Abstract
Spontaneous corneal perforation is very rare in neonates and children. Peters anomaly is associated with spontaneous corneal perforation. Herein, we describe a case of spontaneous corneal perforation in a 13-day-old Saudi infant who was admitted to the neonatal intensive care unit since birth. This report is important to gain more information about corneal perforation clinical presentation in neonates, investigation, and management.
Keywords: Corneal perforation, Neonate, Excessive tearing, Peter's anomaly
1. Introduction
Neonatal corneal perforation is rare in the first weeks of life. Only few cases have been reported in literature. Instrumentation and assisted deliveries have been reported to cause minor ocular trauma, but corneal perforations are a rare occurrence, and to date, very few cases have been reported. Some of these cases are associated with systemic infection and preterm babies [[1], [2], [3], [4]].
Most of the reported cases are discovered during an ophthalmological exam. In this report, we describe a rare case of spontaneous corneal perforation in a 13-day-old Saudi infant who was admitted to the neonatal intensive care unit for symmetrical intrauterine growth retardation.
2. Case report
The infant in our case was born to a 27-year-old Saudi woman, gravida 6, para 2 with 3 abortions. She was unbooked at our hospital, but she had no known medical illnesses. She has two healthy living kids. There was positive consanguinity of first degree. The mother presented to our hospital at 37 weeks and 4 days in active labor. The infant was delivered by spontaneous vaginal delivery and had Apgar scores of 9 and 9 at 1 and 5 minutes, respectively. Measurements such as birth weight 1690 g (<1%), length 40 cm (<1%), and head circumference 29 cm (<1%) were consistent with those of symmetrical IUGR. He was noted to have cloudy cornea with bulging of the eyes more on the right side (Fig. 1). On physical examination, he had microcephaly with open, flat fontanelles; facial dysmorphism; beaked nose; abnormal ears, micrognathia. Eye examination revealed cloudy cornea, which was completely opaque with bulging of the eyes more on the right side and absent red reflex. Eye examination by an ophthalmologist showed bilateral central corneal opacities with calcification and poor formation of the anterior chamber. The fundus in both eyes could not be visualized. There was no evidence of glaucoma with normal eye pressure bilaterally.
Fig. 1.
Right eye opaque cloudy cornea with calcification bulging of the eyes more on the right side.
He had a normal pattern of breathing, no distress with oxygen saturation 95% in room air, and equal breath sounds bilaterally. Cardiovascular examination showed normal S1 and S2; regular rate and rhythm; grade 2 murmur heard over the left second intercostal region. His abdomen was soft to palpation, no hepatosplenomegaly, and no lymphadenopathy. He had a small phallus with normally descended testes. Skeletal examination showed small hands with bilateral clinodactyly.
His initial laboratory studies showed white blood cell count of 9.00 cells/mL (9*109 cells/L) with a normal differential count, hemoglobin of 13 g/dL (130 g/L), platelet count of 240*103 cells/mL (240*109 cells/L). Infant serology screening for toxoplasmosis, syphilis, measles, rubella, cytomegalovirus, and herpes simplex was negative. Skeletal survey was normal. Newborn metabolic screening was negative. Echocardiography showed small PDA. His abdominal ultrasound (US) was normal apart from a mild fullness of right renal pelvis. Chromosome analysis was normal, i.e., 46 XY. The baby was stable in NICU for workup and management of IUGR until day 13 of life when the right eye was suddenly found to be shrunken and smaller with excessive tearing, no redness, or facial swelling.
Urgent eye examination was performed, which revealed corneal perforation, iris protrusion, and a flat anterior chamber. The diagnosis was spontaneous right corneal perforation. The patient was taken for surgery immediately. The operative findings showed a central disc-like melting of the cornea of approximately 3 mm in diameter with a partial rupture medially along the margins. The anterior chamber was found to be collapsed, and the eyeball was soft. A thorough washout of the wound and the eye was done with a balanced salt solution. Following this, a partial-thickness corneal grafting of the descemet membrane was done, which was re-sutured to the cornea to close the perforation. A large bridge of conjunctival flap was mobilized from the lower fornix and was brought over the ulcer, which was sutured to the limbus and the superior conjunctiva. The patient was given intravenous antibiotics for one week postoperatively. The baby had many follow-up examinations after surgery, and there was no evidence of endophthalmitis or evidence of infection at any time.
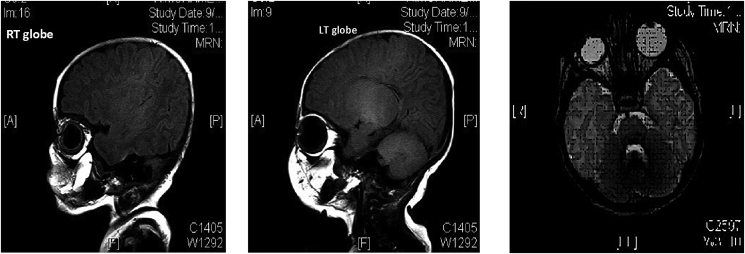
His biochemistry showed hypocalcemia with adjusted calcium levels of 1.6 and deficient parathyroid hormone levels (<3), and he was started on a calcium supplement and one alfacalcidol in conjunction with the endocrinology team. MRI of the brain on day 17 showed a small right corpus callosum and a small right globe (Fig. 2), with rest of the brain reported as normal. On day 40, he had a seizure that responded to calcium infusion, and the EEG was normal. FISH was performed to rule out DiGeorge syndrome, which was negative. A CT of the brain performed at 7 weeks of age showed a small right orbital globe with aphakia (Fig. 3).
Fig. 2.
MRI brain showing a small right globe compared to the left one.
Fig. 3.
CT scan showing normal left eye and a small right globe with irregular outline, C) both eyes.
He remained otherwise hemodynamically stable during his NICU stay and had no other significant issues apart from feeding intolerance and poor weight gain, which improved a little with time. He was discharged home on day 51 with a weight of 1.955 kg. Later on, he developed perforation of the left eye at 4 months of age, which was repaired by amniotic membrane transplantation, but unfortunately, it had to be removed one month later, and the perforation was repaired again.
He is on continued follow-up with the pediatric, endocrine, and ophthalmology teams. There is failure to thrive (all his growth parameters below the third centile), and he has severe developmental delay. His calcium levels are currently stable on one alfacalcidol.
3. Discussion
Neonatal corneal perforation is rare in the first weeks of life. Peters anomaly is characterized by a central corneal opacity from the time of birth and is accompanied by corresponding defects in the posterior stroma, Descemet's membrane, and endothelium, i.e., anterior segment dysgenesis. Peters anomaly has been associated with spontaneous corneal perforation [[5], [6], [7]]. Most of the reported cases are discovered during incidental ophthalmological exam. Signs of corneal perforation in the neonate should be suspected with sudden shallowing or flattening of the anterior chamber, which leads to sudden shrunken eye. They also have aqueous leakage, which is mistaken as excessive tearing.
Early referral of suspected diagnosis for a proper ophthalmological exam by pediatric ophthalmologist and exploration of the eye under anesthesia as soon as possible can establish the diagnosis and initiate prompt management. Our case was further complicated by spontaneous left eye perforation at 4 months of age. It has been postulated that structurally malformed eyes are more prone to corneal perforations.
The best treatment strategies for neonatal corneal perforation are not known. In the absence of excess spontaneous leakage and if the anatomy of the eye is intact (e.g., the iris and lens are in their normal locations), the experts indicate that close observation and broad-spectrum topical antibiotic coverage may be the best option. In these cases, the cornea can heal spontaneously but need daily eye exams for the first few days to ensure that the cornea does not begin to leak. The conjunctival flap is a known treatment for corneal perforation. Its purpose is to restore the integrity of a compromised corneal surface and prevent secondary infection. Although the conjunctival flap does not permit good visual acuity, it is helpful to preserve the eye. Amniotic membrane transplantation (AMT) is an established technique in the treatment of various diseases of the cornea. It promotes epithelialization and differentiation of the epithelium of the ocular surface. As corneal perforation is very rare, there is no consensus on which patient should be treated with which intervention. In our patient, the right corneal perforation was treated with conjunctival flap and the left corneal perforation with AMT and the left eye required a second surgery. However, the final result was the same in both eyes, and vision could not be salvaged.
4. Conclusion
Spontaneous corneal perforation in Peters anomaly may occur in the neonatal period as early as two weeks of life. Therefore, these babies should be monitored for such possibility, especially if they present with sudden shrunken eyes and excessive tearing, and must be referred appropriately for further management. Conjunctival flap and AMT are the treatment options for rapid repair of corneal perforation. However, the final result may not salvage the vision. To the best of our knowledge, this is the first documented case of bilateral spontaneous corneal perforation in Peters anomaly from Saudi Arabia.
Author disclosure
Drs Alallah, Mohtisham, and Khan have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
References
- 1.Bachynski B.N., Andreu R., Flynn J.R. Spontaneous corneal perforation and extrusion of intraocular contents in premature infants. J Pediatr Ophthalmol Strabismus. 1986;23:25–28. doi: 10.3928/0191-3913-19860101-07. [DOI] [PubMed] [Google Scholar]
- 2.Jensen O.A. Necrotizing keratitis (keratomalacia) with corneal perforation and expulsive uveal hemorrhage in a ew-born. Acta Ophthalmol (Copenhagen) 1968;46:215–217. doi: 10.1111/j.1755-3768.1968.tb05180.x. [DOI] [PubMed] [Google Scholar]
- 3.Backes C.R., Makley T.A., Jr., Rogers G.L., Cordero L.C., Forsythe R. Spontaneous corneal perforation with expulsion of the lens and retina in a premature infant. J Pediatr Ophthalmol Strabismus. 1980;17:242–244. doi: 10.3928/0191-3913-19800701-11. [DOI] [PubMed] [Google Scholar]
- 4.Michelson P.E., Rupp R., Efthimiadis B. Endogenous Candida endophthalmitis leading to bilateral corneal perforation. Am J Ophthalmol. 1975;80:800–803. doi: 10.1016/0002-9394(75)90274-3. [DOI] [PubMed] [Google Scholar]
- 5.Krause U., Koivisto M., Rantakallio P. A case of Peters syndrome with spontaneous corneal perforation. J Pediatr Ophthalmol Strabismus. 1969;6:145–149. [Google Scholar]
- 6.Traboulsi E.I., Maumenee I.H. Peters' anomaly and associated congenital malformations. Arch Ophthalmol. 1992;110:1739–1742. doi: 10.1001/archopht.1992.01080240079035. [DOI] [PubMed] [Google Scholar]
- 7.Banning C.S., Blackmon D.M., Song C.D., Grossniklaus H.E. Corneal perforation with secondary congenital aphakia in Peters' anomaly. Cornea. 2005;24:118–120. doi: 10.1097/01.ico.0000134187.19117.6a. [DOI] [PubMed] [Google Scholar]