Abstract
Background:
Although spinal deformities are common in patients with neurofibromatosis type 1 (NF1), there is a paucity of data as to how this impacts outcomes of spinal fusion surgery in pediatric/young adult patients.
Methods:
Using the Nationwide Inpatient Sample (2005–2014) for all patients undergoing spinal fusion ≤26 years of age, we compared the following factors: demographics, comorbidities, and perioperative variables (e.g., between NF1 vs. non-NF1, and between NF1 and propensity score (PS)-matched non- NF1 spinal fusion patients) using univariate hypothesis tests and multivariate regression analyses. Our main interest focused on length of stay, complication rates, adverse postoperative events, and incidence of nonroutine discharges.
Results:
In this study, 238 (0.92%) NF1 spine patients were compared to 25,558 (99.08%) non-NF1 spine patients. NF1 fusion patients were younger, included fewer females, and were more likely to be on Medicaid. Perioperatively, NF1 patients underwent more anterior approaches, had more vertebrae fused, required more transfusions, had a longer length of stay (LOS), and were less likely to be discharged home. However, after PS- matching, all differences between NF1 and non-NF1 groups disappeared were similar (P > 0.05). In PS-matched multivariate analyses, NF1-status was not a significant independent predictor of length of stay or nonroutine discharge disposition.
Conclusion:
NF1-status was, therefore, not an independent predictor of complications, adverse postoperative events, longer LOS, or nonroutine hospital discharge in this cohort analysis. Further prospective studies are necessary to understand how outcomes in patients with NF1 compare to non-NF1 pediatric and young adult patients.
Keywords: Neurofibromatosis type 1, Outcomes, Spinal fusion

INTRODUCTION
Though rare, neurofibromatosis type 1 (NF1) is the most common autosomal dominant disorder found in humans. The patient presents with a heterogeneous range of clinical signs and symptoms. One of the most common and potentially debilitating factors in NF1 patients is the 38% incidence of spinal deformity (e.g., develop dystrophic or nondystrophic).[6]
Here, we evaluated whether, following spinal surgery, the short-term perioperative outcomes of pediatric/young adult patients with NF1 were inferior to those without NF1.
MATERIALS AND METHODS
Data source and patient population
Using the Healthcare Cost and Utilization Project Nationwide Inpatient Sample, we retrospectively analyzed NF1 versus non-NF1 pediatric/young adult patients undergoing elective spinal fusions (2005–2014). We focused on the following major clinical variables: patient demographics, expected payer, diagnoses (e.g., pre- and post-operative diagnoses), procedures, length of stay (LOS), pre-, peri-, and post- operative risk factors associated with prolonged LOS, and nonroutine discharges with/without NF1.
Documentation of NF1
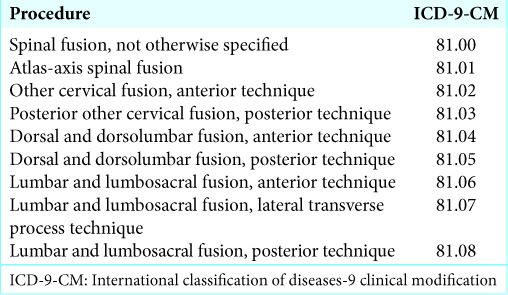
Documenting the diagnosis of NF1 was based on: International Classification of Disease (e.g. International Classification of Diseases-9, Ninth Revision [ICD-9] and ICD-9 clinical modification (ICD-9-CM) diagnosis and procedure codes), evaluation of all hospital discharges for pediatric and young adult patients ≤26 years of age with/ without NF1, Type 1 (237.71), and patients undergoing elective Spinal Fusions (Procedures codes listed in Table 1).
Table 1:
ICD-9-CM used for spinal procedures.
Data collection
Patient demographics, comorbidities, perioperative variables postoperative events/complications, outcomes, LOS, and discharge dispositions, were excluding. In-hospital death and discharge against medical advice and complications were compared between NF1 and non-NF1 patients.
Statistical analysis
Counts and percentages were described for categorical variables for NF1 versus non-NF1 patients. Two-tailed Student’s t-tests were used to compare normally distributed continuous variables between NF1-status cohorts, while Mann–Whitney U-tests were used to compare nonnormally distributed continuous variables. Significance for all statistical tests was assessed with a threshold of P = 0.05. Due to the unbalanced disease status arms in our cohort, a propensity score (PS)-matched No NF1 cohort was generated.
RESULTS
Patient demographics
In our study, 238 (0.9%) had NF1 and 25,558 (99.1%) had no diagnosis of NF1 (No NF1) [Table 2], NF1 was more likely to receive an anterior surgical approach but less likely to undergo a 2–3 level vertebral fusion versus non-NF1 patients [Table 2].
Table 2:
Preoperative and perioperative variables.
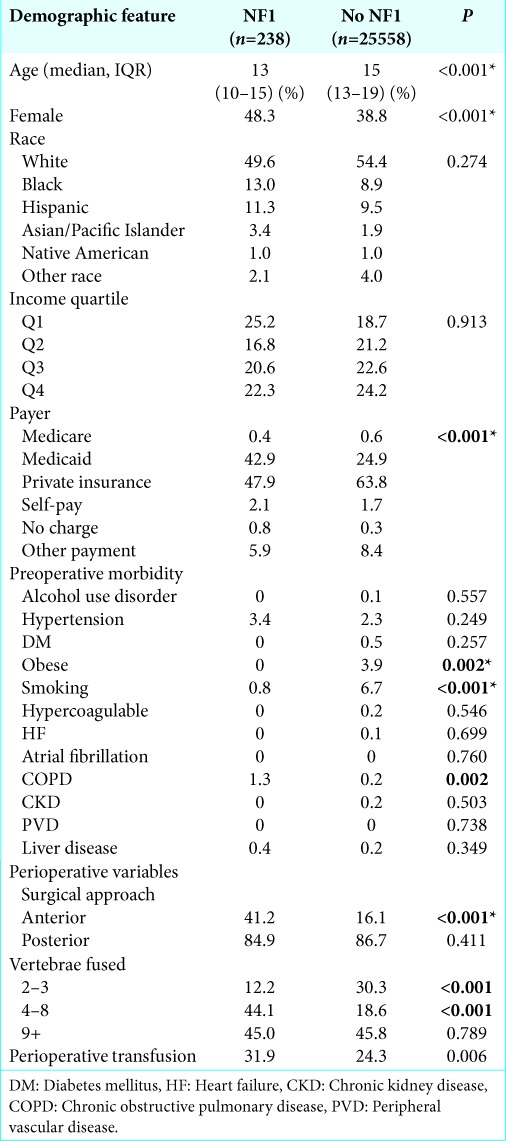
Both patients groups had similar pre-, peri-, and post- operative clinical/other characteristics; age, sex, primary expected payers preoperative comorbidities perioperative variables, rates of complications, median LOS, or rates of nonroutine discharges [Table 2].
NF1 patients were most commonly from the 0–25% income quartile (Q1) (25.2% vs. 18.7%), were more likely to be insured through Medicaid (42.9% vs. 24.9%), and had the most prevalent preoperative morbidities including; (1) hypertension, (2) chronic obstructive pulmonary disease, and (3) smoking; in the non-NF1 group they were (1) smoking, (2) obesity, and (3) hypertension [Table 2].
Perioperative outcomes after spinal fusion
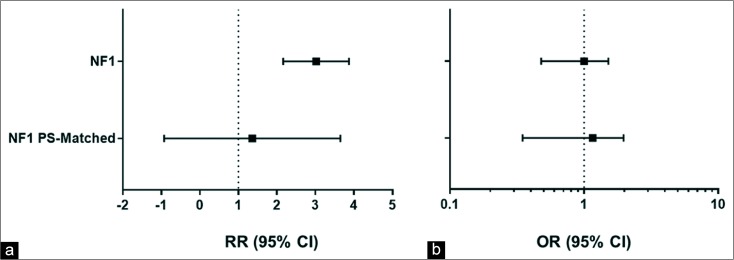
The NF1 patients had more central nervous system complications, postoperative infections, longer length of stay, and more nonroutine discharges, but spinal fusion patients with or without NF1 had similar pre-, peri-, and post- operative characteristics [Tables 1-3]. Table 4 lists the variables for propensity score-matched set data. In multivariate logistic regression analysis, there was no significant difference between the odds of being discharged nonroutinely between spinal fusion patients with NF1 and those without (Odds Ratio [OR]: 0.91, CI: 0.53–1.56; P = 0.73), when controlling for other factors [Table 5]. When comparing PS-matched sets data in multivariate logistic regression analysis, this difference remained statistically insignificant (OR: 0.97, CI: 0.46–2.05; P = 0.93) [Table 5, Figure 1].
Table 3:
Postoperative complications, events, and outcomes.
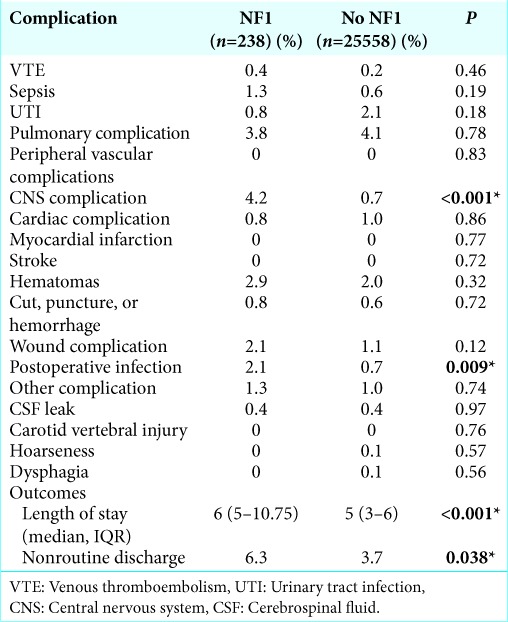
Table 4:
Pre-, peri-, and post-operative variables for propensity score-matched set data.
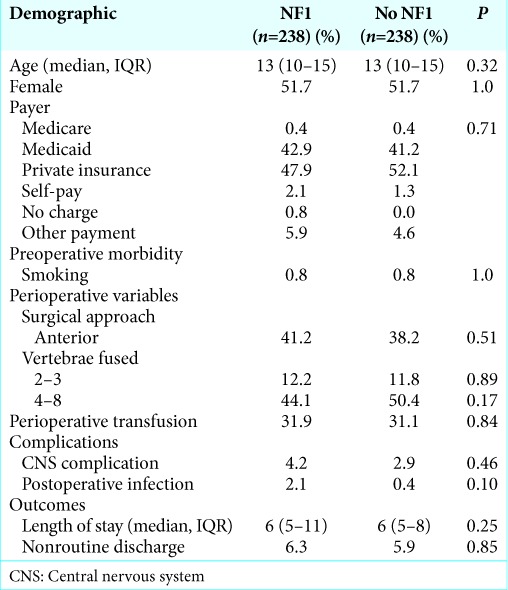
Table 5:
Propensity score matched predictors of home discharge: multivariate linear and logistic regression models and multivariate doubly-robust PS-matched linear and logistic regression models.
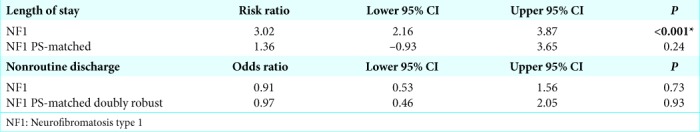
Figure 1:
Forest plots representing relative risks and odds ratios for the regression models in Table 4. (a) Multivariate linear regression models of neurofibromatosis (NF1) status on length of stay and (b) multivariate logistic regression models of NF1-status on nonroutine discharge.
DISCUSSION
In this study, we determined that NF1 (238 [0.9%] pediatric/ young patients undergoing spinal fusions had similar outcomes to non-NF1 patients 25,558 [99.1%]). We also found that those with NF1 were likely to have a greater number of vertebrae fused, and were more likely to receive perioperative transfusions.[1,2,4,7] In our PS-matched analysis, the observed difference in length of stay between patients with and without NF1 did not reach significance. Similarly, we applied a multivariate logistic regression to explore the likelihood of nonroutine discharge in patients with and without NF1 and again found no difference between the two groups.
CONCLUSION
Comparing outcomes for NF1 versus non-NF1 pediatric/ young patients (≤26 years old) undergoing spinal fusion, we found that NF1 patients were no more likely than their counterparts without NF1 to experience inferior surgical outcomes.
Footnotes
How to cite this article: Freedman I, Koo A, Yeagle E, Diluna M, Kolb L, Yeung J. Does neurofibromatosis 1 status impact outcomes for pediatric/ young adults undergoing spinal fusion? Surg Neurol Int 2020;11:60.
Contributor Information
Isaac Freedman, Email: isaac.freedman@yale.edu.
Andrew Koo, Email: andrew.koo@yale.edu.
Erin Yeagle, Email: erin.yeagle@yale.edu.
Michael Diluna, Email: michael.diluna@yale.edu.
Luis Kolb, Email: luis.kolb@yale.edu.
Jacky Yeung, Email: jacky.yeung@yale.edu.
Declaration of patient consent
Patients consent not required as patients idenity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ademiluyi SA, Sowemimo GO, Oyeneyin JO. Surgical experience in the management of multiple neurofibromatosis in Nigerians. West Afr J Med. 1989;8:59–65. [PubMed] [Google Scholar]
- 2.Favaloro EJ, Zafer M, Nair SC, Hertzberg M, North K. Evaluation of primary haemostasis in people with neurofibromatosis Type 1. Clin Lab Haematol. 2004;26:341–5. doi: 10.1111/j.1365-2257.2004.00632.x. [DOI] [PubMed] [Google Scholar]
- 3.McCandless SE, Brunger JW, Cassidy SB. The burden of genetic disease on inpatient care in a children’s hospital. Am J Hum Genet. 2004;74:121–7. doi: 10.1086/381053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niddam J, Matheron C, La Padula S, Wolkenstein P, Meningaud JP. Hemostasis and Type 1 neurofibromatosis. Plast Reconstr Surg Glob Open. 2017;5:e1414. doi: 10.1097/GOX.0000000000001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Safaee MM, Lyon R, Barbaro NM, Chou D, Mummaneni PV, Weinstein PR, et al. Neurological outcomes and surgical complications in 221 spinal nerve sheath tumors. J Neurosurg Spine. 2017;26:103–11. doi: 10.3171/2016.5.SPINE15974. [DOI] [PubMed] [Google Scholar]
- 6.Tsirikos AI, Saifuddin A, Noordeen MH. Spinal deformity in neurofibromatosis Type-1: Diagnosis and treatment. Eur Spine J. 2005;14:427–39. doi: 10.1007/s00586-004-0829-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vitale MG, Guha A, Skaggs DL. Orthopaedic manifestations of neurofibromatosis in children: An update. Clin Orthop Relat Res. 2002;401:107–18. doi: 10.1097/00003086-200208000-00013. [DOI] [PubMed] [Google Scholar]