1. Images in pediatrics
A seven-day-old, fullterm baby girl presented to the emergency room with vomiting and poor feeding. She was born at 38 weeks of gestation through uncomplicated, normal spontaneous vaginal delivery. She was discharged after 24 h with no complication.
The patient started to have poor sucking and vomiting starting on day five. The baby was lethargic and jaundiced in clinical examination. The patient admitted to our hospital for investigation.
Biochemical evaluation revealed mild increased serum glutamic pyruvic transaminase (SGPT)/serum glutamicoxaloacetic transaminase (SGOT) and alkaline phosphatase levels. Also, the patient had elements of mild direct hyperbilirubinemia.
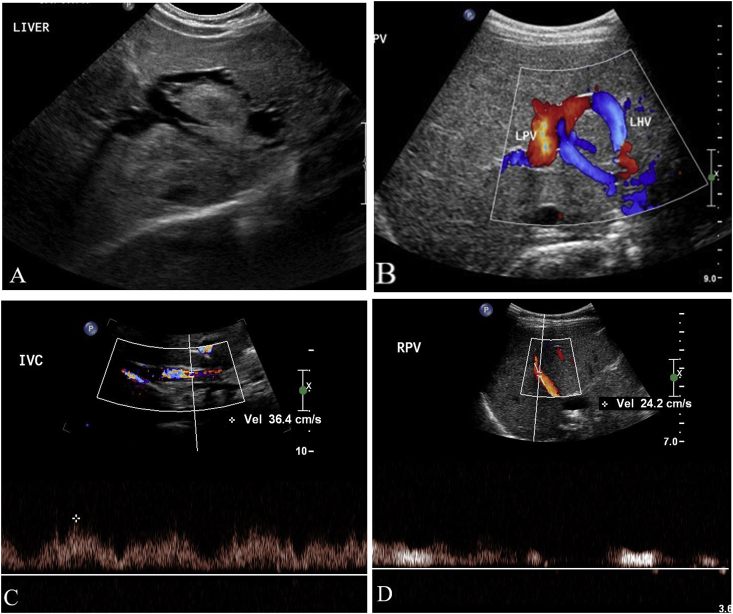
Ultrasound of the abdomen showed normal liver size and echogenicity. There is abnormal communication between the left portal vein and the left hepatic vein (Fig. 1) consistent with congenital porto-systemic shunt type II.
Fig. 1.
A. transvers US image of the left hepatic lobe shows a communication between the left portal vein and the left hepatic vein. B. Color Doppler US image demonstrates the vascular nature of the communication. C and D. The Doppler flow difference between the shunt and MPV is 50%.
The case was discussed with the interventional radiologist considering the risks, benefits, and alternatives management plan. The final decision was made to follow up the patient clinically and by ultrasound for short term interval (every 3 months) as the shunt ration is <60% which is less likely associated with hepatic encephalopathy (dividing the blood flow volume at the shunt orifice by the total portal blood flow volume on Doppler US) [1].
The patient was followed up clinically; her liver enzymes and bilirubin level showed significant improvements. The follow up ultrasound showed stable shunt.
Congenital portosystemic shunt (CPSS) is a condition in which the portomesenteric blood drains into a systemic vein, bypassing the liver through a complete or partial shunt. Portosystemic shunts have been classified as intrahepatic and extrahepatic.
The embryology of the portal vein development is so complicated. It takes place between 4th-10th gestational age. It arises from two vitelline veins, any abnormalities in involution or connection of those veins may led to congenital portosystemic connection.
Congenital intrahepatic portosystemic venous shunt is an uncommon condition that probably results from abnormal embryonic development early in fetal life [2].
2. Classification of intrahepatic congenital portosystemic shunt: Perk et al. (1990)
-
Type 1
Single large vessel connecting the right PV to the IVC.
-
Type 2
Localized peripheral branches of the PV and the hepatic veins.
-
Type 3
Aneurysmal communication between the peripheral PV and the hepatic veins.
-
Type 4
Multiple communications between the PV and the hepatic veins distributed in both lobes.
Clinical presentation: patient with CPSS could be asymptomatic, or they may present with abnormal liver function and metabolic disturbance. The patient also may present with hepatic encephalopathy as a complication later in life.
Radiological diagnosis started with ultrasound especially Doppler study. CT and MRI help in further classification of the anomalies and associated abnormalities. Measuring the shunt ration is crucial to estimate the risk for hepatic encephalopathy.
Conventional angiography is necessary when results of the other tests disagree or are inconclusive.
The treatment of intrahepatic CPSS depends mainly on the type of the shunt. The shunt may close in spontaneously 2 y with no intervention. While some patients need intervention with either by surgical operations such as shunt ligation and hepatic resection or by closure device by interventional radiologist [1,3].
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
Amna Kashgari, Email: drakashgari@gmail.com.
Mohammed Al Otibi, Email: otaibimom@ngha.med.sa.
References
- 1.Lee S., Lee Y., Lee K., Jeon G. Congenital intrahepatic portosystemic venous shunt and liver mass in a child patient: successful endovascular treatment with an Amplatzer vascular plug (AVP) Korean J Radiol. 2010;11:583–586. doi: 10.3348/kjr.2010.11.5.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallego G., Miralles M., Marı´n C., Muyor P.Gonza´lez G., Garcı´a- Hidalgo E. Congenital hepatic shunts. Radiographics. 2004;24:755–772. doi: 10.1148/rg.243035046. [DOI] [PubMed] [Google Scholar]
- 3.Chandrasekharan R., Pullara S., Thomas T., Kader N., Moorthy S. Congenital intrahepatic portosystemic shunts: imaging findings and endovascular management. Indian J Radiol Imag. 2016;26(1):92–94. doi: 10.4103/0971-3026.178349. [DOI] [PMC free article] [PubMed] [Google Scholar]