Abstract
Objective
It is important to know the epidemiologic aspects of traumatic brain injury (TBI) for its rapid detection, appropriate treatment, and prevention. The purpose of this study is to classify the time of arrival of patients in the emergency room (ER) by time of day, day of the week, month, and season, and to analyze the relationship between the frequency of presentation at different times and TBI.
Methods
The time of arrival of 327 patients with TBI between January 2016 to December 2017 at the ER was analyzed retrospectively. The trends regarding the frequency of presentation of patients with TBI were analyzed in relation to arrival time at the ER.
Results
Patients with TBI were found to have the greatest number of hospitalizations at 13:00–18:00, on Saturdays, in December, and during the summer. Surgical treatment was not related to the temporal pattern of TBI patient admission. Patients with TBI in the severe group (GCS score <8) arrived at the ER mainly at 07:00–12:00 (p=0.015). Patients with TBI in the mild group (GCS score 13–15) mainly presented in the ER during the summer (p=0.003), while patients TBI in the moderate group (GCS score 9–12) presented mainly in the winter (p=0.244). The combination of the mild and moderate group presented more often in the winter (p=0.014).
Conclusion
It is worthwhile understanding the temporal trends of TBI patients. These data may provide useful information in predicting the ER visits of TBI patients in advance and preparing for prompt and appropriate treatment.
Keywords: Epidemiology, Traumatic brain injury, Emergency room
INTRODUCTION
When some diseases were studied, several unique trends were discovered, such as trends related to sex, peak age, and time of day. Typical diseases showing a time-related trend in the neurosurgical department include aneurysmal subarachnoid hemorrhage (SAH).4) This disease has seasonal or diurnal trends where they are especially prevalent in the early morning or winter, although some retrospective studies revealed no seasonal or monthly time-related effect in the incidence of SAH.4,7) According to some retrospective studies of patients with traumatic brain injury (TBI), male sex, traffic accidents, and winter season were the main effects increasing incidence of TBI.13) However, there are few studies considering the time-related trends of TBI. It is important to know the epidemiologic aspects of TBI to allow rapid appropriate treatment and prevention of TBI.3) The purpose of this study is to investigate the time of arrival of patients in the emergency room (ER) by time (hour, day, month, and season), and to evaluate the relationship between the time trend and the severity of TBI.
MATERIALS AND METHODS
Data were collected from 327 patients with TBI who were admitted to the Neurosurgical Department through the ER and the time of arrival of patients in the ER was analyzed. Data were retrospectively reviewed from the medical records of patients admitted for TBI from January 2016 to December 2017. All patients confirmed to have TBI based on a CT scan performed in the ER were included in the study. Exclusion criteria were severe extra-cranial injury, chronic subdural hematoma, and cerebral concussion. The study was approved by the Institute Ethical Committee of Wonkwang University Hospital (WKUH) and in compliance with institute's requirements (WKUH 201907028). The demographic characteristics of patients with TBI, including sex, age distribution, cause of injury, diagnosis, Glasgow Coma Scale (GCS) score at admission, and surgical vs. nonsurgical treatment were investigated. Diagnoses included skull fracture alone, acute epidural hematoma (A-EDH), acute subdural hematoma (A-SDH), traumatic subarachnoid hemorrhage (T-SAH), traumatic intracranial hemorrhage (T-ICH), and acute epidural and subdural hematoma (A-ESDH). If the patients had a skull fracture and hemorrhage at the same time, they were classified as hemorrhagic patients. The time of arrival in the ER of all patients with TBI was classified according to the time of day, weekday, month of the year, and season. The time of day was divided into four periods, night (00:00 to 06:00), morning (06:00 to 12:00), afternoon (12:00 to 18:00), and evening (18:00 to 00:00). Patients were divided into two groups according to whether they underwent surgery, and each group was compared according to the time, day, month, and season, and differences between groups were statistically analyzed. The author also categorized the patients into one of three groups according to the severity of the trauma using the GCS score: mild (GCS score 13–15 points), moderate (GCS score 9–12 points), or severe (GCS score below 8). These groups identified the characteristics of time trends.
Statistical analyses
SPSS version 22.0 (IBM SPSS Inc., Armonk, NY, USA) was used for statistical analyses. The categorical variables were assessed using Pearson's χ2 and Fisher's exact tests. Differences were considered statistically significant if p-values were <0.05.
RESULTS
Demographic characteristics
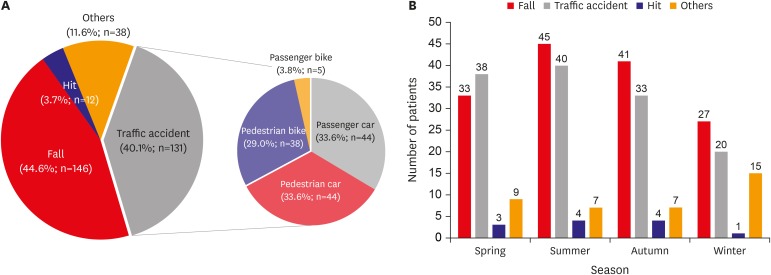
A total of 327 patients with TBI were included in this study. The demographic characteristics of patients are summarized in TABLE 1. The mean patient age was 56.2 years with 238 (72.8%) men and 89 (27.2%) women; the frequency of TBI in men was higher than that in women. The incidence of TBI according to age was highest in those 61–80 years of age (42.2%; n=138), followed by those aged 41–60 years (30.9%; n=101), ≤20 years (10.4%; n=34), 21–40 years (9.8%; n=32), and ≥81 years (6.7%; n=22). The causes of TBI included 146 (44.6%) falls, 131 (40.1%) traffic accidents, 12 (3.7%) hits (direct impact), and 38 (11.6%) others. The hits category is a group of patients whose hard objects (stones, concrete, and rebars, etc.) strike directly on the patient's head. The other category include those who do not know the exact cause of the TBI or have been injured by slipping or other causes. Furthermore, traffic accidents could be divided into 44 (33.6%) passenger car traffic accidents, 44 (33.6%) pedestrian car traffic accidents, 38 (29.0%) passenger bicycle traffic accidents, and five (3.8%) pedestrian bicycle traffic accidents (FIGURE 1A). The number of patients who fell was highest in summer (13.8%; n=45) and lowest in winter (8.3%; n=27). The number of traffic accidents was also highest in summer (12.2%; n=40) and lowest in winter (6.1%; n=20). Although the number of traffic accidents in spring was higher than falls, but the rest of the season had more falls (FIGURE 1B).
TABLE 1. Demographic characteristics of patients with traumatic brain injury.
| Characteristics | Values | ||
|---|---|---|---|
| Sex | |||
| Male | 238 (72.8) | ||
| Female | 89 (27.2) | ||
| Age (years) | |||
| ≤20 | 34 (10.4) | ||
| 21–40 | 32 (9.8) | ||
| 41–60 | 101 (30.9) | ||
| 61–80 | 138 (42.2) | ||
| ≥81 | 22 (6.7) | ||
| Cause of injury | |||
| Fall | 146 (44.6) | ||
| Traffic accident | 131 (40.1) | ||
| Car accident | 87 (66.4) | ||
| Motorcycle accident | 44 (33.6) | ||
| Hits (direct impact) | 12 (3.7) | ||
| Others | 38 (11.6) | ||
| Diagnosis | |||
| Skull fracture alone | 21 (6.4) | ||
| Acute epidural hematoma | 56 (17.1) | ||
| Acute subdural hematoma | 147 (45.0) | ||
| Traumatic subarachnoid hemorrhage | 63 (19.3) | ||
| Traumatic intracranial hemorrhage | 30 (9.2) | ||
| Acute epidural and subdural hematoma | 10 (3.1) | ||
| Glasgow Coma Scale score at admission | |||
| 3–8 | 59 (18.1) | ||
| 9–12 | 36 (11.0) | ||
| 13–15 | 232 (70.9) | ||
| Treatment | |||
| Surgical | 102 (31.2) | ||
| Nonsurgical | 225 (68.8) | ||
Values are presented as number of patients (%).
FIGURE 1. The cause of traumatic brain injury (TBI) (A) and seasonal TBI (B).
The most common diagnosis was A-SDH (45.0%; n=147), followed by T-SAH (19.3%; n=63), A-EDH (17.1%; n=56), T-ICH (9.2%; n=30), skull fracture alone (6.4%; n=21), and A-ESDH (3.1%; n=10). There were 232 patients (73.9%) with mild TBI, 36 patients (11.0%) with moderate TBI, and 59 patients (18.1%) with severe TBI, and the mean initial GCS score was 12.7. A total of 102 patients (31.2%) underwent surgical treatment, and 225 patients (68.8%) underwent nonsurgical treatment (TABLE 1).
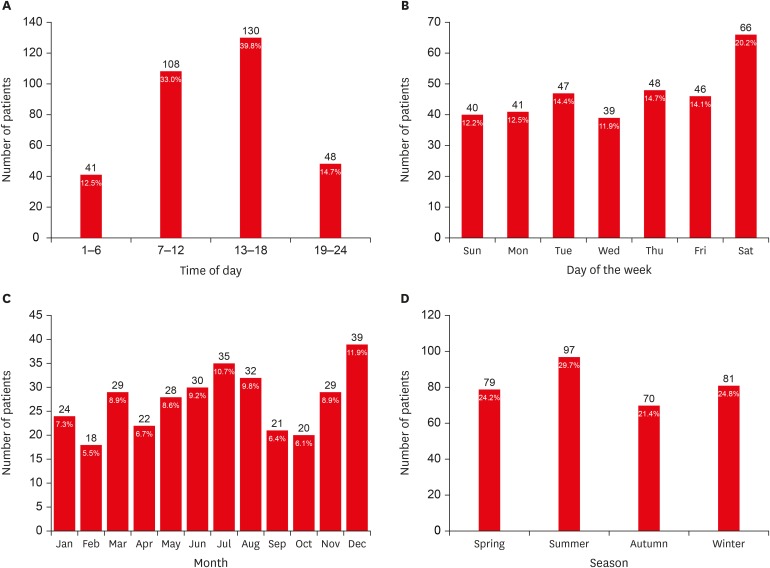
Number of patients with TBI according to the ER visit time
The largest proportion of patients presented at 13:00–18:00 (39.8%; n=130), with the smallest proportion presenting at 00:00–06:00 (12.5%; n=41) (FIGURE 2A). The most common day of presentation was Saturday (20.2%; n=66); however, the number of patients who presented with TBI on days other than Saturday was generally similar (FIGURE 2B). The largest number of presentations was in December (11.9%; n=39) and the lowest number of presentations was in February (5.5%; n=18) (FIGURE 2C). The season with the most presentations was summer (29.7%; n=97) and the season with the fewest presentations was fall (21.4%; n=70) (FIGURE 2D).
FIGURE 2. Number of patients with traumatic brain injury (TBI) according to emergency room visit time. (A) Number of patients with TBI by time of day. (B) Number of patients with TBI by day of the week. (C) Number of patients with TBI by month. (D) Number of patients with TBI by season.
Comparison of ER visit time and surgical and non-surgical treatment groups
We divided patients into surgical and nonsurgical treatment groups, and statistical analyses were performed to determine the relationship between ER visit time and treatment group. Regarding patients in the group that underwent surgery, the largest groups for time of presentation, day of presentation, month of presentation, and season of presentation were 38 (37.2%) patients from 07:00 to 12:00, 19 patients (18.6%) on Friday, 14 (13.7%) in December, and 36 (35.2%) in summer, respectively. Regarding the group that underwent non-surgical treatment, the largest groups for time of presentation, day of presentation, month of presentation, and season of presentation were 94 (41.7%) patients from 13:00 to 18:00, 51 (22.6%) patients on Saturday, 25 (11.1%) patients in May and December, and 65 (28.8%) patients in spring. The differences in ER arrival times according to the time of the day (p=0.429), day of the week (p=0.780), month (p=0.537), and season (p=0.154) between the surgical and non-surgical treatment groups were not statistically significant (TABLE 2).
TABLE 2. Comparison of clinical characteristics between surgical and non-surgical groups.
| Characteristic | Surgery (n=103) | Non-surgery (n=224) | Total | |
|---|---|---|---|---|
| Time of day | ||||
| 01:00–06:00 | 11 (10.7) | 30 (13.4) | 41 (12.5) | |
| 07:00–12:00 | 38 (36.9) | 70 (31.3) | 108 (33.0) | |
| 13:00–18:00 | 36 (35.0) | 94 (42.0) | 130 (39.8) | |
| 19:00–00:00 | 18 (17.4) | 30 (13.4) | 48 (14.7) | |
| Day of the week | ||||
| Sun | 14 (13.6) | 26 (11.6) | 40 (12.2) | |
| Mon | 18 (17.5) | 23 (10.3) | 41 (12.5) | |
| Tue | 16 (15.5) | 31 (13.8) | 47 (14.4) | |
| Wed | 12 (11.7) | 27 (12.1) | 39 (11.9) | |
| Thu | 9 (8.7) | 39 (17.4) | 48 (14.7) | |
| Fri | 19 (18.4) | 27 (12.1) | 46 (14.1) | |
| Sat | 15 (14.6) | 51 (22.8) | 66 (20.2) | |
| Months | ||||
| Jan | 6 (5.8) | 18 (8.0) | 24 (7.3) | |
| Feb | 7 (6.8) | 11 (4.9) | 18 (5.5) | |
| Mar | 8 (7.8) | 21 (9.4) | 29 (8.9) | |
| Apr | 3 (2.9) | 19 (8.5) | 22 (6.7) | |
| May | 6 (5.8) | 25 (11.2) | 28 (8.6) | |
| Jun | 11 (10.7) | 17 (7.6) | 30 (9.2) | |
| Jul | 13 (12.6) | 22 (9.8) | 35 (10.7) | |
| Aug | 12 (11.7) | 18 (8.0) | 32 (9.8) | |
| Sep | 7 (6.8) | 14 (6.3) | 21 (6.4) | |
| Oct | 9 (8.7) | 12 (5.4) | 20 (6.1) | |
| Nov | 7 (6.8) | 22 (9.8) | 29 (8.9) | |
| Dec | 14 (13.6) | 25 (11.2) | 39 (11.9) | |
| Season | ||||
| Spring | 17 (16.5) | 65 (29.0) | 79 (24.2) | |
| Summer | 36 (35.0) | 57 (25.4) | 97 (29.7) | |
| Fall | 23 (22.3) | 48 (21.4) | 70 (21.4) | |
| Winter | 27 (26.2) | 54 (24.1) | 81 (24.8) | |
Values are presented as number of patients (%).
Comparison of ER visit time and GCS score
Patients were divided into 3 groups based on their GCS score: mild, moderate, and severe. Statistical analyses were performed to determine the relationship between ER arrival time and the three groups. There was a statistical significance between the ER arrival times according to the time of day and GCS score (p=0.035). This result suggests that the groups as defined by GCS score arrived at the ER at specific times. Statistical analyses were performed to determine which groups were associated with which times of the day. The mild and moderate groups most frequently presented to the ER at 13:00–18:00 (n=97 and n=15), which was not statistically significant (p=0.289 and p=0.220). The severe group most frequently presented to the ER at 07:00–12:00 (n=29), which was statistically significant (p=0.015). ER arrival times according to the day of the week (p=0.788) and month (p=0.090) was not statistically significant between the three groups. There was also a statistically significant difference in the ER arrival time according to season and GCS score (p=0.005). The mild group had the most frequent visits to the ER in summer (n=76), which was statistically significantly more common (p=0.003). The moderate group and severe group had the most frequent visits to the ER in the winter (n=15 and n=19), which was statistically significantly more common (p=0.003). The severe group had the most frequent visits to the ER in the winter; however, this was not statistically significantly more frequent (p=0.244). However, the combination of the moderate and severe groups most frequently visited the ER in winter (n=34), which was statistically significantly more common (p=0.014).
DISCUSSION
Song et al.10) reported a retrospective review of medical records of 2,617 TBI patients enrolled on the Korean Neuro-Trauma Data Bank System (KNTDBS) website from September 2010 to March 2014. This was a national epidemiological study of The Korean Society of Neurotraumatology involving 20 TBI hospitals in Korea. In their study, 70.8% of patients were male and 29.2% were female. This was similar to the results in the present study (72.8% male patients and 27.2% female patients). Comparing the age groups, the 16.1% of patients in the 21–40-year-old group reported in the previous study was higher than the 9.8% in the present study and the 40.8% of ≥61 years group was lower than the 48.9% in the present study. The incidence of TBI in the other age groups (≤20 and 41–60) was similar to that presented here (11.1% vs. 10.4%, 31.8% vs 30.9%). The previous authors suggested that because of the geographical characteristics of Iksan and the surrounding area, which have a lot of agricultural areas, and authors' hospital is located in a rural area, the size of the younger population is smaller than in other urban areas. The most common diagnosis in Song et al.10) was A-SDH (37.5%) followed by A-EDH (15.1%), T-SAH (14.4%), contused intracranial hemorrhage (9.8%), and diffuse axonal injury (1.6%). This result was similar to the present study when considering the differences in the classification of diagnosis. There were also differences in the proportion of groups when classified according to the initial GCS scores; Song et al. reported that the mild, moderate, and severe groups formed 72%, 12.7%, and 15.3% of their sample respectively. However, in the present study, the mild, moderate, and severe groups accounted for 70.9%, 11.0%, and 18.1% of the sample respectively, with a larger proportion of patients in the severe group than in their study. This was thought to be because the group of elderly people over the age of 61 years was larger in our study. In their study, 26.2% of total patients received surgical treatment; in contrast, 31% of patients in the current study underwent surgical treatment. This was thought to be due to the fact that the severe group was larger in the present study.
In most previous studies, the most common causes of TBI were falls and traffic accidents.2,3,13) The trends regarding TBI have changed with time, and in this study, the number of traffic accidents was found to be less than the number of people who fell. Taylor et al.13) reported that approximately 2,800,000 TBI-related ER visits, hospital admissions, and deaths occurred in the United States in 2013, representing an increase since 2007 that was largely attributed to an increase in the number and rate of TBI-related ER visits. They found that this report indicated that older adults falling accounted for a much larger proportion of the increase in TBI-related ER visits during this period. They emphasized that the modest increase in ER visits that might be attributed to youth sports concussion do not extend to increases in TBI-related hospital admissions and deaths; however, the same cannot be said for TBIs attributable to older adults falling. From 2007 to 2013, increases in TBI-related hospital administrations and deaths attributable to older adults falling suggests the need for greater attention required to prevent older adult falls. In Korea, it is thought that the proportion of accident types are changing over time due to safety devices, such as seat belts and airbags, automobile navigation system, and strong traffic regulations. As a result, the number of falls has increased relative to traffic accidents.
In the present study, 37.8% of traffic accidents were related to bikes (bicycle and motorcycle), which is relatively high compared with other regions or nationwide statistics in Korea.6) This is probably due to the relatively large number of farming areas and aged population in the vicinity, which is why bikes are used as transportation. Unlike automobiles, motorcycles have poor structural stability, so that when a traffic accident occurs, the driver or passenger directly experiences the impact, resulting in many TBIs. Taylor et al.13) reported that the decrease in TBI-related deaths caused by motor vehicle crashes from 2007 to 2013 is likely attributable to efforts to prevent motor vehicle crashes in the United States. In order to reduce the risk of TBI associated with bikes, it is necessary to require the wearing of a helmet, reinforcement of legal enforcement, and safety education.
Agrawal et al.1) categorized the timings based on traffic hours and reported that the highest number of accidents and deaths were reported at 21:00–07:00. They reported that TBI was the most common on Tuesday (17.8%) and Wednesday (16.6%), in January (13.9%) and December (12.8%), and post monsoon (fall) (28.5%), and only admission seasons were significantly related to patient outcome. TBI was most frequent among 20–40-year-olds (49.9%) and 40–60-year-olds (26.7%). In their study, age, sex, and severity as defined by GCS, which were significantly related to outcome and season, were also significantly related to week and treatment with intracranial surgery. They explained that their pilot study provided an eloquent insight into brain injury area in a developing country.
In this study, TBI patients presented most frequently at 13:00–18:00 (38.8%), on Saturday (20.2%), in December (11.9%) and July (10.5%), and in summer (29.7%). According to a study of occupational traumatic brain injury in Ontario by Colantonio et al.,5) accidents most frequently occurred from 09:00 to 11:59 and accidents were most common in January, February, and March. They explained that the reason for this was that there were a lot of shifts in the morning and the period of selecting new employees is mainly concentrated in January and February. However, the effect of weather conditions only account for 5.7% of all causes of TBI. With respect to this, the concentration of TBI in the summer in this study should take into account not only the number of construction works, but also the specificity of employment in secondary industry.
Based on the GCS score at admission, moderate to severe patients were concentrated in December and in winter in this study (TABLE 3). According to a study of TBI in children who needed ICU care in the UK, there was no difference based on day of the week, but the peak time of admission was from 12:00 to 18:00 according to the time of admission, and admission was more prevalent in the summer.8) In a study of patients who died as a result of trauma in the greater Stavanger area from 1996 to 2004, deaths occurred with some monthly variance and demonstrated two monthly peaks in February/March and July/August.11) This is explained by the increase in recreational activities due to the winter and summer vacation seasons and increase in traffic accidents due to an increase in traffic volume. It also suggests that the “July phenomenon”, in which trauma increases in July when inexperienced trainees are mainly employed, plays a role in this situation.9) In a study of TBI-related deaths in children from 1996 to 2005 in Norway, it was reported that fatal child TBI was concentrated in spring (53%) and summer (25%).12) This is due to the fact that there is more daylight in spring and summer in Norway than in fall and winter, so there was more time for the children to move to and from school, and as a result, a longer period of time for children to receive TBI. The results from the present study differed from those of a previous study. The author believes that winter weather is more likely to lead to the occurrence of TBI due to falls or traffic accidents caused by icy roads and bad weather, which is unlikely to occur in the summer. However, in the previously mentioned study of occupational traumatic brain injury in Ontario, it is difficult to identify the increase in TBI in winter as a cause of weather simply because of limited influence of weather.5) Additional statistical studies will be needed to elucidate this relationship.
TABLE 3. Comparison of clinical characteristics between mild, moderate, and severe groups defined based on GCS scores.
| Characteristics | Mild (GCS 13–15) (n=232) | Moderate (GCS 9–12) (n=36) | Severe (GCS 3–8) (n=59) | Total | p-value | |
|---|---|---|---|---|---|---|
| Time of day | 0.035 | |||||
| 01:00–06:00 | 32 (13.8) | 6 (16.7) | 3 (5.1) | 41 (12.5) | ||
| 07:00–12:00 | 72 (31.0) | 7 (19.4) | 29 (49.2) | 108 (33.0) | ||
| 13:00–18:00 | 97 (41.8) | 15 (41.7) | 18 (30.5) | 130 (39.8) | ||
| 19:00–00:00 | 31 (13.4) | 8 (22.2) | 9 (15.3) | 48 (14.7) | ||
| Day of the week | 0.788 | |||||
| Sun | 28 (12.1) | 7 (19.4) | 5 (8.5) | 40 (12.2) | ||
| Mon | 28 (12.1) | 5 (13.9) | 8 (13.6) | 41 (12.5) | ||
| Tue | 31 (13.4) | 3 (8.3) | 13 (22.0) | 47 (14.4) | ||
| Wed | 28 (12.1) | 5 (13.9) | 6 (10.2) | 39 (11.9) | ||
| Thu | 36 (15.5) | 4 (11.1) | 8 (13.6) | 48 (14.7) | ||
| Fri | 31 (13.4) | 5 (13.9) | 10 (16.9) | 46 (14.1) | ||
| Sat | 50 (21.6) | 7 (19.4) | 9 (15.3) | 66 (20.2) | ||
| Months | 0.090 | |||||
| Jan | 18 (7.8) | 3 (8.3) | 3 (5.1) | 24 (7.3) | ||
| Feb | 12 (5.2) | 3 (8.3) | 3 (5.1) | 18 (5.5) | ||
| Mar | 21 (9.1) | 6 (16.7) | 2 (3.4) | 29 (8.9) | ||
| Apr | 15 (6.5) | 1 (2.8) | 6 (10.2) | 22 (6.7) | ||
| May | 21 (9.1) | 6 (16.7) | 1 (1.7) | 28 (8.6) | ||
| Jun | 23 (9.9) | 3 (8.3) | 4 (6.8) | 30 (9.2) | ||
| Jul | 26 (11.2) | 1 (2.8) | 8 (13.6) | 35 (10.7) | ||
| Aug | 27 (11.6) | 0 (0.0) | 5 (8.5) | 32 (9.8) | ||
| Sep | 14 (6.0) | 1 (2.8) | 6 (10.2) | 21 (6.4) | ||
| Oct | 14 (6.0) | 1 (2.8) | 5 (8.5) | 20 (6.1) | ||
| Nov | 24 (10.3) | 2 (5.6) | 3 (5.1) | 29 (8.9) | ||
| Dec | 17 (7.3) | 9 (25.0) | 13 (22.0) | 39 (11.9) | ||
| Season | 0.005 | |||||
| Spring | 57 (24.6) | 13 (36.1) | 9 (15.3) | 79 (24.2) | ||
| Summer | 76 (32.8) | 4 (11.1) | 17 (28.8) | 97 (29.7) | ||
| Fall | 52 (22.4) | 4 (11.1) | 14 (23.7) | 70 (21.4) | ||
| Winter | 47 (20.3) | 15 (41.7) | 19 (32.2) | 81 (24.8) | ||
Values are presented as number of patients (%).
GCS: Glasgow Coma Scale.
In the present study, a statistical relationship between time of day and season when the patients were divided into groups based on their initial GCS scores. Patients in the severe group presented to the hospital mainly in the morning and winter, while patients in the mild group presented mainly to the hospital in summer. This phenomenon is thought to be influenced by various conditions such as the climatological characteristics of winter weather, demographic characteristics of the elderly population, and geographical characteristics of many agricultural areas among others, in addition to their inevitable interaction.
Study limitations
There are several limitations of this study. First, the study period is only two years; therefore, the period is very short to accurately represent the time-related influence. Second, despite the fact that the timing of the injury is an important factor that affects outcome, the author could not clarify the time difference between when the injury occurred and when the patient presented to the hospital. Third, multiple factors have not been taken into account that may significantly affect the result because this study was carried out in only one center. Fourth, there was no evaluation of the length of hospital stay or the prognosis of the patient according to the time of ER visit.
CONCLUSION
In summary, patients with TBI were found to most frequently present at 13:00–18:00, on Saturday, in December, and in summer. Surgical treatment was not related to any temporal trends in the presentation of TBI patients. A significant relationship between ER arrival time and season according to GCS score was seen. In particular, TBI patients in the severe group arrived at the ER mainly at 07:00–12:00. TBI patients in the mild group primarily presented to the ER in summer, while TBI patients in the moderate group presented mainly in winter. The combination of the mild and moderate groups showed greater presentation in winter. Although the study has many limitations, it is worthwhile to know the temporal trends of the presentation of TBI patients. These data would help to obtain useful information to predict the ER visits of TBI patients in advance and prepare for prompt and appropriate treatment. Further studies with larger samples and multi-institutional integration are required to provide better insight in this area
Footnotes
Conflict of Interest: The author has no financial conflicts of interest.
References
- 1.Agrawal A, Munivenkatappa A, Rustagi N, Rammohan P, Subrahmanyam BV. Time of admission and outcome in traumatic brain injury patients. Med J DY Patil Univ. 2016;9:465–468. [Google Scholar]
- 2.Annegers JF, Grabow JD, Kurland LT, Laws ER., Jr The incidence, causes, and secular trends of head trauma in Olmsted County, Minnesota, 1935–1974. Neurology. 1980;30:912–919. doi: 10.1212/wnl.30.9.912. [DOI] [PubMed] [Google Scholar]
- 3.Asemota AO, George BP, Bowman SM, Haider AH, Schneider EB. Causes and trends in traumatic brain injury for United States adolescents. J Neurotrauma. 2013;30:67–75. doi: 10.1089/neu.2012.2605. [DOI] [PubMed] [Google Scholar]
- 4.Chyatte D, Chen TL, Bronstein K, Brass LM. Seasonal fluctuation in the incidence of intracranial aneurysm rupture and its relationship to changing climatic conditions. J Neurosurg. 1994;81:525–530. doi: 10.3171/jns.1994.81.4.0525. [DOI] [PubMed] [Google Scholar]
- 5.Colantonio A, Mroczek D, Patel J, Lewko J, Fergenbaum J, Brison R. Examining occupational traumatic brain injury in Ontario. Can J Public Health. 2010;101 Suppl 1:S58–S62. doi: 10.1007/BF03403848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korea Road Traffic Authority. Traffic accident analysis system (TAAS) Wonju: Korea Road Traffic Authority; c2020. [Accessed December 31, 2017]. http://taas.koroad.or.kr/web/shp/sbm/initUnityAnalsSys.do?menuId=WEB_KMP_OVT_UAS. [Google Scholar]
- 7.McDonald RJ, McDonald JS, Bida JP, Kallmes DF, Cloft HJ. Subarachnoid hemorrhage incidence in the United States does not vary with season or temperature. AJNR Am J Neuroradiol. 2012;33:1663–1668. doi: 10.3174/ajnr.A3059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parslow RC, Morris KP, Tasker RC, Forsyth RJ, Hawley CA, et al. UK Paediatric Traumatic Brain Injury Study Steering Group. Epidemiology of traumatic brain injury in children receiving intensive care in the UK. Arch Dis Child. 2005;90:1182–1187. doi: 10.1136/adc.2005.072405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schroeppel TJ, Fischer PE, Magnotti LJ, Croce MA, Fabian TC. The “July phenomenon”: is trauma the exception? J Am Coll Surg. 2009;209:378–384. doi: 10.1016/j.jamcollsurg.2009.05.026. [DOI] [PubMed] [Google Scholar]
- 10.Song SY, Lee SK, Eom KS, KNTDB Investigators Analysis of mortality and epidemiology in 2617 cases of traumatic brain injury: Korean Neuro-Trauma Data Bank System 2010–2014. J Korean Neurosurg Soc. 2016;59:485–491. doi: 10.3340/jkns.2016.59.5.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Søreide K. Temporal patterns of death after trauma: evaluation of circadian, diurnal, periodical and seasonal trends in 260 fatal injuries. Scand J Surg. 2010;99:235–239. doi: 10.1177/145749691009900411. [DOI] [PubMed] [Google Scholar]
- 12.Søreide K, Krüger AJ, Ellingsen CL, Tjosevik KE. Pediatric trauma deaths are predominated by severe head injuries during spring and summer. Scand J Trauma Resusc Emerg Med. 2009;17:3. doi: 10.1186/1757-7241-17-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, And Deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017;66:1–16. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]