Abstract
Background
To analyze the expression of miRNA (microRNA) in peripheral blood mononuclear cells in patients with Psoriasis vulgaris with different TCM syndromes by miRNA chip. It further revealed the micromaterial basis of different syndrome types of psoriasis at the miRNA level.
Methods
Peripheral blood monocytes were collected and prepared from 30 patients with Psoriasis vulgaris (including 9 patients of blood heat syndrome, 8 patients of blood stasis syndrome, and 13 patients of blood dry syndrome) and 9 healthy controls. The miRNA expression profile of peripheral blood monocytes was detected by Agilent Hum miRNA chip.
Results
Compared to the healthy control group, 156 upregulated and 242 downregulated miRNAs were detected in all psoriasis patients. Compared to the healthy control group, 40 miRNAs were upregulated and 44 were downregulated in the blood heat syndrome group. Furthermore, there were 49 upregulated miRNAs and 44 downregulated miRNAs in the dry syndrome group as compared to the healthy control group. Also, 67 miRNAs were upregulated and 154 miRNAs were downregulated in the blood stasis syndrome group as compared to the healthy control group.
Conclusions
There are common different miRNAs and pathways, as well as specific miRNAs between the psoriasis and the healthy control groups.
Trial registration ChiCTR-TRC-14005185 registered on August 8, 2014.
Keywords: miRNA chip, miRNA expression, Psoriasis, TCM syndrome type
Background
Psoriasis is a chronic and recurrent skin inflammatory disease. In 2016, the World Health Organization (WHO) reported that the global prevalence of psoriasis ranged from 0.09 to 11.43% [1], and the incidence of psoriasis in China has increased from 0.12 to 1.49% in the past 25 years. Psoriasis has become a common disease endangering public health. Currently, there are defects in the treatment of psoriasis, such as a short remission period; also, the disease is easy to relapse or tolerate. Moreover, most drugs have considerable side effects. Traditional Chinese Medicine (TCM) treatment of psoriasis has the advantages of a long remission period, stable condition, not easy to rebound, and less toxicity and side effects. In recent years, it has attracted the attention of the medical community worldwide. Traditional Chinese medicine (TCM) has a unique theoretical system in the treatment of psoriasis and has accumulated abundant clinical experience for a prolonged period. TCM syndrome is the core of clinical TCM and vital for the modernization of TCM. Our research group analyzed the distribution of Psoriasis vulgaris-related literature from 1979 to 2010, and found that among all the syndromes of the disease, the top three were blood heat syndrome (32.86%), blood dry syndrome (23.56%), and blood stasis syndrome (19.43%), accounting for a total of 75.85% [2]. Moreover, blood stasis syndrome is related to a stable period, while the regression period is related to the blood dry syndrome [3].
Precision medicine is based on individualized medicine; it uses genomics, proteomics, and data analysis to achieve personalized and precise prevention and treatment of the diseases [4]. The connotation coincides with the doctrine “treatment based on syndrome differentiation” in traditional Chinese medicine. It can summarize the classification of TCM syndrome differentiation at the microscopic and molecular level based on the combination of genomics and proteomics to achieve accurate diagnosis and treatment as well as improve the therapeutic effect.
No correlation has been established between TCM classification of psoriasis and miRNA omics. In this study, we analyzed the differences of miRNA expression in common TCM types of psoriasis (blood heat syndrome, blood dry syndrome, and blood stasis syndrome) by miRNA microarray method and revealed the microscopic variations of the different syndrome types of psoriasis at the miRNA level.
Materials and methods
Recruitment and characteristics of patients
All patients were from the Dermatology Clinic and Ward of Guangdong Hospital of Traditional Chinese Medicine. This study was approved by the ethics committee of our hospital, and all patients and healthy individuals signed the informed consent. Psoriasis vulgaris group consisted of 30 patients, including 9 patients of blood heat syndrome, 8 patients of blood stasis syndrome, and 13 patients of the dry syndrome. The age of the patients was from 19 to 60 years, the duration of the disease was 1–10 years, the diagnostic standard was consistent with Psoriasis vulgaris [5], and the diagnosis of TCM syndrome was consistent with the diagnosis of bai bi syndrome [6]. The healthy control group comprised of 9 healthy patients as assessed in an outpatient physical examination and matched with the psoriasis group in gender and age. All the human studies were in accordance with the Helsinki declaration and Chinese relevant clinical trial research standards and regulations. All subjects included in this study were introduced to the purpose and treatment of this study by the researcher before specimen collection.
Exclusion criteria
Pregnant or lactating women; patients administered steroids and/or retinoids or biological agents in the last six months; patients who used steroids or retinoids within 1 month; patients with primary diseases such as hyperthyroidism, cardiovascular, cerebrovascular, liver, kidney and hematopoietic system, as well as those on long-term medication; a variety of Chinese medicine syndrome type inclusion of patients.
Instruments and reagents
TRI Reagent (catalogue no. T9424; Sigma, Germany), miRNeasy Micro Kit (cat alogue no. T9424 217084; Qiagen, Germany), RNase-Free DNase Set (cat alogue no. 79254; Qiagen), Tiangen miRcute miRNA cDNA First-Strand Synthesis Kit (cat alogue no. KR201; Tiangen, Beijing, China), SYBR Green PCR kit (cat alogue no. Fp411-02; Tiangen, Beijing, China), Agilent Bioanalyzer 2100 analyzer (Agilent Technologies, Santa Clara, CA, USA); Scanner G2505C (Agilent Technologies), feature extraction (version 10.7.1.1, Agilent Technologies), data processing software Genespring (version 13.1, Agilent Technologies), and Affymetrix Agilent Human miRNA, Release 21.0 (8 × 60K, Design ID: 070156) chip were utilized for this study.
Sample collection and processing
A volume of 10 mL elbow vein blood was collected in an anticoagulant tube containing heparin, and peripheral blood monocytes (PBMCs) were separated according to the manufacturer’s instructions and stored at − 80 °C.
Extraction and quality control of RNA
Total RNA was extracted using TRI reagent according to the manufacturer’s protocol and purified using the miRNeasy Micro Kit and RNase-Free DNase Set. During each RNA extraction experiment, a control total RNA was utilized as positive quality control and RNase-free water as negative quality control. After quality control (QA) evaluation, the integrity of the purified total RNA was detected by Agilent Bioanalyzer 2100 (Agilent technologies).
Agilent miRNA microarray experiment
The chip used in this study was Agilent Human miRNA, Release 21.0 (8 × 60K, Design ID: 070156), and a total of 39 samples were on-chip and analyzed. Total RNA was quantified by NanoDrop ND-2000 (Thermo Scientific, MA, USA) and detected by Agilent Bioanalyzer 2100. After passing the RNA quality inspection, the samples were labeled, hybridized, and eluted according to the standard chip procedure. First, total RNA was dephosphorylated and denatured, followed by labeling with cyanine-3-CTP (Cy3). The labeled RNA was purified and hybridized with the chip. After elution, the original image was scanned by Agilent Scanner G2505C.
Feature Extraction software was used to extract the original data from the original image, and Genespring software was utilized for standardization and subsequent processing. The standardized data were filtered, and at least one set of 100% probes labeled “Detected” from each set of samples used for comparison was stored for subsequent analysis. P-values and multiple change values of T-test were used to screen differential miRNAs, and the screening criteria were upregulated or downregulated multiple change value ≥ 2.0 and P ≤ 0.05. Then, three databases (TargetScan, microRNA.org, PITA) were used to jointly predict the target genes of different miRNAs, followed by GO and KEGG enrichment analysis of the target genes to determine the biological functions or pathways mainly affected by different miRNAs. Finally, unsupervised hierarchical clustering was carried out for different miRNAs, and the expression patterns of different miRNAs in different samples were displayed in the form of a heatmap.
Validation by quantitative real-time polymerase chain reaction (qRT-PCR)
The isolated RNA from the PBMC samples from different groups was reverse transcribed directly into cDNA using a SuperScript IV Reverse Transcriptase (Thermo Fisher, Dalian, China) according to the manufacturer’s instructions. PCR amplification conditions were as follows: initial denaturation at 95 °C for 15 min, followed by 40 cycles of denaturation at 94 °C for 20 s and annealing at 60 °C for 34 s. The expression of microRNAs was examined using qRT-PCR by a SYBR Green PCR Kit.
Statistical analysis
Statistical analyses were performed using SPSS software 19.0 and represented using GraphPad Prism 5.0 (La Jolla, CA, USA). The results are expressed as means ± standard errors of the means. Student’s t-test was used for the statistical analysis. P-values < 0.05 were considered significant.
Results
Quality control of RNA chip data is satisfactory
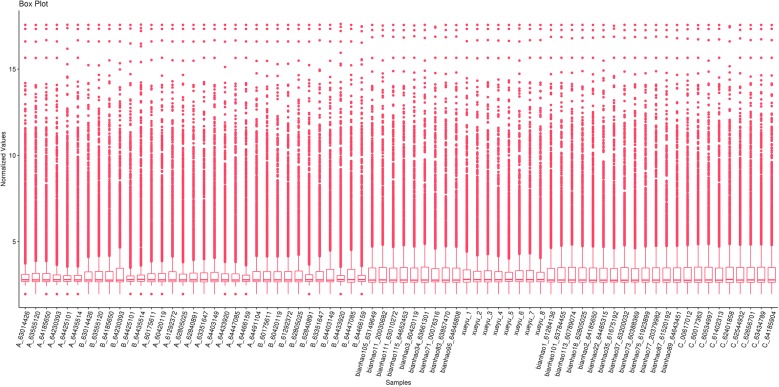
Combined with the clinical sample information, we selected 39 samples (9 samples of hematic psoriasis, 13 samples of dry psoriasis, 8 samples of blood stasis psoriasis, and 9 samples of the control group) to perform Agilent miRNA microarray analysis. The quality control of the original result data was satisfactory (Fig. 1).
Fig. 1.
Quality control of RNA chip data is satisfactory
Analysis of miRNA microarray results of blood heat syndrome and control groups
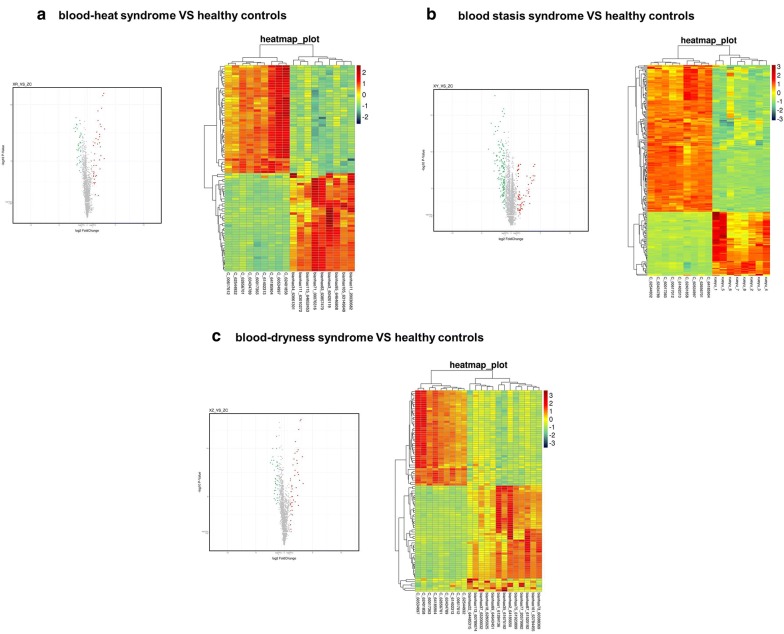
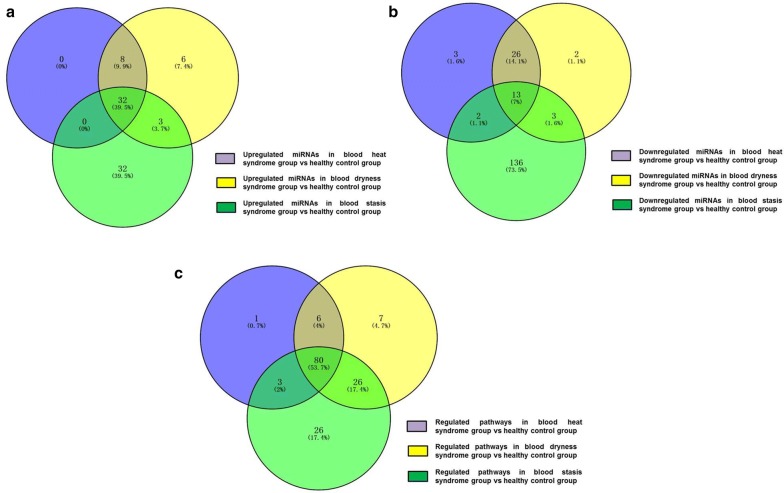
Next, we conducted a preliminary analysis of miRNA microarray results from the blood heat syndrome and the control groups, and miRNAs with fold-change > 2 and P-value < 0.05 were screened out. Among these differential miRNAs, 40 were upregulated and 44 were downregulated. The Volcano Map was used to reflect the differences in the expression of miRNAs between the blood heat syndrome and the control groups (Fig. 2). The heatmap displayed the results of unsupervised hierarchical clustering of miRNAs differences between both groups (Fig. 2). In addition, Venn analysis of the differentially expressed genes compared the miRNA microarray data from both groups (Fig. 3).
Fig. 2.
Volcanic map (left panel) and heat map (right) show the distribution of miRNAs in three different syndromes
Fig. 3.
Wayne analysis of differential miRNAs and pathways between three syndromes of psoriasis and healthy control groups
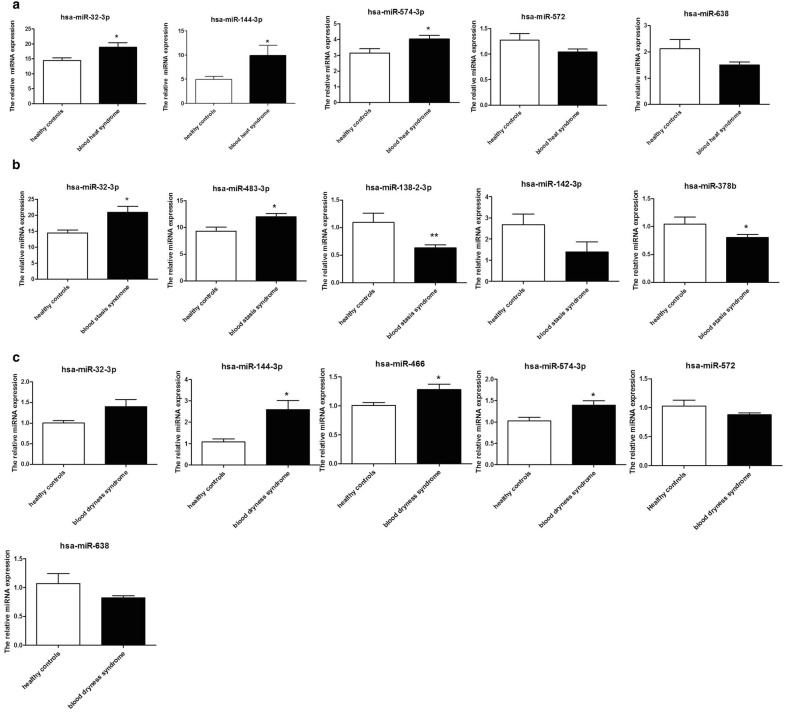
According to the results of the miRNA microarray, the first three upregulated miRNAs were miR-32-3p, miR-144-3p, and -miR-574-3p, and the first two downregulated miRNAs were miR-638 and miR-572. The verification results of qRT-PCR were consistent with those of miRNA microarray (Fig. 4).
Fig. 4.
Differential miRNAs validated by qRT-PCR (*P < 0.05, **P < 0.01 in qRT-PCR verification while comparing the data of different syndrome groups to the healthy control group)
Analysis of miRNA microarray results of psoriasis blood dry syndrome and control groups
Herein, we conducted a preliminary analysis of miRNA microarray results in the blood dry syndrome and the control groups and miRNAs with fold-change > 2 and P-value < 0.05 screened out. Among these differential miRNAs, 49 were upregulated and 44 were downregulated. The Volcano Map reflected the differences in the expression of miRNAs between the blood dry syndrome and the control groups (Fig. 2), while the Heatmap showed the results of unsupervised hierarchical clustering of miRNA differences between both control group (Fig. 2). We also performed a Venn analysis of the differentially expressed genes to compare the miRNA microarray data in the blood dry syndrome and control groups (Fig. 3).
According to the results of miRNA microarrays, the first four upregulated miRNAs were miR-144-3p,miR-32-3p, miR-574-3p, and miR-466, and the first two down-regulated miRNAs were miR-638 and miR-572, and the verification results of qRT-PCR were consistent with the results of miRNA microarray (Fig. 4).
Analysis of miRNA microarray results of psoriasis blood stasis syndrome and control groups
A preliminary analysis of miRNA microarray results was conducted in the blood stasis syndrome and the control groups, and miRNAs with fold-change > 2 and P-value < 0.05 were screened out. Among these differential miRNAs, 67 were upregulated and 154 were downregulated. The Volcano Map was used to reflect the differences in the expression of miRNAs between the blood stasis syndrome and the control groups (Fig. 2), and Heatmap showed the results of unsupervised hierarchical clustering of miRNAs differences between both groups (Fig. 2). Next, a Venn analysis of the differentially expressed genes was used to compare the miRNA microarray data from both group (Fig. 3).
According to the results of miRNA microarray, the first two upregulated miRNAs were miR-32-3p and miR-483-3p, and the first three downregulated miRNAs were miR-138-2-3p, miR-378b, and miR-142-3p; also, the verification results of qRT-PCR were consistent with those of miRNA microarray (Fig. 4).
miRNA-enrichment pathways and of the three psoriasis syndromes were analyzed from the control group
After the target gene prediction of the different miRNAs in the control group, we used three databases (TargetScan, microRNA.org, and PITA) to enrich the pathways for the three psoriasis syndromes. Venn analysis was performed on the pathways of the three syndromes (Fig. 3).
As seen from Table 1, the unique differential pathway in the psoriatic blood heat syndrome group was pancreatic secretion, while that in the psoriatic blood dry syndrome group included Shigellosis, bacterial invasion of epithelial cells, endocrine, and other factor-regulated calcium reabsorption and Th17 cell differentiation. The unique differential pathway in the psoriatic blood stasis syndrome group included human T-cell leukemia virus 1 infection, calcium signaling pathway, and ECM-receptor interaction.
Table 1.
Common and specific regulated pathways in different syndromes
| The common pathways between the three syndromes (1) | The common pathways between the three syndromes (2) | Specific pathways in blood heat syndrome | Specific pathways in blood dryness syndrome | Specific pathways in blood stasis syndrome |
| Signaling pathways regulating pluripotency of stem cells | Thyroid hormone signaling pathway | Pancreatic secretion | Shigellosis | Human T-cell leukemia virus 1 infection |
| Proteoglycans in cancer | Glutamatergic synapse | Bacterial invasion of epithelial cells | Calcium signaling pathway | |
| Breast cancer | Arrhythmogenic right ventricular cardiomyopathy (ARVC) | Endocrine and other factor-regulated calcium reabsorption | ECM-receptor interaction | |
| Transcriptional misregulation in cancer | Hedgehog signaling pathway | Th17 cell differentiation | Cell cycle | |
| Gastric cancer | Circadian entrainment | Insulin secretion | Inositol phosphate metabolism | |
| Hepatocellular carcinoma | Non-small cell lung cancer | Glucagon signaling pathway | Glycosaminoglycan biosynthesis—heparan sulfate/heparin | |
| Parathyroid hormone synthesis, secretion and action | Long-term depression | Epithelial cell signaling in Helicobacter pylori infection | Type II diabetes mellitus | |
| Wnt signaling pathway | Neurotrophin signaling pathway | Measles | ||
| Focal adhesion | Phospholipase D signaling pathway | Mitophagy—animal | ||
| EGFR tyrosine kinase inhibitor resistance | Human papillomavirus infection | Amyotrophic lateral sclerosis (ALS) | ||
| Axon guidance | Renal cell carcinoma | Hippo signaling pathway—multiple species | ||
| Rap1 signaling pathway | Endometrial cancer | Protein digestion and absorption | ||
| Ras signaling pathway | mRNA surveillance pathway | Osteoclast differentiation | ||
| MAPK signaling pathway | Cholinergic synapse | NF-kappa B signaling pathway | ||
| TGF-beta signaling pathway | Choline metabolism in cancer | Nicotine addiction | ||
| Adherens junction | Adrenergic signaling in cardiomyocytes | Synaptic vesicle cycle | ||
| Glioma | GnRH signaling pathway | Apoptosis—multiple species | ||
| Melanoma | Yersinia infection | Apoptosis | ||
| FoxO signaling pathway | Long-term potentiation | Glycosaminoglycan biosynthesis—chondroitin sulfate /dermatan sulfate | ||
| Oxytocin signaling pathway | Insulin resistance | Platinum drug resistance | ||
| Prostate cancer | Ubiquitin mediated proteolysis | Vasopressin-regulated water reabsorption | ||
| cAMP signaling pathway | Platelet activation | SNARE interactions in vesicular transport | ||
| Hippo signaling pathway | Human cytomegalovirus infection | Cocaine addiction | ||
| Cushing syndrome | AMPK signaling pathway | JAK-STAT signaling pathway | ||
| Prolactin signaling pathway | Insulin signaling pathway | RNA transport | ||
| Circadian rhythm | Relaxin signaling pathway | Other types of O-glycan biosynthesis | ||
| Dopaminergic synapse | Cellular senescence | |||
| Regulation of actin cytoskeleton | Fluid shear stress and atherosclerosis | |||
| Gap junction | TNF signaling pathway | |||
| Melanogenesis | Tight junction | |||
| cGMP-PKG signaling pathway | Chagas disease (American trypanosomiasis) | |||
| Endocrine resistance | Dilated cardiomyopathy (DCM) | |||
| Apelin signaling pathway | Longevity regulating pathway | |||
| Colorectal cancer | Pancreatic cancer | |||
| Endocytosis | Longevity regulating pathway—multiple species | |||
| Basal cell carcinoma | Sphingolipid signaling pathway | |||
| Chronic myeloid leukemia | Central carbon metabolism in cancer | |||
| PI3K-Akt signaling pathway | Aldosterone-regulated sodium reabsorption | |||
| Morphine addiction | mTOR signaling pathway | |||
| ErbB signaling pathway | Small cell lung cancer |
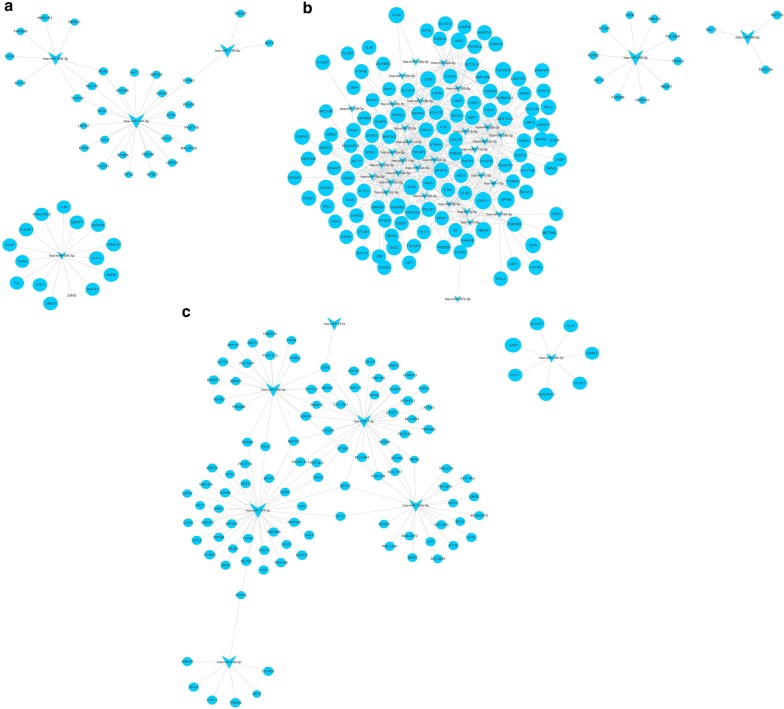
Furthermore, the DIANA TOOLS online tool and its three databases (TarBase v7.0, microt-cds (v 5.0) and TargetScan) were used to correlate the differentially expressed miRNAs and genes (Fig. 5).
Fig. 5.
Correlation analysis of differentially expressed miRNAs and genes between three syndromes of psoriasis and healthy control groups. a Correlation analysis of differentially expressed miRNAs and genes between blood-heat syndrome and healthy control groups. b Correlation analysis of differentially expressed miRNAs and genes between blood-stasis syndrome and healthy control groups. c Correlation analysis of differentially expressed miRNAs and genes between blood-dryness syndrome and healthy control groups
Discussion
In this study, miRNA microarray was used to analyze the three most common TCM types of psoriasis at the level of miRNA expression. First, a preliminary analysis of miRNA microarray results was conducted and miRNAs with fold-change > 2 and P-value < 0.05 were screened out. Among these differential miRNAs, 40 were upregulated and 44 were downregulated in patients with blood heat, 49 were upregulated and 44 were downregulated in patients with blood dry, and 67 were upregulated and 154 were downregulated in patients with blood stasis as compared to the normal group. The comparison of the miRNA microarray data of the three psoriasis types of blood heat, blood stasis, and blood dry to that of the control group found that the three types of psoriasis had unique but different miRNAs as well as common miRNAs.
In the current analysis, compared to the control group, we found that the three syndromes of psoriasis had a common upregulated different miRNA: mir-32-3p. Reportedly, this miRNA is related to malignant pleural mesothelioma, acute ischemic stroke, chronic rhinosinusitis, and is also a potential biomarker [7–9]. The upregulation of miR-144-3p in both hematopoiesis and dry inhibits cell proliferation by negative regulation of the expression of Tie2 in pulmonary microvascular endothelial cells (PMVECs), and the overexpression of miR-144-3p can be used in the treatment of hepatopulmonary syndrome (HPS) [10]. In addition, miR-144-3p is significantly increased in the bone marrow and peripheral blood of patients with acute myeloid leukemia. miR-144-3p promotes the proliferation of HL-60 cells by inhibiting NRF2. Therefore, miR-144-3p can be considered as a non-invasive biological marker of leukemia [11]. The expression of miR-574-3p is upregulated in the syndrome of blood heat and dry, and the automatic regulation feedback loop of iASPP/p63 requires miR-574-3p to regulate homeostasis of the tunable and stratified epithelium [12]. In addition, miR-574-3p is also involved in the adipogenesis of the sebaceous gland [13]. The upregulation of miR-466 in dry syndrome is related to host immunity in the skin [14] and is involved in skin and mucosal HPV infection [15]. The upregulation of miR-483-3p in blood stasis syndrome is significantly increased in the plasma of pancreatic cancer patients [16], which suggests poor prognosis in pancreatic duct adenocarcinoma patients [17]. The miR-638 and miR-572 are significantly downregulated in basal cell carcinoma [18], suggesting their involvement in the pathogenesis of the disease. The downregulated miR-378b in blood stasis syndrome promotes keratinocyte differentiation by acting on NKX3.1 [19]. In addition, the downregulated miR-142-3p in blood stasis syndrome is a RANKL-dependent inducer of osteoclast death [20].
Next, we predicted the different miRNA target genes between the three syndromes and the control group and carried out KEGG enrichment. After Venn analysis on the pathway, we found that the three syndromes had a common as well as a specific pathway. The common different pathways of the three syndromes, signaling pathways regulating the pluripotency of stem cells, needed the activation of MAPK and PI3K signaling pathways that are closely related to the occurrence of psoriasis [21]. A PI3K-Akt signaling pathway is associated with the occurrence and development of psoriasis. A previous study reported that PI3K signaling regulates the proliferation of keratinocytes by activating Akt and other targets and inducing the downregulation of FOXO [22]. In addition, the PI3K-Akt-mTOR pathway induces keratinocyte proliferation and inflammatory cytokine secretion by inhibiting autophagy in keratinocytes. The inhibition of the PI3K-Akt-mTOR pathway alleviates the psoriasis symptoms [23–28]. The common different pathways of the three syndromes include the MAPK signaling pathway. The MAPK signaling pathway is a serine/threonine protein kinase, which mainly includes extracellular signal-regulated protein kinases (ERK), C-jun N-terminal kinases (JNK), and p38 MAPK. Some studies have shown that excessive activation of p38 MAPK leads to decreased function of the skin barrier in psoriasis as well as skin inflammation [29–32].
The common pathway of the three syndromes is axon guidance, which is involved in the occurrence and development of psoriasis. Reportedly, the axonal guide molecules, CD100 and Plexin-B2, are involved in the inflammatory process of psoriasis by activating NF-κB and NLRP3 inflammasome in keratinocytes [33].
The specific pathway of dry psoriasis includes Th17 cell differentiation. Genetic studies have reinforced that Th17 cells play a central role in psoriasis [34]. These cells are responsible for the production of the cytokine IL-17A. TGF- β with IL -6 or IL -21 causes initial CD4+ T cells to differentiate into the Th17 subgroup, and IL -23, which is the growth-stabilizing factor that affects the normal secretion process of IL-17. A large number of Th17 cells were infiltrated into the lesions of psoriasis. Lewis et al. [35] isolated and counted Th17 cells in the plaque tissues of patients, and found the proportion of CD4+ Th cells was 49–93%. Th17 cells exert an effect by secreting IL-17A, IL-17F, IL-26, and TNF in psoriasis, forming a feedforward inflammatory network with KCs, activating STAT-1 and NF-κB signaling pathway, and inducing keratinocytes (KCs) to secrete several pro-inflammatory factors. IL-17 and TNF can jointly stimulate the high expression of KCs CCL20 [36] to collect the activated CD11c + macrophage-derived dendritic cells (mDCs) and adjacent CCR6 + T17 cells and induce the differentiation of T cells in skin drainage lymph nodes towards Th17 and Tc17.
The human T-cell leukemia 1 infection pathway is abnormal in blood stasis psoriasis. A previous study showed that ustekinumab could successfully treat psoriasis with human -cell leukemia/type 1 lympho virus infection [37]. Further analysis found that osteoclast differentiation, a unique pathway, was abnormal in blood stasis psoriasis. Raimondo et al. demonstrated that skin inflammation in psoriasis promoted the differentiation of human monocytes into active osteoclasts and bone injury [38].
Conclusions
In this study, we connected three common TCM syndromes of psoriasis with miRNAs and provided a reference for understanding the TCM syndromes of psoriasis. In the future study, we will explore the mechanism of the differentially expressed miRNAs from different TCM syndromes.
Acknowledgements
Not applicable.
Abbreviations
- TCM
Traditional Chinese Medicine
- PBMCs
Peripheral blood mononuclear cells
- qRT-PCR
Quantitative real-time polymerase chain reaction
- miRNA
microRNA
- PMVECs
Pulmonary microvascular endothelial cells
- HPS
Hepatopulmonary syndrome
- ERK
Extracellular signal-regulated protein kinases
- JNK
C-jun N-terminal kinases
- KCs
Keratinocytes
- mDCs
Macrophage-derived dendritic cells
Authors’ contributions
All authors have participated extensively in the study and had proofread the final manuscript. CJL, LH and HJG conceived and designed the research. YL and YQ conducted the experiments. YHY, DNY, HD, JWD, and SYY collected patients. QBC helped sample preservation and transportation. YL and YQ analyzed the data. YL wrote the manuscript. CJL, LH and HJG approved and reviewed the final manuscript. All authors read and approved the final manuscript.
Funding
This research was financially supported by the Guangdong Province Science and Technology Planning Project (2017A050506041, 2017B030314166); the Guangdong Provincial Department of Education Project (2018KQNCX046); the Guangzhou Science and Technology Project (201807010051) and the Guangdong Provincial Hospital of Chinese Medicine Special Fund (YN2018HK01, YN2018ZD08, YN2018RBA02, YN2016XP02, YN2019QJ04, YN2019QJ08).
Availability of data and materials
The datasets used and/or analyzed during the current study would be available from the corresponding author on reasonable request.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of Guangdong Provincial Hospital of Chinese Medicine Clinical Research Ethics Committee (Ethical approval No. B2012-53-03) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all eligible participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hengjun Gao, Email: hengjun_gao@shbiochip.com.
Ling Han, Email: linghan36@163.com.
Chuanjian Lu, Email: luchuanjian888@vip.sina.com.
References
- 1.World Health Organization . Global report on psoriasis. Geneva: WHO; 2016. pp. 7–9. [Google Scholar]
- 2.Lu CJ, Zeng Z, Xie XL, Ning J. Distribution of Chinese Medical Syndrome in ordinary psoriasis: literature from 1979 to 2010. J Tradit Chin Med. 2012;53(11):959–961. [Google Scholar]
- 3.Yan YH, Lu CJ, Yao DN, Du H, Li HL. Study on the correlation between the basic Syndrome of traditional Chinese Medicine and the stage and condition of Psoriasis vulgaris. J Guangzhou Univ Tradit Chin Med. 2012;04:22–26. [Google Scholar]
- 4.Li XH, Jia LL, Liu XX. Preliminary discussion of diagnosis and treatment mode of future medicine from treating based on syndrome differentiation and precision medicine. Chin J Tradit Chin Med. 2018;33(11):4789–4792. [Google Scholar]
- 5.Boehncke WH, Schön MP. Psoriasis. Lancet. 2015;386(9997):983–994. doi: 10.1016/S0140-6736(14)61909-7. [DOI] [PubMed] [Google Scholar]
- 6.Lu CJ, Yu JJ, Deng JW. Disease-syndrome combination clinical study of psoriasis: present status, advantages, and prospects. Chin J Integrat Med. 2012;18(3):166–171. doi: 10.1007/s11655-012-1006-1. [DOI] [PubMed] [Google Scholar]
- 7.Xuan L, Luan G, Wang Y, Lan F, Zhang X, Hao Y, et al. MicroRNAs regulating mucin type O-glycan biosynthesis and transforming growth factor beta signaling pathways in nasal mucosa of patients with chronic rhinosinusitis with nasal polyps in Northern China. Int Forum Allergy Rhinol. 2019;9(1):106–113. doi: 10.1002/alr.22230. [DOI] [PubMed] [Google Scholar]
- 8.Li P, Teng F, Gao F, Zhang M, Wu J, Zhang C. Identification of circulating microRNAs as potential biomarkers for detecting acute ischemic stroke. Cell Mol Neurobiol. 2015;35(3):433–447. doi: 10.1007/s10571-014-0139-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bononi I, Comar M, Puozzo A, Stendardo M, Boschetto P, Orecchia S, et al. Circulating microRNAs found dysregulated in ex-exposed asbestos workers and pleural mesothelioma patients as potential new biomarkers. Oncotarget. 2016;7(50):82700–82711. doi: 10.18632/oncotarget.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang C, Lv K, Chen B, Yang Y, Ai X, Yu H, et al. miR144-3p inhibits PMVECs excessive proliferation in angiogenesis of hepatopulmonary syndrome via Tie2. Exp Cell Res. 2018;365(1):24–32. doi: 10.1016/j.yexcr.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Sun X, Liu D, Xue Y, Hu X. Enforced miR-144-3p expression as a non-invasive biomarker for the acute myeloid leukemia patients mainly by targeting NRF2. Clin Lab. 2017;63(4):679–687. doi: 10.7754/Clin.Lab.2016.161116. [DOI] [PubMed] [Google Scholar]
- 12.Chikh A, Matin RN, Senatore V, Hufbauer M, Lavery D, Raimondi C, et al. iASPP/p63 autoregulatory feedback loop is required for the homeostasis of stratified epithelia. EMBO J. 2011;30(20):4261–4273. doi: 10.1038/emboj.2011.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schneider MR, Samborski A, Bauersachs S, Zouboulis CC. Differentially regulated microRNAs during human sebaceous lipogenesis. J Dermatol Sci. 2013;70(2):88–93. doi: 10.1016/j.jdermsci.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Wu J, Gong H, Bai Y, Zhang W. Analyzing the miRNA-Gene Networks to Mine the Important miRNAs under Skin of Human and Mouse. Biomed Res Int. 2016;2016:5469371. doi: 10.1155/2016/5469371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gu W, An J, Ye P, Zhao KN, Antonsson A. Prediction of conserved microRNAs from skin and mucosal human papillomaviruses. Arch Virol. 2011;156(7):1161–1171. doi: 10.1007/s00705-011-0974-3. [DOI] [PubMed] [Google Scholar]
- 16.Abue M, Yokoyama M, Shibuya R, Tamai K, Yamaguchi K, Sato I, et al. Circulating miR-483-3p and miR-21 is highly expressed in plasma of pancreatic cancer. Int J Oncol. 2015;46(2):539–547. doi: 10.3892/ijo.2014.2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang C, Sun Y, Wu H, Yu S, Zhang L, Meng Y, et al. Elevated miR-483-3p expression is an early event and indicates poor prognosis in pancreatic ductal adenocarcinoma. Tumour Biol. 2015;36(12):9447–9456. doi: 10.1007/s13277-015-3690-x. [DOI] [PubMed] [Google Scholar]
- 18.Sand M, Skrygan M, Sand D, Georgas D, Hahn SA, Gambichler T, et al. Expression of microRNAs in basal cell carcinoma. Br J Dermatol. 2012;167(4):847–855. doi: 10.1111/j.1365-2133.2012.11022.x. [DOI] [PubMed] [Google Scholar]
- 19.Wang XL, Zhang T, Wang J, Zhang DB, Zhao F, Lin XW, et al. MiR-378b promotes differentiation of keratinocytes through NKX3.1. PLoS ONE. 2015;10(8):e0136049. doi: 10.1371/journal.pone.0136049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fordham JB, Guilfoyle K, Naqvi AR, Nares S. MiR-142-3p is a RANKL-dependent inducer of cell death in osteoclasts. Sci Rep. 2016;6:24980. doi: 10.1038/srep24980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harding A, Cortez-Toledo E, Magner NL, Beegle JR, Coleal-Bergum DP, Hao D, et al. Highly efficient differentiation of endothelial cells from pluripotent stem cells requires the MAPK and the PI3K pathways. Stem Cells. 2017;35(4):909–919. doi: 10.1002/stem.2577. [DOI] [PubMed] [Google Scholar]
- 22.Zhang M, Zhang X. The role of PI3K/AKT/FOXO signaling in psoriasis. Arch Dermatol Res. 2019;311(2):83–91. doi: 10.1007/s00403-018-1879-8. [DOI] [PubMed] [Google Scholar]
- 23.Lu Y, Wang AL, Zhang JW, Li L, Wei JA, Li L, et al. PSORI-CM02 ameliorates psoriasis in vivo and in vitro by inducing autophagy via inhibition of the PI3K/Akt/mTOR pathway. Phytomedicine. 2019;64:153054. doi: 10.1016/j.phymed.2019.153054. [DOI] [PubMed] [Google Scholar]
- 24.Said A, Bock S, Lajqi T, Muller G, Weindl G. Chloroquine promotes IL-17 production by CD4 + T cells via p38-dependent IL-23 release by monocyte-derived Langerhans-like cells. J Immunol. 2014;193(12):6135–6143. doi: 10.4049/jimmunol.1303276. [DOI] [PubMed] [Google Scholar]
- 25.Wang RC, Levine B. Calcipotriol induces autophagy in HeLa cells and keratinocytes. J Invest Dermatol. 2011;131(4):990–993. doi: 10.1038/jid.2010.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajawat Y, Hilioti Z, Bossis I. Autophagy: a target for retinoic acids. Autophagy. 2010;6(8):1224–1226. doi: 10.4161/auto.6.8.13793. [DOI] [PubMed] [Google Scholar]
- 27.Anguiano J, Garner TP, Mahalingam M, Das BC, Gavathiotis E, Cuervo AM. Chemical modulation of chaperone-mediated autophagy by retinoic acid derivatives. Nat Chem Biol. 2013;9(6):374–382. doi: 10.1038/nchembio.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang Y, Wang H, Wang S, Xu M, Liu M, Liao M, et al. GSK3beta signaling is involved in ultraviolet B-induced activation of autophagy in epidermal cells. Int J Oncol. 2012;41(5):1782–1788. doi: 10.3892/ijo.2012.1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eckert RL, Efimova T, Dashti SR, Balasubramanian S, Deucher A, Crish JF, et al. Keratinocyte survival, differentiation, and death: many roads lead to mitogen-activated protein kinase. J Investig Dermatol Symp Proc. 2002;7(1):36–40. doi: 10.1046/j.1523-1747.2002.19634.x. [DOI] [PubMed] [Google Scholar]
- 30.Roux PP, Blenis J. ERK and p38 MAPK-activated protein kinases: a family of protein kinases with diverse biological functions. Microbiol Mol Biol Rev. 2004;68(2):320–344. doi: 10.1128/MMBR.68.2.320-344.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zarubin T, Han J. Activation and signaling of the p38 MAP kinase pathway. Cell Res. 2005;15(1):11–18. doi: 10.1038/sj.cr.7290257. [DOI] [PubMed] [Google Scholar]
- 32.Kanemaru K, Nakamura Y, Totoki K, Fukuyama T, Shoji M, Kaneko H, et al. Phospholipase Cdelta1 regulates p38 MAPK activity and skin barrier integrity. Cell Death Differ. 2017;24(6):1079–1090. doi: 10.1038/cdd.2017.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang C, Xiao C, Dang E, Cao J, Zhu Z, Fu M, et al. CD100-Plexin-B2 promotes the inflammation in psoriasis by activating NF-kappaB and the inflammasome in keratinocytes. J Invest Dermatol. 2018;138(2):375–383. doi: 10.1016/j.jid.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 34.Conrad C, Gilliet M. Psoriasis: from pathogenesis to targeted therapies. Clin Rev Allergy Immunol. 2018;54(1):102–113. doi: 10.1007/s12016-018-8668-1. [DOI] [PubMed] [Google Scholar]
- 35.Lewis BJ, Rajpara S, Haggart AM, Wilson HM, Barker RN, Ormerod AD. Predominance of activated, clonally expanded T helper type 17 cells within the CD4+ T cell population in psoriatic lesions. Clin Exp Immunol. 2013;173(1):38–46. doi: 10.1111/cei.12086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao L, Xia J, Wang X, Xu F. Transcriptional regulation of CCL20 expression. Microbes Infect. 2014;16(10):864–870. doi: 10.1016/j.micinf.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Kazama M, Umezawa Y, Itoh M, Nobeyama Y, Ito T, Kikuchi S, et al. Successful treatment of ustekinumab in a psoriasis patient with human T-cell leukemia/lymphotropic virus type 1 infection. J Dermatol. 2017;44(11):1334–1335. doi: 10.1111/1346-8138.13678. [DOI] [PubMed] [Google Scholar]
- 38.Raimondo A, Lembo S, Di Caprio R, Donnarumma G, Monfrecola G, Balato N, et al. Psoriatic cutaneous inflammation promotes human monocyte differentiation into active osteoclasts, facilitating bone damage. Eur J Immunol. 2017;47(6):1062–1074. doi: 10.1002/eji.201646774. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study would be available from the corresponding author on reasonable request.