Abstract
This study has been conducted in an effort to establish metabolic and inflammatory responses of the myocardium during aortic valve surgery on the beating heart with CPB and continuous coronary sinus perfusion with normothermic blood. Twenty patients, divided into two groups, participated in this study. Conventional aortic valvular operations were performed on first 10 patients, while the second group, consisting of 10 patients as well, was subjected to the operations with CPB on the beating heart with continuously perfusion with blood through coronary sinus. There were total of 14 biological and 6 mechanical valves implanted in aortic position. In this study, cardiac markers and inflammatory mediators IL8 and TNF, were measured preoperatively and postoperatively. Metabolic changes were documented based on the levels of CK-MB, Troponin I, Mioglobin and LDH. Inflammatory factors we measured through IL-8 and TNF. All measurements were taken in 6 hour intervals during the initial 48 hours following the operations. The patients of “the beating heart” group had significantly lower dose of markers and cytokines in comparison to those who had undergone the conventional valvular operation (1). The elimination of the adverse effects of global ischemia produced from reperfusion injury and the similarity to the physiological condition, suggests that the revival of the beating heart procedure is more reasonable. This procedure of valvular surgery on the beating heart can be one of the good surgical options for the high-risk valvular patients (2),
Keywords: inflammatory and metabolic response, beating heart surgery, aortic valve surgery
INTRODUCTION
Does myocardial perfusion with warm blood or some another cardioplegic solution carry the same risk as similar perfusion with just warm blood without arresting cardiac function? There is some evidence that continuous warm blood perfusion offers good myocardial protection. First successful operation on the aortic valve, using continuous retrograde perfusion on the beating heart through catheter placed in the coronary sinus, was performed by Lillehei and his colleagues in 1956 (3). As we know, after aortic declamping some general reperfiision occurs resulting in adequate inflammatory response at the same time. This inflammatory response depresses cardiac function and the activation of neutro-philes, which represents the main problem, reperfusion injury, for it allows cytokines to exert direct negative inotropic effects on the heart (4, 5). This method can be one of the approaches for aortic valve patients because it prevents reperfusion injury and prevents myocardial ischemia while it provides the heart with more physiologic condition for duration of operation. This can be useful method for high-risk valvular patients (6).
PATIENTS AND METHODOLOGY
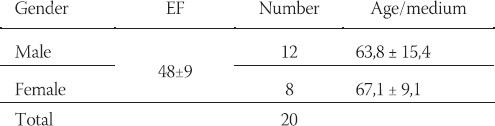
A number of 20 patients had participated in this study and they were divided in two groups. In the first group, with 10 patients, we performed conventional aortic valve replacements and in the second group of 10 patients we performed beating heart procedures with continuous warm blood perfusion through coronary sinus. All operations were done in the department for Cardiac surgery of Hospital “G. Pasquinucci” Massa – Italy. All patients had routine preoperative and postoperative checking for all significant parameters for this study. We replaced aortic valves with biological prosthesis (Carpentier-Edwards and Mitro-flow) or with mechanical prosthesis-(Carbomedics) Operations were performed in 20 patients (12 male age/medium 63,8±15,4 and 8 female age/medium 67,1 ± 9,1) (Graph 1). All patients preoperatively were classified as NYHA functional class III-IV and mean left ventricular ejection fraction 48±9 (Table 1).
GRAPH 1.
Distribution by gender
TABLE 1.
NYHA and demographic data
SURGICAL PROCEDURE
Conventional median sternotomy approach was performed on all patients. Before CPB each patient was administrated 300U/kg of heparin and all operations were performed in normothermia. After successful induction in CPB we placed coronary sinus cannula through right atrium without opening and previous inspection of the coronary sinus. We tried to place cannula in position where balloon of the cannula is positioned just under the orifice of the coronary sinus because we tried to prevent malperfiision of the right coronary vein. The same catheter we fixed with tourniquet and another stitch, which we put through the right atrium wall over the cannula with two big pledges. After that the perfusion cannula line was connected to the CPB oxygenated blood perfusion line. All patients have been left with ventricular venting. After cross clamping of aorta, we started with one dose of cardioplegic solution and we spent only few minutes for valve inspection, in order to avoid possible unexpected problems. After that we started with continuous normothermic blood perfusion through coronary sinus. The entire time of operations coronary sinus flow was maintained at more than 300 ml/min with intracoronary sinus pressure of approximately 55 to 60 mm Hg. Substitution of aortic valve was performed under good visual conditions which was supported with normal coronary sucker during the procedure. All valves were replaced in accord with standard techniques of our hospital. After closure of aortic wall, cannula was removed and we started to wean the patient from the CPB. The first blood sample was taken from the coronary sinus cannula immediately after decan-nulation. The second sample was taken from coronary ostium before closure of aorta. Finally peripheral venous samples were obtained in the intensive care units every 4 hours. Transoesophageal echocardiography was routinely performed on all patients, preoperatively and postoperatively, for significant changes in parameters.
RESULTS
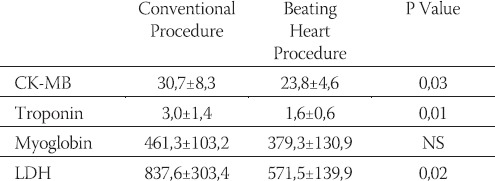
This study has been conducted in the time period between December 2001 and December 2003, and it included 20 patients all of which underwent isolated aortic valve replacement. Intraoperatively, the visual on the retrograded coronary sinus perfusion was just as good as the operative field itself. All operations were performed without any difficulty. Mean retrograde flow was 300-350 ml/min at a coronary sinus pressure of 50-55 mm/Hg. There were no differences in total cardiopulmonary bypass time and aortic clamping time between two groups of patients (Table 2). All patients were hemodinamically stable with no need for inotropic support. There was not any postoperative deterioration of organ functions. For metabolic changes we controlled levels of CK-MB, Tro-ponin I, Mioglobin and LDH. All measurements were performed every 3 hours after the operation. Among patients in beating heart group CK-MB concentration were within normal limit (238±4,6) and were significantly lower than those of conventional valvular operations (30,7±8,3) P-value 0,03. The level of troponin was also lower in group of the beating heart surgery than those in conventional approach. The same differences were with LDH concentrations and lactates. Lactate release during reperfusion was found to be multivariable predictor of low cardiac output syndrome. Other authors, such as the ones from Center for Cardiovascular research in Toronto, Ontario Canada, believe that myocardial lactate release during reperfusion is sign of inadequate myocardial protection during cardioplegic arrest. All of these results we can see in Table 3.
TABLE 2.
CPB Cardiopulmonary bypasss; NS non significant
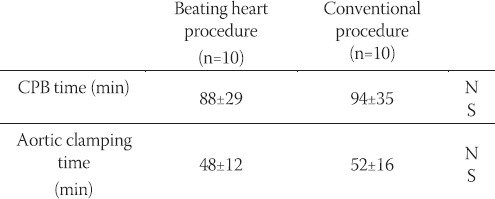
TABLE 3.
Cardiac markers
INFLAMMATORY MEDIATORS
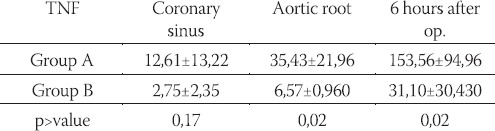
In the given study we controlled level of significant cytokines IL-8 and TNF. All of them were significantly lower in the beating heart group than in conventional group as it shown in Table 4-a and Table 4-b. Measurement tests were performed with EASIA TEST-(Biosource Europe S.A-Belgium). On each patient right ventricular function was assessed by transesophageal echocar-diography and we did not find any pathological changes. There was no operative mortality and no occurrence of major complications such as low output syndrome, bleeding requiring reexploration, cerebral infarction, perioperative myocardial infarction and mediastinitis.
TABLE 4-a.
IL8-level among tested patients
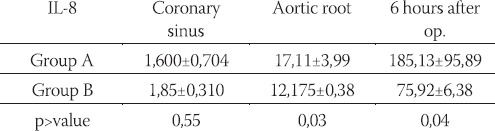
TABLE 4-b.
TNF level among tested patients
DISCUSSION
The opinion that the most hold is that continuous warm blood cardioplegia is the best form of myocardial protection because it keeps the heart in an aerobic state but some degree of postoperative myocardial stunning still occurs (7, 8, 9). Cardiac dysfunction may be caused by myocardial oedema intrinsic to the diastolic state of the arrested heart and every cardioplegic arrest technique will inevitably produce some degree of reperfusion injury (10, 11, 12). In contrast, keeping the heart beat results in less myocardial edema and better cardiac function. To perform beating heart valvular operations we adopted a procedure in which oxygenated blood is supplied to the heart in a retrograde fashion through the coronary venous system from the coronary ostium. Oxygenated blood is perfused from the coronary sinus and flows through the coronary venous system, capillaries and arterial system just as retrograde blood cardioplegia. This study shows that postoperative levels of creatinine kinase MB, troponin and LDH are significantly lower in beating heart group. Consistent with these results, the present findings indicate that the maintenance of a heart in a beating state, throughout the operation, results in less damage than cardioplegic arrest. One of the most important things is that retrograde coronary sinus perfusion maintained myocardial SO2 at levels almost identical to preoperative physiologic values as we can see in the study by dr. Matusumato and coll.(Kanazawa University of Medicine – Japan -2002). Despite the motion of the heart, the on – pump and well decompressed state of the heart caused by cardiac venting resulted in fair quality of visual field equal to that of conventional valvular operation. The advantages of retrograde coronary sinus perfusion include avoidance of injury and postcannulation ostial stenosis of the coronary arteries; performance of valve surgery procedures without interruption; a long period of continuous oxygenated blood delivery which maintains beating of the heart and appropriate pH, and allows effective delivery of substrates or drugs and removal of acid metabolites and more uniform oxygenated blood distribution in the presence of coronary artery stenosis or obstruction. The optimal level of retrograde coronary sinus perfusion flow is unknown to date. As previously mentioned, our flow was maintained at 300 ml/min to avoid adverse effects of hypoperfusion. Since patients with a hypertrophied heart require high flow rates of retrograde perfusion for adequate myocardial protection, it was, thus, necessary to use high pressures during retrograde coronary sinus perfusion. The optimal safe perfusion pressure during retrograde coronary sinus perfusion is closely related to coronary sinus flow. Among our patients there was no failure of coronary sinus perfusion. However, if myocardial malperfusion is suspected, it may be better to use antegrade infusion of cardiopegia. The most important points of this procedure are to maintain high coronary sinus perfusion flow rate and to keep adequate venting. Of course, the sample of patients in our study was not numerous enough for drawing a conclusive statement. The reasons for such a small pool of patients included in this study are mainly due to the high expenses related to the procedures for measurement of inflammatory factors.
CONCLUSION
The obtained results indicate that an on pump beating heart valvular operation is a sound surgical alternative for valvular disease. The advantages of this procedure include: avoidance of injury and postcannulation ostial stenosis of the coronary arteries, performance of surgical procedure without interruption, a long period of continuous oxygenated blood delivery in addition to the fact that the heart itself can then function in conditions more closely related to its natural, physiologic conditions, than is the case in operations involving cardioplegic arrest (with left ventricular beating tonus). Furthermore, implementation of this procedure ensures elimination of adverse effects of global myocardial ischemia produced from reperfiision injury which are all good reasons to revive this surgical alternative. However, the efficiency of this procedure requires further study and more thorough comparison with cardioplegic arrest method. In any case, this procedure should be considered as one of the most appropriate ones when it comes to the highrisk valvular patients.
REFERENCES
- 1.Biagoli B, Giomarelli P, Gnudi G, et al. Myocardial function in early hours after coronary artery bypass grafting: comparison of two cardioplegic methods. Ann. Thorac. Surg. 1993;56:1315–1323. doi: 10.1016/0003-4975(93)90672-5. [DOI] [PubMed] [Google Scholar]
- 2.Fremes SE, Weisel RD, Mickle DAG, Ivanov VJ, Madonik MM, Seawright SJ, Houle S, Mc Laughlin PR, Baird RJ. Myocardial metabolism and ventricular function following cold potassium cardople-gia. J. Thorac. Cardiovasc. Surg. 1985;8:531–546. [PubMed] [Google Scholar]
- 3.Calafiore AM, Teodori G, Mezzeti M, Bosco G, Verna AM, Di Gianamarco G, Lapenna D. Intermittent antegrade warm blood cardioplegia Ann. Thorac. Surg. 1995;59:398–402. doi: 10.1016/0003-4975(94)00843-v. [DOI] [PubMed] [Google Scholar]
- 4.Hansen Pr. Role of neutrophils in myocardial ischemia and reperfu-sion. Circulation. 1995;91:1872–1885. doi: 10.1161/01.cir.91.6.1872. [DOI] [PubMed] [Google Scholar]
- 5.Crawford MH, Grover FL, Kolb WP, et al. Complement and neutrophil activation in the pathogenesis of ischemic myocardial injury. Circulation. 1988;78:1449–1458. doi: 10.1161/01.cir.78.6.1449. [DOI] [PubMed] [Google Scholar]
- 6.Flack JE, III, Cook JR, May SJ, Lemeshow S, Engleman RM, Rosou JA, Deaton DW. Does cardioplegia type affect outcome and survival in patients with advanced left ventricular disfunction? Results from the CABG Patch Trial. doi: 10.1161/01.cir.102.suppl_3.iii-84. [DOI] [PubMed] [Google Scholar]
- 7.Hayashida N, Weisel RD, Shirai T, Ikonomidis JS, Ivanov J, Carson SM, Mohabeer MK, Tumiati LC, Mickle DA. Tepid antegrade and retrograde cardioplegia, Ann. Thorac. Surg. 1995;59:723–729. doi: 10.1016/0003-4975(94)01056-0. [DOI] [PubMed] [Google Scholar]
- 8.Bessho R, Chambers DJ. Myocardial protection with oxigenated esmolol cardioplegia during prolonged normothermic ischemia in the rat. J. Thorac. Cardiovasc. Surg. 2002;124:340–345. doi: 10.1067/mtc.2002.121976. [DOI] [PubMed] [Google Scholar]
- 9.Dagenais F, Pelleteir LC, Carrier M. Antegrade/retrograde cardoplegia for valve replacement: a prospective study. Ann. Thorac. Surg. 1999;68:1681–1685. doi: 10.1016/s0003-4975(99)00837-1. [DOI] [PubMed] [Google Scholar]
- 10.Menasché P, Subayi J.-B, Piwnica A. Retrograde coronary sinus cardioplegia for aortic valve operations: clinical report in 500 patients. Ann. Thorac. Surg. 1995;49:556–556. doi: 10.1016/0003-4975(90)90301-l. [DOI] [PubMed] [Google Scholar]
- 11.Edi LJ, Goeddel DV, Wong GHW. Tumor necrosis factor a-pretreat-ment is protective in a rat model of myocardial ischemia-reperfusion injury. Biochem. Biophys. Res. Commun. 1992;184:1056–1059. doi: 10.1016/0006-291x(92)90698-k. [DOI] [PubMed] [Google Scholar]
- 12.Frangogiannis NG, Lindsey ML, Michael LH, et al. Resident cardiac mast cells degranulate and release preformed TNF-a initiating the cytokine cascade in experimental canine myocardial ischemia/re-perfusion. Circulation. 1988;98:699–710. doi: 10.1161/01.cir.98.7.699. [DOI] [PubMed] [Google Scholar]


