This cohort study of commercially insured employees assessed the utilization and cost of a comprehensive primary care model that incorporates employer-sponsored on-site, near-site, and virtual primary care.
Key Points
Question
What are the utilization rates and costs of service of a comprehensive primary care model that incorporates employer-sponsored on-site, near-site, and virtual primary care?
Findings
In this cohort study of 23 518 commercially insured employees, the employer-sponsored services cost a mean (SD) of $87 ($32) per member per month after accounting for infrastructure and service costs, with members using the model clinics for most of their primary care having higher primary care costs but lower total health care costs in a matched cohort analysis controlling for demographics, diagnoses, and risk.
Meaning
The findings suggest that lower total health care costs per person and higher primary care costs may be associated with preferential use by lower-risk persons and/or with the use of comprehensive primary care.
Abstract
Importance
Primary care is increasingly delivered at or near workplaces, yet utilization and cost of employer-sponsored primary care services remain unknown.
Objective
To compare the health care utilization and cost of an employer-sponsored on-site, near-site, and virtual comprehensive primary care service delivery model with those of traditional community-based primary care.
Design, Setting, and Participants
This population-based cohort study of 23 518 commercially insured employees and dependents of an engineering and manufacturing firm headquartered in southern California was performed from January 1, 2016, to July 1, 2019. A subset of the population with most (≥50%) primary care visits through employer-sponsored on-site, near-site, or virtual care clinics was matched to a subset not having most such visits through the employer-sponsored clinics using propensity score matching (n = 1983 each). In sensitivity analyses, employees were matched to dependents at neighboring firms that lacked access to the employer-sponsored primary care delivery model (additional n = 1680).
Exposures
Integrated primary care, mental health, and physical therapy delivered through on-site, near-site, and virtual clinics.
Main Outcomes and Measures
Utilization (inpatient, outpatient, emergency department, pharmaceutical, radiology, and laboratory visits per 1000 member-months) and spending (2019 costs per member per month in US dollars) by service type.
Results
A total of 23 518 individuals (mean [SD] age, 27 [15] years; 14 604 [62.1%] male) were included in the full population sample and had been enrolled in the employer-sponsored health plan for a mean of 29 months (interquartile range, 14-48 months). Of eligible members, 5292 (22.5%) used the employer-sponsored services, with 2305 (9.8%) using them for most of their primary care. The mean (SD) cost of employer-sponsored service delivery was $87 ($32) per member month. Among the matched populations (mean [SD] age, 31 [11] years; 3349 [84.5%] male) of primary users vs control individuals, total spending was 45% lower per member per month (95% CI, 35%-55%; cost difference, −$167 per member per month; 95% CI, −$204 to −$130; P < .001) among users after adjustment. The lower spending was associated with lower spending on non–primary care services, such as emergency department (−33%; 95% CI, −44% to −22%) and hospital visits (−16%; 95% CI, −22% to −10%), despite higher spending on primary care (109%; 95% CI, 102%-116%) and mental health (20%; 95% CI, 13%-27%).
Conclusions and Relevance
The findings suggest that individuals who used the models’ services for most of their primary care had lower total spending despite higher primary care spending, which may be associated with self-selection of lower-risk persons to the employer-sponsored services and/or with the use of comprehensive primary care.
Introduction
Primary care has been ideally conceptualized as accessible, timely, first-contact, coordinated, long-term, and holistic ambulatory care for most common conditions and most people.1 Primary care accessibility and comprehensiveness have recently become the subjects of employer interest as employers seek to accomplish several objectives: (1) facilitating employee well-being and associated retention, (2) encouraging preventive care for employees and dependents to prevent potentially costly disease complications that often produce costs through employer-sponsored insurance and through productivity losses, and (3) potentially direct contracting with primary care organizations to help ensure quality and coordination and potentially control health care delivery costs.2,3,4,5 Primary care delivery through worksites has been piloted through a small set of employers, but evidence on the utilization and cost implications has been limited to on-site occupational health, physical therapy, or chiropractic services6,7; expansion to comprehensive primary care has been limited in part because of uncertainty about the utilization and cost implications for employers.8,9
A comprehensive primary care delivery model that incorporates workplace on-site, near-site, and virtual care services was introduced by a southern California employer (an aerospace engineering and manufacturing firm in Los Angeles County) in November 2015 and may serve as a case study for examining utilization and cost through employer-sponsored primary care. An independent primary care delivery service company was contracted by the employer to provide access to a single on-site primary care clinic at the firm's headquarters and 15 near-site primary care clinics in the same commuting zones as the firm's company locations (in the Los Angeles, California, Seattle, Washington, and Washington, DC, metropolitan areas). The primary care delivery model was based on 5 principles rooted in the primary care medical home model (Table 1).2
Table 1. Principles and Delivery Strategies Adopted by the Comprehensive Primary Care Delivery Model.
| Principle | Definition | Delivery strategy |
|---|---|---|
| Comprehensiveness | Delivering whole-person care, defined as addressing the most commonly needed ambulatory care at a single site | Having licensed, board-certified family medicine or internal medicine practitioners offering full preventive, acute, and chronic care services with the same bandwidth as a community-based, patient-centered medical home, supplemented by full-time licensed nurse practitioners, physician assistants, psychotherapists, physical therapists, and phlebotomists on site |
| Patient-centeredness | Enable patients to define needs, obtain guidance to address needs, and provide feedback that is integrated into delivery model | Offer a mobile application and website to guide patients to practitioners, supplemented by in-person patient condition–specific focus groups, patient satisfaction surveys for process improvements, and clinical grand rounds for continued medical education for practitioners on shared decision-making, motivational interviewing, mental health, and patient-centered care |
| Coordination | Practitioners should communicate easily and coordinate planning of care and execution of care plan | Having all on-site and near-site practitioners on a single integrated electronic health record, supplemented by in-person care navigators supporting patients with specific conditions (particularly mental health, cancer, and chronic diseases) to arrange follow-up care; assistance with prescription medication adherence difficulties; and to coordinate auxiliary services, such as counseling, specialist referrals, and communication back to a single assigned primary care practitioner |
| Accessibility | Minimal obstacles to obtaining primary care | Having same-day or next-day appointments guaranteed, office hours from 8 am through 5 pm or 6 pm Monday through Friday for in-person visits (with 1 near-site location having additional 8 am to 5 pm Saturday hours), around-the-clock virtual (video) visits with a licensed practitioner |
| Quality and safety | Meet practice guidelines and minimize the risk for harm | Automated screenings for depression and related conditions, health care maintenance reminders, evidence-based clinical decision support flow processes for practitioners, and drug-drug interaction checks built into the electronic health record, along with quality improvement collaborative projects to improve screening and treatment |
We sought to characterize the utilization and cost of services delivered through the employer-sponsored comprehensive primary care model. We specifically evaluated the degree of utilization and type of services used and characterized any differences among individuals who primarily used the employer-sponsored services for most of their primary care vs those who remained primary users of traditional community-based primary care services. This information may be useful for other employers interested in identifying the types of employees who may avail of the comprehensive primary care model and the implications of such utilization for health care costs.
Methods
This retrospective cohort study was approved by the Western Institutional Review Board. Claims data access was reviewed and authorized by the health plan and the independent institutional review board under the Permitted Uses and Disclosures for Health Care Operations rule of the Health Insurance Portability and Accountability Act, which allows for utilization, cost, and quality research evaluations of self-insured employer health care delivery programs without additional patient consent or authorization. The third-party claims database administrator deidentified the data using the Safe Harbor Method to avoid identifiable information from being accessible to the employer or sponsor of the clinics. Methods followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.10
Two analyses were performed: (1) a descriptive analysis of utilization and costs at the firm level, comparing on-site, near-site, and virtual care utilization and cost by type of service to their community-based equivalents, and (2) a propensity score matching–based analysis of utilization and cost differences among members who used the employer-sponsored comprehensive primary care delivery services for most of their primary care visits vs members who did not (who used traditional community-based care for most of their primary care visits). Both analyses relied on claims data from employees and covered dependents of the commercial, employer-sponsored health plan from a single firm. For the propensity score matching–based analysis, primary care evaluation and management visits were defined by the combination of having a visit in which the practitioner was considered a primary care provider per the Centers for Medicare & Medicaid Services Healthcare Provider Taxonomy (including general practice, family medicine, general internal medicine, general pediatrics, and related designations; [eTable 1 in the Supplement])11 and in which the visit type (not applicable to virtual services) was labeled with Current Procedural Terminology codes 99201 through 99205 (office-based new patient visits) or 99211 through 99215 (office-based established patient visits). Virtual visits were classified as triage encounters (telephone call with practitioner to determine future diagnosis and treatment needs), video visits (application-based visit with a primary care practitioner), “treat me now” visits (member completes an online survey for specific common symptoms, typically upper respiratory tract infections or urinary tract or gynecologic infections, and a practitioner responds via secure message within 1-4 hours), and digital dermatology (application-based visit with a dermatologist instead of a primary care practitioner). Service was not contingent on data inclusion or study participation. Employees were provided with a Notice of Privacy Practices and offered the choice of opting out of their data transmission for research purposes from the third-party health plan administrator claims database used for this research; none chose to opt out.
Setting
The primary analysis focused on a single employer’s covered population from January 1, 2016, through July 1, 2019, corresponding to the full duration of insurance claims data availability. The setting for the comprehensive primary care model was a single on-site clinic, 15 near-site clinics, and a virtual care platform (web and mobile) available to all employees and dependents. The employer subsidized the onsite clinic's fees, such that the on-site clinic and virtual visits charged $0 to employees and their dependents for all services (ie, no visit co-payment or subsequent bill), whereas the near-site clinics had no such incentive and had a $25 co-payment ($0 for virtual visits) but no deductible, except for employees on a high-deductible plan who faced a $1500 individual deductible and 0% coinsurance for all on-site visits or 20% coinsurance for all near-site visits after meeting the deductible. For this analysis, all claims from the on-site clinic were reverted to the unsubsidized contracted allowed amounts (by visit code) (eTable 2 in the Supplement) because the subsidy was paid by the employer and thereby not a true cost savings from an employer perspective. The employer had a separate occupational health service data feed, such that worksite occupational health claims were not included in the third-party claims administrative database being analyzed.
Participants
Inclusion criteria for the primary analysis was being enrolled in an employer-sponsored health plan at any point during the study period and having complete data on date of birth, sex, principal diagnostic code, place of service code, national provider identifier code of the practitioner, and allowed amount (employer plus member total spend, including the member’s coinsurance and co-payment, if any). All descriptive statistics incorporated the full enrolled population sample. The propensity score matching–based subgroup analysis involved propensity score matching between those having most of their primary care evaluation and management visits through the employer-sponsored comprehensive primary care program (the treatment group) vs not using employer-sponsored clinics (the control group). Missing data were imputed using chained equations,12 with 2% of persons having any data missing (primarily practitioner identifiers).
Outcomes
Outcomes were defined from January 1, 2017, through July 1, 2019, to permit propensity score matching based on data from the preoutcome period of January 1, 2016, through December 31, 2016 (see below). Outcomes included utilization (encounters per 1000 member-months) of the on-site, near-site, and virtual care services by primary care, mental health, and physical therapy categories compared with community-based services not part of the comprehensive primary care model. Additional outcomes for the propensity score matching–based analysis included utilization, cost (total allowed amount, including employer and member portions), and cost per utilization (unit cost), expressed as the difference between the treatment and control groups in each outcome by place of service (ie, emergency department, inpatient hospital, and radiology or imaging departments) and service type (ie, primary care, specialty care, mental health, physical therapy, drug administration, and laboratory or pathology). Place of service and service type were defined using Centers for Medicare & Medicaid Service category definitions.13 Costs were expressed in 2019 US dollars, updated for inflation from the medical service date to July 2019 using the Consumer Price Index.14
Statistical Analysis
Propensity score matching was performed based on individual characteristics during the preoutcome period of January 1, 2016, through December 31, 2016. Propensity score matching between the treatment and control groups was performed using a 1-to-1 nearest-neighbor propensity score matching algorithm15 that used a logistic regression model to estimate the propensity score for being in the treatment group, with the predictor covariates of age at enrollment, sex, risk score (using the hierarchical condition category [HCC] risk adjuster for the preoutcome period of 201616), home residence 3-digit zip code, duration of enrollment in the health plan (in months), and the Clinical Classifications Software (CCS) category17 corresponding to the persons’ most common (modal) evaluation and management visits’ principal diagnosis code for the preoutcome period of 2016 (with ties broken at random). We included all claims for propensity score matching, including those at the on-site or near-site clinic and all other clinics (ie, including outside practitioners) because the claims database included all utilization and costs at all sites for the eligible members. The HCC risk adjuster algorithm takes a combination of age, sex, and diagnostic code variables to assign the member a level of estimated chronic illness severity.16 The rationale for including age, sex, risk score, and diagnostic code was their associations with overall utilization and cost, whereas zip code is known as a socioeconomic proxy for area-level unmeasured confounders associated with health (ie, social determinants of health) and use of enrollment duration helps statistically compare individuals more vs less likely to be enrolled in a health plan for brief periods (which is associated with utilization and cost). We a priori set statistical significance to P < .05 with 2-sided hypothesis testing. Variance inflation factors for the covariates were less than 1.18.
We compared the 1-to-1 nearest-neighbor matching with exact, full, genetic, and optimal matching with an up to 1-to-5 (treatment to control) ratio and calipers that varied from 0.1 to 0.315 to verify that the 1-to-1 nearest-neighbor matching with a caliper of 0.1 produced the largest sample matched with the lowest absolute standardized difference across all covariates between matched individuals. Within the matched sample, each outcome variable was normalized by adding 1 unit and log transforming the value (eFigure 1 in the Supplement gives a quantile-quantile plot of normality). The transformation had the advantage over Poisson and negative binomial models of allowing the regression coefficients to be interpreted as percentage point changes in a value. Ordinary least-squares regression of the matched pairs was performed while controlling for age, sex, risk score, home zip code, duration of enrollment, and modal CCS diagnosis category. Regression coefficients were expressed as the percentage change in each dependent outcome variable for a 1-unit change in each independent variable.
Sensitivity analyses were performed to estimate the regression coefficients after excluding newborns; those with neonatal intensive care unit admissions, pregnancy, dialysis, hospice, rehabilitation, or organ transplant histories; members with more than $50 000 in claims spending per year; those with less than 12 months of enrollment; and those for whom the modal principal diagnosis was only a medical examination or immunization.
A second sensitivity analysis was performed in which the treatment group was matched to an alternative control group: employees and dependents enrolled in employer health plans at employers who did not provide employer-sponsored comprehensive primary care through on-site, near-site, or virtual care services within the group of 48 employers in the third-party-administrator claims data set available to us (31 497 individuals in the same zip codes as the treatment group who were rendered eligible for the match). The same inclusion criteria and propensity score matching process noted above were used for this alternative control group.
In addition to the sensitivity analyses, the E-value was computed, which is a statistic that assesses how strongly unmeasured confounders would need to be associated with being in the treated group and with the outcome of total spending to produce a false correlation from our regressions (to explain away an observed association).18,19 The E-value statistic serves as an assessment of robustness because a high E-value indicates that the associations observed are less likely to be explained away by unobserved confounding.
Analyses were performed using R statistical software, version 3.6.0 (R Foundation for Statistical Computing), using the statistical code uploaded to github.20
Results
Population Characteristics
A total of 23 518 people (mean [SD] age, 27 [15] years; 14 604 [62.1%] male) were included in the full population sample and had been enrolled in the employer-sponsored health plan for a mean of 29 months (interquartile range [IQR], 14-48 months). Descriptive statistics on the study populations’ health care utilization and cost by type of service and site of service are detailed in Table 2. During the outcome observation period of January 1, 2017, through July 1, 2019, the population had a mean (SD) primary care utilization rate of 106 (63) per 1000 member-months (median, 31 per 1000 member-months; IQR, 0-125 per 1000 member-months) and had a total medical and pharmaceutical cost (allowed amounts, including employer and member share) of $412 per member per month (PMPM) (median, $48 PMPM; IQR, $0-$240 PMPM). Users of the comprehensive primary care services tended to be older (mean [SD], 31 [9] years vs 27 [16] years), were less often female (2770 [15.2%] vs 2122 [40.1%] female), and had a lower median HCC risk score (0.002 [IQR, 0.000-0.000] vs 0.004 [IQR, 0.000-0.000]) but had a longer median duration of enrollment (33 months [IQR, 22-48 months] vs 28 months [IQR, 14-48 months]) (Table 2).
Table 2. Descriptive Statistics for the Study Population Before and After Propensity Score Matchinga.
| Characteristic | Control group | Treatment group | P value | Standardized mean difference |
|---|---|---|---|---|
| Before propensity score matching | ||||
| No. | 21 410 | 2108 | <.001 | 0.334 |
| Age, mean (SD), y | 26.6 (15.7) | 30.8 (8.7) | <.001 | 0.581 |
| Male | 12 819 (59.9) | 1788 (84.8) | .006 | 0.073 |
| HCC risk score, mean (SD) | ||||
| Including those at zero risk | 0.004 (0.034) | 0.002 (0.022) | <.001 | 0.204 |
| For those above zero risk | 0.326 (0.045) | 0.317 (0.033) | <.001 | 0.343 |
| Months of enrollment, mean (SD) | 28.3 (15.9) | 33.4 (13.9) | <.001 | 0.334 |
| Common CCS diagnostic categories | ||||
| Medical examination or evaluation | 4349 (20.3) | 402 (19.1) | NA | NA |
| Immunizations and screening for infectious disease | 858 (4.0) | 583 (27.7) | NA | NA |
| Spondylosis, intervertebral disc disorders, and other back problems | 864 (4.0) | 91 (4.3) | NA | NA |
| Other upper respiratory tract infections | 480 (2.2) | 42 (2.0) | NA | NA |
| Other nontraumatic joint disorders | 430 (2.0) | 69 (3.3) | NA | NA |
| Highest-cost CCS diagnostic categories (2019 US dollars) | ||||
| Cancer of esophagus ($72 801 PMPM) | 1 (<0.1) | 0 (0.0) | NA | NA |
| Cancer of bone and connective tissue ($60 526 PMPM) | 1 (<0.1) | 0 (0.0) | NA | NA |
| Paralysis ($59 918 PMPM) | 1 (<0.1) | 0 (0.0) | NA | NA |
| Short gestation, low birth weight, and fetal growth retardation ($45 826 PMPM) | 1 (<0.1) | 0 (0.0) | NA | NA |
| Shock ($34 680 PMPM) | 1 (<0.1) | 0 (0.0) | ||
| After propensity score matching | ||||
| No. | 1983 | 1983 | .967 | 0.001 |
| Age, mean (SD), y | 30.8 (14.1) | 30.8 (8.5) | .861 | 0.007 |
| Male | 1677 (84.6) | 1672 (84.3) | .235 | 0.038 |
| HCC risk score, mean (SD) | ||||
| Including those at zero risk | 0.003 (0.029) | 0.002 (0.023) | .106 | 0.051 |
| For those above zero risk | 0.319 (0.044) | 0.317 (0.033) | .494 | 0.022 |
| Length enrollment, mean (SD), mo | 33.6 (13.6) | 33.9 (13.7) | .967 | 0.001 |
| Common CCS diagnostic categories | ||||
| Medical examination or evaluation | 389 (19.6) | 395 (19.9) | NA | NA |
| Immunizations and screening for infectious disease | 457 (23.0) | 483 (23.4) | NA | NA |
| Spondylosis, intervertebral disc disorders, and other back problems | 98 (4.9) | 90 (4.5) | NA | NA |
| Other upper respiratory tract infections | 46 (2.3) | 42 (2.1) | NA | NA |
| Other nontraumatic joint disorders | 72 (3.6) | 68 (3.4) | NA | NA |
| Highest-cost CCS diagnostic categories (2019 US dollars) | ||||
| Chronic kidney disease ($17 637 PMPM) | 1 (<0.1) | 1 (<0.1) | NA | NA |
| Alcohol-related disorders ($4290 PMPM) | 7 (0.4) | 5 (0.3) | NA | NA |
| Intracranial injury ($4188 PMPM) | 4 (0.2) | 2 (0.1) | NA | NA |
| Thyroid disorders ($3398) | 0 | 3 (0.2) | NA | NA |
| Hepatitis ($2650) | 0 | 1 (<0.1) | NA | NA |
Abbreviations: CCS, Clinical Classifications Software; HCC, hierarchical condition category; NA, not applicable; PMPM, per member per month.
Data are presented as number (percentage) of participants unless otherwise indicated. The treatment group includes those using the subsidized on-site or near-site primary care clinics for most primary care evaluation and management visits, whereas the control group does not. The propensity score matching included all 3022 CCS categories of which the top 5 most prevalent and most costly (on a per-person basis) are listed here. To reduce the risk of identification, zip codes are not listed but were included in the propensity score matching process.
Members in the treatment group (those with >50% of their primary care visits at on-site or near-site clinics) had lower mean (SD) spending before the match ($223 [$526] PMPM [median, $72 PMPM; IQR, $29-$207 PMPM] vs $431 [$2431] PMPM [median, $44 PMPM; IQR, $0-$244 PMPM]) but had higher mean (SD) primary care spending ($26 [$42] PMPM [median, $14 PMPM; IQR, $7-$28 PMPM] vs $11 [$34] PMPM [median, $2 PMPM; IQR, $0-$13 PMPM]) and higher mean (SD) primary care utilization (165 [264] encounters per 1000 member-months [median, 91 per 1000 member-months; IQR, 44-180 per 1000 member-months] vs 100 [313] [median, 21 per 1000 member-months; IQR, 0-125 per 1000 member-months]) (Table 3). Individuals in the treatment group also had higher mean (SD) mental health utilization (50 [200] per 1000 member-months [median, 0 per 1000 member-months; IQR, 0-0 per 1000 member-months] vs 21 [211] per 1000 member-months [median, 0 per 1000 member-months; IQR, 0-0 per 1000 member-months]) but had generally lower utilization of other services besides primary care and mental health (Table 3).
Table 3. Unadjusted Outcome Rates for the Study Population Before and After Propensity Score Matching.
| Service Type | Spending, 2019 US dollars PMPM | Utilization, encounters per 1000 member-months | Spending per encounter, 2019 US dollars per encounter | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Control group | Treatment group | P value | Control group | Treatment group | P value | Control group | Treatment group | P value | |
| Before propensity score matching, mean (SD) | |||||||||
| No. | 21 410 | 2108 | NA | 21 410 | 2108 | NA | 21 410 | 2108 | NA |
| Total medical and pharmaceutical | 430.7 (2430.8) | 222.5 (526.0) | <.001 | NA | NA | NA | NA | NA | NA |
| Pharmaceutical | 50.3 (686.3) | 27.2 (163.8) | .12 | NA | NA | NA | NA | NA | NA |
| Emergency department | 26.3 (131.2) | 21.4 (125.8) | .10 | 74.4 (390.9) | 49.3 (218.3) | .004 | 405.6 (285.5) | 418.9 (359.6) | .48 |
| Hospitalization | 20.3 (353.3) | 4.1 (59.5) | .04 | 12.0 (116.7) | 3.0 (32.0) | <.001 | 1286.8 (2759.8) | 1766.2 (3933.7) | .25 |
| Primary care | 11.3 (33.8) | 26.0 (41.9) | <.001 | 100.1 (312.5) | 165.4 (264.3) | <.001 | 114.6 (46.4) | 160.1 (40.5) | <.001 |
| Specialist | 5.9 (16.4) | 2.9 (6.7) | <.001 | 53.1 (152.4) | 23.7 (51.4) | <.001 | 117.4 (50.0) | 125.7 (55.4) | <.001 |
| Mental health | 4.5 (70.3) | 9.1 (39.1) | .003 | 20.9 (211.3) | 49.6 (200.0) | <.001 | 284.3 (1268.2) | 202.1 (292.2) | .21 |
| Physical therapy | 5.9 (39.0) | 10.7 (42.6) | <.001 | 143.8 (941.3) | 172.4 (643.7) | .17 | 49.1 (60.7) | 69.7 (38.6) | <.001 |
| Drug administration | 12.0 (267.5) | 8.6 (82.8) | .56 | 108.7 (600.3) | 88.6 (235.7) | .13 | 81.1 (844.8) | 76.0 (106.5) | .85 |
| Surgery | 56.2 (698.1) | 13.6 (88.0) | .005 | 61.0 (290.0) | 27.6 (94.2) | <.001 | 567.4 (1675.9) | 362.4 (1541.4) | .006 |
| Laboratory and pathology | 8.4 (36.4) | 7.1 (16.9) | .10 | 279.3 (1063.0) | 327.4 (604.5) | .04 | 27.1 (37.2) | 26.3 (30.8) | .41 |
| Imaging | 10.9 (91.0) | 5.1 (31.5) | .004 | 54.6 (176.0) | 32.1 (88.0) | <.001 | 143.0 (200.0) | 133.6 (236.4) | .26 |
| After propensity score matching, mean (SD) | |||||||||
| No. | 1828 | 1828 | NA | 1828 | 1828 | NA | 1828 | 1828 | NA |
| Total medical and pharmaceutical | 538.0 (1933.3) | 204.5 (521.7) | <.001 | NA | NA | NA | NA | NA | NA |
| Pharmaceutical | 69.3 (442.5) | 27.8 (168.7) | <.001 | NA | NA | NA | NA | NA | NA |
| Emergency department | 36.4 (174.1) | 22.2 (128.4) | .003 | 98.4 (647.6) | 51.2 (223.1) | .002 | 413.4 (326.9) | 542.9 (530.1) | <.001 |
| Hospitalization | 32.2 (390.5) | 4.3 (61.4) | .002 | 15.2 (107.9) | 3.2 (33.0) | <.001 | 1389.7 (2695.9) | 3877.1 (5014.0) | <.001 |
| Primary care | 16.8 (36.7) | 22.7 (35.9) | <.001 | 134.0 (264.5) | 141.3 (214.6) | .34 | 127.7 (48.7) | 160.5 (40.7) | <.001 |
| Specialist | 9.7 (30.0) | 2.5 (6.1) | <.001 | 85.6 (297.6) | 19.6 (44.0) | <.001 | 115.4 (49.9) | 133.9 (50.5) | <.001 |
| Mental health | 5.7 (35.0) | 6.8 (36.5) | .32 | 30.5 (310.8) | 38.4 (186.5) | .33 | 173.9 (282.5) | 139.2 (205.2) | <.001 |
| Physical therapy | 11.3 (49.8) | 9.8 (39.5) | .31 | 255.7 (1007.2) | 163.7 (618.9) | .001 | 46.2 (42.3) | 64.5 (39.8) | <.001 |
| Drug administration | 15.3 (156.1) | 7.3 (84.8) | .04 | 138.9 (742.4) | 76.3 (224.7) | <.001 | 68.7 (148.1) | 75.7 (136.8) | .120 |
| Surgery | 52.8 (376.1) | 14.0 (90.7) | <.001 | 84.3 (313.0) | 27.0 (96.2) | <.001 | 368.1 (955.1) | 286.8 (880.8) | .005 |
| Laboratory and pathology | 14.9 (64.5) | 5.9 (15.0) | <.001 | 431.2 (1326.0) | 268.2 (455.2) | <.001 | 27.9 (37.0) | 25.5 (28.7) | .02 |
| Imaging | 13.5 (56.0) | 5.1 (32.1) | <.001 | 70.6 (161.1) | 29.1 (81.1) | <.001 | 134.5 (186.7) | 125.4 (192.0) | .13 |
Abbreviations: NA, not applicable; PMPM, per member per month.
Utilization and Cost of the Comprehensive Primary Care Model
Among the individuals in the full population sample, 5292 members (22.5%) used any aspect of the comprehensive primary care model, with 2305 (9.8%) using them for most of their primary care. Utilization rates were a mean (SD) of 64 (0.4) per 1000 member-months (with 5127 people [21.8%] in the eligible population having at least 1 visit) for the on-site clinic, 4 (0.2) per 1000 member-months (with 988 people [4.2%] in the eligible population having at least 1 visit) for the near-site clinics, and 105 (0.3) per 1000 member-months (with 1505 people [6.4%] in the eligible population having at least 1 visit) for the virtual visits. At the on-site and near-site clinics, 15 981 visits (63.4%) were for primary care evaluation and management services, 4008 (15.9%) for physical therapy visits, 2596 (10.3%) for mental health, and 2622 (10.4%) for immunizations without additional evaluation or management. The most common diagnosis categories for evaluation and management primary care visits were influenza (1007 [6.3%]) and spondylosis, intervertebral disc disorders and other back problems (288 [1.8%]), and other bone disease and musculoskeletal deformities (282 [1.8%]). Among virtual visits, 894 (31.4%) were triage encounters, 971 (34.1%) were video visits, 725 (25.5%) were “treat me now” encounters, and 254 (8.9%) were digital dermatology visits.
Although on-site users rarely overlapped with near-site users (only 588 people [2.5%] in the population using both the on-site and at least 1 near-site clinic), both on-site and near-site users often used virtual care (974 on-site users [19.0%] and 329 near-site users [33.3%] also using virtual care). Conversely, 392 virtual care users (20.0%) did not use on-site or near-site care.
The mean (SD) overall cost of the comprehensive primary care service for the users was $87 ($32) PMPM (median, $38 PMPM; IQR, $23-$86 PMPM), including infrastructure and service costs, with 47% of the cost for primary care services, 26% for physical therapy, 17% for mental health care, and 10% for immunizations. The cost includes all services provided at on-site or near-site centers for any member (not only those who mostly used the service), and the denominator of PMPM refers to all eligible members (not only those who mostly used the services).
Utilization and Cost Among Persons Primarily Using vs Not Using the Primary Care Model
A total of 1983 individuals in the treatment group were propensity score matched 1:1 with 1983 in the control group, with a standardized mean difference of less than 0.1 across all demographic and clinical characteristics (Table 2). The matched population (mean [SD] age, 31 [11] years; 3348 [84.5%] male) had been enrolled for a mean (SD) of 34 (13.7) member-months.
The matched population sample had mean (SD) total medical and pharmaceutical claims spending of $383 ($1228) PMPM (median, $89 PMPM; IQR, $32-$267 PMPM), with the highest costs by service category being for pharmaceuticals (mean [SD], $51 [$306] PMPM; median, $2 PMPM; IQR, $0-$10 PMPM, including $0 values for nonusers) followed by operations ($36 [$233] PMPM; median, $0 PMPM; IQR, $0-$29 PMPM), emergency department visits ($27 [$151] PMPM; median, $0 PMPM; IQR, $0-$0 PMPM), and hospitalizations ($21 [$226] PMPM; median, $0 PMPM; IQR, $0-$0 PMPM) (Table 3). The matched population had the highest utilization rate per 1000 member-months of laboratory encounters (mean [SD], 334 [891]; median, 147; IQR, 0-396) followed by physical therapy encounters (mean [SD], 210 [813]; median, 0; IQR, 0-42), primary care encounters (mean [SD], 133 [240]; median, 80; IQR, 32-160), and drug administration encounters, including immunizations, chemotherapy, and infusions (mean [SD], 95 [484]; median, 0; IQR, 0-100) (Table 3). The demographic, clinical, cost, and utilization differences among those using the on-site vs near-site clinics are detailed in eTable 3 in the Supplement and suggested a lower risk and cost profile among on-site than near-site users.
Three sets of statistics were estimated from the multivariable regression analyses of the matched sample to help identify the extent to which differences in total spending were associated with differences in utilization vs differences in cost per utilization episode: (1) the association of on-site or near-site clinic use with differences in spending, (2) the association of on-site or near-site clinic use with differences in utilization, and (3) the association of on-site or near-site clinic use with differences in spending per utilization episode.
As detailed below, the overall results suggested an association of on-site or near-site clinic use with lower total spending across most categories other than primary care, which was associated with lower utilization across most categories but higher spending per utilization episode (ie, higher price per episode but fewer episodes, producing overall lower spending among those with most evaluation and management visits at the on-site or near-site primary care clinics).
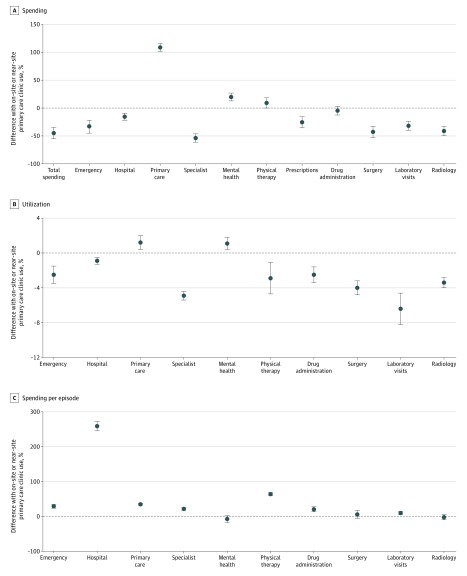
Differences in Spending
The multivariable regressions within the matched sample adjusted for age, sex, risk score, zip code, months of enrollment, and CCS diagnosis category during the preoutcome period suggested that members using the subsidized on-site or near-site primary care clinics for most of their primary care evaluation and management visits had 45% PMPM (95% CI, 35%-55% PMPM; P < .001; cost difference, −$167 PMPM; (95% CI, −$204 to −$130; unadjusted difference, 61%) lower total adjusted medical and pharmaceutical claims spending (Figure and eTable 4 in the Supplement). The largest absolute dollar difference in spending between the treatment and control populations was in emergency department spending (−$16 PMPM; 95% CI, −$21 to −$11%; P < .001) followed by surgery spending (−$14; 95% CI, −$18 to −$11; P < .001) and specialist care spending (−$11; 95% CI, −$12 to −$9, P < .001); in relative (percentage) terms, the difference in spending was the largest for specialist spending (−54%; 95% CI, −61% to −46%; P < .001) followed by surgery (−43%; 95% CI, −53% to −33%, P < .001), emergency department spending (−33%; 95% CI, −44% to −22%; P < .001), and hospital visits (−16%; 95% CI, −22% to −10%; P < .001) (eTable 4 and eFigure 2A in the Supplement). However, use of the subsidized on-site and near-site primary care clinics for the most of primary care evaluation and management visits was associated with higher primary care spending ($20 PMPM absolute; 95% CI, $19-$21; 109% relative; 95% CI, 102%-116%; P < .001) and mental health spending ($1 PMPM absolute; 95% CI, $1-$2; 20% relative; 95% CI, 13%-27%; P < .001) (eTable 4 and eFigure 2A in the Supplement), which did not fully counterbalance the lower spending in the aforementioned areas and thus the overall lower total spend.
Figure. Relative Differences in Spending, Utilization, and Spending per Encounter Based on Multivariable-Adjusted Regressions After Propensity Score Matching.
Percentage of differences in spending (US $2019) per member per month (A), percentage differences in utilization (encounters per 1000 member-months) by place of service and type of practitioner (B), and percentage differences in spending per encounter (2019 US dollars per encounter) by place of service and type of practitioner among those most commonly using subsidized on-site or near-site clinics for primary care compared with those most commonly using unsubsidized off-site clinics (C). Error bars indicate 95% CIs from multivariable regressions among matched cohorts adjusted for age, sex, risk score, home zip code, enrollment duration, and modal Clinical Classifications Software diagnosis category.
Differences in Utilization
The adjusted multivariable regressions suggested lower utilization across nearly all services categories among members using the subsidized on-site or near-site primary care clinics for most primary care evaluation and management visits (eTable 5 and eFigure 2B in the Supplement). In the multivariable-adjusted regressions, differences included reduced utilization of laboratory services (−6%; 95% CI, −8% to −4%; 22 per 1000 member-months; 95% CI, 16-29; P < .001), specialist encounters (−5%; 95% CI, −4% to −6%; 3 per 1000 member-months; 95% CI, 2-3 per 1000 member-months; P < .001), drug administration encounters (−3%; 95% CI, −2% to −4%; 3 per 1000 member-months; 95% CI, 2-4 per 1000 member-months; P < .001), surgery (−4%; 95% CI, −3% to −5%; 2 per 1000 member-months; 95% CI, 2-3 per 1000 member-months), emergency department (−3%; 95% CI, −2% to −4%; 2 per 1000 member-months; 95% CI, 1-3 per 1000 member-months; P < .001), and hospitalizations (−1%; 95% CI, −1% to −1%; 0.1 per 1000 member-months; 95% CI, 0.1-0.1 per 1000 member-months; P < .001).
Differences in Cost Per Utilization
Despite the lower utilization noted above, the adjusted multivariable regressions suggested higher cost per utilization episode for nearly all categories of service (with the exception of imaging) among members using the subsidized on-site or near-site primary care clinics for most primary care evaluation and management visits (eTable 6 and eFigure 2C in the Supplement). For primary care, encounters cost a mean (SD) of 33% (3%) more per episode (95% CI, 30%-35%; $47 per episode; P < .001) in the multivariable regressions, and costs were higher for other encounter types, including hospitalizations (246%; 95% CI, 232%-259%; $6468 per episode; P < .001), physical therapy (59.5%; 95% CI, 55%-64%; $33 per episode; P < .001), drug administration (13.4%; 95% CI, 6%-21%; $10 per episode; P < .001), and emergency department spending (24%; 95% CI, 18%-29%; $112 per episode; P < .001) in the context of overall fewer encounters. The cost per episode was, however, lower for mental health (−17%; 95% CI, −28% to −7%; −$27 per episode; P < .001) and imaging (−5%; 95% CI, −17% to −2%; −$12 per episode; P = .01).
Sensitivity Analyses
Results remained consistent in both sensitivity analyses (eTables 7-14 in the Supplement). The E-value of the association between being in the treatment group and the primary outcome of total spending difference was 2.13 (95% CI, 1.94-2.26) (ie, unmeasured confounders would have to have a risk ratio association independent of age, sex, risk score, zip code, enrollment duration, or principal diagnosis of at least 2.13 with both being in the treated group and with total spending to explain away the association between on-site or near-site clinic use and total spending).18,19
Discussion
Primary care is increasingly delivered at or near workplaces, but utilization and cost of employer-sponsored primary care services has been minimally characterized and a source of uncertainty that limits employer participation in comprehensive primary care delivery.8,9 In this study, we observed that 22.5% of eligible members used a comprehensive primary care delivery model that incorporated workplace on-site, near-site, and virtual care services sponsored by a southern California employer; 9.8% of the population used the on-site and near-site clinics for most of their primary care evaluation and management visits. The employer-sponsored services cost a mean of $87 PMPM after accounting for both infrastructure and service costs. In a matched-pair observational cohort analysis, those using on-site or near-site primary care services had lower total spending, primarily because of lower utilization of services despite services costing more per utilization episode. The results may be associated with the self-selection phenomena; that is, unmeasured differences between the matched cohorts that led members with lower utilization toward subsidized on-site or near-site primary care and away from specialists, operations, and related services (despite matching on and controlling for risk score and principal diagnosis). Alternatively, the results may be associated with the increased availability, convenience, or quality of the on-site or near-site primary care in helping to avoid utilization through effective prevention or chronic disease management, such that the remaining emergency department visits, hospitalizations, and specialist encounters had higher cost per encounter because the services were more complex and less avoidable. Both pathways may occur simultaneously because they are not mutually exclusive.
Future work may include qualitative study to identify the reasons some members choose subsidized on-site or near-site primary care, whereas others continue to go to unsubsidized off-site locations perhaps because of having an existing long-term relationship with a practitioner, which has its own potential benefits.21
Limitations
This study has limitations. First, the study was retrospective and not randomized or prospective and thus is particularly subject to selection or misclassification bias and to confounding by indication. Using the E-value statistic, we found it unlikely that the degree of association between on-site or near-site use and total spending could be fully explained away by unmeasured confounders, but such a possibility cannot be entirely eliminated. Second, the population who primarily used the on-site or near-site clinics for most primary care differed from the general population. The propensity score matching process limited our study sample to individuals who were older, were more commonly male, and had longer periods of enrollment than the general employee population at the firm being studied. The groups that were matched are likely to no longer be representative of the populations from which they were drawn; thus, any conclusions about the matched sample do not necessarily apply to the full population. The overall study sample from which the matched population was derived was working at an aerospace engineering and manufacturing firm and included participants from occupational classes including labor and professional scientific jobs. As such, further research must be conducted to determine the generalizability of our findings to other employer-sponsored insured populations. Third, we used the HCC risk score for risk adjustment because it is nonproprietary and transparent. Alternative scores are marketed as capturing greater variability in spending among commercially insured populations, although independent evaluations suggest comparability between the HCC risk adjuster and “black box” alternatives.22
Conclusions
The current study suggests high utilization of a comprehensive primary care delivery model sponsored by an employer and that those primarily using such services tended to have higher primary care and mental health utilization but lower utilization across multiple alternative care types and settings, resulting in lower total health care spending. The observed associations may be attributable to self-selection of lower-risk persons to the employer-sponsored services and/or the influence of comprehensive primary care.
eTable 1. Specialty Designations of Primary Care Providers
eTable 2. Allowed Amount Schedule (by Visit Code) for Common Current Procedural Terminology (CPT) Billing Codes
eTable 3. Unadjusted Descriptive Statistics Among Persons Primarily Using the On-Site Clinic Vs Primarily Using the Near-Site Clinics for Their Primary Care Evaluation and Management Visits
eTable 4. Percent Differences in Spending ($US 2019)
eTable 5. Percent Differences in Utilization (Encounters per 1,000 Member Months)
eTable 6. Percent Differences in Spending per Encounter ($US 2019/Encounter)
eTable 7. Sensitivity Analysis on Percent Differences in Spending ($US 2019)
eTable 8. Sensitivity Analysis on Percent Differences in Utilization (Encounters per 1,000 Member Months)
eTable 9. Sensitivity Analysis on Percent Differences in Spending per Encounter ($US 2019/encounter)
eTable 10. Descriptive Statistics for the Primary Treatment Group Versus the Alternative Control Group of Unsubsidized Members From Other Employers
eTable 11. Sensitivity Analysis of Alternative Control Group
eTable 12. Sensitivity Analysis on Percent Differences in Spending ($US 2019)
eTable 13. Sensitivity Analysis on Percent Differences in Utilization (Encounters per 1,000 Member Months)
eTable 14. Sensitivity Analysis on Percent Differences in Spending per Encounter ($US 2019/Encounter)
eFigure 1. Quantile-Quantile Plot of Log-Transformed Total Medical and Pharmaceutical Spending ($US 2019) Compared to the Theoretically-Optimal Line For Ordinary Least Squares Regression
eFigure 2. Absolute Differences in Spending, Utilization, and Spending per Encounter
References
- 1.Institute of Medicine (US) Committee on the Future of Primary Care . Donaldson MS, Yordy KD, Lohr KN, Vanselow NA. Defining primary care. In: Primary Care: America’s Health in a New Era. National Academies Press (US); 1996. Accessed August 9, 2019. https://www.ncbi.nlm.nih.gov/books/NBK232631/ [PubMed]
- 2.Jackson GL, Powers BJ, Chatterjee R, et al. The patient centered medical home: a systematic review. Ann Intern Med. 2013;158(3):-. doi: 10.7326/0003-4819-158-3-201302050-00579 [DOI] [PubMed] [Google Scholar]
- 3.Henke RM, Lenhart G, Berko J, Cutler E, Goetzel RZ. Return on investment for a payer–provider partnership to improve care management of employees and early retirees. J Occup Environ Med. 2018;60(3):241-247. doi: 10.1097/JOM.0000000000001279 [DOI] [PubMed] [Google Scholar]
- 4.McLellan RK. Work, health, and worker well-being: roles and opportunities for employers. Health Aff (Millwood). 2017;36(2):206-213. doi: 10.1377/hlthaff.2016.1150 [DOI] [PubMed] [Google Scholar]
- 5.Intensive Outpatient Care Program . A care model for the medically complex piloted by employers—DRIVE. Published September 25, 2017. Accessed September 23, 2019. https://www.commonwealthfund.org/publications/case-study/2017/sep/intensive-outpatient-care-program-care-model-medically-complex
- 6.Lord DJ, Wright JR, Fung R, et al. Integrated physical medicine at employer-sponsored health clinics improves quality of care at reduced cost. J Occup Environ Med. 2019;61(5):382-390. doi: 10.1097/JOM.0000000000001536 [DOI] [PubMed] [Google Scholar]
- 7.Kindermann SL, Hou Q, Miller RM. Impact of chiropractic services at an on-site health center. J Occup Environ Med. 2014;56(9):990-992. doi: 10.1097/JOM.0000000000000215 [DOI] [PubMed] [Google Scholar]
- 8.Shahly V, Kessler RC, Duncan I. Worksite primary care clinics: a systematic review. Popul Health Manag. 2014;17(5):306-315. doi: 10.1089/pop.2013.0095 [DOI] [PubMed] [Google Scholar]
- 9.LaPenna MA. Workplace Clinics and Employer Managed Healthcare: A Catalyst for Cost Savings and Improved Productivity. CRC Press; 2009. [Google Scholar]
- 10.Vandenbroucke JP, von Elm E, Altman DG, et al. ; STROBE Initiative . Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297. doi: 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services . Taxonomy. Accessed August 9, 2019. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/Taxonomy
- 12.van Buuren S, Groothuis-Oudshoorn K. mice: multivariable imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 13.List of Codes. November 2018. Accessed August 13, 2019. https://www.cms.gov/Medicare/Fraud-and-Abuse/PhysicianSelfReferral/List_of_Codes
- 14.CPI Inflation Calculator. Accessed August 12, 2019. https://www.bls.gov/data/inflation_calculator.htm
- 15.Ho D, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(1):1-28. doi: 10.18637/jss.v042.i08 27818617 [DOI] [Google Scholar]
- 16.Risk Adjustment CMS. Accessed August 12, 2019. https://data.nber.org/data/cms-risk-adjustment.html
- 17.Beta Clinical Classifications Software (CCS) for ICD-10-CM/PCS . Accessed August 12, 2019. https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp
- 18.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 19.Localio AR, Stack CB, Griswold ME. Sensitivity analysis for unmeasured confounding: E-values for observational studies. Ann Intern Med. 2017;167(4):285-286. doi: 10.7326/M17-1485 [DOI] [PubMed] [Google Scholar]
- 20.Github. Accessed March 19, 2020. https://github.com/CH-SanjayBasu/onemedical
- 21.DeVoe JE, Saultz JW, Krois L, Tillotson CJ. A medical home versus temporary housing: the importance of a stable usual source of care. Pediatrics. 2009;124(5):1363-1371. doi: 10.1542/peds.2008-3141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Society of Actuaries . Accuracy of Claims-Based Risk Scoring Models. Accessed August 15, 2019. https://www.soa.org/resources/research-reports/2016/2016-accuracy-claims-based-risk-scoring-models/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Specialty Designations of Primary Care Providers
eTable 2. Allowed Amount Schedule (by Visit Code) for Common Current Procedural Terminology (CPT) Billing Codes
eTable 3. Unadjusted Descriptive Statistics Among Persons Primarily Using the On-Site Clinic Vs Primarily Using the Near-Site Clinics for Their Primary Care Evaluation and Management Visits
eTable 4. Percent Differences in Spending ($US 2019)
eTable 5. Percent Differences in Utilization (Encounters per 1,000 Member Months)
eTable 6. Percent Differences in Spending per Encounter ($US 2019/Encounter)
eTable 7. Sensitivity Analysis on Percent Differences in Spending ($US 2019)
eTable 8. Sensitivity Analysis on Percent Differences in Utilization (Encounters per 1,000 Member Months)
eTable 9. Sensitivity Analysis on Percent Differences in Spending per Encounter ($US 2019/encounter)
eTable 10. Descriptive Statistics for the Primary Treatment Group Versus the Alternative Control Group of Unsubsidized Members From Other Employers
eTable 11. Sensitivity Analysis of Alternative Control Group
eTable 12. Sensitivity Analysis on Percent Differences in Spending ($US 2019)
eTable 13. Sensitivity Analysis on Percent Differences in Utilization (Encounters per 1,000 Member Months)
eTable 14. Sensitivity Analysis on Percent Differences in Spending per Encounter ($US 2019/Encounter)
eFigure 1. Quantile-Quantile Plot of Log-Transformed Total Medical and Pharmaceutical Spending ($US 2019) Compared to the Theoretically-Optimal Line For Ordinary Least Squares Regression
eFigure 2. Absolute Differences in Spending, Utilization, and Spending per Encounter