with Depressor anguli oris composite flaps. In 9 of the patients, the mental nerve was preserved and included to the flap, while in remaining patients it was sacrificed. The results were evaluated in terms of sensation, function, and aesthetic appearance.
Results:
In unilaterally reconstructed cases, the results regarding sensation and general complications were similar. However, in bilaterally reconstructed cases, especially where the mental nerve was preserved, the limited arc of rotation has resulted in functional complications, such as whistle deformity in the midline and drooling.
Conclusion:
The mental nerve does not just limit the arc of rotation of the Depressör anguli oris composite flap but also remains as a potential route for metastasis via perineural invasion. Preservation and inclusion of the mental nerve during reconstruction with Depressor anguli oris flap do not provide any superior outcome; on the contrary, these results in various unfavorable events make this flap a poor option. The skin and mucosa of the DAO flap are innervated by the buccal branch of the trigeminal nerve; thus, the mental nerve should not be preserved during surgery.
Keywords: Depressor anguli oris, lower lip, mental nerve
The lips, with their unique anatomical structures, form important esthetic units on the lower 1/3 of the face.[1] Lips are very important in terms of motor and sensory functions. Defects in the lips developed for any reason should be repaired in such a way to preserve the functions of nutrition, respiration, speech, facial expressions, kissing, blowing and self-expression.
The most common cause of defects in lips is defects that occur after cancer surgery.[2] Once the lower lip cancers have reached a certain size, it is not possible to remove the tumor and to repair the defect. In such cases, regional or distant flaps are used for reconstruction of the defect. The most appropriate method for repair is the use of local flaps when there is a defect that does not exceed the mental fold and remains only within the margins of the lips. Many local flaps that are well-known to plastic surgery specialists have been described in the literature.
Depressor anguli oris (DAO) flap is a relatively less frequently used and less often discussed alternative of reconstructive surgery. In fact, depressor anguli oris flap is a very easy repair method in cases of defect of the lower lip extending to commissure. Although depressor anguli oris flap has some disadvantages, it is possible to say that it is an elite method for repairing lost mucosa, muscle and skin with similar tissues in lip reconstruction. If the mental nerve is preserved as described, the rotation of the flap is less preferred in reconstruction as the arc of rotation flap is limited. In this study, reconstruction with DAO flaps with and without preservation of mental nerve and sensory results were shared.
Methods
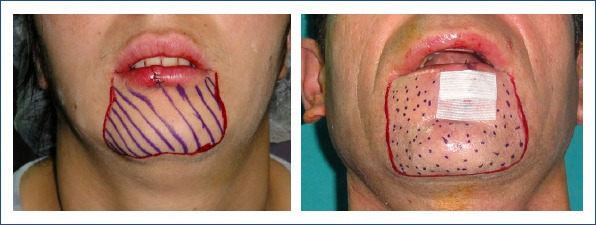
This study was approved by the Ethics Committee of Istanbul Training and Research Hospital. The present study included 16 patients who presented to our clinic with a non-healing wound on the lower lip and underwent reconstruction for defects occupying more than 30% of the lower lip developed after surgical excision. Fourteen patients were male and 2 were female and their ages ranged between 42 and 79 (mean 58.9) years. Patients who underwent surgery for BCC and SCC and lentigo melanoma and required lower lip reconstruction were included in this study. A detailed history of the patients was obtained, and their physical examinations were performed. The lesions were biopsized preoperatively, and their histopathologic diagnoses were made. The operations were planned under general or local anesthesia considering the age and general health of the patients, the size of the tumor and whether or not lymph node dissection was performed. Male patients were allowed to shave beards and mustaches the evening before the surgery. The surgical site was disinfected with 10% povidone- iodine solution after patients received appropriate anesthesia in the operating room. The boundaries of the induration area of the mass were marked in patients undergoing tumor surgery. In accordance with the pathology of the present mass, the mass was excised with an intact skin border of 0.5cm for BCC, 1cm for SCC and 1cm for lentigo melanoma.
All surgical instruments and gloves were replaced after tumor resection. To close the present defect in the lower lip, a plan was made in accordance with the topography of the lower depressor anguli oris muscle on the same side of the defect. The width of the flap was planned to be as much as the vertical dimension of the defect, and the flap length was planned to be about 1 cm longer than the horizontal length of the defect and drawings were made accordingly. The possible entry point of the facial artery to the flap was marked on the planned flap. The flap up to 0.5 cm close to the vascular access site was removed with full preservation of the mental nerve in nine patients and without preservation of the mental nerve in seven patients (Fig. 1). Proximal to this level, only skin and subcutaneous incisions were performed. Facial artery and marginal mandibular nerve were dissected and preserved by blunt dissection. The flap was transposed to the defect. A 3-layer repair, including mucosa, muscle and skin, was applied. The donor area was sutured primarily. After the operation, antibiotics were administered to the patients for one week, and they were requested to gargle with antiseptic solutions. Intake of liquid and soft food was prescribed for five days. The sutures of the surgical wound were removed seven-ten days later. All patients were referred to the radiation oncology outpatient clinic after the pathology results were obtained.
Figure 1.

Rotation arc of the flap in case of preservation or resection of the mental nerve. Black arrow, Marginal mandibular nerve; Green arrow. Preserved mental nerve; Yellow arrow: The cut point of the mental nerve.
Mouth openings of the patients were evaluated postoperatively for microstomy. As a standard easy insertion of the tablespoon into the existing mouth opening and patients’using oral prosthesis without difficulty were accepted as sufficient criteria.
Postoperatively, the patients were compared objectively in terms of fixed two-point discrimination test, hot- cold test, Semmes-Weinstein test and oral continence. Semmes-Weinstein test results were evaluated statistically. SPSS 15.0 for Windows program was used for statistical analysis. In descriptive statistics; categorical variables were expressed as numbers and percentages. The ratios in groups were compared with chi-square analysis. Alpha level of statistical significance was accepted as p<0.05.
Results
Of 16 patients who underwent reconstruction for lower lip defect, 14 were male (87.5%) and two were female (12.5%), including 14 smokers. The ages of these patients ranged from 40 to 79 years. In our study, all of the large lower lip defects (n=16) that could not be closed primarily and been formed as a result of lip cancer surgery. The most common histological diagnoses were SCC (n=14), followed by BCC (n=1) and lentigo malignant melanoma (n=1). The defects secondary to tumor surgery ranged from 3 cm to 7.5 cm (mean, 4.5 cm) in length. Four patients underwent bilateral reconstruction, and 12 patients underwent unilateral depressor anguli oris composite flap surgery. The patients were followed up for six months to two years (median nine months). Complications, such as detachment of sutures, wound dehiscence, fistula formation, sialocele and wound site infection, did not develop in our clinical study (Figs. 2, 3 and 4).
Figure 2.

Patient no 16. (a, b, c) perop, (d) postop 2nd month, (e, f) postop 9th month.
Figure 3.

Patient no 13, (a) preop, (b) perop, (c) postop 1st week, (d, e) postop 8th month.
Figure 4.
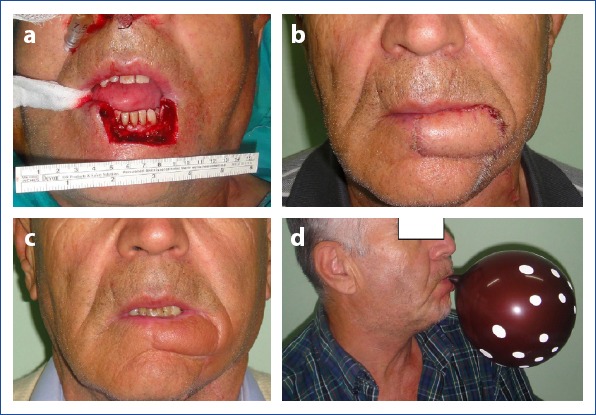
Patient no14, (a) perop, (b) postop two weeks, (c, d) postop five months.
Whistle deformity or drooling was not observed in any of the patients whose mental nerve was not preserved postoperatively, whereas whistle deformity and drooling were seen in one patient due to insufficiency of the flap rotation arch in cases where the mental nerve was preserved. Two patients with these complications were treated with implantation of bilateral flaps with the preservation of mental nerve.
In the two-point discrimination test, all patients were able to discern 6 mm close to normal values after an average of three months postoperatively. In the hot-cold test, it was observed that all patients were able to differentiate between hot and cold sensations one month after the operation.
Cooperative patients were requested to blow balloons to evaluate oral sphincter. It was observed that 12 patients easily inflated the balloons without air leakage. The patients who could not inflate balloons were thought to be unable to do so because of their advanced age and asked to keep water in their mouths. It was observed that the remaining four patients retained the water in their mouth, indicating lack of leakage and sufficient oral continence.
Nine patients with normal tooth integrity were evaluated, and the spoon could easily enter the mouth, and in seven patients who used a prosthesis, the placement and removal of the dental prosthesis through the mouth opening was evaluated, and the mouth opening was sufficient in all patients during all these manipulations.
In the evaluation of beard and mustache integrity in male patients, none of the patients complained about the position or shape of their mustaches while two patients stated that they had problems shaving due to hair growth in the region compatible with the dry mucosa of the lips In one of these patients hairy area was excised, and mucosal advancement flap was used for reconstruction.
According to the results of the evaluation with Semmes Weinstein test, decreased preserved sensation loss or decreased light touch sensation was observed at about postoperative one month after the surgery, decreased light touch or normal sensation in three months. None of the patients had a sensory loss in the upper lip (Table 1, Note: Patients did not apply to our clinic for follow-up as indicated with empty cells of the table.). According to the results of statistical evaluation, the findings showed that there was no significant difference in sensations whether mental nerve was preserved or not (p>0.5).
Table 1.
Semmes-Weinstein test results of the patients who underwent reconstruction with depressor anguli otis flap, at postoperative 1st, 3rd, and 6th months
| Diagnosis | Age | Gender | Preservation of Mental Nerve | Complication | Size of the defects | Flap type | 1 months | 3 months | 6 months | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | SCC | 72 | Male | Yes | Absent | 3.4 cm | Unilateral | Purple | Blue | |
| 2 | SCC | 75 | Female | Yes | Yes | 3 cm | Unilateral | Purple | Blue | |
| 3 | SCC | 40 | Male | Yes | Edema | 4.2 cm | Unilateral | Blue | Green | Green |
| 4 | SCC | 65 | Male | Yes | Absent | 4 cm | Unilateral | Purple | Blue | Green |
| 5 | SCC | 44 | Male | Yes | Edema | 3.4 cm | Unilateral | Blue | Green | Green |
| 6 | SCC | 67 | Male | Yes | Absent | 3.8 cm | Unilateral | Purple | Blue | |
| 7 | SCC | 43 | Male | Yes | Edema | 3.6 cm | Unilateral | Blue | Green | Green |
| 8 | SCC | 73 | Male | Yes | Whistle | 7 cm | Bilateral | Red | Purple | Blue |
| 9 | SCC | 55 | Male | Yes | Drooling | 6.8 cm | Bilateral | Blue | Green | |
| 10 | SCC | 43 | Male | No | Edema | 7.5 cm | Bilateral | Red | Blue | Blue |
| 11 | Lentigo MM | 55 | Male | No | Edema | 4.1 cm | Unilateral | Blue | Green | Green |
| 12 | SCC | 53 | Male | No | Edema | 3.5 cm | Unilateral | Blue | Yeşil | Green |
| 13 | SCC | 76 | Male | No | Absent | 4 cm | Unilateral | Purple | Blui | Blue |
| 14 | SCC | 61 | Male | No | Edema | 3.8 cm | Unilateral | Blue | Blue | Green |
| 15 | BCC | 79 | Male | No | Absent | 3.4 cm | Unilateral | Red | Blue | |
| 16 | SCC | 42 | Male | No | Absent | 7 cm | Bilateral | Blue | Green | Green |
Green color: normal perception, blue colordecreased light touch sensation, purple: decreased preserved sensation, red color: loss of preserved sensation.
Discussion
The deterioration in the structure of the lips, which are the most important aesthetic units of the human face, for whatever reason, leads to significant functional as well as aesthetic deficits. The tissue required for lip reconstruction is a fully composite tissue. A successful lip repair of the skin defect must use a skin resembling the color and tissue of the lip and should contain sufficient amounts of the mucosa to reconstruct vermillion defect and appropriate amounts of muscle tissue to replenish orbicularis oris muscle defects. In addition, it should also contain neural structures for motor and sensory innervation of all these tissues. Instead of skin flaps that only cover the tissue, musculocutaneous flaps, which can perform the functions of oral sphincter also better tolerate the radiation treatment to be performed in the postoperative period.[3]
Many methods have been described for lip reconstruction, [4–11] each of which has its own advantages and disadvantages. Although these methods were of great interest when they were first introduced, some of them were abandoned with time and increasing knowledge of reconstructive surgery. However, some methods have been in use since the earliest times.
The depressor anguli oris composite flap was first described by Tobin in 1983. When Tobin first designed this flap, he planned it as a triangular composite flap with a proximal pedicle located just lateral to the commissure and tapering inferiorly in accordance with the topography of the depressor anguli oris muscle. He determined the maximum length and width of the flap as 4cm and 2.5cm, respectively. They reported that the muscle should be adapted to the orbicularis oris muscle by rotating it for 90 degrees.
In an article, Tobin stated that the mental nerve and marginal mandibular nerve should be preserved. The authors reported that the dissection of the marginal mandibular nerve was difficult and that an incision could be made at the mandibular corpus level to make this dissection more comfortably.[12] Few studies on this flap have been published years after Tobin’s article. In the study of Yenidunya et al.,[13] the authors performed reconstruction of lower lip defect and repaired mental nerve damage using a DAO flap in a male patient and found that the sensation of the flap was intact. Thereafter, they used DAO flap in two patients with lower lip defect without preserving the mental nerve, and the sensation of the lower lip was found to be normal. Moschella et al.[14] performed reconstructive surgeries using depressor angulis oris muscle flaps in 70 patients and stated that the mental nerve could be easily visualized during the elevation of the muscle, but if this nerve was cut, the sensation would be provided from the buccal nerve. They argued that the mental nerve, which makes the rotation of the flap difficult, should not be included in the flap.[13, 14]
To determine the area innervated by sensory branches of mental nerve, the patients were admitted to our clinic because of a mass or scar on the lower lip, and underwent bilateral mental nerve block. Then, the boundaries of the anesthetized area were marked. In these patients, the results showed that the lower lip and chin skin were numbed after a mental block (Fig. 5). The anesthetized area remains outside the planned flap area in the jaw.
Figure 5.
Anesthetized area innervated by mental nerve.
Hendy et al.[15] marked the anesthetized area before the oral intervention in 20 patients who had mental blocks before the oral intervention, and according to the results they obtained, it was found that the boundaries of this area were between two premolar teeth posteriorly and between the incisors anteriorly. The defined area of anesthesia is usually located in the lower lip region excised due to a tumor. The mucosal component of the depressor anguli oris composite flap is prepared from outside the area innervated by the mental nerve. Mental nerve receives sensory stimuli from the skin and mucosa of the lower lip and chin.[13, 16–19]
Available anatomical studies in the literature showed that the buccal nerve receives sensory impulses coming from the lower buccal gingiva, lower buccal sulcus, buccal mucosa and the skin of the cheek.[13, 18, 20] The depressor anguli oris composite flap is prepared from the cheek skin and mucosa and the sensation of the region is not related to the mental nerve.
Hun-Mu Yang et al. conducted an anatomical study on the distribution of buccal nerve using Sihler staining method in eight cadavers. Muscles are made translucent by Sihler staining method, and nerve distribution is observed more clearly. To investigate basically the distribution pattern of the buccal nerve, the distribution of the buccal nerve was investigated by dividing the mouth, and its surroundings into four sections as superomedial, superolateral, inferolateral and inferomedial parts with vertical lines passing through the base of the facial columella and horizontal imaginary lines passing through the mental foramen level and the commissure level. The authors indicated that in the majority of the investigated series, the main branch of buccal nerve receives the sensory impulses from the inferomedial region of the buccal area that lies lateral to the commissure. Some of the fibers separated from the main branch of the buccal nerve extend into the inferomedial region and receive the sensation thereof. They found out that some branches of the buccal nerve terminated near the commissure in the superomedial part and mixed with the branches of the infraorbital nerve, while the buccal nerve gave branches to the upper lip localized lateral to the ala nasi. In 66.7% of the cases, a branch arising from the main root of the buccal nerve leads a vertical course and receives the sensory impulses from the inferolateral region. In addition, in this study, it was stated that the skin and mucosal sensation of the mandibular area (cheek) close to the lower lip region is provided by the buccal nerve and that both mental and buccal nerves receive sensory impulses from the lower lip around the commissure.[21]
In our clinic, in four of seven patients who underwent reconstruction with DAO flap and whose mental nerve was not preserved, nearly normal sensation in four patients at the first postoperative month (Semmes Weinstein blue), normal sensation in three, and nearly normal sensation in three patients at the third month (Semmes Weinstein green) were observed. Still, normal sensation was noted in four, and nearly normal sensation in three patients at 6th month normal sensation was observed in four patients and near-normal sensation in three patients. In all patients where the mental nerve was preserved or not, two-point discrimination test results were close to normal values at three months postoperatively. The distinction between hot and cold sensations could be discerned by all patients at the first postoperative month. In the light of this information, we conclude that the sensation is normal or close to normal in operations where the mental nerve is not preserved.
There are studies in the relevant literature that demonstrated that the most frequent condition that affects the trigeminal nerve peripherally was a perineural spread of head and neck carcinomas. The perineural spread is seen in SCC, BCC, adenoid cystic carcinoma, mucoepidermoid carcinoma, lymphoma, sarcoma and malignant melanoma, but it is most commonly observed in SCC with a rate of 5-14%.[22] Perineural spread may be forward or backward.[23] Clinically, the diagnosis of perineural spread cannot be made without extensive perineural spread. Perineural invasion is associated with a high rate of recurrence and metastasis. Therefore, we think that cutting the mental nerve provides an advantage for the patients who have DAO flap prepared for tumor surgery.
DAO flap is a very reliable flap rergarding vascularization and can be applied easily because it can be perfused with reverse flow through the angular artery even in the patient group with bilateral neck dissection in whom both facial arteries are ligated.
Conclusion
Preservation of mental nerve which is the pathway of cranial metastasis through a perineural spread in carcinomas causes whistle deformity due to restriction of rotation arc via restricting rotation of the anguli oris muscle to the defect during the preparation of the flap. Therefore, it does not confer any advantages, contrarily, it leads to many adverse conditions and causes this flap to be almost forgotten. The sensation of the skin and mucosa in the flap is provided by the buccal branch of the trigeminal nerve.
The results were similar in terms of sensory and general complications in cases of unilateral flap implantation, particularly in bilateral flap reconstruction procedures where the mental nerve is preserved lower lip midline whistle deformity or drooling complications due to inadequate flap rotation arc may develop. To prevent such complications, there is no need to preserve the mental nerve that does not provide sensory stimuli to the flap and restricts rotation arc of the flap.
Disclosures
Ethics Committee Approval: The study was approved by the Local Ethics Committee.
Peer-review: Externally peer-reviewed.
Conflict of interest: None declared.
Authorship Contributions: Concept – S.S.Ş., M.O.Y.; Design – S.S.Ş., M.O.Y.; Supervision – M.O.Y.; Materials – S.S.Ş., M.O.Y.; Data collection &/or processing – S.S.Ş., M.O.Y.; Analysis and/or interpretation – S.S.Ş., M.O.Y.; Literature search – S.S.Ş.; Writing – S.S.Ş.; Critical review – S.S.Ş.
References
- 1.Tellioglu AT, Kocer U, Celebioglu S, Sensoz O, Akyuz M. Applications of innervated depressor anguli oris flap in lower lip reconstruction. Türk Plast Cer Derg. 1994;2:41–5. [Google Scholar]
- 2.Siegert R, Weerda H. The history of lip reconstruction. Facial Plast Surg. 1990;7:63–71. doi: 10.1055/s-2008-1064666. [DOI] [PubMed] [Google Scholar]
- 3.Denewer AD, Setit AE, Hussein OA, Aly OF. Functinal and aesthetic outcome of reconstruction of large oro-facial defects involving the lip after tumor resection. J Egypt Natl Canc Inst. 2006;18:61–6. [PubMed] [Google Scholar]
- 4.Mazzola RF, Lupo G. Evolving concepts in lip reconstruction. Clin Plast Surg. 1984;11:583–617. [PubMed] [Google Scholar]
- 5.Williams EF, 3rd, Setzen G, Mulvaney MJ. Modified Bernard-Burow cheek advancement and cross-lip flap for total lip reconstruction. Arch Otolaryngol Head Neck Surg. 1996;122:1253–8. doi: 10.1001/archotol.1996.01890230097017. [DOI] [PubMed] [Google Scholar]
- 6.Madaree A, McGibbon IC, Morris WM. Reconstruction of both upper and lower lips. J Craniomaxillofac Surg. 1993;21:168–71. doi: 10.1016/s1010-5182(05)80107-6. [DOI] [PubMed] [Google Scholar]
- 7.Adler N, Amir A, Hauben D. Modified von Bruns'technique for total lower lip reconstruction. Dermatol Surg. 2004;30:433–7. doi: 10.1111/j.1524-4725.2004.30121.x. [DOI] [PubMed] [Google Scholar]
- 8.Pirgousis P, Fernandes R. Reconstruction of subtotal defects of the lower lip:a review of current techniques and a proposed modification. J Oral Maxillofac Surg. 2011;69:295–9. doi: 10.1016/j.joms.2010.05.079. [DOI] [PubMed] [Google Scholar]
- 9.Mutaf M, Bulut O, Sunay M, Can A. Bilateral musculocutaneous unequal-Z procedure:a new technique for reconstruction of total lower-lip defects. Ann Plast Surg. 2008;60:162–8. doi: 10.1097/SAP.0b013e3180582533. [DOI] [PubMed] [Google Scholar]
- 10.Kayıkçıoğlu A, Mavili E, Moray G. Dudak defektlerinin rekonstrüksiyonu. Cerrahi Tıp Bülteni. 1993;2:173–80. [Google Scholar]
- 11.Baumann D, Robb G. Lip reconstruction. Semin Plast Surg. 2008;22:269–80. doi: 10.1055/s-0028-1095886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tobin GR, O'Daniel TG. Lip reconstruction with motor and sensory innervated composite flaps. Clin Plast Surg. 1990;17:623–32. [PubMed] [Google Scholar]
- 13.Yenidunya MO, Yilmaz S, Demirseren ME. Sensorial innervation of the depressor anguli oris flap:from the buccal nerve or the mental nerve? Plast Reconstr Surg. 2000;105:2623–5. doi: 10.1097/00006534-200006000-00062. [DOI] [PubMed] [Google Scholar]
- 14.Moschella F, Cordova A. “Depressor flaps” for large defects of the lower lip and mental region. Plast Reconstr Surg. 2005;115:252–6. [PubMed] [Google Scholar]
- 15.Hendy CW, Robinson PP. The sensory distribution of the buccal nerve. Br J Oral Maxillofac Surg. 1994;32:384–6. doi: 10.1016/0266-4356(94)90030-2. [DOI] [PubMed] [Google Scholar]
- 16.Langstein HN, Robb GL. Lip and perioral reconstruction. Clin Plast Surg. 2005;32:431–45. doi: 10.1016/j.cps.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Mellette JR, Jr, Chapman JT. Practical perioral closures. Semin Cutan Med Surg. 2003;22:255–62. doi: 10.1016/S1085-5629(03)00075-0. [DOI] [PubMed] [Google Scholar]
- 18.Craven J. Cranial nerves. Anaesthesia & Intensive Care Medicine. 2004;5:395–9. [Google Scholar]
- 19.Galyon SW, Frodel JL. Lip and perioral defects. Otolaryngol Clin North Am. 2001;34:647–66. doi: 10.1016/s0030-6665(05)70010-4. [DOI] [PubMed] [Google Scholar]
- 20.Malard O, Corre P, Jégoux F, Durand N, Dréno B, Beauvillain C, et al. Surgical repair of labial defect. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:49–62. doi: 10.1016/j.anorl.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Yang HM, Won SY, Lee JG, Han SH, Kim HJ, Hu KS. Sihler-stain study of buccal nerve distribution and its clinical implications. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:334–9. doi: 10.1016/j.tripleo.2011.03.031. [DOI] [PubMed] [Google Scholar]
- 22.Maroldi R, Farina D, Borghesi A, Marconi A, Gatti E. Perineural tumor spread. Neuroimaging Clin N Am. 2008;18:413–29. doi: 10.1016/j.nic.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Borges A, Casselman J. Imaging the trigeminal nerve. Eur J Radiol. 2010;74:323–40. doi: 10.1016/j.ejrad.2010.02.006. [DOI] [PubMed] [Google Scholar]


