Abstract
Purpose
The purpose of this study is the prevention of Candida colonies on PMMA Denture Base by altering the surface and incorporations of Nanoparticles.
Materials and methods
The Pub Med/Medline was searched to identify 100 relevant studies published from 2011 to 2020. The search strategy employed the following keywords related to “use of Nanoparticles in dentistry”, “Antimicrobial agents and PMMA”, “Candidiasis and nanomaterials”, “Prevention of oral Candidiasis”, “Incorporation of antimicrobial agents in acrylic dentures,” “nanoparticles as therapeutic agents for denture stomatitis”, “Nanodentistry” or “Nanotechnology” or “Nanocomposite” or “Nanodrugs” or “Nanomaterials”.
Results
Most of the studies shows that modified PMMA denture base resin containing different antimicrobial coatings and incorporation of metal oxides Nanoparticles and other nanomaterials showed antifungal activity in vitro; however some materials in higher concentration showing altered physical and mechanical properties possibly due to aggregation of Nanoparticles in the lattice of PMMA molecules.
Conclusion
Metal oxides nanomaterials revealed cytotoxicity to Candida and other microbes present in oral biofilm including PMMA denture surface. Nano toxicity may attribute to direct interaction of nanoparticles with cell membrane, hindrance in protein synthesis and early adhesion & interfere with physiology of pathogens.
Keywords: Nanotechnology, Oral biofilm, Oral candidiasis, Nanoparticles & nanomaterials, Polymethyl meth acrylate (PMMA), Nanodentistry
1. Introduction
Nanotechnology, a technology which deals objects of nanometer size and the particles are called as Nanoparticles (NPs). The term “nano” derived from the Greek word “dwarf.” In recent times, new methods have been developed to manufacture Nanoparticles so that shape and size of different Nanoparticles can be machined as per assigned work. Nanomaterials are presents in various morphologies:Nanorods, Nanotubes,Nanoprizms, Nanosphere,Nanofibers, Nanoplates,Nanoshells, Dendrimers,Nanobelts, Nanorings,Nanocapsules, Fullerenes,Nanowires, Nanobelts,Nanoparticles and nanosheets.1 The basic idea is to employ every individual atoms and molecules to construct its functional structures. The Nanoparticles can improve the quality of the dental products by adding many functional groups to it.2 Nano medicine is the controlled use of nanotechnologies in healthcare leading to new pathways for diagnosis and treatment of diseases.3,4
Nanoparticles are not new entity. NPs were in daily uses even during ancient civilizations like Mesopotamia and Egypt culture. The Nanoparticles can improve the quality of the dental products by adding many functional groups to it. Similarly many Nanoparticles viz: carbon based nanomaterials, hydroxy apatite, silica, TiO2, Ag2O, ZnO, ZrO2 & CuO have been appreciated as antimicrobial agents for Candida species and other oral microbial species. Some metal oxides Nanoparticles which are ionic in nature have antimicrobial properties, since they have high surface area and different crystalline structure with more number of reactive sites.5 Metal Nanoparticles and nonmetal Nanoparticles when combined with PMMA and other polymers or applied to material surfaces have impending relevance to the desired function in dental prosthesis.6
Candida albicans is an opportunist fungus found in human mucosa but, under local or systemic conditions,it might invade tissues and become virulent. Candida albicans is the most common species found in oral candidiasis or denture stomatitis, other species are C.tropacalis,C.glabrata.7 Oral Candidiasis is a common disease found in elderly dental patients especially in immunocompromised like transplanted patients and those patients who are under chemotherapy.8
The regular antifungal medicine used for local and systemic candidiasis have shown some serious side effects and subsequently leads to development of resistant in Candida strains which became a serious health concern.9 The toxicity of these antifungal agents is responsible for the resistance to fungi strains and further serious crisis by drug interactions demands more effective treatment with less toxicity.10 In present scenario, some alternate antifungal therapy is being trying to make effective treatment options for the treatment of Candidiasis like probiotic therapy & many metal Nanoparticles have been considered in the treatment of Candidiasis and have received significant results.11, 12, 13
Many Nanoparticles like, gold, silver, copper, titanium, zirconium, zinc oxide, graphene and other carbon Nanoparticles, including chitosan, have been mentioned. In between, alloy Nanoparticles, silica, metal oxides Nanoparticles and iodine have also been intended for their effects on different microorganisms including Candida.14, 15, 16, 17At present time, antifungal drugs used to treat Candidiasis are in limited use.18 A special attention is being given to Nanoparticles. Nanoparticles have a higher level of fungicidal effect than conventional antifungal medicines, as they have better penetration in host cells & tissues even in small concentrations. Antimicrobial action of some metal oxide Nanoparticles, such as zinc oxide, copper oxide, and silver oxide, have been proven through many studies.19 Some metal-oxide NPs, such as TiO2, ZrO2,Ag2O and ZnO, have proved their antimicrobial action due to its oxidative stress incited by photo generated reactive oxygen species (ROS).Nanoparticles have greater efficiency in ROS generation than their bulk materials due to their high surface area and high charge density providing them more active sites and positions.20 Titanium dioxide (Titania) is the most common antimicrobial agent used in the biomedical devices. TiO2 nanomaterial has great opportunity to encounter microbial adhesion on various dental materials and prosthesis including PMMA, Ceramic glass, stainless steel, dental implants.21 The application of 1% of Cu–Ti Oxide nanotube coatings in dental implants significantly reduces number of adherent bacteria compared to untreated Ti surfaces.22 Nanoparticles have capacity for attaching and penetrating cell walls of both Gram-positive and Gram-negative microbes through reactive ions.23 Although The antibacterial action of NPs is not yet clear but broadly their mode of action may be: (1) reaction with peptidoglycan cell wall and cell membrane subsequently cell death; (2) inhibition of protein synthesis; (3) conjugation with bacterial DNA and obstructing DNA replication.24 Most of the fungicidal activity of ZnO NPs was because of bacterial cell wall lysis.25 Graphene as nanomaterials has different active forms like layered graphene(few to multi), reduced graphene oxide, thin and ultra-thin graphite. These all forms have significant antimicrobial effect on oral biofilm.26 Zinc oxide is synthesized with graphene material and producing graphene/zinc oxide (GZNC) Nano composite, it has synergistic antimicrobial effect by producing unique Nano interface but also shown much lower toxicity as compared to ZnO alone.27
2. Materials and methods
The Pub Med/Medline was searched to identify around 100 relevant studies published from 2011 to 2020. The search strategy employed the following keywords related to “use of Nanoparticles in dentistry”, “Antimicrobial agents and PMMA”, “Candidiasis and nanomaterials”, “Prevention of oral Candidiasis”, “Incorporation of antimicrobial agents in acrylic dentures,” “treatment of denture stomatitis through Nanomaterials,” “nanoparticles as therapeutic agents for denture stomatitis” or “Nanotechnology and dentistry” or “Nanocomposites and candida infection” or “Nano drugs as antimicrobial agents” or “Nanomaterials”.
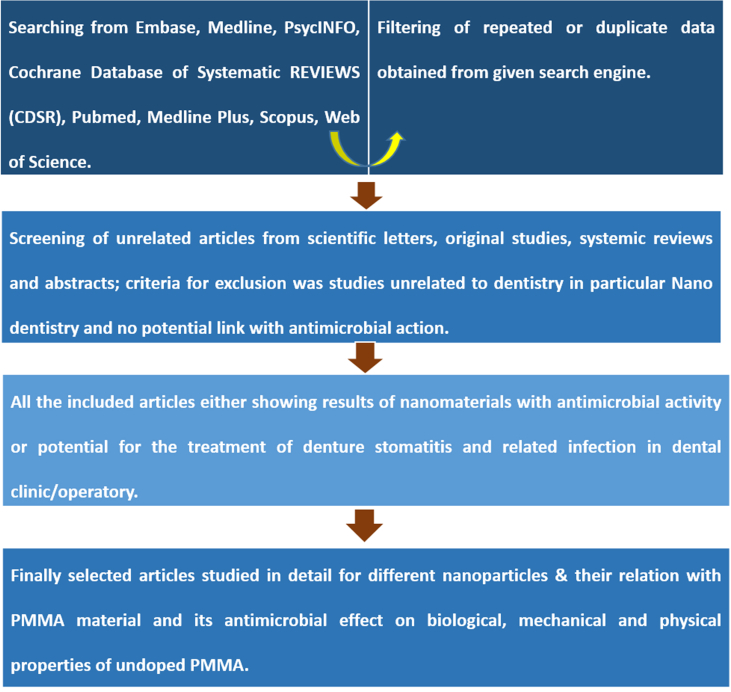
Inclusion and exclusion criteria is given in Fig. 1.
Fig. 1.
Inclusion/exclusion criteria and study flow for the systematic review.
3. Antimicrobial nanoparticles (NPs)
Nanoparticles have all the properties to vanish the microorganism presents in oral cavity having bacteria and fungi. NPs acts on these microbes by attaching and penetrating into their cell walls, which disturbs cell function by releasing active ions. Therefore, NPs are beneficial for the prevention and treatment of dental diseases including denture stomatitis. PMMA is the most common prosthetic material used for complete dentures, as it exhibits quite poor antimicrobial properties so various nanoparticles are need to incorporated into PMMA to improve its antibacterial activity. The addition of inorganic NPs such as Ag, platinum, Zn/ZnO, Ti/TiO2 and zirconium oxide (ZrO2) have shown excellent antibacterial effects.28, 29, 30, 31
4. Titanium dioxide-TiO2 (titania) NPs
TiO2 NPs have a large spectrum of activity against microorganisms in Gram-negative,Gram positive bacteria and fungi. Incorporation of silica/titania nanoparticle coating in dental prosthesis significantly reduces microbial adhesion.32 As TiO2 ratio increased in PMMA-TiO2 it improved the antimicrobial behaviour of PMMA by drastically decreasing bacterial adherence.32, 33The integration of TiO2 Nanoparticles to PMMA reduces the porosity of the denture bases. This finding revealed the aptness of metal oxide Nanoparticles as additives for the improvement of PMMA formulations since high porosities increases the growth of candida hyphae that is accountable for denture stomatitis.34
5. Silver nanoparticles (AgNPs)
Silver nanoparticles (AgNPs) have well know antimicrobial properties, perhaps they were the first in metal NPs using for inhibitions of microbial growth in various dental materials. Incorporation of AgNPs decreases microbial colonization over dental prosthesis and increases oral health.35 The PMMA containing 1 μg/ml of AgNPs shown significantly less Candida Albicans hyphae attachment compared to pure PMMA.36The synthesis of biologically active silver nanoparticles (AgNPs) have proved potential antifungal activity. This in vitro study shown that the antifungal activity of Artemisia annua synthesized AgNPs against three Candida species. These AgNPs were effective against all three species with minimum inhibitory concentration (MIC) in order of Candida glabrata>Candida tropicalis >and C. albicans.37 The miniature size of AgNPs facilitate their entry into bacterial cell membrane resulting in rapid bactericidal activity providing interference with DNA replication and protein synthesis, unwinding cell wall and also alters the base pairing of DNA subsequently respiratory failure resulting in cell death.38
6. Zirconium oxide (ZrO2) NPs
Zirconium oxide nanoparticles (ZrO2 NPs) have excellent biocompatibility. They are white in color so unlike to other metal oxide NPs, Zirconium Oxide NPs display excellent aesthetics.39It is proven by many studies that addition of ZrO2 NPs to PMMA denture base increases the density and decreases porosity which increases its flexural strength, tensile strength, and fracture toughness.40 Gad. et al. examined the effect of ZrO2NPs on C. albicans adhesion of cold-cured acrylic resin and reported that adhesion and proliferation of C. albicans were decreased in ZrO2-NPs added PMMA specimen due to its less porous and more dense lattice.41 The findings of Gowri et al., revealed that nano-ZrO2 almost showed significant inhibition effect against fungal strains by interfering in cell function and causing distortion in fungal hyphae.42
7. Zinc oxide (ZnO) NPs
Zinc oxide is well known antibacterial agent since ages.43 Even in 2000 BC; In the regime of Pharaohs of Egypt historical records confirms the use of zinc oxide as ointments for wound dressings of injuries and boils.44 Zinc Oxide nanorod arrays reduced the growth of Candida albicans in specimens by continuously releasing metal ions for two months.45 Zinc Oxide NPs have shown a significant photo-catalytic effect, which is responsible for their antimicrobial action on bacteria and fungi.46 Even in low concentration of 0.01 mg/ml, ZnO NPs showed the significantly antifungal activity against C.albicans but surprisingly the efficiency of ZnO NPs was enhanced at 0.01–5.8 mg/ml.This fungicidal action of ZnO NPs was because of damage of fungal cell membrane integrity.47
The biofilm staining, XTT analysis and quantitative analysis of adhered C. albicans revealed that Composites of PMMA doped with ZnO-NPs in concentrations of 2.5%, 5%, 7.5% by wt. have significant influence on Candida albicans solution, These studies proved the antifungal activity of both Nanocomposites PMMA–ZnO-NPs and the effectiveness of sputtering of zinc oxide nanoparticles on the PMMA.48
8. Chitosan–silver–copper nanocomposites
This Nanocomposites material provided comparable results to amphotericin B a well-known antifungal agent in vitro. The results shows that this effect was higher for copper–silver–chitosan Nanocomposites than for other nanoparticles studied. Although all these individual NPs have good antimicrobial effect but combined together have synergistic effect and have shown antifungal effects.49
9. Copper oxide (CuO) NPs
The study shows the potential antibacterial activity of Copper Oxide NPs on various cariogenic bacteria, these NPs might be good candidate control agent for preventing cariogenic activity and other dental infections. Moreover, antimicrobial action of Nano copper oxide on all three species of candida albicans, C. krusei and C. glabrata was not as much of effective as on cariogenic bacteria.50
10. Zinc Ferrite Nanoparticles (ZnFe2O4NPs)
It is confirmed that the Zinc Ferrite Nanoparticles hybrid nanostructures radially inhibit the biofilm formation of Candida albicans cells. This antimicrobial action is due to infiltration of ZnFe2O4 NPs into cell membrane and successive interaction of ZnFe2O4 NPs with Candida cells. These results specify that the Zinc Ferrite Nanoparticles hybrid nanostructures have great potential to be a material of choice to prevent candida infection in denture patients.51
11. Diamond-like Carbon(DLC) thin film
DLC thin films significantly reduced C. albicans biofilm formation on the PMMA specimen surface as compared to control group. The action of DLC was verified after seeing that these thin films were showing same results with undoped and doped with silver NPs. PMMA denture bases coated with thin film of DLC could be an alternative treatment option for the prevention of denture stomatitis.52
12. Curcumin -loaded polymeric Nanoparticles(CUR-NP)
Antimicrobial photodynamic therapy has tested as an alternative treatment for oral candidiasis. In the study encapsulation of curcumin by NPs improves the water solubility of curcumin. Nystatin was used as a positive control. Results were encouraging to show the highest reduction of Candida albicans in Nystatin group followed by Antimicrobial photodynamic therapy mediated by free curcumin. The cationic and anionic forms of CUR-NP were synthesized. Anionic CUR-NP does not have any significant antifungal effect but cationic CUR-NP diminishes Candida albicans hyphae even in dark.53
13. Graphene Oxide(GO) nanosheets
The Antimicrobial effect of GO nanosheets is excellent. In higher concentration, GO nanosheets antimicrobial action was observed more prominent to Suppress the viability of microorganisms of oral cavity. GO nanosheets mode of action was due to damage in pathogens cell wall and membrane & followed by cell lysis.54
14. Mechanism of action of nanoparticles
All the Nanoparticles have proven action on PMMA biofilm to prevent denture stomatitis. Although their mode of action is little different from each other but common pathway of all nanoparticles is shown in Fig. 2.55
Fig. 2.
Mode of action of nanoparticles.
15. Conclusion
In this analysis, applications of different Nanoparticles in dentistry are explored. The antimicrobial activities of metal and other nanoparticles are discussed. Our results validated that wide range nanoparticles have shown antimicrobial action on candida species on PMMA denture, dental implant surface, dental prostheses, orthodontics and other dental infections. Most NPs have an exceptional antimicrobial effect, but their actions are largely affected by their shapes, concentration, form and other factors. The common mode of actions of nanoparticles are discussed. In selected doses toxicity of NPs is either unknown or very less. So further more scientific research is needed to deal with mechanism and toxicity as well. Limitation of the study was that only high rated articles were selected and reviewed. As we are comfortable with English language, other languages articles were not reviewed.
Declaration of competing interest
No conflict of interest, necessary references are mentioned in the article.
Acknowledgement
We are thankful to organizers of JTACON-2020.
Contributor Information
Nafis Ahmad, Email: nahmad7@jmi.ac.in.
Zeba Jafri, Email: zjafri@jmi.ac.in.
Zishan H. Khan, Email: zishanhk@jmi.ac.in.
References
- 1.ISO/TR 10993-22 . International Organization for Standardization; 2016. Biological Evaluation of Medical Devices—Part 22: Guidance on Nanomaterials. [Google Scholar]
- 2.ISO/TS 80004-1 . International Organization for Standardization; 2010. Nanotechnologies – Vocabulary – Part 1: Core Terms. [Google Scholar]
- 3.ETPN Association . 2017. Nanomedicine—European Nanotechnology Platform. [Google Scholar]
- 4.Shah P.N., Kapoor S. Nano-Biomaterials and their biocompatibility inb restorative dentistry: a review. April 2017;6(4) P. 01-06. [Google Scholar]
- 5.Stoimenov P.K., Klinger R.L., Marchin G.L. Metal oxide Nanoparticles as bactericidal agents. Langmuir. 2002;18:6679–6686. [Google Scholar]
- 6.Monteiro D.R., Gorup L.F., Takamiya A.S. The growing importance of materials that prevent microbial adhesion: antimicrobial effect of medical devices containing silver. Int J Antimicrob Agents. 2009;34:103–110. doi: 10.1016/j.ijantimicag.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Rautemaa R., Ramage G. Oral candidosis-clinical challenges of a biofilm disease. Crit Rev Microbiol. 2011;37:328–336. doi: 10.3109/1040841X.2011.585606. [DOI] [PubMed] [Google Scholar]
- 8.Telles D.R., Karki N., Marshall M.W. Oral fungal infections: diagnosis and management. Dent Clin. 2017;61:319–349. doi: 10.1016/j.cden.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Roca I., Akova M., Baquero F. The global threat of antimicrobial resistance: science for intervention. New Microbes New Infect. 2015;6:22–29. doi: 10.1016/j.nmni.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kothavade R.J., Kura M., Valand A.G., Panthaki M. Candida tropicalis: its prevalence, pathogenicity and increasing resistance to fluconazole. J Med Microbiol. 2010;59(8):873–880. doi: 10.1099/jmm.0.013227-0. [DOI] [PubMed] [Google Scholar]
- 11.Khan S., Alam F., Azam A., Khan A.U. Gold Nanoparticles enhance methylene blue–induced photodynamic therapy: a novel therapeutic approach to inhibit Candida albicans biofilm. Int J Nanomed. 2012;7:3245. doi: 10.2147/IJN.S31219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yousefi B., Eslami M., Ghasemian A., Kokhaei P., Sadeghnejhad A. Probiotics can really cure an autoimmune disease? Gene Rep. 2019;15:100364. [Google Scholar]
- 13.Ghasemian A., Eslami M., Shafiei M., Najafipour S., Rajabi A. Probiotics and their increasing importance in human health and infection control. RMM. 2018;29(4):153–158. [Google Scholar]
- 14.Espitia P.J.P., Soares N.D.F.F., dos Reis Coimbra J.S., de Andrade N.J., Cruz R.S., Medeiros E.A.A. Zinc oxide nanoparticles: synthesis, antimicrobial activity and food packaging applications. Food Bioprocess Technol. 2012;5(5):1447–1464. [Google Scholar]
- 15.Palza H. Antimicrobial polymers with metal nanoparticles. Int. J. Mol. 2015;16(1):2099–2116. doi: 10.3390/ijms16012099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eslami M., Peyghan A.A. DNA nucleobase interaction with graphene like BC3 nano-sheet based on density functional theory calculations. Thin Solid Films. 2015;589:52–56. [Google Scholar]
- 17.Eslami M., Vahabi V., Ahmadi Peyghan A. Sensing properties of BN nanotube toward carcinogenic 4-chloroaniline: a computational study. Phys. E. 2016;76:6–11. [Google Scholar]
- 18.Chen S.C., Sorrell T.C. Antifungal agents. Med. J. Aust. 2007;187(7):404. doi: 10.5694/j.1326-5377.2007.tb01313.x. [DOI] [PubMed] [Google Scholar]
- 19.Kumar V.V., Anthony S.P. Antimicrobial studies of metal and metal oxide Nanoparticles. In: Kumar V.V., Anthony S.P., editors. Surface Chemistry of Nano Biomaterials. Elsevier; 2016. pp. 265–300. [Google Scholar]
- 20.Li Y., Zhang W., Niu J., Chen Y. Mechanism of photo generated reactive oxygen species and correlation with the antibacterial properties of engineered metal oxide nanoparticles. ACS Nano. 2012;6:5164–5173. doi: 10.1021/nn300934k. [DOI] [PubMed] [Google Scholar]
- 21.Leyland N.S., Podporska-Carroll J., Browne J., Hinder S.J., Quilty B., Pillai S.C. Highly efficient F, Cu doped TiO2 anti-bacterial visible light active photo catalytic coatings to combat hospital-acquired infections. Sci Rep. 2016;6:24770. doi: 10.1038/srep24770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hang R., Gao A., Huang X. Antibacterial activity and cytocompatibility of Cu-Ti-O nanotubes. J Biomed Mater Res. 2014;102:1850–1858. doi: 10.1002/jbm.a.34847. [DOI] [PubMed] [Google Scholar]
- 23.Cao W., Zhang Y. Development of a novel resin-based dental material with dual biocidal modes and sustained release of Ag+ ions based on photocurable core-shell AgBr/cationic polymer nanocomposites. J Mater Sci Mater Med. 2017;28 doi: 10.1007/s10856-017-5918-3. [DOI] [PubMed] [Google Scholar]
- 24.Chen R., Han Z. Antibacterial activity, cytotoxicity and mechanical behaviour of nano-enhanced denture base resin with different kinds of inorganic antibacterial agents. Dent Mater J. 2017;36:693–699. doi: 10.4012/dmj.2016-301. [DOI] [PubMed] [Google Scholar]
- 25.Suha T A., Abbas F.A. Effect of zinc oxide nanoparticles on Candida albicans of human saliva (in vitro study) Eur J Med. 2015;10:235–244. [Google Scholar]
- 26.Chatterjee N., Eom H.-J., Choi J. A systems toxicology approach to the surface functionality control of graphene-cell interactions. Biomaterials. 2014;35(4):1109–1127. doi: 10.1016/j.biomaterials.2013.09.108. [DOI] [PubMed] [Google Scholar]
- 27.Kulshrestha S., Khan S., Meena R., Singh B.R., Khan A.U. A graphene/zinc oxide nanocomposite film protects dental implant surfaces against cariogenic Streptococcus mutans. Biofouling. 2014;30(10):1281–1294. doi: 10.1080/08927014.2014.983093. [DOI] [PubMed] [Google Scholar]
- 28.Yamada R., Nozaki K. Ag nanoparticle-coated zirconia for antibacterial prosthesis. Mater. Sci. Eng. C Mater.Biol. Appl. 2017;78:1054–1060. doi: 10.1016/j.msec.2017.04.149. [DOI] [PubMed] [Google Scholar]
- 29.Suganya S., Ahila S.C. Evaluation and comparison of anti-Candida effect of heat cure polymethylmethacrylate resin enforced with silver nanoparticles and conventional heat cure resins: an in vitro study. Indian J Dent Res. 2014;25:204–207. doi: 10.4103/0970-9290.135923. [DOI] [PubMed] [Google Scholar]
- 30.Jo J.K., El-Fiqi A. Rechargeable microbial anti-adhesive polymethyl methacrylate incorporating silver sulfadiazine-loaded mesoporous silica nanocarriers. Dent Mater. 2017;33:e361–e372. doi: 10.1016/j.dental.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 31.Li Z., Sun J. Effect of a denture base acrylic resin containing silver nanoparticles on Candida Albicans adhesion and biofilm formation. Gerodontology. 2016;33:209–216. doi: 10.1111/ger.12142. [DOI] [PubMed] [Google Scholar]
- 32.Alrahlah A., Fouad H. Titanium oxide (TiO2)/polymethylmethacrylate (PMMA) denture base nanocomposites: mechanical, viscoelastic and antibacterial behavior. Materials. 2018;11:1096. doi: 10.3390/ma11071096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Totu E.E., Nechifor A.C. Poly (methyl methacrylate) with TiO2 nanoparticles inclusion for stereolithographic complete denture manufacturing—the future in dental care for elderly edentulous patients? J Dent. 2017;59:68–77. doi: 10.1016/j.jdent.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 34.Shirkavand S., Moslehifard E. Effect of TiO2 nanoparticles on tensile strength of dental acrylic resins. J Dent Res Dent Clin Dent Prospects. 2014;8:197–203. doi: 10.5681/joddd.2014.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Corrêa J.M., Mori M., Sanches H.L., Cruz ADd, Poiate E., Poiate I.A.V.P. Silver nanoparticles in dental biomaterials. Int J Biomater. 2015;485275:1–10. doi: 10.1155/2015/485275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Acosta-Torres L.S., Mendieta I., Nuñez-Anita R.E., Cajero-Ju’arez M., Castaño V.M. Cytocompatible antifungal acrylic resin containing silver nanoparticles for dentures. Int J Nanomed. 2012;7:4777–4786. doi: 10.2147/IJN.S32391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khatoon N., Sharma Y., Sardar M., Manzoor N. Mode of action and anti-Candida activity of Artemisia annua mediated-synthesized silver nanoparticles. J Mycolog Med. 2019;29:201–209. doi: 10.1016/j.mycmed.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Priyadarsini S. Nanoparticles used in dentistry: a review. J. Oral Biol. Craniofacial Res. 2018;8:58–67. doi: 10.1016/j.jobcr.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abualsaud R. Reinforcement of PMMA denture base material with a mixture of ZrO 2 nanoparticles and glass fibers. Int. J. Dentistry. 2019:1–11. doi: 10.1155/2019/2489393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmed M.A., Ebrahim M.I. Effect of zirconium oxide nano-fillers addition on the flexural strength, fracture toughness, and hardness of heat-polymerized acrylic resin. World J Nano Sci Eng. 2014:50–57. 04.02. [Google Scholar]
- 41.Gowri S., Rajiv Gandhi R., Sundrarajan M. Structural, optical, antibacterial and antifungal properties of zirconia nanoparticles by bio based protocol. J Mater Sci Technol. 2014;30(8):782–790. [Google Scholar]
- 42.Gad Inhibitory effect of ZrO2 nanoparticles on Candida Albicans”. Int J Nanomed. 2017;vol. 12:5409–5419. doi: 10.2147/IJN.S142857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frederickson C.J., Koh J.Y., Bush A.I. The neurobiology of zinc in health and disease. Nat Rev Neurosci. 2005;6:449–462. doi: 10.1038/nrn1671. [DOI] [PubMed] [Google Scholar]
- 44.Halioua B., Ziskind B. Press of Harvard University Press; Belknap: 2005. Medicine in the Days of the Pharaohs. [Google Scholar]
- 45.Eskandari M., Haghighi N., Ahmadi V., Haghighi F., Mohammadi S.H. Growth and investigation of antifungal properties of ZnO nanorod arrays on the glass. Physica B. 2011;406:112–114. [Google Scholar]
- 46.He L., Liu Y., Mustapha A., Lin M. Antifungal activity of zinc oxide nanoparticles against Botrytis cinerea and Penicillium expansum. Microbiol Res. 2011;166:207–215. doi: 10.1016/j.micres.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 47.Perez C., Pauli M., Bazevque P. An antibiotic assay by the agar well diffusion method. Acta Biologiae et Medicine Experimentalis. 1990;15:113–115. [Google Scholar]
- 48.Cierech M. Significance of polymethylmethacrylate (PMMA) modification by zinc oxide nanoparticles for fungal biofilm formation. 2016;510:323–335. doi: 10.1016/j.ijpharm.2016.06.052. [DOI] [PubMed] [Google Scholar]
- 49.Ashrafi M., Bayat M., Mortazavi P., Hashemi S.J., Meimandipour A. Antimicrobial effect of chitosan–silver–copper nanocomposite on Candida albicans. J Nanostruct Chem. 2020;10:87–95. [Google Scholar]
- 50.Amiri M., Etemadifar Z., Daneshkazemi A., Nateghi M. Antimicrobial effect of copper oxide nanoparticles on some oral bacteria and Candida species. J Dent Biomater. 2017;4(1):347–352. [PMC free article] [PubMed] [Google Scholar]
- 51.Thakur D., Govindaraju S., Yun K., Noh J.-S. Vol. 9. 2019. The Synergistic E_ect of Zinc ferrite Nanoparticles uniformly Deposited on Silver Nanowires for the Biofilm Inhibition of Candida albicans Nanomaterials; p. 1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Queiroz Effect of diamond-like carbon thin film coated acrylic resin on Candida albicans biofilm formation. J Prosthodont. 2013;22:451–455. doi: 10.1111/jopr.12029. [DOI] [PubMed] [Google Scholar]
- 53.Sakima V.T. Antimicrobial photodynamic therapy mediated by curcumin-loaded polymeric nanoparticles in a murine model of oral candidiasis. Molecules. 2018;23:2075. doi: 10.3390/molecules23082075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.He Jianliang. Killing dental pathogens using antibacterial graphene oxide. ACS Appl Mater Interfaces. 2015;7:5605–5611. doi: 10.1021/acsami.5b01069. [DOI] [PubMed] [Google Scholar]
- 55.Qais F.A., Khan M.S.A., Ahmad I., Althubiani A.S. Potential of nanoparticles in combating Candida infections. Lett Drug Des Discov. 2019;16:478–491. [Google Scholar]