Abstract
Background:
Patients undergoing the addition of a contralateral prophylactic mastectomy with unilateral breast cancer have an increased and potentially doubled post-operative complication rate. One documented detriment from post-operative complications is the potential delay in initiating adjuvant therapy. To determine if the addition of a gynecologic and/or plastic reconstructive procedure to breast surgery results in an increased risk of post-operative complications and re-admissions, we evaluated outcomes in patients undergoing single vs multi-site surgery in a large national surgical database.
Methods:
We utilized the National Surgery Quality Improvement Program (NSQIP) database to identify patients who underwent breast surgery between 2011–2015. We extracted patients who underwent prophylactic oophorectomy with or without hysterectomy as a comparison group. Chi square analysis was used to assess post-operative outcomes including complications, readmission, and reoperation. All statistics were performed in SPSS v. 24.
Results:
During the study timeframe, 77,030 patients had a solitary or combined breast surgical procedure and a second cohort of 124 patients underwent gynecologic surgery. Breast patients who did not have a simultaneous reconstruction or gynecologic procedure were older with more comorbidities. Patients undergoing coordinated procedures had a significantly longer length of stay, higher complication, readmission, and reoperation rates (p<0.001 for all) as compared with patients who underwent single site surgery.
Conclusions:
Patients with surgery for a breast cancer, either with a plastic or gynecologic procedure, have greater post-operative complications. Higher complication rates for those with coordinated operations may lead to delays in adjuvant therapy and discussions regarding the indications for simultaneous surgery are recommended.
Keywords: Combined breast surgery
Introduction
Breast cancer is the most common cancer in women, accounting for >250,000 new cases annually in the United States. Furthermore, it is expected that >40,000 women will die from breast cancer in 2017. Timely adjuvant systemic therapy (within 8–12 weeks of surgery) in patients with an invasive breast cancer has been found to improve survival.1 A meta-analysis has demonstrated that for every four week delay in adjuvant therapy a 15% decrease in survival can occur; emphasizing the importance of reducing post-operative recovery time from a breast cancer surgery.2
Many patients undergo coordinated breast cancer surgery in association with an immediate reconstruction inclusive of contralateral prophylactic mastectomy (CPM). Previous studies have demonstrated increased post-operative complications in breast cancer patients who undergo bilateral mastectomy as compared with unilateral mastectomy.3,4 Patients who undergo contralateral prophylactic mastectomy have higher rates of overall complications and wound complications.5 One study, however demonstrated a 50% reoperation rate in patients who experienced complications after CPM, yet identified no correlation with a delay in initiation of adjuvant therapy.6 There is therefore conflicting evidence from observational studies regarding the impact of breast reconstruction on adjuvant therapy delays with an ongoing prospective cohort evaluating this issue in the United Kingdom.7
In addition to coordinated plastic surgery, a subset of patients at high risk for breast cancer and those with existing breast cancer undergo coordinated gynecologic surgery. There is limited data evaluating the outcomes from these multi-site coordinated surgeries and the subsequent effects on adjuvant therapy initiation. An analysis of 62 patients with BRCA 1 or 2 mutations evaluated complications in patients who underwent breast surgery and sequential versus coordinated risk reduction salpingo-oophrectomy.8 The authors identified a complication rate of 21% in patients who underwent coordinated procedures compared with 5% in patients who had sequential procedures. Batista and colleagues reviewed 12 high risk patients who had simultaneous prophylactic mastectomy and BSO.9 The majority of patients also had plastic surgery procedures and one third of patients in the study experienced complications. There is however a paucity of data evaluating the potential risks of coordinated surgeries in patients with a known breast malignancy.
We hypothesized that patients who underwent coordinated gynecologic and plastic surgery procedures at the time of surgery for breast cancer would have greater post-operative complications and hospital re-admissions. Our aim in this study was to assess the proportion of patients who underwent breast surgery with simultaneous gynecologic and plastic surgery procedures in a modern national surgical dataset, compare patient demographics and comorbidities in patients who underwent coordinated surgery versus those with breast surgery alone, and evaluate post-operative outcomes in patients by procedure type.
Methods
We identified patients who underwent breast surgery from the American College of Surgeons National Surgery Quality Improvement Project (ACS NSQIP) database between 2011–2015. The experimental protocol was approved by the institutional review committee and met the guidelines of the responsible governmental agency. We included patients who underwent partial or total mastectomy and excluded individuals who did not undergo axillary surgery to include those with a presumed primary breast cancer. We also identified patients who underwent prophylactic oophorectomy with or without hysterectomy as a comparative group. Patients were grouped by procedure type including: breast surgery alone, gynecologic surgery alone, breast and gynecologic surgery, breast and plastic surgery, and breast, gynecologic, and plastic surgery.
Patient demographics and ACS NSQIP defined comorbidities were evaluated in each surgical group. Age was categorized in four groups, defined by quartiles. Obesity was defined as BMI >25. We evaluated the following operative values: breast procedure, type of axillary procedure, and operative time in minutes. The index hospitalization length of stay was compared between groups. The primary outcome of interest was post-operative complication. Complication was defined as having any ACS NSQIP defined complication within 30 days of surgery. Secondary outcomes of interest included 30 day readmission, reoperation, and mortality rates.
The prevalence of coordinated surgery was evaluated by assessing the frequency of each surgical group. Descriptive statistics were performed to describe the study population. Chi square analysis was utilized to assess explanatory variables as well as operative characteristics and length of stay. Independent t tests were utilized to assess continuous variables. A logistic regression analysis was performed with explanatory variables found to be significant on univariate analysis for each outcome of interest. Correlation coefficients were calculated for all explanatory variables to assess for collinearity. All statistics were performed in SPSS v 24 and p values <0.05 were considered significant.
Results
During the study period, 164,716 patients underwent solitary or combined breast surgery. After applying exclusions, 77,030 patients comprised the final study sample. There were 55,766 (72%) patients who underwent breast surgery alone, 21,055 (27%) who had combined breast and plastic surgery, 135 (<1%) underwent combined breast and gynecologic surgery, and 74 (<1%) patients had coordinated breast, gynecologic, and plastic surgery. The cohort of patients who underwent a non-malignant gynecologic operation without breast surgery was 124 patients.
Patient demographic and comorbidity data is listed by surgical group in Table 1. Patients who underwent breast surgery alone, were significantly more likely to be older with >50% over the age of 60 (p < 0.001). Conversely, in the group of patients who underwent breast, gynecologic, and plastic surgery, 75% were <50 years of age. Patients with coordinated operations were also much less likely to be obese or have diabetes, as compared with patients who underwent breast surgery alone (p < 0.001). Patients who underwent plastic surgery as part of their combined surgery were less likely to be actively smoking when compared with other groups (p <0.001).
Table 1:
Study Population
| Breast N = 55,766 n (%) | Breast, Plastics N = 21,055 n (%) | Breast, Gynecology N = 135 n (%) | Breast, Plastics, Gynecology N = 74 n (%) | Gynecology N = 124 n (%) | P value | |
|---|---|---|---|---|---|---|
| Age (Quartile) | <0.001 | |||||
| 18–50 | 10,286 (18.4) | 9,979 (47.4) | 69 (51.1) | 55 (74.3) | 77 (62.1) | |
| 51–60 | 13,447 (24.1) | 6,329 (30.1) | 30 (22.2) | 14 (18.9) | 26 (21.0) | |
| 61–69 | 15,070 (27) | 3,661 (17.4) | 22 (10.4) | 4 (5.4) | 11 (8.9) | |
| 70+ | 16,767 (30.1) | 1,085 (5.2) | 14 (10.4) | 1 (1.4) | 10 (8.1) | |
| BMI > 25 | 41,461 (74.3) | 13,670 (64.9) | 90 (66.7) | 48 (64.9) | 90 (72.6) | <0.001 |
| Diabetes | 8,382 (15.0) | 1,227 (5.8) | 11 (8.1) | 1 (1.4) | 34 (27.4) | <0.001 |
| Smoker | 7,178 (12.9) | 2,427 (11.5) | 23 (17.0) | 6 (8.1) | 13 (10.5) | <0.001 |
Table 2 demonstrates operative characteristics and length of stay by surgery type. Patients who underwent combined procedures were significantly more likely to undergo total mastectomy (p < 0.001). Both operative time and length of stay increased with coordinated procedures (p < 0.001). The longest operative time and length of stay was in the combined surgery group that underwent breast, plastic, and gynecologic surgery with mean operative time of 349 minutes.
Table 2:
Operative Characteristics and Length of Stay
| Breast N = 55,766 n (%) | Breast, Plastics N = 21,055 n (%) | Breast, Gynecology N = 135 n (%) | Breast, Plastics, Gynecology N = 74 n (%) | Gynecology N = 124 n (%) | P value | |
|---|---|---|---|---|---|---|
| Breast Procedure | ||||||
| Partial Mastectomy | 28,848 (52) | 927 (4) | 34 (25) | 3 (4) | ||
| Total Mastectomy | 26,918 (48) | 20,128 (96) | 101 (75) | 71 (96) | N/A | <0.001 |
| Axillary Procedure | ||||||
| Sentinel Biopsy | 36,578 (66) | 14,315 (68) | 83 (62) | 44 (59) | ||
| ALND | 19,188 (34) | 6,740 (32) | 51 (38) | 30 (41) | N/A | <0.001 |
| Operative Time (Mean) | 103 min. | 128 min. | 241 min. | 349 min. | 106 min. | <0.001 |
| Length of Stay (Days) | 0.77 | 1.84 | 1.76 | 2.34 | 1.27 | <0.001 |
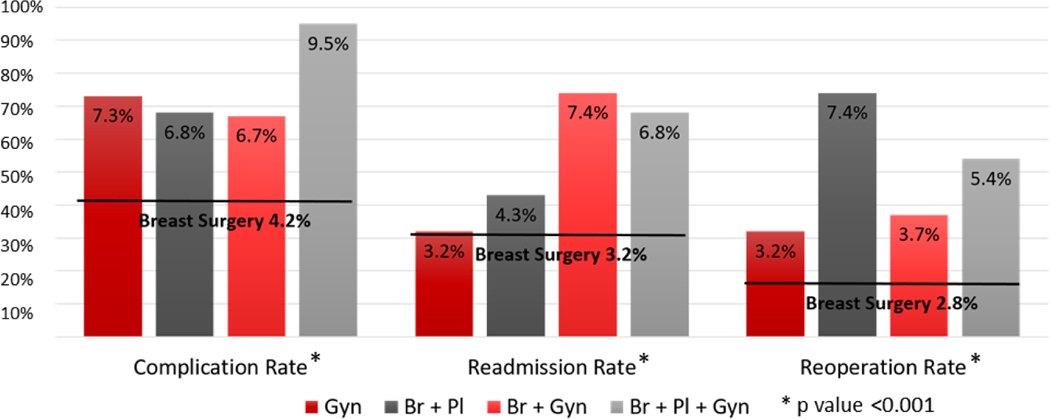
Thirty day post-operative outcomes by procedure type are displayed in Figure 1. Patients who had coordinated surgery were significantly more likely to suffer post-operative complications, with a 2-fold increase in complications in patients who had surgery with all three specialties (p<0.001). Similarly, readmission (p<0.001) and reoperation rates (p<0.001) were increased in patients who had combined procedures. Patients undergoing gynecologic surgery alone had equivalent readmission and reoperation rates to breast surgery alone but had greater post-operative complications as compared with the breast surgery alone group.
Figure 1:
Post-operative outcomes by procedure type. The black horizontal line represents complication rates for patients who underwent breast surgery alone. Br: Breast Surgery, Gyn: Gynecologic Surgery, Pl: Plastic Surgery
The results of the multivariate analysis for post-operative complications are summarized in Table 3. All assessed variables were found to independently predict post-operative complications. The strongest predictors of complications were mastectomy (OR 1.903, 95% CI 1.741–2.080) and diabetes (OR 1.674, 95% CI 1.531–1.831). Multivariate analysis for readmission revealed obesity (OR 1.312, 95% CI 1.194–1.441), diabetes (OR 1.427, 95% CI 1.282–1.589), smoking (OR 1.338, 95% CI 1.201–1.490), longer operative time (OR 1.002, 95% CI 1.001–1.002), and mastectomy (OR 1.277, 95% CI 1.167–1.398) to be independent predictors for worse outcomes. Independent predictors of reoperation included obesity (OR 1.176, 95% CI 1.080–1.280), smoking (OR 1.448, 95% CI 1.314–1.596), longer operative time (OR1.003, 95% CI 1.003–1.003), and mastectomy (OR 1.935, 95% CI 1.761–2.126).
Table 3:
Independent Predictors of Post-Operative Complications
| OR | 95% CI | P value | |
|---|---|---|---|
| Age (Quartile) | |||
| 51–60 | 1.203 | 1.098–1.317 | <0.001 |
| 61–69 | 1.203 | 1.091–1.327 | <0.001 |
| 70+ | 1.369 | 1.235–1.519 | <0.001 |
| BMI > 25 | 1.442 | 1.326–1.567 | <0.001 |
| Diabetes | 1.694 | 1.549–1.852 | <0.001 |
| Smoker | 1.508 | 1.378–1.651 | <0.001 |
| Operative Time | 1.003 | 1.003–1.004 | <0.001 |
| Mastectomy | 2.064 | 1.892–2.251 | <0.001 |
Discussion
We evaluated patients with a primary breast malignancy who underwent breast surgery alone as compared with patients who underwent concurrent gynecologic or plastic surgery procedures in the NSQIP database. We found that patients in this selected dataset who underwent breast surgery alone were older with more comorbidity than patients who underwent combined surgery. Coordinated surgery was found to correlate with higher mastectomy rates, longer operative time, and longer length of hospital stay. Patients who underwent concurrent gynecologic or plastic surgery were found to have higher complication, readmission, and reoperative rates when compared with patients who underwent breast surgery alone. Patients undergoing primary gynecologic surgery had an increased complication rate in comparison to those with breast surgery alone but similar readmission and reoperation rates. These findings suggest that coordinated gynecologic and plastic surgery increases post-operative morbidity in comparison to single site surgery.
This is one of the first studies to assess outcomes after coordinated procedures in patients with presumed breast cancer in a national surgical dataset. Despite increased age and comorbidity in the breast only group, these patients were found to have less post-operative complications as compared with patients who underwent coordinated surgery. Patients who underwent gynecologic procedures alone also had more comorbidity, but were of similar age to patients who had coordinated surgery. Del Corral10 and colleagues studied patients with BRCA mutations who underwent bilateral free flap breast reconstruction and gynecologic procedures and compared post-operative outcomes with patients who had immediate reconstruction without gynecologic surgery. Specifically, there was no difference in DVT (p=1.0), arrhythmia (p=0.195), cardiac complications (p=0.088), gastrointestinal bleeding (p=0.119), or heart failure (p=0.251) between the two groups. The authors evaluated 42 patients who had simultaneous breast, plastic, and gynecologic surgery and found no difference in post-operative complications compared to more than 400 patients who had breast and plastic procedures without concurrent gynecologic surgery. We would expect higher complication rates in our study given that we included only patients who had axillary procedures in an effort to isolate patients with primary breast cancer. However, we identified a significant increase in complications when adding gynecologic surgery to breast and plastic surgery (9.5% vs 6.8%), which differs from the conclusions of Del Corral and colleagues.10
We found the group at highest risk for post-operative complications was patients who underwent simultaneous breast, plastic, and gynecologic procedures, this group had a 2-fold increase in complications as compared with patients who underwent breast surgery alone. Previous studies utilizing ACS NSQIP data have identified complication rates similar to the rate of 4.2% we found in patients who underwent breast surgery alone. Lyle et al.11 found that 3.5% of patients undergoing breast conservation surgery suffered complications. A NSQIP analysis of more than 11,000 patients found complications in 2.1% of patients who underwent breast conservation therapy and 5.5% of patients who underwent mastectomy with expander or implant reconstruction.12 Other single institution studies have demonstrated higher complication rates between 3– 33% in patients who underwent prophylactic oophorectomy at the time of surgery for breast cancer.8,9,13 Similarly, multiple studies have found that the addition of contralateral prophylactic mastectomy confers a 1.3–1.8 fold increase in complication rates for patients with breast cancer.3–5 We found that the addition of simultaneous gynecologic and plastic surgery corresponded to an increase in post-operative complications, which increased incrementally with more coordinated procedures.
Evaluating the differences in complications and readmission rates in patients who undergo coordinated versus sequential plastic and gynecologic procedures will help inform patients regarding the risks and benefits of these approaches. Chapman et al.8 studied patients with BRCA1 or BRCA2 mutations and breast cancer. The authors found that women who underwent sequential risk reducing salpingo-oophrectomy (RRSO) following surgery for breast cancer had longer operative times (8.25 vs 6.38 hours, p=0.006) and longer length of stay (4.79 vs 3.44 days, p=0.01) as compared with patients who underwent simultaneous RRSO. Comorbidity between the sequential and simultaneous RRSO groups were similar, while older patients were more likely to have coordinated surgery (45 vs 39 years, p=0.025). Unfortunately, given the limitations of the ACS NSQIP database, we were unable to identify a comparison group of patients who underwent sequential plastic or gynecologic surgery for the purposes of this study.
We evaluated independent predictors of post-operative outcomes in the study population. We found all explanatory variables to independently predict post-operative complications, while obesity, smoking, longer operative time, and mastectomy independently predicted both readmission and reoperation within 30 days. Chapman et al. performed an analysis of coordinated versus sequential RRSO8 and also identified longer operative times as a predictor for post-operative complications. The authors found that patients with complications had operations an average of 2.2 hours longer than patients without complications. Batista et al.9 evaluated women at high risk for breast cancer who underwent prophylactic mastectomy and RRSO simultaneously. Four of the 12 patients included in the study suffered complications, interestingly, only patients who also had plastic surgery reconstruction suffered complications.
This study has several limitations. The ACS NSQIP database does not reliably capture breast cancer diagnosis in patients who have breast surgery, making it difficult to identify a group of patients known to have primary breast cancer. We controlled for this by including only patients who underwent breast surgery with a simultaneous axillary procedure. Similarly, the database does not capture patients at high risk for breast cancer including status of BRCA1 or BRCA2 mutations. The ACS NSQIP database only collects data for the 30 day post-operative period which therefore does not include complications which are diagnosed later in the post-operative course or longer term patient outcomes. As ACS NSQIP selectively captures data, this limits the number of patients identified over a 5 year period. We also found a higher than expected proportion of patients who underwent mastectomy in the database, which can be explained by targeting of reconstruction procedures by the NSQIP database. Finally, the details of the reconstructive procedures were unable to be ascertained from the database.
Despite these limitations, we believe this study strengthens the literature on coordinated surgery in breast cancer patients. Although the number of patients in each group are small in our study, this is a much larger study than previously published work evaluating combined surgery in breast cancer patients. We utilized a national dataset, while much of the current literature is single institution studies. We were also able to compare outcomes across 4 groups of patients who underwent breast surgery and identified a comparison group of patients who underwent gynecologic surgery alone.
Conclusion
Patients who underwent coordinated procedures at the time of breast surgery for presumed breast cancer were found to be younger with less comorbidity. While the combined surgery groups were healthier pre-operatively, patients who underwent coordinated surgery had higher post-operative morbidity when compared with patients who underwent breast surgery alone. Future research may focus on the effect of this post-operative morbidity on timing of adjuvant chemotherapy and long term outcomes.
Footnotes
This manuscript was presented in poster format at the American Society of Breast Surgeons Annual Meeting in 2017. The authors have no disclosures to report.
References
- 1.Yu KD, Huang S, Zhang JX, Liu GY, Shao ZM. Association between delayed initiation of adjuvant CMF or anthracycline-based chemotherapy and survival in breast cancer: a systematic review and meta-analysis. BMC Cancer. 2013;13:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raphael MJ, Biagi JJ, Kong W, Mates M, Booth CM, Mackillop WJ. The relationship between time to initiation of adjuvant chemotherapy and survival in breast cancer: a systematic review and meta-analysis. Breast cancer research and treatment. 2016;160(1):17–28. [DOI] [PubMed] [Google Scholar]
- 3.Miller ME, Czechura T, Martz B, et al. Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Ann Surg Oncol. 2013;20(13):4113–4120. [DOI] [PubMed] [Google Scholar]
- 4.Momoh AO, Cohen WA, Kidwell KM, et al. Tradeoffs Associated With Contralateral Prophylactic Mastectomy in Women Choosing Breast Reconstruction: Results of a Prospective Multicenter Cohort. Ann Surg. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osman F, Saleh F, Jackson TD, Corrigan MA, Cil T. Increased postoperative complications in bilateral mastectomy patients compared to unilateral mastectomy: an analysis of the NSQIP database. Ann Surg Oncol. 2013;20(10):3212–3217. [DOI] [PubMed] [Google Scholar]
- 6.Eck DL, Perdikis G, Rawal B, Bagaria S, McLaughlin SA. Incremental risk associated with contralateral prophylactic mastectomy and the effect on adjuvant therapy. Ann Surg Oncol. 2014;21(10):3297–3303. [DOI] [PubMed] [Google Scholar]
- 7.Dave R, O’Connell R, Rattay T, et al. The iBRA-2 (immediate breast reconstruction and adjuvant therapy audit) study: protocol for a prospective national multicentre cohort study to evaluate the impact of immediate breast reconstruction on the delivery of adjuvant therapy. BMJ Open. 2016;6(10):e012678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.J SC, Roddy E, Panighetti A, et al. Comparing Coordinated Versus Sequential Salpingo-Oophorectomy for BRCA1 and BRCA2 Mutation Carriers With Breast Cancer. Clinical breast cancer. 2016;16(6):494–499. [DOI] [PubMed] [Google Scholar]
- 9.Batista LI, Lu KH, Beahm EK, Arun BK, Bodurka DC, Meric-Bernstam F. Coordinated prophylactic surgical management for women with hereditary breast-ovarian cancer syndrome. BMC Cancer. 2008;8:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Del Corral GA, Wes AM, Fischer JP, Serletti JM, Wu LC. Outcomes and Cost Analysis in High-Risk Patients Undergoing Simultaneous Free Flap Breast Reconstruction and Gynecologic Procedures. Annals of plastic surgery. 2015;75(5):534–538. [DOI] [PubMed] [Google Scholar]
- 11.Lyle B, Landercasper J, Johnson JM, et al. Is the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator applicable for breast cancer patients undergoing breast-conserving surgery? Am J Surg. 2016;211(4):820–823. [DOI] [PubMed] [Google Scholar]
- 12.Pyfer B, Chatterjee A, Chen L, et al. Early Postoperative Outcomes in Breast Conservation Surgery Versus Simple Mastectomy with Implant Reconstruction: A NSQIP Analysis of 11,645 Patients. Ann Surg Oncol. 2016;23(1):92–98. [DOI] [PubMed] [Google Scholar]
- 13.Willsher P, Ali A, Jackson L. Laparoscopic oophorectomy in the management of breast disease. ANZ J Surg. 2008;78(8):670–672. [DOI] [PubMed] [Google Scholar]