Abstract
The aim of the study was to analyze the 5-year survival after first-ever ischemic stroke and intracerebral hemorrhage. In this study 836 patients were analyzed with a first-ever stroke admitted at the Department of Neurology Tuzla, Bosnia and Herzegovina, from January 1st 1997 to December 31st 1998. Of these 613 (73,3%) were ischemic strokes and 223 intracerebral hemorrhages (26,7%) Subarachnoid hemorrhages were excluded. After hospitalization surviving patients examined periodically, and a final examination was performed 5 years after the stroke. Overall, case-fatility at the first month was 36% (301/836) and the mortality rate was significantly higher in the patients with intracerebral hemorrhage (58,3% vs. 27,9%, p<0,0001). The first year survived 60% patients with ischemic stroke, and 38% with intracerebral hemorrhage. After 5 years, 188 (31%) patients with ischemic stroke and 53 (24%) with intracerebral hemorrhage were alive (p=0,5), and the cumulative survival rate for the entire study was 29%. Among 30-day survivors (n=535) surviving rate after 5 years was significantly higher in patients with intracerebral hemorrhage (57% vs. 42,5%, p=0,01). The survival rate was the highest for those 50 years and younger (57%), and the lowest for those aged over 70 years (9%). Predictors of 5-year mortality were older age and hypertension for both types of stroke, heart diseases for ischemic stroke and diabetes for intracerebral hemorrhage. Long-term survival after first-ever ischemic stroke and intracerebral hemorrhage is similar. However, among 30-day survivors the 5-year survival is better in patients with intracerebral hemorrhage.
Keywords: ischemic stroke, intracerebral hemorrhage, long-term prognosis
INTRODUCTION
Among all the neurological diseases of adult life, the cerebrovascular ones clearly rank first in frequency and importance. Despite considerable improvement in primary prevention, diagnostic workup and therapy, stroke is on the second or third place on a mortality list, and all projections indicate that this will remain in the year 2020. Furthermore, stroke is a leading cause of disability (1, 2). Age- and sex-standardized annual incidence of stroke is between 300-500/100 000, and stroke incidence is 16 to 35% greater in men than women (3), but recent issues emphasize the importance of stroke in women (4). In classifying the cerebrovascular diseases (CVD) it is most practical, from the clinical viewpoint, to preserve the classic division into ischemic stroke (IS), accounting for 70 to 85% of all strokes, intracerebral hemorrhage (ICH) (10 to 20% of the cases), and subarachnoid hemorrhage (SAH) with frequency one-third to one-half that of ICH (5). At the Deparment of Neurology Tuzla during a five-year post-war period (1996-2000) 2664 stroke patients were treated: 65% with ischemic stroke, 28,5% with ICH, and 6,5% with SAH (6). Stroke mortality varies greatly form country to country, averaging 50-100/100 000 per year in developed countries and 200-250/100 000 in Eastern European populations (7). Prior research in stroke prognosis focuses mainly on in-hospital and short-term mortality, but recently a few studies of the long-term prognosis after stroke have been published (8, 9, 10, 11). Mortality rates of 7% to 46% after ischemic stroke have been reported in the first year after a stroke and a 5-year mortality of 45% to 72%. Accurate information about the long-term prognosis after stroke is important to the patient and family and helps the stroke team to set appropriate goals, balance the potential risks and benefits of treatment options, develop a treatment and discharge plan, and make rationing decisions if resources are limited. The aim of this study was to describe the 5-year survival after first-ever stroke and to determine the factors among all individuals and among 30-day survivors of first-ever stroke that predict an increased risk of death over the next 5 years.
PATIENTS AND METHODS
In this study it was analyzed patients with a first-ever stroke admitted at the Department of Neurology, University Clinical Centre Tuzla, Bosnia and Herzegovina, from January 1st 1997 to December 31st 1998. Subarach-noid hemorrhages were excluded. Medical history was obtained and presence of risk factors was evaluated on the day of admission. Computed tomography (CT) was performed for all patients during hospitalization. The procedure was obtained on spiral CT scanner (Siemens ELSCINT Twin, Siemens) with contiguous 1-cm transaxial slices. If the CT scan showed a cerebral hemorrhage or infarction the type of stroke was coded accordingly. In case of no abnormality on CT, the stroke was classified as cerebral infarction. All patients were followed up until death or up to 5 year after their stroke. We used the World Health Organization (WHO) definition of stroke as “rapidly developing symptoms and/or signs of focal, and at times global, loss of cerebral function, with symptoms lasting more than 24 hours or leading to death with no apparent cause other than that of vascular origin” (12). A history of hypertension was defined as systolic blood pressure >140 mmHg, or diastolic blood pressure >90 mmHg, or both diagnosed at least twice before the stroke or documented treatment of hypertension. History of heart disease (angina pectoris, myocardial infarction, atrial fibrillation, congestive heart failure) was accepted if it was diagnosed by a specialist of internal medicine or cardiologist. Diabetes mellitus was defined as use of a blood sugar lowering drug before the stroke onset or a documented fasting blood glucose concentration exceeding 7,0 mmol/l. Smoking was considered present when a patients smoked daily previous to the stroke and was considered absent when the patient had never smoked or stopped smoking for at least 1 year before the stroke onset. A history of transient ischemic attack (TIA) was defined when a patient had a temporary, focal neurological deficit presumably related to ischemia and lasting less than 24 hours, diagnosed by a neurologist. After hospitalization surviving patients examined periodically, and final examination was performed 5 years after stroke. Continuous and categorical data were analyzed using t-test and Chi-square (X2) test, and a value of p<0,05 was considered to be significant. To evaluate witch factors contribute to 5 year mortality, we compared the baseline characteristics for those patients who died within 5 years after stroke with those who not die within 5 years. We used X2 tests to assess differences in mortality for binary independent variables.
RESULTS
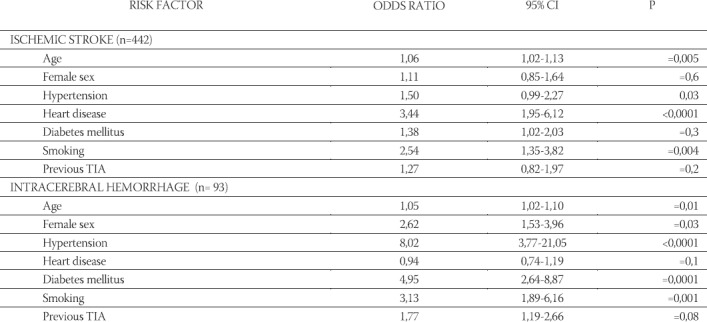
In the analysing period a total of 836 patients were hospitalized at the Department of Neurology Tuzla with a diagnosis of first-eveer stroke. Of these 613 (73,3%) were ischemic strokes and 223 intracerebral hemorrhages (26,7%). Overall, case-fatility at the first month was 36% (301/836) and the mortality rate was significantly higher in the patients with intracerebral hemorrhage (58,3% vs. 27,9%, 95% CI, Relative risk 2,09, p<0,0001) (Table 1). Furthemore, the highest mortality for both tipes of stroke was within the 5 days from the stroke onset. The annual mortality rate for the first year was 40% for ischemic stroke and 62% for intracerebral hemorrhage. The annual mortality rate in patients with intracerebral hemorrhage was a relatively constant 4% to 5% for years 2 through 5, while in patients with ischemic stroke was 14% for the second year and 5% to 7% for years 3 through 5 (Figure 1). After 5 years, 31% patients with ischemic stroke and 24% with intracerebral hemorrhage were alive (p=0,5), and the cumulative survival rate for the entire study was 29% after the fifth year after stroke onset. At the other hand, among 30-day survivors (n=535) 45% were alive at 5 years and surviving rate was significantly higher in patients with intracerebral hemorrhage (57% vs. 42,5%, 95% CI, Relative risk 1,62, p=0,01). In the five-year period survival rate decreased with age from 57% (73 out of 127) for those 50 years and younger up to only 9% (22 out of 241) for those aged over 70 years (Figure 2). The patients who died were significantly older than survived patients (68+9,6 vs. 63+9,3; p=0,005). Table 2 shows the prediction model for death at 5 years after first-ever stroke among 836 patients, of whom 595 died. The significant predictors of 5-year mortality for the patients with ischemic stroke were older age, hypertension, heart disease, diabetes mellitus and smoking, and for the patients with ICH were older age, hypertension and diabetes mellitus. The significant prognostic factors among 30-day survivors (n=535, of whom 294 died over 5 years) of first-ever stroke for death at 5 years were older age, hypertension, heart disease and smoking for the patients with ischemic stroke, and for the patients with ICH were older age, female sex, hypertension, diabetes mellitus and smoking (Table 3).
TABLE 1.
Stroke mortality whitin the first month

FIGURE 1.

Five-year survival according to stroke type
FIGURE 2.

Five-year survival according to age
TABLE 2.
Predictors of five-year mortality after first-ever stroke

TABLE 3.
Predictors of five-year mortality among survivors of >30-days after first-ever stroke
DISCUSSION
The principal findings of this hospital-based study are that the cumulative risk of death at 5 years after first-ever stroke is 71%; every third patient with ischemic stroke and fourth patient with intracerebral hemorrhage survive 5 years; older age, hypertension, heart diseases and diabetes mellitus affect mortality; and quality of life 5 years after stroke onset is better among survivors with intracerebral hemorrhage. Unfortunately, the overall case-fatility at the first month in our study (36%) is higher to those reported in other studies. In the study of Hankey et al (13) the case-fatility in the first 30 days after stroke was 23,5%, 26,5% in the Arcadia Stroke Registry Study (14), and 28% in the study of Bronnum-Hansen et al (15). The high rates of comorbidity, higher incidence of the intracerebral hemorrhage and negative social, economic, and diet factors in the post-war period in Bosnia and Herzegovina may contribute to our relatively poor prognosis in the acute phase of stroke. Additionally, this study started in 1997, just one year after the war, when the human and capacity resources at our Department were limited and, Stroke Unit” was not established. At the other hand, 20 years ago, stroke mortality at the first month in Tuzla area was 45% (16). After one year, 46% of patients with stroke in our study had died stressing the fact that the mortality after a stroke is high. In the previously mentioned study in our region, in the early 80’s, stroke mortality after one year was 58% (16). However, in the study from the central Italy, mortality at 1 year was 36,9% (32,4% for ischemic stroke and 58,2% for intracerebral hemorrhage)(17), and Vemmos et al (14) reported 37% mortality one year after stroke (31,5% for ischemic stroke and 53,2% for intracerebral hemorrhage). Furthermore, the risk of death in the first year after stroke in the Perth Community Stroke Study was 36,5% (13), and the Danish MONICA Study Group found 41% mortality in the first year after the stroke (15).
At the first sight the mortality rate within the first year after first-ever stroke is significantly higher in our study comparing with other reports. However, if we look the mortality rate within one year among 30-day survivors, the mortality in our study (10%) is similar to those seen in the last tree mentioned studies (10%, 13%, and 13% respectively). The cumulative risk of death at 5 years after the first-ever stroke in our study was 71%. The risk of death was greatest in the first year after stroke (46%), 11% of patients died in the second year, and the annual mortality rate for years 3 through 5 was 4% to 6%. Among 30-day survivors, about half survived 5 years, and prognosis was better for the patients with intracerebral hemorrhage. Hankey et al (13) reported the cumulative risk of death at 5 years after the first-ever stroke of 60%, and the annual risk of death of 10% between 1 and 5 years after stroke. Moreover, hemorrhagic stroke was associated with a substantially greater 30-day case fatility than ischemic stroke, but the subsequent case fatility was similar, if not lower, among survivors of hemorrhagic stroke. In the other study, among 277 patients who survived to 30 days after first-ever stroke, 152 (55%) were alive at 5 years (18). Bravata et al (19) followed 5123 patients with acute ischemic stroke, TIA, and carotid stenosis and found that patients with ischemic stroke had the highest 5-year mortality (60%). Recently, in the study of Hardie et al (20), the authors analyzed trends in survival over 5 years after first-ever stroke for 2 cohorts of patients in 1989-90 and 1995-96. The 5-year cumulative risk of death was 59% and 58% respectively. We found that increasing age, hypertension, diabetes mellitus were important predictors of 5-year mortality for both, isch-emic stroke and intracerebral hemorrhage, while heart diseases and smoking were predictors only for patients with ischemic stroke. Prior research has identified age, stroke severity, atrial fibrilation, heart diseases, TIA, co-morbidity and disability at discharge as important predictors of late mortality after stroke (14, 18, 19, 21, 22).
CONCLUSION
We found that stroke is associated with a very high risk for death in the acute and subacute phases. One third of patients with first-ever stroke died within the 30 days, and one third died in the next five years. Better primary and secondary prevention, treating a stroke as a medical emergency, and management of acute stroke in, Stroke Unit” may improve the early and long-term survival rate and functional outcome.
REFERENCES
- 1.Warlow C. Epidemiology of stroke. Lancet. 1998;352(suppl III):1–4. doi: 10.1016/s0140-6736(98)90086-1. [DOI] [PubMed] [Google Scholar]
- 2.Murray CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 3.Sudlow CLM, Warlow CP. Comparable studies of the incidence of stroke and its pathological types. Stroke. 1997;28:491–499. doi: 10.1161/01.str.28.3.491. [DOI] [PubMed] [Google Scholar]
- 4.Bousser MG. Stroke in women. Circulation. 1999;99:463–467. doi: 10.1161/01.cir.99.4.463. [DOI] [PubMed] [Google Scholar]
- 5.Sacco RL. Pathogenesis, classification, and epidemiology of cere-brovascular disease. In: Rowland L.P, editor. Merrit’s textbook of neurology. 9th ed. Media: Wíffiams&Wükíns; 1995. [Google Scholar]
- 6.Smajlović Dž, Ibrahimagić O, Dostović Z, Tupković E, Sinanović O. Main epidemiological characteristics of cerebrovas-cular diseases at the Deparment of Neurology Tuzla during a five-year post-war period (1996-2000) Acta Clin Croat. 2002;41(suppl 3):57. [Google Scholar]
- 7.Argentino C, Prencipe M. The burden of stroke: a need for prevention. In: Fieschi C, Fisher M, editors. Prevention of ischemic stroke. London: Martin Dunitz; 2000. pp. 1–5. [Google Scholar]
- 8.Scmidt EV, Smirnov VE, Ryabova VS. Results of the seven-year prospective study of stroke patients. Stroke. 1988;19:942–949. doi: 10.1161/01.str.19.8.942. [DOI] [PubMed] [Google Scholar]
- 9.Dennis MS, Burn JPS, Sandercock PAG, Bamford JM, Wade DT, Warlow CP. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke. 1993;24:796–800. doi: 10.1161/01.str.24.6.796. [DOI] [PubMed] [Google Scholar]
- 10.Petty G, Brown R, Whisnant J, Sicks J, O’Fallon W, Wiebers D. Survival and recurrence after first cerebral infarction: a population-based study in Rochester, Minnesota 1975 thourgh 1989. Neurology. 1998;50:208–216. doi: 10.1212/wnl.50.1.208. [DOI] [PubMed] [Google Scholar]
- 11.Smajlović Dž, Kojić B, Sinanović O, Burina A, Hodžić R. Long-term prognosis and quality of life after first-ever stroke. Cerebro-vasc. Dis. 2005;19(suppl 2):83. [Google Scholar]
- 12.Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ. 1980;58:113–130. [PMC free article] [PubMed] [Google Scholar]
- 13.Hankey GJ, Jamrozik K, Broadhurst RJ, Forbes S, Burvill PW, Anderson CS, Stewart-Wynne EG. Five-year survival after first-ever stroke and related prognostic factors in the Perth Community stroke study. Stroke. 2000;31:2080–2084. doi: 10.1161/01.str.31.9.2080. [DOI] [PubMed] [Google Scholar]
- 14.Vemmos KN, Bots ML, Tsibouris PK, Zis VP, Takis CE, Grobbee DE, Stamatelopoulos S. Prognosis of stroke in the south of Greece: 1 year mortality, functional outcome and its determinants: the Arcadia Stroke Registry. J. Neurol. Neurosurg. Psychiatry. 2000;69:595–600. doi: 10.1136/jnnp.69.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bronnum-Hansen H, Davidsen M, Thorvaldsen P. Long-term survival and causes of death after stroke. Stroke. 2001;32:2131–2136. doi: 10.1161/hs0901.094253. [DOI] [PubMed] [Google Scholar]
- 16.Sinanović O. Master thesis. Medical School, University of Tuzla; 1983. Prognosis of the medicamentouse and physical treatment in patients with acute stroke. [Google Scholar]
- 17.Carolei A, Marini C, Di Napoli M, et al. High stroke incidence in the prospective comunity-based L’Aquily Registry (1994-98): first year results. Stroke. 1997;28:2500–2506. doi: 10.1161/01.str.28.12.2500. [DOI] [PubMed] [Google Scholar]
- 18.Hankey GJ, Jamrozik K, Broadhurst RJ, Forbes S, Anderson CS. Long-term disability after first-ever stroke and related prognostic factors in the Perth Community Stroke Study 1989-1990. Stroke. 2002;33(4):1034–1040. doi: 10.1161/01.str.0000012515.66889.24. [DOI] [PubMed] [Google Scholar]
- 19.Bravata DM, Ho SY, Brass LM, Concato J, Scito J, Meehan TP. Long-term mortality in cerebrovascular disease. Stroke. 2003;34:699–705. doi: 10.1161/01.STR.0000057578.26828.78. [DOI] [PubMed] [Google Scholar]
- 20.Hardie K, Jamrozik K, Hankey GJ, Broadhurst RJ, Anderson C. Trends in five-years survival and risk of recurrent stroke after first-ever stroke in the Perth Community Stroke Study. Cerebro-vasc Dis. 2005;19(3):179–185. doi: 10.1159/000083253. [DOI] [PubMed] [Google Scholar]
- 21.Appelros P, Nydevik I, Viitanen M. Poor outcome after first-ever stroke: predictors for death, dependency, and recurrent stroke within the first year. Stroke. 2003;34(1):122–126. doi: 10.1161/01.str.0000047852.05842.3c. [DOI] [PubMed] [Google Scholar]
- 22.Yokota C, Minematsu K, Hasegawa Y, Yamaguchi T. Long-term prognosis, by stroke subtypes, after a first-ever stroke: a hospitalbased study over a 20-year period. Cerebrovasc Dis. 2004;18(2):111–116. doi: 10.1159/000079258. [DOI] [PubMed] [Google Scholar]


