Abstract
Brucellosis is primarily an animal disease, and in them it passes as an asymptomatic chronic infection. In humans, brucellosis can be acute, subacute and/or chronic disease, but its geographical distribution follows the pattern found in animals. After the last war, the first Brucella cases in Bosnia and Herzegovina were reported in 2000, in returnees, owners of donated livestock. The objective of this paper was to address an increased public health problem regarding brucellosis in Bosnia and Herzegovina and to initiate better cooperation among epidemiologists, veterinarians, microbiologists and infectologists and responsible authorities toward elimination and eradication of this severe disease. Retrospective analysis of Brucella case histories and treatment protocols of all the cases hospitalized in Clinic for Infectious Diseases, University of Sarajevo Clinics Center (CCUS) was conducted. All the patients hospitalized between 1 January 2000 and 1 July 2005 were included. The diagnoses were confirmed by laboratory tests, chemo culture or serologically. The Rose Bengal agglutination and ELISA tests were used as laboratory confirmation methods. The number of hospitalized cases over the last 5 years was compared with total number of reported cases in the first 6 months of 2005. The results of this study showed that Brucella infections in humans, compared to other zoonoses, was represented with 11,8%. Brucellosis was the second zoonose in a ranking of zoonotic diseases cases with steady increase in the number of reported cases each year. The number of cases treated in the first 6 months of 2005 already exceeded half of the total number of cases treated in the last 5 years. Human brucellosis is an increasing public health problem in Bosnia and Herzegovina, and it reflects spreading of the same disease in animals. The applied prevention measures have been insufficient, so it is necessary to mobilize all the available resources of human and veterinary medicine, as well as the authorities, microbiological laboratory diagnostics in order to identify foci of epidemics and to try to eliminate and eradicate this complicated disease.
INTRODUCTION
Brucellosis is an anthropozoonoses which, in animals may pass as asymptomatic chronic infection, while in humans, it may result in acute, subacute or chronic disease, mainly with clear clinical signs and symptoms (1). It is a bacterial disease, caused by a Gram negative facultative intracellular cocco-bacillus from Brucella genus, 4 species of which are pathogenic in humans. It can be transmitted to humans through direct contact, or by consumption of un-pasteurized milk and cheese harvested from an infected animal (2). Airborne infections may occur by inhalation of infectious aerosol in laboratories and abattoirs (3, 4). Therefore, brucellosis is most frequently occupational disease among farmers, butchers, veterinarians, veterinary technicians and laboratory workers (5). Brucella bacteria have affinity toward all organs where they cause granulomatosus inflammation. The disease starts either as unclear prolonged febrile condition with possible lymphade-nopathy, or moderate hepatic and spleen enlargement (hepatosplenomegaly) (4). The signs and symptoms associated with brucellosis are protean in nature and no constellation of clinical findings can be considered characteristic (4). After 4-6 weeks the disease localizes in certain organs and may appear as pulmonary brucellosis (pneumonitis, emphysema and pleural effusions); granulomatous hepatitis; osteoarticular brucellosis; genitourinary brucellosis; endocarditis; central nervous system brucellosis (meningitis, radiculopathy, optical neuropathies, intracerebral hemorrhages…); abscess formation in liver, spleen, thyroid gland and other organs (6,7,8,9,10,11,12). Diagnosis is confirmed by positive chemo cultures (blood cultures) in 80% of cases; and serologically by: agglutination method (Agl), complement binding (RVK), Rose Bengal agglutination, ELISA and finally by PCR. ELISA is less significant then other diagnostic tests but it can be very helpful while waiting for blood culture results. PCR results positive in 75% of the cases, and combined with ELISA can by highly sensitive. Brucella could be highly important as a bioterroristic agent. The objective of this study was to explore whether brucellosis presented an increasing health problem in Bosnia and Herzegovina over the last five years and to initiate better cooperation among epidemiologists, veterinarians, microbiologists and infectologists and the responsible authorities toward elimination and eradication of this severe disease.
PATIENTS AND METHODS
A retrospective study of records of patients treated at the Clinic for Infectious diseases, University of Sarajevo Clinics Center between 1 January 2000 and 1 July 2005 was conducted. Simultaneously, we performed an analysis of annual reports on brucellosis patients treated on the territory of Bosnia and Herzegovina. The disease diagnosis in all cases was confirmed either by isolation of causative agent or serologically – tests used were Rose Bengal test of agglutination and ELISA. In our study we observed ethical principles outlined in World Medical Association Declaration of Helsinki.
RESULTS
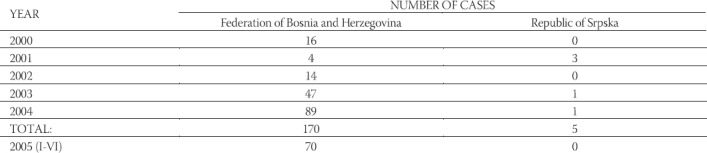
The first case of brucellosis was hospitalized in our Clinic in 2000. That very same year there was a report of five new hospitalized cases among our patients. As it is shown in Table 1, over the next 5 years the number patients hospitalized due to brucellosis in our Clinic only, progressively increased. From 2000 until the end of 2004 the cumulative number of reported patients was 85. Gender structure of those patients was: 20 female, 64 male and one preschool child. The average age of patients was 40,6 years of life (range from 9,5 to 67). Most of the cases were between 25 and 45 years. Most commonly they were workers, then school children and housewives (Table 2). Out of 85 patients 13 had osteoarticular complications of the disease, five had epididymitis, three had endocarditis, and one patient had neurobrucellosis. As it is shown in Table 3, most of the patients were from Sara jevo, Central Bosnia and Herzegovina-Neretva Canton. During the first half (January-June) of 2005 a total number of patients hospitalized at Infectious diseases Clinic, CCUS was 44, plus one case treated in outpatient department with the approval and consultation of hospital. One of the cases was 6-years old girl from Cazin, Una Sana Canton; one patient was from Sanski Most (the same Canton), two were from Hadzici (Sarajevo Canton); and all the others were from Bugojno and its surroundings (Central Bosnia Canton). Number of Brucella cases in the Federation of Bosnia and Herzegovina starting in 2000 (taken as the Index year) shows almost geometrical progression in the last two years as it is shown in Table 4. A total of 170 cases were reported in 5 years period. In Republic of Srpska (RS) only 5 cases were reported over the same period. Three of those were treated in 2003.
TABLE 1.
Number of hospitalized brucellosis patients according to age and sex and year of hospitalization
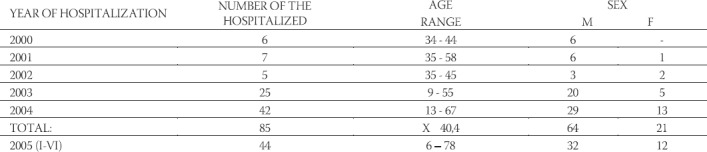
TABLE 2.
Distribution of patients according to their profession
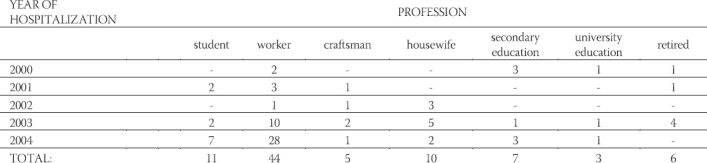
TABLE 3.
Geographical distribution of patents (by Cantons)
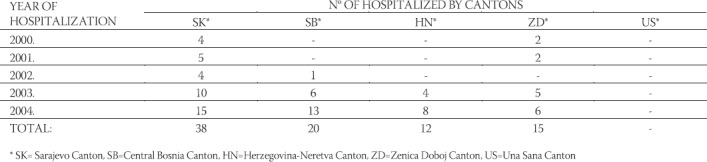
TABLE 4.
Human Brucella cases in Bosnia and Herzegovina over the last five and a half years
DISCUSSION
Brucellosis has proven to be a great public health issue wherever it is present due to the two main reasons: it damages livestock and causes human illness. Long-term treatment, severe complications and sequelas influencing life quality demand an increase in mobilized material resources and costs, and burden national income (13,14,15,16,17,18,19). Until the recent War (1992-95) Bosnia and Herzegovina was considered brucellosis free country. Only one outbreak was reported on Manjača Mountain, in a military training camp (Vojni poligon) in 1985. It was proven that Brucella was imported from Israel via Macedonia and Serbia. This outbreak was localized to 40-sh cases only, soldiers and cattle handlers who worked at the farm. The outbreak was quickly and successfully placed under control. Some cases were treated at the Infectious diseases Clinic in Banjaluka, while over 30 cases were hospitalized at the Military Medical Academy in Belgrade. All the infected cattle were slaughtered. After the recent War, brucellosis occurred in the areas in Bosnia and Herzegovina where the cattle was donated to refugeesreturnees and displaced persons. In the total number of patients treated for zoo-noses, brucellosis participates with 11,8 %, and it is the second ranking zoonoses over the last 5 years (20). As our results show, since the index case reported in spring 2000, number of brucellosis cases has increased from one year to another. According to our results, number of patients hospitalized in the first 6 months of 2005 amount to half of the total number of cases registered as hospitalized since 2000. That shows that the disease significantly spread among livestock. It is an alarming fact that shows that the undertaken measures in control of the disease among livestock were neither systematic nor radical, but palliative, partial, and very limited in effects. This is quite concerning as this agent is very persistent in environment and once infected, soil remains a source of infection for live stock as well as for humans for quite some time, despite the fact that sometimes, infected herd could be eliminated months earlier. On the other hand, 21% of all our Brucella treated patients over this 5-year period had osteoarticular manifestation of Brucellosis with severe forms of spondilodiscitis and cox-athrosis. Their medication treatment was extended to 12 and 24 weeks with constant outpatient controls. That burdens health budget and the country budget in general. Comparing to 69% of the described cases in 1995, by Gur A et al, the number of osteo-articular manifestations among our patients is three times lower (19). The same authors describe 17% of dermal lesions, which we have not found among our patients, and 8% of genitourinary and 7% of neurological complications. Our Brucella patients of generative age developed orchiepididymitis in 5,9 % of them. The issue of their consecutive sterility remains open. Only one patient had neurobrucellosis (1,2%), a veterinarian, 56 years old, who had osteoarticu-lar, central nervous and liver complications. Sub-acute endocarditis was found in 1,2% (1 case out of 85 total until the end of 2004). The heart vitium was so developed that aortal valves had to be implanted. The patients life quality was drastically changed, as he remained life-long invalid with necessary long-term treatment and permanent controls by cardiologists, infectologists and cardio-sugeons, with possibility of receives. During the first six months of this year, two of the total of 44 patients developed subacute endocarditis. When compared with previous year’s findings that number is found significant. Every other of our treated patients had liver lesion, meaning that one third of our patients developed liver complications. Reviewing literature, it is possible to find different hematological complications described during brucellosis, such as bone marrow aplasia, extreme thrombocytopenia and erythropenia, individually or together with other complications, which we did not find in our patients (18, 19, 22). Analyzing Table 4 it is clearly visible that after index 2000 year when 16 Brucella cases were registered, the number of reported cases was in decline for couple of years. So, in 2001 only 4 cases were reported in Federation of Bosnia and Herzegovina, and 2002 slightly more – 14 cases. Starting 2003 further progressive increase of brucellosis among humans is evident. We assume that the main reasons for that are bad diagnostics and failure to recognize the disease in primary health care setting and, on the other hand, broad application of kinolone combined with cephalo-sporines 3rd generation and amino-glycosides. Unusual distribution of the disease in different Bosnia and Heze-govina areas (which was after the 1992-95 war politically divided in two entities) remains a question for epidemiologists to answer and explain. It is more important to bear in mind that brucellosis is an antropozoonoses very suitable for bioterrorism and biological war. Due to the severity of the disease among humans, treatment length as well as consequences of sub-acute and chronic forms, it is our opinion that it is necessary to engage all the available resources at the national level in order to identify foci of brucellosis in animals and interrupt ways of transmissions in order to eliminate this zooanthroponoses. Only more radical approach to prevention and elimination (furthermore eradication) of brucellosis can prevent further spreading of a disease. That means early detection of this disease in both animals and humans, good laboratory diagnostics of the disease, reporting of each suspicious case, mobilization of all the available resources of epidemiological departments and veterinary medicine, farmers education, education of population, participation of the adequate state-level organizations due to programs planning and financial resources for the termination of the infection agents and interruption of its biological chain. All of this should entail the scientific sphere of human and animal medicine on one side, and governmental structures on the other side and it can lead to the establishment and observance of the adequate legislation.
CONCLUSION
Human brucellosis is an actual and increasing public health problem in Bosnia and Herzegovina.
Most common cases are workers, age 25-45 years of life.
Men are almost three times more frequently affected then women.
Disease spreading points at the ow level of prevention measures and insufficiency in national (state) eradication program.
Better cooperation among epidemiologists, veterinarians, infectologists, microbiologists and public health professionals is necessary in order to identify epidemic foci and try to eradicate this disease.
REFERENCES
- 1.Godfroid J, Cloeckaert A, Liautard JP, Kohler S, Fretin D, Walravens K, Garin-Bastuji B, Letesson JJ. From the discovery of the Malta fever’s agent to the discovery of a marine mammal reservoir, brucellosis has continuously been a re-emerging zoonosis. Vet. Res. 2005;36(3):313–326. doi: 10.1051/vetres:2005003. [DOI] [PubMed] [Google Scholar]
- 2.Husseini AS, Ramlawi AM. Brucellosis in the West, Bank Palestine. Saudi Med J. 2004;25(11):1640–1643. [PubMed] [Google Scholar]
- 3.Heymann D.L, editor. APHA. 18th Edition. 2004. Control of Communicable diseases Manual; pp. 75–78. [Google Scholar]
- 4.Young JE. Brucella species. In: Mandell GL, Dolin R, Benett JE, editors. Principles and practice of infectious diseases. New York: Churchill Livingstone; 1995. pp. 2053–2057. [Google Scholar]
- 5.Robichaud S, Libman M, Behr M, Rubin E. Prevention of laboratory-acquired brucellosis. Clin. Infect. Dis. 2004;38(12):e119–e122. doi: 10.1086/421024. [DOI] [PubMed] [Google Scholar]
- 6.Mantur BG, Akki AS, Mangalgi SS, Patil SV, Gobbur RH, Peerapur BV. Childhood brucellosis-a microbiological, epide-miological and clinical study. J Trop Pediatr. 2004;50(3):153–157. doi: 10.1093/tropej/50.3.153. [DOI] [PubMed] [Google Scholar]
- 7.Hatipoglu CA, Yetkin A, Ertem GT, Tulek N. Unusual clinical presentations of brucellosis. Scand J.Infect Dis. 2004;36(9):694–697. doi: 10.1080/00365540410017554. [DOI] [PubMed] [Google Scholar]
- 8.Tunc M, Durukan H. Bilateral several visual loss in brucellosis. Occul. Immunol. Inflamm. 2004;12(3):233–236. doi: 10.1080/092739490500183. [DOI] [PubMed] [Google Scholar]
- 9.Taliani G, Bartoloni A, Tozzi A, Bartalesi F, Corti G, Paradisi F. Lumbar pain in a married couple who likes cheese: Brucella strikes again. Clin Exp Rheumatol. 2004;22(4):477–480. [PubMed] [Google Scholar]
- 10.Wortmann G. Pulmonary manifestations of other agents: bru-cella, Q-fever, tularemia and smallpox. Respir. Care Clin. N. Am. 2004;10(1):99–109. doi: 10.1016/S1078-5337(03)00052-2. [DOI] [PubMed] [Google Scholar]
- 11.Kalaycioglu S, Imren Y, Erer D, Zor H, Arman D. Brucella endocarditis with repeated mitral valve replacement. J. Card. Surg. 2005;20(2):189–192. doi: 10.1111/j.0886-0440.2005.200428.x. [DOI] [PubMed] [Google Scholar]
- 12.Ozden M, Demirdag K, Kalkn a, Ozdemir H, Yuce P. A case of brucella spondylodiscitis with extended, multiple-level involvement. South Med. J. 2005;98(2):229–231. doi: 10.1097/01.SMJ.0000152755.07937.60. [DOI] [PubMed] [Google Scholar]
- 13.Seidel G, Pardo CA, Newman-Toker D, Olivi A, Eberhart CG. Neurobrucellosis presenting as leucoencephalopathy: the role of cytotoxic T lymphocytes. Arch Pathol Lab Med. 2003;127(9):e374–e377. doi: 10.5858/2003-127-e374-NPALTR. [DOI] [PubMed] [Google Scholar]
- 14.Cesur S, Ciftci A, Sozen TH, Tekeli E. A case of epididymo-or-chitis and paravertebral abscess due to brucellosis. J. Infect. 2003;46(4):251–253. doi: 10.1053/jinf.2002.1121. [DOI] [PubMed] [Google Scholar]
- 15.Hesseling AC, Marais BJ, Cotton MF. A child with neurobru-cellosis. Ann. Trop. Paediatr. 2003;23(2):145–148. doi: 10.1179/027249303235002224. [DOI] [PubMed] [Google Scholar]
- 16.Namiduru M, Karaoglan I, Gursoy S, Bayazit N, Sirikci A. Brucellosis of the spine: evaluation of the clinical, laboratory, and radiological findings of 14 patients. Rheumathol. Int. 2004;24(3):125–129. doi: 10.1007/s00296-003-0339-7. [DOI] [PubMed] [Google Scholar]
- 17.Almuneef M, Memish ZA, Al Shaalan M, Al Banyan E, Al-ALOLA S, Balkhy HH. Brucella melitensis bacteremia in children: review of 62 cases. J. Chemother. 2003;15(1):76–80. doi: 10.1179/joc.2003.15.1.76. [DOI] [PubMed] [Google Scholar]
- 18.Yildirmak Y, Palanduz A, Telhan L, Arapoglu M, Kayaalp N. Bone marrow hypoplasia during Brucella infection. J. Pediatr. Hematol. Oncol. 2003;25(1):63–64. doi: 10.1097/00043426-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Gur A, Geyik MF, Dikici B, Nas K, Cevik R, Sarac J, Hosoglu S. Complications of brucellosis in different age groups: a study of 283 cases in southeastern Anatolia of Turkey. Yonsei Med J. 2003;44(1):33–44. doi: 10.3349/ymj.2003.44.1.33. [DOI] [PubMed] [Google Scholar]
- 20.Dautović-Krkić S, Lukovac E, Mostarac N, Hadžović M, Gazi-bera B, Muratović P. Zoonosis in infectious practica. Prvi sim-pozijum o zoonozama sa međunar. učešć. 2005:88. [Google Scholar]
- 21.Sevinc A, Buyukberber N, Camci C, Buyukberber S, Karlsligil T. Thrombocytopenia in brucellosis: case report and literature review. J. Natl. Med. Assoc. 2005;97(2):290–293. [PMC free article] [PubMed] [Google Scholar]


