Abstract
Acute respiratory failure requiring assisted ventilation is one of the most common reasons for admission to the neonatal intensive care unit. Respiratory failure is the inability to maintain either normal delivery of oxygen to the tissues or normal removal of carbon dioxide from the tissues. It occurs when there is an imbalance between the respiratory workload and ventilatory strength and endurance. Definitions are somewhat arbitrary but suggested laboratory criteria for respiratory failure include two or more of the following: PaCO2 > 60 mmHg, PaO2 < 50 mmHg or O2 saturation <80 % with an FiO2 of 1.0 and pH < 7.25 (Wen et al. 2004).
Respiratory Failure of Non-pulmonary Origin
Apnoea of Prematurity
Educational Aims
To describe the key features of the central control of breathing, the coordinated output to the motor effectors, the resultant mechanical events resulting in ventilation and the nature of the nervous and chemical feedbacks to the controller
To describe the importance of behavioural state in fetal ‘breathing’
To describe apnoea in terms of breathing homoeostasis and its limits
To describe apnoea of prematurity, its different categories and its association with oxygen desaturation and bradycardia and thus potentially with life-threatening tissue hypoxia
To describe the pathophysiology of apnoea of prematurity in terms of the central circuitry and its outputs, the responses to blood gases, the associated reflex bradycardia, the motor responses to afferent inputs and the upper airway protective and exaggerated responses
To describe the clinical presentation and differential diagnosis of apnoea of prematurity
To describe the avoidance of clinical factors that can aggravate apnoea of prematurity and its non-pharmacologic and pharmacologic therapies
To describe the specifics of caffeine therapy including recommended dosages, efficacy, cessation of therapy and benefits on long-term outcome
To describe the natural history of apnoea of prematurity, the preparation for safe discharge home, the indications for home monitoring and the lack of a firm association with SIDS
To describe the concerns about long-term morbidity with recurrent preterm apnoea and the advisability of follow-up care
Introduction
When you can’t breathe, nothing else matters. – American Lung Association Motto.
Breathing, Central Control and Fetal Development
Breathing consists of motor acts that enable tidal ventilation for gas exchange. Immediately at birth the newborn employs intricate breathing patterns that establish and maintain airway volume and attain ventilation. Thereafter, throughout life the normal breathing pattern, eupnoea, can be gentle tidal breathing that is involuntary and hardly sensed, but many other breathing patterns are employed in normal conditions. Thus, an expanded view of normal breathing is that it consists of centrally controlled coordinated muscular activities which aim to ensure that the airway is protected and has optimal supra- and sub-glottic volumes to maintain homoeostasis and provide a stable platform to enable ventilation with ensuing efficient gas exchange and transport (Hutchison 2007). Normal breathing involves central coordination with other motor acts, e.g. swallowing, speech and walking.
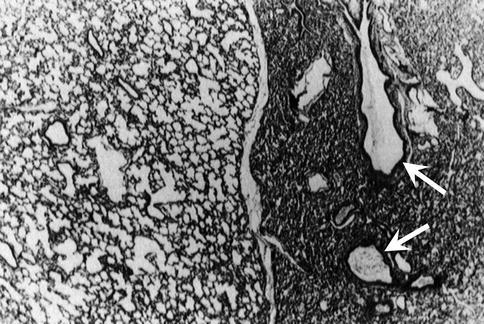
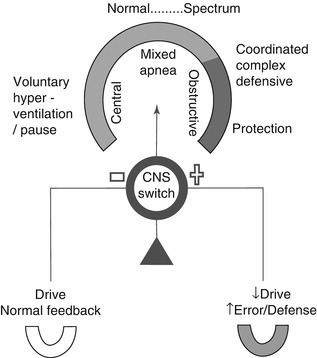
Breathing control is primarily determined by the intrinsic nature of the central nervous system (CNS) controller and is modified by integration of all inputs (Fig. 47.5). Two features of central control deserve emphasis. There is a redundancy to the circuitry, with alternative drives and pathways, and there is a motor control hierarchy: rapid airway protection takes precedence over control of absolute airway volume, which in turn takes precedence over relative tidal volume changes. Control of breathing is exercised by the coordinated activities of the nasal, pharyngeal, laryngeal and pump muscles which, in concert with lower airway smooth muscle tone that adjusts airway wall stiffness, alter the transairway pressure gradients. The result is that tidal ventilation occurs simultaneously with the control of total airway volume, which adjusts airway pressure critical for patency, central feedback and likely drive threshold (Adrian 1933). Airway and chest wall neural feedback is rapid (milliseconds) and crucial for homoeostasis, enabling the controller to adjust flow within a breath and match motor outputs with the structural characteristics of the different parts of the respiratory system and their associated mechanics. Feedback from blood gaseous and chemical sensors occurs within seconds.
…thoracic gymnastics in preparation for the great extrauterine function of atmospheric respiration. – John W. Ballantyne, 1902.
Fig. 47.5.
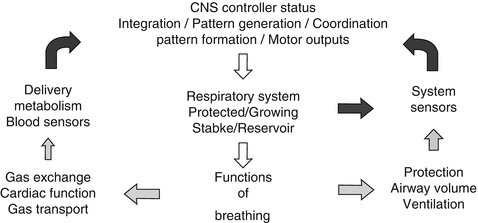
Breathing control. This diagram of the central control of breathing shows its functions both in enabling ventilation with gas exchange and the simultaneous maintenance of airway patency and respiratory system homoeostasis. The central generation and formation of motor breathing patterns involve integration of all sensory inputs in a hierarchical manner
Fetal ‘breathing’ develops when gas exchange is placental and blood oxygen tension is low. Central state is a dominant factor. In fetal sheep, in the high-voltage state, phasic diaphragmatic activity is absent and laryngeal narrowing occurs (Harding 1994). In the low-voltage state, the laryngeal and diaphragmatic activities pattern is similar to that seen postnatally. Both state-related fetal ‘breathing’ patterns are important for lung growth (Harding 1994). Fetal hypercapnia augments ‘breathing’ muscle activities mainly in the low-voltage state (Harding 1994). In contrast, hypoxia, acting at a pontine site, inhibits fetal diaphragmatic activity in the low-voltage state (Harding 1994).
Apnoea, Breathing and Apnoea: A Spectrum of Homoeostasis and Limits
Apnoea is a lack of tidal airflow. Transient lacks of airflow are seen in patterns with glottic closure, e.g. during swallowing, defecating, lifting, coughing, yawning, crying or vocalising. Apnoea occurs with a minimal fall in the carbon dioxide tension (PCO2) to below the apnoeic threshold (Khan et al. 2005). Brief apnoeas are typified by the brain’s subsequent ability to return quickly to muscle activities that ventilate the airway. Clinical apnoea is a persistent lack of airflow without a spontaneous return to breathing.
Breathing patterns and apnoea can be viewed as a spectrum/continuum (Fig. 47.6). Throughout life, rapid changes in pattern are dependent upon the status of the central circuitry, its response hierarchy and its different inputs. Central setting of optimal homoeostatic limits must vary constantly with inputs sensing changes in growth and in the individual’s internal and external environments. It is speculated that during sleep, ‘virtual’ central conditions allow the limits to be reset/tuned (Hutchison 2007).
Fig. 47.6.
Spectrum of breathing and apnoea. This diagram shows the spectrum of breathing patterns used in daily life including coordination with complex acts such as swallowing and coughing. A centrally controlled pattern switch can rapidly alter the breathing patterns from ones typified in expiration by a more open glottis to ones characterised by a more closed glottis. This occurs transiently in airway volume maintenance, airway protection and speech and is determined by central drive/status and afferent inputs. Expiratory laryngeal closure increases as central drive decreases. It is postulated that in mixed apnoea a switch from central apnoea to obstructive apnoea accompanies a progressive decrease in central drive and that this may be enhanced by a decrease in airway volume during central apnoea with an open glottis
Apnoea of Prematurity
. . . They seem to do the most unreasonable things with their respiration . . . – Kenneth Cross, 1954
Definition and Types of Apnoea
Apnoea of prematurity is associated with physiological characteristics and pathological conditions found in the preterm infant born at <37 completed postmenstrual weeks. Its incidence is inversely related to gestational age (Henderson-Smart 1981). Brief cessations of airflow lasting a few seconds are common in sleep and may represent a transient return to fetal life. Apnoea demanding attention and meriting the clinical diagnosis of apnoea of prematurity is that lasting 15–20 s or that accompanied by bradycardia, cyanosis or pallor. Apnoea is categorised into different types. Central apnoea (incidence ~10–25 %) is a lack of tidal airflow accompanied by a lack of pump muscle activity (with or without an open glottis). Obstructive apnoea (~10–20 %) is an absence of tidal airflow accompanied by upper airway obstruction, which can commence in expiration and continue despite pump muscle activity and in the subsequent neural expiration. Mixed apnoea (~50–75 %) is both central and obstructive apnoeas occurring serially, usually in that order. Bradycardia (heart rate <100/min) usually follows the onset of apnoea of prematurity. Oxygen saturation values fall (<85 %) and can produce cyanosis. An associated pallor can indicate the occurrence of a dive reflex response with preferential blood flow to the heart, brain and adrenals but diminished blood flow to other important organs, e.g. the gut. The newborn brain is more tolerant than the adult to hypoxia, but if apnoea is ongoing, death results.
Pathophysiology
Central Circuitry and Output Determinants
Rostral and caudal CNS structures influence the control of breathing patterns (Feldman and Del Negro 2006; Rybak et al. 2008). Lesioning studies in animals have identified that, at a minimum, eupnoea requires a pontomedullary neuronal network (Rybak et al. 2008). When both upper pontine respiratory neuronal groups (PRG) and vagal afferents are removed, the lower pontine-medullary output is apneusis, a pattern typified by prolonged inspiratory drive. The generation of signals for coordination of laryngeal and diaphragmatic activities appears to be dependent upon an intact lower pons (Hutchison and Speck 2003). Inspiratory and pre-inspiratory neurons involved in rhythm generation have been identified in the ventral medullary pre-Bötzinger and parafacial regions, respectively. Neurons in the Bötzinger complex exert mainly expiratory control (Feldman and Del Negro 2006). Specific types of premotor medullary neurons have been classified by their signal shapes and timings. Their actions result in a central breathing cycle consisting of three phases: inspiration, post-inspiration and expiration (Feldman and Del Negro 2006). Mechanical changes following these outputs are seen well in grunting (see Sect. 10.1007/978-3-642-01219-8_4). Protective, mechanical and speech-related changes occur quickly within a breath; thus, phase-switching and pattern-switching neurons are important (Rybak et al. 2008) (Fig. 47.6).
Apnoea of prematurity is associated with incomplete brain development, including decreased cell synapses, dendrites, myelinisation and brainstem conduction (Darnall et al. 2006). Gene abnormalities are reported in the central hypoventilation syndrome (Abu-Shaweesh and Martin 2008). Neurotransmitters (γ-aminobutyric acid (GABA), adenosine, prostaglandin E, serotonin, endorphins, catecholamines, glutamate) affect respiratory-related neuronal function (Darnall et al. 2006). The neurochemistry in preterm infants favours neuronal inhibition over excitation. In animals, prostaglandin E production can be triggered by the cytokine IL-1β, while adenosine stimulates GABA production (Abu-Shaweesh and Martin 2008). Metabolism is increased by hyperthermia and decreased by hypothermia. Both hypothermia and hyperthermia can decrease breathing, suggesting that hypothermia decreases excitation more than inhibition and that hyperthermia augments the dominant intrinsic inhibitory pathways and their inputs. Thus, the importance of temperature homoeostasis is emphasised.
Central apnoea may result from altered PRG input (Hutchison and Speck 2003). When the PRG is removed from decerebrate cats, the response to an expiratory airway load is a pattern similar to central apnoea with an open glottis. In this circumstance, expiratory flow will occur passively until the relaxation volume (Vr) is reached (see Chap. 10.1007/978-3-642-01219-8_4, Fig. 10.1007/978-3-642-01219-8_4_Fig6). Preterm infants actively maintain sub-glottic volume above their low Vr when awake, but during central sleep apnoeas the sub-glottic volume can decrease. This is especially seen in REM sleep when all types of apnoeas are more common and longer and can be associated with profound bradycardia. Central apnoea with glottic closure can also occur, e.g. in some human newborns who are depressed at birth, in preterm lambs (Praud and Reix 2005) and in gasping animals with exposure to acute cerebral hypoxia/ischaemia (Hutchison et al. 2002). Gasping is typified by short diaphragmatic bursts and long expirations with glottic closure. Initially, this incremental breathing pattern (see Sect. 10.1007/978-3-642-01219-8_4) maintains sub-glottic volume, which is probably critical in autoresuscitation (Hutchison et al. 2002). In lambs, when central depression results in prolonged expiratory apnoea, glottic adductor activity persists until all muscle activity ceases (Praud and Reix 2005). During mixed apnoea, obstructive upper airway closure commences before diaphragmatic activity and its associated fall in airway pressure (Idiong et al. 1998) and thus appears to be due to centrally altered laryngeal or pharyngeal muscle activities (Idiong et al. 1998; Upton et al. 1992). Obstructive apnoea is due to insufficient pharyngeal opening pressure, which reflects an imbalance between factors that decrease pharyngeal patency (see Sect. 10.1007/978-3-642-01219-8_4) and the central motor output that dictates a compensatory increase in muscle tone. In the preterm infant, pharyngeal collapse can occur passively with neck flexion or actively in sleep, when pharyngeal wall muscle tone can be low (Thach and Stark 1979). Expiratory laryngeal closure, triggered by a low lung volume, could play a role by reducing intrapharyngeal pressure below its critical value for patency.
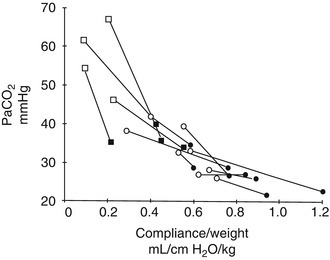
Central Responses to Blood Gases and Apnoea of Prematurity
Throughout life, hypocarbia decreases the central drive to breathe (Khan et al. 2005), and during the associated hypopnoea/apnoea, laryngeal adductor activity (glottic closure) is found (Jounieaux et al. 1995; Kuna et al. 1993). The apnoeic threshold is higher in preterm infants with apnoea (Gerhardt and Bancalari 1984), making apnoea more likely with a fall in PCO2, e.g. with normal activity, sighing. Hypercapnia increases ventilation, but the response is depressed by accompanying hypoxia (Rigatto 1986) and can be accompanied by expiratory laryngeal closure (Eichenwald et al. 1993). At high PCO2 levels apnoea can occur (Alvaro et al. 1992). Marked hypercapnia may act via central inhibition of respiratory muscle output and/or by inducing chest wall distortion that can trigger apnoea with laryngeal closure. The preterm infant’s response to hypoxaemia may or may not start with a transient increase in ventilation, which, if present, is dependent upon carotid body integrity. A decrease in central output to the diaphragm follows; this decrease is attenuated in non-rapid eye movement sleep (Rigatto 1986). Hypoxia can result in periodic breathing and then apnoea (Rigatto 1986). The responsiveness of the carotid body is depressed after birth but recovers within 2 weeks (Abu-Shaweesh and Martin 2008). Repeated exposure to hypoxaemia postnatally may augment the carotid body sensitivity to hypoxaemia with a resultant hyperventilation, followed by hypocarbia and decreased ventilation (Al-Matary et al. 2004; Nock et al. 2004). These cycles may produce periodic breathing and apnoea. However, prenatal exposure to cigarette smoke may diminish the response to hypoxaemia (Gauda et al. 2004; Schneider et al. 2008), and exposure to hyperoxia at critical periods of development can inhibit carotid body development in animals (Gauda et al. 2004). Diminished stimulatory responses to hypoxaemia have been found in preterm infants (Gauda et al. 2004). Thus, central integration of both increased and decreased carotid body inputs may promote apnoea (Gauda et al. 2004).
Sinus Arrhythmia and Reflex Bradycardia
Vagal cardiac efferent output decreases in inspiration when airway vagal afferent input increases. Therefore, heart rate increases during inspiration, while it slows during expiration – sinus arrhythmia. The heart rate changes help maintain a constancy of cardiac output and blood pressure. Augmented ventilation in respiratory distress can produce cardiac output volume swings detected as pulsus paradoxus (Goldstein and Brazy 1990). During apnoea, vagal afferent input falls and vagal cardiac efferent output increases; thus, the onset of bradycardia can be immediate. Bradycardia in older preterm infants with apnoea follows the onset of a decrease in oxygen saturation, reflecting the importance of central integration of vagal afferent and chemoreceptor inputs (Poets 2003) (see Sects. 10.1007/978-3-642-01219-8_4 and 47.3.1.2.2.5). Vagal efferent activity occurs in swallowing, urinating and defecating and can be accompanied by bradycardia.
Motor Responses to Chest Wall and Airway Inputs
Active maintenance of sub-glottic volume is noted in the newborn, whose elastic chest wall is ideal for growth and atraumatic birth. Chest wall distortion, inward movement that threatens airway volume, occurs easily and stimulates chest wall afferents that inhibit phrenic activity (intercostal-phrenic reflex) and/or produce glottic closure. Newborn infant motor responses to vagal afferents are easily elicited (Thach 2001). Lower airway slowly adapting receptors (SARs) detect within-breath volume/stretch, while rapidly adapting irritant receptors (RARs) detect distortion/deflation. C-fibre receptors, associated with the pulmonary vasculature, detect chemical changes. In animals, the SAR inputs stimulate the chest wall and diaphragmatic pump muscles during inspiration until peak afferent activity is reached when inspiration is inhibited. Increased vagal afferent feedback accompanies a large inflation and triggers expiratory apnoea – the Hering-Breuer inflation reflex, a response modulated by airway CO2 in animals. After a large inflation, abdominal expiratory muscle activity is triggered – the Hering-Breuer expiration reflex. Prevention of inspiration by airway occlusion causes a fall in upper and lower airway vagal input, prolonging inspiration. During partial vagal blockade, inflation produces a second inspiratory effort – Head’s paradoxical reflex. Prevention of expiration by airway occlusion maintains vagal afferent input, thus prolonging expiratory time. In adult animals, when airway volume is considerably reduced, irritant receptor stimulation triggers an inspiration – the Hering-Breuer deflation reflex. However, irritant receptor input in preterm infants, with deflation or with tracheal stimulation, can result in apnoea (Fleming et al. 1978; Hannam et al. 1998). A cough response is only noted after 34 weeks postmenstrual age (Fleming et al. 1978).
The Hering-Breuer and Head reflexes may act to optimise lung inflation without tissue damage during inspiration and tailor expiratory time for a given expired volume. The stretch receptors may also act to increase central neuronal activity during expiration such that inspiration begins at a higher level of expiratory vagal input and thus peaks sooner, signalling an earlier cessation of tidal inspiration and promoting respiratory rate (Al-Matary et al. 2004). There is support for Head’s viewpoint. Infants use laryngeal and diaphragmatic means of maintaining higher absolute airway volumes and breathe faster (Sect. 10.1007/978-3-642-01219-8_4) (Thach 2001). In the preterm neonate, atelectasis/deflation post-extubation is associated with apnoea (Hannam et al. 1998). A lower end-expiratory volume (EEV) is noted in REM sleep and in apnoeic infants (Poets 2003). Furthermore, in lambs breathing through a tracheostomy, absence of laryngeal control of EEV is associated with apnoea (Johnson 1979). Airway pressure support after birth is the mainstay for reversal of apnoea and bradycardia, the latter being used in initial stabilisation as a sign to indicate the need for airway volume support. After birth, the intensivist employs the ‘open lung (airway) approach’ during artificial ventilation. Failure to maintain sub-glottic airway volume when the preterm infant is on a ventilator results in desaturation/bradycardia (Bolivar et al. 1995). This stresses that, when handling the endotracheal tube and/or moving the preterm infant’s thorax, the maintenance of sub-glottic airway volume is important.
Upper Airway Protective and Exaggerated Interactive Central Responses
Stimulation of protective receptors, e.g. laryngeal chemoreceptors with superior laryngeal nerve (SLN) afferents, can rapidly interrupt ventilation and close the larynx (Davies et al. 1988). In immature humans and animals, the SLN inputs can instigate apnoea and bradycardia, although a re-distribution of blood flow to the heart, brain and adrenals also occurs – the dive reflex response (Abu-Shaweesh and Martin 2008; Daly 1997). This response to SLN input decreases with advancing age but can be rekindled by a concurrent central depression or an upper airway infection (Daly 1997). The coexistence of central inhibition (e.g. with sedation or hypo-/hyperthermia), followed by SLN stimulation (e.g. at intubation) and then hypoxia, can produce an exaggerated and potentially lethal response, even in the adult (Daly 1997) (Sect. 10.1007/978-3-642-01219-8_4). This stresses the roles of central status and the motor response hierarchy in determining pattern (Fig. 47.7).
Fig. 47.7.

Afferent interactions and the motor response hierarchy. This diagram illustrates how factors influencing motor pattern may interact. Sudden decreases in any excitatory input can alter the balance affecting the outputs to the heart, airway smooth muscle and laryngeal and diaphragmatic muscles producing a more protective pattern (right side of diagram). The motor response determining expiratory glottic closure is seen as being determined primarily by the central drive/status, amplified secondly by decreased or error signals in neural afferent inputs and amplified thirdly by input from carotid body stimulation. Thus, increased carotid body stimulation can amplify an existing pattern. By contrast, a sudden decrease in carotid body input can trigger a switch to a protective pattern. This provides a possible explanation for the proposed roles of both increased and decreased carotid body inputs in the genesis of apnoea with glottic closure. CNS central nervous system, CSN carotid sinus nerve, HR heart rate, Airway SM airway smooth muscle, PCA E expiratory posterior cricoarytenoid, TA E expiratory thyroarytenoid
Clinical Aspects
Presentation and Differential Diagnosis
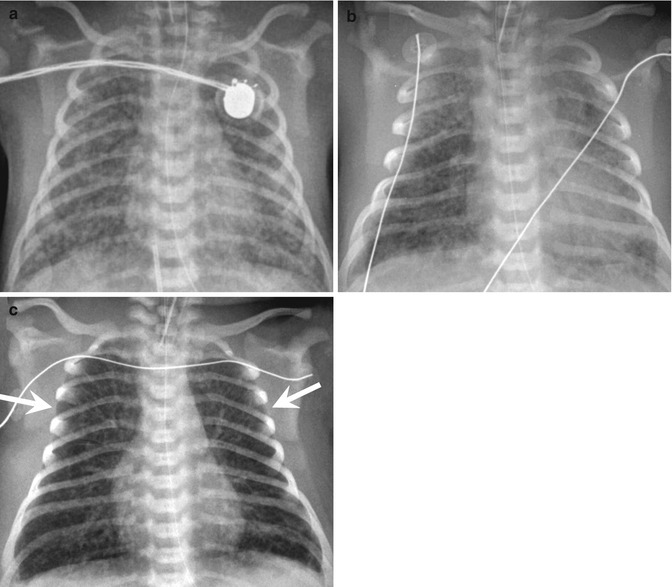
Apnoea can present on the first day of life and is virtually universal in preterm infants born at <28 weeks gestational age (Fig. 47.8) (Henderson-Smart 1981). The severity of apnoea is defined by its duration, the degrees of associated oxygen desaturation and bradycardia, and the type of therapeutic intervention provided, from minimal stimulation to total respiratory support. The assessment of the apnoeic patient consists of the nose-to-diaphragm then the head-to-toe approach. Apnoea of prematurity is differentiated from periodic breathing, a repetitive series of pauses in breathing separated by a crescendo-decrescendo pattern of breaths. Periodic breathing in normal preterm infants is considered benign, but it can be associated with hypocarbia, hypoxia and CNS hypoxia/ischaemia and with a fall in sub-glottic airway volume (Khan et al. 2005; Rigatto 1986). Conditions resulting in apnoea, including structural lesions (Brazy et al. 1987), are considered before a diagnosis of idiopathic apnoea is made (Fig. 47.9). Upper airway contact with food or with gastric contents can result in apnoea, but episodes of gastroesophageal reflux do not appear to be temporally linked to apnoea. In animals, prior upper airway exposure to acid can alter the response to subsequent mechanical loads (Sant’Ambrogio et al. 1998). Thus, the clinical impression that the two are related may be indirect. Pre-existing anaemia exacerbates the apnoeic response to SLN stimulation in animals and is important in postoperative apnoea (Cote et al. 1995). However, blood transfusion therapy for apnoea of prematurity is debated.
Fig. 47.8.
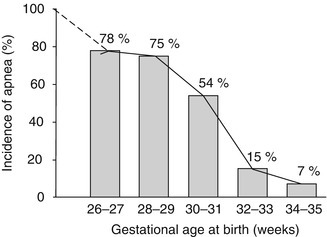
Incidence of apnoea of prematurity. The incidence of apnoea of prematurity increases inversely with the gestational age at birth, being virtually universal in the preterm infant <28 weeks (Modified and reproduced with permission from Henderson-Smart (1981))
Fig. 47.9.
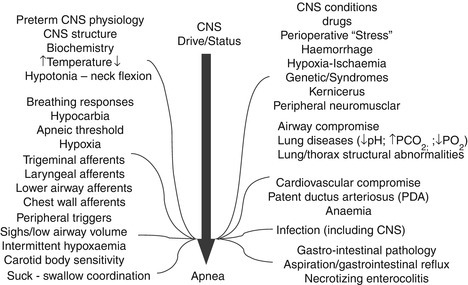
Aetiology of apnoea of prematurity. Multiple physiological and pathological conditions affect central nervous system (CNS) control and are associated with an increased propensity to apnoea of prematurity
Therapy
Specific therapy is given for the conditions listed in Fig. 47.9, e.g. a patent ductus arteriosus (PDA) resulting in hypoxaemia and pulmonary oedema that can trigger lower airway receptors resulting in apnoea. Conditions that can enhance apnoea are avoided. Hyperoxia can diminish recovery from SLN stimulation in lambs and, with altered carotid chemosensitivity, will increase apnoea (Al-Matary et al. 2004). Careful attention is paid to nasal patency (secretions, proper prong size and attachment of nasal continuous airway positive pressure [NCPAP] device), environmental temperature, correct neck posture (neck flexion) and abdominal distention (air in the stomach, correct positioning of gastric tube, a tight diaper forcing abdominal contents into the chest). Apnoea and bradycardia or bradycardia alone during feeding is usually a benign condition that responds to cessation of the suck/swallow stimulus.
The importance of central ‘drive’ and airway stability/patency as causative factors in apnoea of prematurity is reflected in the main forms of therapy, namely, peripheral tactile stimulation, xanthine therapy and respiratory airway support (Table 47.2). Xanthine therapy primarily enhances central drive and treats central apnoea (Table 47.3), while NCPAP therapy maintains airway stability and thus prevents mixed apnoea (Miller and Martin 2004). However, caffeine therapy enhances breathing peripherally by improving diaphragmatic function, while NCPAP therapy enhances central drive by increasing airway vagal feedback and decreasing oxygen saturation variability that may stabilise carotid body feedback.
Table 47.2.
Therapies for apnoea of prematurity
| Effective therapies for idiopathic apnoea | Comments |
|---|---|
| Physiological stimulation | |
| Tactile stimulation | Used for minor apnoea |
| Air cushion | Infrequently used |
| Inhaled low-concentration CO2 | Experimental (Abu-Shaweesh and Martin 2008) |
| Pharmacologic stimulation | |
|
Xanthines Caffeine used in recommendeddosing |
Safe; serum concentration monitoring not needed; ↓ bronchopulmonary dysplasia and ↑ neurodevelopment ↓ Postoperative apnoea in former preterms up to ~60 postmenstrual weeks |
| Theophylline | Bronchodilator properties may be useful |
| Doxapram | In high dose ↑ seizures; rarely used |
| Respiratory support | |
| Nasal cannulae: high flow | Alternative to NCPAP but applied pressure not monitored; used in weaning from NCPAP |
| Nasal CPAP |
Mainstay of therapy; modern device available with low work of breathing Mixed apnoea > central apnoea |
| Non-invasive positive pressure ventilation | May be useful; more trials awaited |
| Invasive artificial ventilation | Final resort: has risks of ‘endotrauma’ |
Table 47.3.
Caffeine effects and side effects
| Effects | Side effects |
|---|---|
| Competitive antagonism of adenosine receptors (A1 and A2a) |
↑ Irritability (restlessness) ↑ Jitteriness |
| Inhibition of phosphodiesterase (minor) | ↑ Seizure tendency |
| Mobilisation of cellular calcium (at high dose) | ↑ Diuresis/dehydration |
|
↑ Central ‘drive’: ↑ minute ventilation ↓ Threshold to hypercapnia |
↑ Gastric aspirates ↑ GI intolerance (− gastric acid) |
| ↑ Pulmonary blood flow; ↓ BPD | ↑ Tachycardia,arrhythmias |
| ↑ Skeletal muscle and myocardium activity | ↑ Hyper-/hypoglycaemia |
| ↑ Metabolism (− O2 consumption) | ↑ Failure to gain weight |
| ↑ Neurodevelopment (recommended doses) | ↑ Sleeplessness |
Despite appearing as a ‘simple’ therapy, NCPAP requires care in its application and excellent bedside monitoring and nursing (Hutchison and Bignall 2008). Laboratory and clinical studies strongly support the use of a modern NCPAP device (Hutchison and Bignall 2008; Pantalitschka et al. 2009). Weaning from NCPAP is little studied. In general, when an infant is receiving <30 % supplementary oxygen, a switch to high-flow nasal cannulae can be made. The advantage of nasal cannulae lies in their ease of use. The disadvantages are that the airway pressure they generate is not monitored and there may be increased infectious risks. Severe apnoea can warrant invasive mechanical ventilation but involves the complications of ‘endotrauma’ (Hutchison and Bignall 2008). There is interest in non-invasive positive pressure ventilation (NIPPV) for apnoea, and larger trials are awaited (Hutchison and Bignall 2008; Pantalitschka et al. 2009). Since coordination between the upper airway and pump muscles is critical, NIPPV is applied synchronously with the central outputs to the breathing muscles (Jounieaux et al. 1995); this may be difficult during sleep.
Caffeine therapy with a loading dose of 20 mg/kg followed by 5–6 mg/kg/day produces therapeutic serum concentrations (8–20 mcg/L) independent of the patients’ gestational age between 24 and 35 weeks and of their renal and liver functions over wide ranges (Leon et al. 2007). Thus, monitoring of serum caffeine concentrations is unnecessary if the recommended dosing is used. Tachycardia with caffeine can result from a pharmacodynamic effect. It resolves with cessation of therapy despite a normal serum concentration. Slightly higher and significantly higher caffeine dosing regimens have been used. The latter regimen increased successful weaning from a ventilator (Steer et al. 2003). Concerns about the extensive use of caffeine relate to its action as an antagonism of adenosine, a body-wide mediator of vasodilatation, which is involved in neurodevelopment. However, a controlled trial of early postnatal administration (<10 days) of caffeine versus placebo found that those receiving caffeine in recommended doses had less bronchopulmonary dysplasia (by 10 %) and improved cognitive outcome (by 5 %) (Schmidt et al. 2007; Schmidt et al. 2006b). Adenosine blockade may still be problematic. Caffeine therapy has been linked to necrotising enterocolitis, albeit weakly. Preterm infants are susceptible to white matter injury and thus at increased risk when cerebral blood flow is low (Darnall et al. 2006). If an infant on caffeine therapy develops hypocarbia during ventilatory support, any hypocarbia-associated decrease in cerebral perfusion may be aggravated.
Caffeine therapy is started regularly in infants born at <28 weeks gestational age, and in more mature infants, it is prescribed based upon an increased frequency of minor apnoea, the occurrence of severe apnoea or the presence of respiratory support. Cessation of caffeine therapy is attempted when the apnoea-free infant reaches 32 weeks postmenstrual age. This is successful ~80 % of the time (Spitzer 2002) ensuring a sufficient period for caffeine elimination prior to a hospital discharge decision. Recurrence of apnoea off caffeine may indicate that the apnoea is not idiopathic, e.g. infection related (Darnall et al. 1997).
Natural History/Discharge/Home Monitoring
The duration of apnoea is inversely related to the postmenstrual age at birth. In general, apnoea is absent by 37–40 weeks in those born at >28 weeks postmenstrual age (Darnall et al. 1997; Eichenwald et al. 1997). By contrast, for those born at <28 weeks, apnoea can persist up to 44 weeks postmenstrual age (Darnall et al. 1997; Eichenwald et al. 1997). Home monitoring is indicated under certain circumstances (Table 47.4). There is no evidence for an association between apnoea of prematurity and SIDS, nor has monitoring for apnoea of prematurity been shown to affect the incidence of SIDS (Darnall et al. 2006). If caffeine therapy has been discontinued and the infant has been free of apnoea and bradycardia for 5–7 days, then discharge is not delayed and home monitoring is not prescribed. Infants should adopt a ‘back to sleep’ posture prior to discharge and be tested in a car seat. Families should receive regular SIDS counselling advice, including the avoidance of sleeping in situations where the infant can be compressed or have their upper airway blocked.
Table 47.4.
Indications for home monitoring
| Persistent apnoea and bradycardia (43 weeks) |
| Apnoea and bradycardia with gastroesophageal reflux |
| Apnoea and bradycardia with other pathology |
| Xanthine therapy |
| Home oxygen – bronchopulmonary dysplasia |
| Tracheostomy |
| Home ventilator |
Prognosis/Follow-Up
Recurrent preterm apnoea may result in short-term and/or long-term morbidity (Abu-Shaweesh and Martin 2008; Darnall et al. 1997). However, no definitive proof exists that apnoea of prematurity per se causes neurodevelopmental delay, as it is almost impossible to control for the multiple confounding intrinsic and extrinsic factors that can influence brain development in the neonatal period and thereafter. Ongoing apnoea in infancy requires investigation and treatment. Follow-up of high-risk preterm infants and provision of required interventions and educational assistance are advised.
Essentials to Remember
Breathing consists of motor acts that enable ventilation and maintain airway stability.
Breathing muscle activities can alter rapidly to ensure airway protection or coordinate with other simultaneous motor functions. Afferent inputs monitor breathing rapidly.
Breathing patterns and apnoea can be viewed as a spectrum.
Apnoea, a lack of tidal airflow, can be physiological or pathological.
Apnoea of prematurity is categorised into central, mixed and obstructive types. It is often accompanied by bradycardia and oxygen desaturation. Thus, severe apnoea is life-threatening.
Apnoea results from changes in the central outputs to the muscles of breathing and changes induced by altered intrinsic/extrinsic, central/peripheral and neural/chemical inputs.
Apnoea is exaggerated when upper airway afferents are stimulated during central depression. This can be evident during intubation of the sedated patient.
Conditions associated with clinical apnoea are excluded before a diagnosis of idiopathic apnoea of prematurity is made.
Apnoea can recur postoperatively in former preterm infants up to ~60 postmenstrual weeks, and this is exaggerated with anaemia. Perioperative caffeine therapy may prevent this apnoea.
Management includes avoiding factors that trigger apnoea and non-pharmacologic and pharmacologic therapies, the latter usually with caffeine which, using recommended dosing, has short-term and long-term respiratory and neurodevelopmental benefits.
Knowledge of the natural history of apnoea of prematurity and caffeine pharmacokinetics allows for the planning of safe home discharge and home monitoring, if required.
Follow-up for interim medical care and neurodevelopmental evaluation is advised.
Acknowledgements The author thanks L.S. Segers, PhD; B.G. Lindsey, PhD; B.M. Schnapf, DO; and F. Marchal, MD, for critical review and J.D. Carver, PhD, and M-F. Hutchison, MA, for editorial input.
Contributor Information
Peter C. Rimensberger, Phone: 22382 4323, FAX: 22382 4675, Email: peter.rimensberger@hcuge.ch
Desmond Bohn, Email: desmond.bohn@criticall.org.
Peter A. Dargaville, Email: peter.dargaville@dhhs.tas.gov.au
Peter G. Davis, Email: pgd@unimelb.edu.au
Alastair A. Hutchison, Email: ahutchi2@health.usf.edu, Email: aahutch@msn.com
Louise S. Owen, Email: owen@thewomens.org.au
References
- Abu-Osba YK. Treatment of persistent pulmonary hypertension of the newborn: update. Arch Dis Child. 1991;66:74–77. doi: 10.1136/adc.66.1_spec_no.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Shaweesh JM, Martin RJ. Neonatal apnea: what’s new? Pediatr Pulmonol. 2008;43:937–944. doi: 10.1002/ppul.20832. [DOI] [PubMed] [Google Scholar]
- Adams FH, Fujiwara T, Emmanouilides GC, Raiha N. Lung phospholipids of human fetuses and infants with and without hyaline membrane disease. J Pediatr. 1970;77(5):833–841. doi: 10.1016/s0022-3476(70)80244-x. [DOI] [PubMed] [Google Scholar]
- Adrian ED. Afferent impulses in the vagus and their effect on respiration. J Physiol. 1933;79:332–358. doi: 10.1113/jphysiol.1933.sp003053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aghai ZH, Saslow JG, Nakhla T, Milcarek B, Hart J, Lawrysh-Plunkett R, et al. Synchronized nasal intermittent positive pressure ventilation (SNIPPV) decreases work of breathing (WOB) in premature infants with respiratory distress syndrome (RDS) compared to nasal continuous positive airway pressure (NCPAP) Pediatr Pulmonol. 2006;41(9):875–881. doi: 10.1002/ppul.20461. [DOI] [PubMed] [Google Scholar]
- Aghajafari F, Murphy K, Matthews S, Ohlsson A, Amankwah K, Hannah M. Repeated doses of antenatal corticosteroids in animals: a systematic review. Am J Obstet Gynecol. 2002;186(4):843–849. doi: 10.1067/mob.2002.121624. [DOI] [PubMed] [Google Scholar]
- Ahluwalia JS, White DK, Morley CJ. Infant Flow Driver or single prong nasal continuous positive airway pressure: short-term physiological effects. Acta Paediatr. 1998;87(3):325–327. doi: 10.1080/08035259850157408. [DOI] [PubMed] [Google Scholar]
- Ali N, Claure N, Alegria X, D’Ugard C, Organero R, Bancalari E. Effects of non-invasive pressure support ventilation (NI-PSV) on ventilation and respiratory effort in very low birth weight infants. Pediatr Pulmonol. 2007;42(8):704–710. doi: 10.1002/ppul.20641. [DOI] [PubMed] [Google Scholar]
- Al-Matary A, Kutbi I, Qurashi M, Khalil M, Alvaro R, Kwiatkowski K, Cates D, Rigatto H. Increased peripheral chemoreceptor activity may be critical in destabilizing breathing in neonates. Semin Perinatol. 2004;28:264–272. doi: 10.1053/j.semperi.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Al-Shanafey S, Giacomantonio M, Henteleff H. Congenital diaphragmatic hernia: experience without extracorporeal membrane oxygenation. Pediatr Surg Int. 2002;18(1):28–31. doi: 10.1007/s003830200006. [DOI] [PubMed] [Google Scholar]
- Alvaro RE, Weintraub Z, Kwiatkowski K, Cates DB, Rigatto H. A respiratory sensory reflex in response to CO2 inhibits breathing in preterm infants. J Appl Physiol. 1992;73:1558–1563. doi: 10.1152/jappl.1992.73.4.1558. [DOI] [PubMed] [Google Scholar]
- Aly H, Milner JD, Patel K, El-Mohandes AA. Does the experience with the use of nasal continuous positive airway pressure improve over time in extremely low birth weight infants? Pediatrics. 2004;114(3):697–702. doi: 10.1542/peds.2003-0572-L. [DOI] [PubMed] [Google Scholar]
- Aly H, Massaro AN, Hammad TA, Narang S, Essers J. Early nasal continuous positive airway pressure and necrotizing enterocolitis in preterm infants. Pediatrics. 2009;124(1):205–210. doi: 10.1542/peds.2008-2588. [DOI] [PubMed] [Google Scholar]
- Ambalavanan N, Carlo WA. Ventilatory strategies in the prevention and management of bronchopulmonary dysplasia. Semin Perinatol. 2006;30(4):192–199. doi: 10.1053/j.semperi.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Ammari A, Suri M, Milisavljevic V, Sahni R, Bateman D, Sanocka U, et al. Variables associated with the early failure of nasal CPAP in very low birth weight infants. J Pediatr. 2005;147(3):341–347. doi: 10.1016/j.jpeds.2005.04.062. [DOI] [PubMed] [Google Scholar]
- Anderson PJ, Doyle LW. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin Perinatol. 2006;30(4):227–232. doi: 10.1053/j.semperi.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Annibale DJ, Hulsey TC, Engstrom PC, Wallin LA, Ohning BL. Randomized, controlled trial of nasopharyngeal continuous positive airway pressure in the extubation of very low birth weight infants. J Pediatr. 1994;124(3):455–460. doi: 10.1016/s0022-3476(94)70375-2. [DOI] [PubMed] [Google Scholar]
- Annibale DJ, Hulsey TC, Wagner CL, Southgate WM. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995;149(8):862–867. doi: 10.1001/archpedi.1995.02170210036006. [DOI] [PubMed] [Google Scholar]
- Apisarnthanarak A, Holzmann-Pazgal G, Hamvas A, Olsen MA, Fraser VJ. Ventilator-associated pneumonia in extremely preterm neonates in a neonatal intensive care unit: characteristics, risk factors, and outcomes. Pediatrics. 2003;112:1283–1289. doi: 10.1542/peds.112.6.1283. [DOI] [PubMed] [Google Scholar]
- Aranda JV, Carlo W, Hummel P, Thomas R, Lehr VT, Anand KJ. Analgesia and sedation during mechanical ventilation in neonates. Clin Ther. 2005;27:877–899. doi: 10.1016/j.clinthera.2005.06.019. [DOI] [PubMed] [Google Scholar]
- Arena F, Romeo C, Baldari S, Arena S, Antonuccio P, Campenni A, et al. Gastrointestinal sequelae in survivors of congenital diaphragmatic hernia. Pediatr Int. 2008;50(1):76–80. doi: 10.1111/j.1442-200X.2007.02527.x. [DOI] [PubMed] [Google Scholar]
- Arioni C, Bellini C, Scopesi F, Mazzella M, Serra G. Pulmonary interstitial emphysema in preterm twins on continuous positive airway pressure. J Matern Fetal Neonatal Med. 2006;19(10):671–673. doi: 10.1080/14767050600853344. [DOI] [PubMed] [Google Scholar]
- Austin MT, Lovvorn HN, 3rd, Feurer ID, Pietsch J, Earl TM, Bartilson R, et al. Congenital diaphragmatic hernia repair on extracorporeal life support: a decade of lessons learned. Am Surg. 2004;70(5):389–395. [PubMed] [Google Scholar]
- Auten RL, Notter RH, Kendig JW, Davis JM, Shapiro DL. Surfactant treatment of full-term newborns with respiratory failure. Pediatrics. 1991;87:101–107. [PubMed] [Google Scholar]
- Avery ME, Fletcher BD, Williams RG (1981) The lung and its disorders in the newborn infant. Major Probl Clin Pediatr. 1 4th Edition:1–367 [PubMed]
- Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987;79(1):26–30. [PubMed] [Google Scholar]
- Azarow K, Messineo A, Pearl R, Filler R, Barker G, Bohn D. Congenital diaphragmatic hernia – a tale of two cities: the Toronto experience. J Pediatr Surg. 1997;32(3):395–400. doi: 10.1016/s0022-3468(97)90589-3. [DOI] [PubMed] [Google Scholar]
- Bagolan P, Morini F. Long-term follow up of infants with congenital diaphragmatic hernia. Semin Pediatr Surg. 2007;16(2):134–144. doi: 10.1053/j.sempedsurg.2007.01.009. [DOI] [PubMed] [Google Scholar]
- Bagolan P, Casaccia G, Crescenzi F, Nahom A, Trucchi A, Giorlandino C. Impact of a current treatment protocol on outcome of high-risk congenital diaphragmatic hernia. J Pediatr Surg. 2004;39(3):313–318. doi: 10.1016/j.jpedsurg.2003.11.009. [DOI] [PubMed] [Google Scholar]
- Bahrami KR, Van Meurs KP. ECMO for neonatal respiratory failure. Semin Perinatol. 2005;29(1):15–23. doi: 10.1053/j.semperi.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Bancalari E, del Moral T. Bronchopulmonary dysplasia and surfactant. Biol Neonate. 2001;80(Suppl 1):7–13. doi: 10.1159/000047170. [DOI] [PubMed] [Google Scholar]
- Bang AT, Bang RA, Morankar VP, Sontakke PG, Solanki JM. Pneumonia in neonates: can it be managed in the community? Arch Dis Child. 1993;68:550–556. doi: 10.1136/adc.68.5_spec_no.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington KJ, Bull D, Finer NN. Randomized trial of nasal synchronized intermittent mandatory ventilation compared with continuous positive airway pressure after extubation of very low birth weight infants. Pediatrics. 2001;107(4):638–641. doi: 10.1542/peds.107.4.638. [DOI] [PubMed] [Google Scholar]
- Bartlett RH, Gazzaniga AB, Toomasian J, Coran AG, Roloff D, Rucker R. Extracorporeal membrane oxygenation (ECMO) in neonatal respiratory failure. 100 cases. Ann Surg. 1986;204(3):236–245. doi: 10.1097/00000658-198609000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra JE, Rowley DL, Atrash HK. Case fatality rates associated with conditions originating in the perinatal period: United States, 1986 through 1987. Pediatrics. 1992;89(6 Pt 2):1256–1259. [PubMed] [Google Scholar]
- Beck J, Reilly M, Grasselli G, Mirabella L, Slutsky AS, Dunn MS, et al. Patient-ventilator interaction during neurally adjusted ventilatory assist in low birth weight infants. Pediatr Res. 2009;65(6):663–668. doi: 10.1203/PDR.0b013e31819e72ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeram MR, Dhanireddy R. Effects of saline instillation during tracheal suction on lung mechanics in newborn infants. J Perinatol. 1992;12:120–123. [PubMed] [Google Scholar]
- Beligere N, Rao R. Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. J Perinatol. 2008;28(Suppl 3):S93–S101. doi: 10.1038/jp.2008.154. [DOI] [PubMed] [Google Scholar]
- Bell EF, Warburton D, Stonestreet BS, Oh W. Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. N Engl J Med. 1980;302(11):598–604. doi: 10.1056/NEJM198003133021103. [DOI] [PubMed] [Google Scholar]
- Bellu R, de Waal KA, Zanini R (2005) Opioids for neonates receiving mechanical ventilation. Cochrane Database Syst Rev (1):CD004212 [DOI] [PMC free article] [PubMed]
- Berger TM, Allred EN, Van Marter LJ. Antecedents of clinically significant pulmonary hemorrhage among newborn infants. J Perinatol. 2000;20:295–300. doi: 10.1038/sj.jp.7200372. [DOI] [PubMed] [Google Scholar]
- Berggren E, Liljedahl M, Winbladh B, Andreasson B, Curstedt T, Robertson B, et al. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Paediatr. 2000;89(4):460–464. doi: 10.1080/080352500750028195. [DOI] [PubMed] [Google Scholar]
- Bernbaum J, Schwartz IP, Gerdes M, D’Agostino JA, Coburn CE, Polin RA. Survivors of extracorporeal membrane oxygenation at 1 year of age: the relationship of primary diagnosis with health and neurodevelopmental sequelae. Pediatrics. 1995;96(5 Pt 1):907–913. [PubMed] [Google Scholar]
- Bernstein G, Knodel E, Heldt GP. Airway leak size in neonates and autocycling of three flow-triggered ventilators. Crit Care Med. 1995;23:1739–1744. doi: 10.1097/00003246-199510000-00020. [DOI] [PubMed] [Google Scholar]
- Bernstein G, Mannino FL, Heldt GP, et al. Randomized multicenter trial comparing synchronized and conventional intermittent mandatory ventilation in neonates. J Pediatr. 1996;128:453–463. doi: 10.1016/s0022-3476(96)70354-2. [DOI] [PubMed] [Google Scholar]
- Bhandari V, Gavino RG, Nedrelow JH, Pallela P, Salvador A, Ehrenkranz RA, et al. A randomized controlled trial of synchronized nasal intermittent positive pressure ventilation in RDS. J Perinatol. 2007;27(11):697–703. doi: 10.1038/sj.jp.7211805. [DOI] [PubMed] [Google Scholar]
- Bhandari V, Finer NN, Ehrenkranz RA, Saha S, Das A, Walsh MC, et al. Synchronized nasal intermittent positive-pressure ventilation and neonatal outcomes. Pediatrics. 2009;124(2):517–526. doi: 10.1542/peds.2008-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat RY, Rao A. Meconium-stained amniotic fluid and meconium aspiration syndrome: a prospective study. Ann Trop Paediatr. 2008;28:199–203. doi: 10.1179/146532808X335642. [DOI] [PubMed] [Google Scholar]
- Bisceglia M, Belcastro A, Poerio V, Raimondi F, Mesuraca L, Crugliano C, et al. A comparison of nasal intermittent versus continuous positive pressure delivery for the treatment of moderate respiratory syndrome in preterm infants. Minerva Pediatr. 2007;59(2):91–95. [PubMed] [Google Scholar]
- Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res. 1997;42(3):348–355. doi: 10.1203/00006450-199709000-00016. [DOI] [PubMed] [Google Scholar]
- Blennow M, Jonsson B, Dahlstrom A, Sarman I, Bohlin K, Robertson B. Lung function in premature infants can be improved. Surfactant therapy and CPAP reduce the need of respiratory support. Lakartidningen. 1999;96(13):1571–1576. [PubMed] [Google Scholar]
- Bohlin K, Gudmundsdottir T, Katz-Salamon M, Jonsson B, Blennow M. Implementation of surfactant treatment during continuous positive airway pressure. J Perinatol. 2007;27(7):422–427. doi: 10.1038/sj.jp.7211754. [DOI] [PubMed] [Google Scholar]
- Bohn D. Congenital diaphragmatic hernia. Am J Respir Crit Care Med. 2002;166(7):911–915. doi: 10.1164/rccm.200204-304CC. [DOI] [PubMed] [Google Scholar]
- Bohn D, Tamura M, Perrin D, Barker G, Rabinovitch M. Ventilatory predictors of pulmonary hypoplasia in congenital diaphragmatic hernia, confirmed by morphologic assessment. J Pediatr. 1987;111(3):423–431. doi: 10.1016/s0022-3476(87)80474-2. [DOI] [PubMed] [Google Scholar]
- Bolivar JM, Gerhardt T, Gonzalez A, Hummler H, Claure N, Everett R, Bancalari E. Mechanisms for episodes of hypoxemia in preterm infants undergoing mechanical ventilation. J Pediatr. 1995;127:767–773. doi: 10.1016/s0022-3476(95)70171-0. [DOI] [PubMed] [Google Scholar]
- Boloker J, Bateman DA, Wung JT, Stolar CJ. Congenital diaphragmatic hernia in 120 infants treated consecutively with permissive hypercapnea/spontaneous respiration/elective repair. J Pediatr Surg. 2002;37(3):357–366. doi: 10.1053/jpsu.2002.30834. [DOI] [PubMed] [Google Scholar]
- Bond DM, Froese AB. Volume recruitment maneuvers are less deleterious than persistent low lung volumes in the atelectasis-prone rabbit lung during high-frequency oscillation. Crit Care Med. 1993;21(3):402–412. doi: 10.1097/00003246-199303000-00019. [DOI] [PubMed] [Google Scholar]
- Bouchard S, Johnson MP, Flake AW, Howell LJ, Myers LB, Adzick NS, et al. The EXIT procedure: experience and outcome in 31 cases. J Pediatr Surg. 2002;37(3):418–426. doi: 10.1053/jpsu.2002.30839. [DOI] [PubMed] [Google Scholar]
- Bouchut JC, Dubois R, Moussa M, Godard J, Picaud JC, Di Maio M, et al. High frequency oscillatory ventilation during repair of neonatal congenital diaphragmatic hernia. Paediatr Anaesth. 2000;10(4):377–379. doi: 10.1046/j.1460-9592.2000.00503.x. [DOI] [PubMed] [Google Scholar]
- Boumecid H, Rakza T, Abazine A, Klosowski S, Matran R, Storme L. Influence of three nasal continuous positive airway pressure devices on breathing pattern in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2007;92(4):F298–F300. doi: 10.1136/adc.2006.103762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazy JE, Kinney HC, Oakes WJ. Central nervous system structural lesions causing apnea at birth. J Pediatr. 1987;111:163–1757. doi: 10.1016/s0022-3476(87)80062-8. [DOI] [PubMed] [Google Scholar]
- Brion LP, Soll RF (2001) Diuretics for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev (2):CD001454 [DOI] [PubMed]
- British Association of Perinatal Medicine T (2005) Early care of the newborn infant. Statement on current level of evidence
- Brudno DS, Boedy RF, Kanto WP., Jr Compliance, alveolar-arterial oxygen difference, and oxygenation index changes in patients managed with extracorporeal membrane oxygenation. Pediatr Pulmonol. 1990;9:19–23. doi: 10.1002/ppul.1950090105. [DOI] [PubMed] [Google Scholar]
- Bryner BS, West BT, Hirschl RB, Drongowski RA, Lally KP, Lally P, et al. Congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: does timing of repair matter? J Pediatr Surg. 2009;44(6):1165–1171. doi: 10.1016/j.jpedsurg.2009.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buettiker V, Hug MI, Baenziger O, Meyer C, Frey B. Advantages and disadvantages of different nasal CPAP systems in newborns. Intensive Care Med. 2004;30(5):926–930. doi: 10.1007/s00134-004-2267-8. [DOI] [PubMed] [Google Scholar]
- Buss M, Williams G, Dilley A, Jones O. Prevention of heart failure in the management of congenital diaphragmatic hernia by maintaining ductal patency. A case report. J Pediatr Surg. 2006;41(4):e9–e11. doi: 10.1016/j.jpedsurg.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Cacciari A, Ruggeri G, Mordenti M, Ceccarelli PL, Baccarini E, Pigna A, et al. High-frequency oscillatory ventilation versus conventional mechanical ventilation in congenital diaphragmatic hernia. Eur J Pediatr Surg. 2001;11(1):3–7. doi: 10.1055/s-2001-12204. [DOI] [PubMed] [Google Scholar]
- Callen P, Goldsworthy S, Graves L, Harvey D, Mellows H, Parkinson C. Mode of delivery and the lecithin/sphingomyelin ratio. Br J Obstet Gynaecol. 1979;86(12):965–968. doi: 10.1111/j.1471-0528.1979.tb11245.x. [DOI] [PubMed] [Google Scholar]
- Campbell DM, Shah PS, Shah V, Kelly EN. Nasal continuous positive airway pressure from high flow cannula versus infant flow for preterm infants. J Perinatol. 2006;26(9):546–549. doi: 10.1038/sj.jp.7211561. [DOI] [PubMed] [Google Scholar]
- Carlton DP, Cho SC, Davis P, Lont M, Bland RD. Surfactant treatment at birth reduces lung vascular injury and edema in preterm lambs. Pediatr Res. 1995;37:265–270. doi: 10.1203/00006450-199503000-00003. [DOI] [PubMed] [Google Scholar]
- Carter JM, Gerstmann DR, Clark RH, et al. High-frequency oscillatory ventilation and extracorporeal membrane oxygenation for the treatment of acute neonatal respiratory failure. Pediatrics. 1990;85:159–164. [PubMed] [Google Scholar]
- Castellheim A, Lindenskov PH, Pharo A, Aamodt G, Saugstad OD, Mollnes TE. Meconium aspiration syndrome induces complement-associated systemic inflammatory response in newborn piglets. Scand J Immunol. 2005;61:217–225. doi: 10.1111/j.1365-3083.2005.01532.x. [DOI] [PubMed] [Google Scholar]
- Castillo A, Sola A, Baquero H, Neira F, Alvis R, Deulofeut R, et al. Pulse oxygen saturation levels and arterial oxygen tension values in newborns receiving oxygen therapy in the neonatal intensive care unit: is 85% to 93% an acceptable range? Pediatrics. 2008;121(5):882–889. doi: 10.1542/peds.2007-0117. [DOI] [PubMed] [Google Scholar]
- Cayabyab RG, Kwong K, Jones C, Minoo P, Durand M. Lung inflammation and pulmonary function in infants with meconium aspiration syndrome. Pediatr Pulmonol. 2007;42:898–905. doi: 10.1002/ppul.20675. [DOI] [PubMed] [Google Scholar]
- Chan V, Greenough A. Comparison of weaning by patient triggered ventilation or synchronous intermittent mandatory ventilation in preterm infants. Acta Paediatr. 1994;83(3):335–337. doi: 10.1111/j.1651-2227.1994.tb18108.x. [DOI] [PubMed] [Google Scholar]
- Chang GY, Cox CC, Shaffer TH (2005) Nasal cannula, CPAP and Vapotherm: effect of flow on temperature, humidity, pressure and resistance. Pediatric Academic Society, Washinton, DC, p 1248
- Cheema IU, Ahluwalia JS. Feasibility of tidal volume-guided ventilation in newborn infants: a randomized, crossover trial using the volume guarantee modality. Pediatrics. 2001;107(6):1323–1328. doi: 10.1542/peds.107.6.1323. [DOI] [PubMed] [Google Scholar]
- Chen JY, Ling UP, Chen JH. Comparison of synchronized and conventional intermittent mandatory ventilation in neonates. Acta Paediatr Jpn. 1997;39:578–583. doi: 10.1111/j.1442-200x.1997.tb03644.x. [DOI] [PubMed] [Google Scholar]
- Chen XK, Lougheed J, Lawson ML, Gibb W, Walker RC, Wen SW, et al. Effects of repeated courses of antenatal corticosteroids on somatic development in children 6 to 10 years of age. Am J Perinatol. 2008;25(1):21–28. doi: 10.1055/s-2007-995222. [DOI] [PubMed] [Google Scholar]
- Chinese Collaborative Study Group for Neonatal Respiratory Diseases Treatment of severe meconium aspiration syndrome with porcine surfactant: a multicentre, randomized, controlled trial. Acta Paediatr. 2005;94:896–902. doi: 10.1111/j.1651-2227.2005.tb02008.x. [DOI] [PubMed] [Google Scholar]
- Chiu P, Hedrick HL. Postnatal management and long-term outcome for survivors with congenital diaphragmatic hernia. Prenat Diagn. 2008;28(7):592–603. doi: 10.1002/pd.2007. [DOI] [PubMed] [Google Scholar]
- Chiu PP, Sauer C, Mihailovic A, Adatia I, Bohn D, Coates AL, et al. The price of success in the management of congenital diaphragmatic hernia: is improved survival accompanied by an increase in long-term morbidity? J Pediatr Surg. 2006;41(5):888–892. doi: 10.1016/j.jpedsurg.2006.01.026. [DOI] [PubMed] [Google Scholar]
- Cho SD, Krishnaswami S, McKee JC, Zallen G, Silen ML, Bliss DW. Analysis of 29 consecutive thoracoscopic repairs of congenital diaphragmatic hernia in neonates compared to historical controls. J Pediatr Surg. 2009;44(1):80–86. doi: 10.1016/j.jpedsurg.2008.10.013. [DOI] [PubMed] [Google Scholar]
- Chou P, Blei ED, Shen-Schwarz S, Gonzalez-Crussi F, Reynolds M. Pulmonary changes following extracorporeal membrane oxygenation: autopsy study of 23 cases. Hum Pathol. 1993;24:405–412. doi: 10.1016/0046-8177(93)90089-y. [DOI] [PubMed] [Google Scholar]
- Claure N, Bancalari E. Mechanical ventilatory support in preterm infants. Minerva Pediatr. 2008;60(2):177–182. [PubMed] [Google Scholar]
- Cleary GM, Wiswell TE. Meconium-stained amniotic fluid and the meconium aspiration syndrome. An update. Pediatr Clin North Am. 1998;45:511–529. doi: 10.1016/s0031-3955(05)70025-0. [DOI] [PubMed] [Google Scholar]
- Cleary JP, Bernstein G, Mannino FL, Heldt GP. Improved oxygenation during synchronized intermittent mandatory ventilation in neonates with respiratory distress syndrome: a randomized, crossover study. J Pediatr. 1995;126(3):407–411. doi: 10.1016/s0022-3476(95)70460-4. [DOI] [PubMed] [Google Scholar]
- Cochrane CG, Revak SD, Merritt TA, et al. Bronchoalveolar lavage with KL4-surfactant in models of meconium aspiration syndrome. Pediatr Res. 1998;44:705–715. doi: 10.1203/00006450-199811000-00013. [DOI] [PubMed] [Google Scholar]
- Cohen M, Carson BS. Respiratory morbidity benefit of awaiting onset of labor after elective cesarean section. Obstet Gynecol. 1985;65(6):818–824. [PubMed] [Google Scholar]
- Cohen MS, Rychik J, Bush DM, Tian ZY, Howell LJ, Adzick NS, et al. Influence of congenital heart disease on survival in children with congenital diaphragmatic hernia. J Pediatr. 2002;141(1):25–30. doi: 10.1067/mpd.2002.125004. [DOI] [PubMed] [Google Scholar]
- Colaizy TT, Younis UM, Bell EF, Klein JM. Nasal high-frequency ventilation for premature infants. Acta Paediatr. 2008;97(11):1518–1522. doi: 10.1111/j.1651-2227.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole FS, Hamvas A, Rubinstein P, King E, Trusgnich M, Nogee LM, et al. Population-based estimates of surfactant protein B deficiency. Pediatrics. 2000;105(3 Pt 1):538–541. doi: 10.1542/peds.105.3.538. [DOI] [PubMed] [Google Scholar]
- Cools F, Offringa M (2005) Neuromuscular paralysis for newborn infants receiving mechanical ventilation. Cochrane Database Syst Rev (2):CD002773 [DOI] [PMC free article] [PubMed]
- Cote CJ, Zaslavsky A, Downes JJ, Kurth CD, Welborn LG, Warner LO, Malviya SV. Postoperative apnea in former preterm infants after inguinal herniorrhaphy. A combined analysis. Anesthesiology. 1995;82:809–822. doi: 10.1097/00000542-199504000-00002. [DOI] [PubMed] [Google Scholar]
- Cotton RB, Olsson T, Law AB, Parker RA, Lindstrom DP, Silberberg AR, et al. The physiologic effects of surfactant treatment on gas exchange in newborn premature infants with hyaline membrane disease. Pediatr Res. 1993;34(4):495–501. doi: 10.1203/00006450-199310000-00022. [DOI] [PubMed] [Google Scholar]
- Courtney SE, Barrington KJ. Continuous positive airway pressure and noninvasive ventilation. Clin Perinatol. 2007;34(1):73–92. doi: 10.1016/j.clp.2006.12.008. [DOI] [PubMed] [Google Scholar]
- Courtney SE, Pyon KH, Saslow JG, Arnold GK, Pandit PB, Habib RH. Lung recruitment and breathing pattern during variable versus continuous flow nasal continuous positive airway pressure in premature infants: an evaluation of three devices. Pediatrics. 2001;107(2):304–308. doi: 10.1542/peds.107.2.304. [DOI] [PubMed] [Google Scholar]
- Courtney SE, Durand DJ, Asselin JM, Hudak ML, Aschner JL, Shoemaker CT. High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N Engl J Med. 2002;347(9):643–652. doi: 10.1056/NEJMoa012750. [DOI] [PubMed] [Google Scholar]
- Crowley PA. Antenatal corticosteroid therapy: a meta-analysis of the randomized trials, 1972 to 1994. Am J Obstet Gynecol. 1995;173(1):322–335. doi: 10.1016/0002-9378(95)90222-8. [DOI] [PubMed] [Google Scholar]
- Crowther CA, Harding JE (2007) Repeat doses of prenatal corticosteroids for women at risk of preterm birth for preventing neonatal respiratory disease. Cochrane Database Syst Rev. (3):CD003935 [DOI] [PubMed]
- Crowther CA, Doyle LW, Haslam RR, Hiller JE, Harding JE, Robinson JS. Outcomes at 2 years of age after repeat doses of antenatal corticosteroids. N Engl J Med. 2007;357(12):1179–1189. doi: 10.1056/NEJMoa071152. [DOI] [PubMed] [Google Scholar]
- Cuestas RA, Lindall A, Engel RR. Low thyroid hormones and respiratory-distress syndrome of the newborn. Studies on cord blood. N Engl J Med. 1976;295(6):297–302. doi: 10.1056/NEJM197608052950601. [DOI] [PubMed] [Google Scholar]
- D’Agostino JA, Bernbaum JC, Gerdes M, Schwartz IP, Coburn CE, Hirschl RB, et al. Outcome for infants with congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: the first year. J Pediatr Surg. 1995;30(1):10–15. doi: 10.1016/0022-3468(95)90598-7. [DOI] [PubMed] [Google Scholar]
- D’Angio CT, Chess PR, Kovacs SJ, Sinkin RA, Phelps DL, Kendig JW, et al. Pressure-regulated volume control ventilation vs synchronized intermittent mandatory ventilation for very low-birth-weight infants: a randomized controlled trial. Arch Pediatr Adolesc Med. 2005;159(9):868–875. doi: 10.1001/archpedi.159.9.868. [DOI] [PubMed] [Google Scholar]
- Daly M d B. Peripheral arterial chemoreceptors and respiratory-cardiovascular integration. Oxford: Oxford University Press; 1997. Clinical implications of chemoreceptor reflexes; pp. 557–589. [Google Scholar]
- Dargaville PA, Copnell B. The epidemiology of meconium aspiration syndrome: incidence, risk factors, therapies, and outcome. Pediatrics. 2006;117:1712–1721. doi: 10.1542/peds.2005-2215. [DOI] [PubMed] [Google Scholar]
- Dargaville PA, Mills JF. Surfactant therapy for meconium aspiration syndrome: current status. Drugs. 2005;65:2569–2591. doi: 10.2165/00003495-200565180-00003. [DOI] [PubMed] [Google Scholar]
- Dargaville PA, South M, McDougall PN. Surfactant and surfactant inhibitors in meconium aspiration syndrome. J Pediatr. 2001;138:113–115. doi: 10.1067/mpd.2001.109602. [DOI] [PubMed] [Google Scholar]
- Dargaville PA, Mills JF, Headley BM, et al. Therapeutic lung lavage in the piglet model of meconium aspiration syndrome. Am J Respir Crit Care Med. 2003;168:456–463. doi: 10.1164/rccm.200301-121OC. [DOI] [PubMed] [Google Scholar]
- Dargaville PA, Mills JF, Copnell B, Loughnan PM, McDougall PN, Morley CJ. Therapeutic lung lavage in meconium aspiration syndrome: a preliminary report. J Paediatr Child Health. 2007;43:539–545. doi: 10.1111/j.1440-1754.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Dargaville PA, Copnell B, Mills JF, Haron I, Lee JKF, Tingay DG et al (2011) Randomized controlled trial of lung lavage with dilute surfactant for meconium aspiration syndrome. J Pediatr 158:383–389 [DOI] [PubMed]
- Darnall RA, Kattwinkel J, Nattie C, Robinson M. Margin of safety for discharge after apnea in preterm infants. Pediatrics. 1997;100:795–801. doi: 10.1542/peds.100.5.795. [DOI] [PubMed] [Google Scholar]
- Darnall RA, Ariagno RL, Kinney HC. The late preterm infant and the control of breathing, sleep, and brainstem development: a review. Clin Perinatol. 2006;33:883–914. doi: 10.1016/j.clp.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Davey AM, Becker JD, Davis JM. Meconium aspiration syndrome: physiological and inflammatory changes in a newborn piglet model. Pediatr Pulmonol. 1993;16:101–108. doi: 10.1002/ppul.1950160205. [DOI] [PubMed] [Google Scholar]
- Davies PA, Aherne W. Congenital pneumonia. Arch Dis Child. 1962;37:598–602. doi: 10.1136/adc.37.196.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies AM, Koenig JS, Thach BT. Upper airway chemoreflex responses to saline and water in preterm infants. J Appl Physiol. 1988;64:1412–1420. doi: 10.1152/jappl.1988.64.4.1412. [DOI] [PubMed] [Google Scholar]
- Davis GM, Bureau MA. Pulmonary and chest wall mechanics in the control of respiration in the newborn. Clin Perinatol. 1987;14(3):551–579. [PubMed] [Google Scholar]
- Davis PG, Henderson-Smart DJ (2000) Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev (3):CD000143 [DOI] [PubMed]
- Davis PG, Henderson-Smart DJ (2001) Extubation from low-rate intermittent positive airways pressure versus extubation after a trial of endotracheal continuous positive airways pressure in intubated preterm infants. Cochrane Database Syst Rev (4):CD001078 [DOI] [PubMed]
- Davis PG, Henderson-Smart DJ (2003) Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev (2):CD000143 [DOI] [PubMed]
- Davis JM, Richter SE, Kendig JW, Notter RH. High-frequency jet ventilation and surfactant treatment of newborns with severe respiratory failure. Pediatr Pulmonol. 1992;13:108–112. doi: 10.1002/ppul.1950130209. [DOI] [PubMed] [Google Scholar]
- Davis PG, Lemyre B, de Paoli AG (2001) Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev (3):CD003212 [DOI] [PubMed]
- Davis PG, Tan A, O’Donnell CP, Schulze A. Resuscitation of newborn infants with 100% oxygen or air: a systematic review and meta-analysis. Lancet. 2004;364(9442):1329–1333. doi: 10.1016/S0140-6736(04)17189-4. [DOI] [PubMed] [Google Scholar]
- Davis PJ, Firmin RK, Manktelow B, Goldman AP, Davis CF, Smith JH, et al. Long-term outcome following extracorporeal membrane oxygenation for congenital diaphragmatic hernia: the UK experience. J Pediatr. 2004;144(3):309–315. doi: 10.1016/j.jpeds.2003.11.031. [DOI] [PubMed] [Google Scholar]
- Davis PG, Morley CJ, Owen LS. Non-invasive respiratory support of preterm neonates with respiratory distress: continuous positive airway pressure and nasal intermittent positive pressure ventilation. Semin Fetal Neonatal Med. 2009;14(1):14–20. doi: 10.1016/j.siny.2008.08.003. [DOI] [PubMed] [Google Scholar]
- Dawson JA, Kamlin COF, Vento MT, Wong C, Donath S, Davis PG, Morley CJ (2009) Defining the ‘normal’ range for oxygen saturations in newly born infants. Pediatric Academic Society, Baltimore
- Dawson JA, Kamlin COF, Te Pas AB, Schmoelzer G, Donath SM, O’Donnell CPF, Davis PG, Morley CJ (2009) Neopuff compared with Laerdal self-inflating bag for the first five minutes of resuscitation in infants < 29 weeks gestation at birth: a randomized controlled trial. Pediatric Academic Society, Baltimore, 3212.7
- de Beaufort AJ, Pelikan DM, Elferink JG, Berger HM. Effect of interleukin 8 in meconium on in-vitro neutrophil chemotaxis. Lancet. 1998;352:102–105. doi: 10.1016/S0140-6736(98)85013-7. [DOI] [PubMed] [Google Scholar]
- De Klerk AM, De Klerk RK. Nasal continuous positive airway pressure and outcomes of preterm infants. J Paediatr Child Health. 2001;37(2):161–167. doi: 10.1046/j.1440-1754.2001.00624.x. [DOI] [PubMed] [Google Scholar]
- De Paoli AG, Morley CJ, Davis PG, Lau R, Hingeley E. In vitro comparison of nasal continuous positive airway pressure devices for neonates. Arch Dis Child Fetal Neonatal Ed. 2002;87(1):F42–F45. doi: 10.1136/fn.87.1.F42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Paoli AG, Lau R, Davis PG, Morley CJ. Pharyngeal pressure in preterm infants receiving nasal continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 2005;90(1):F79–F81. doi: 10.1136/adc.2004.052274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Paoli AG, Davis PG, Faber B, Morley CJ (2008) Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database Syst Rev (1):CD002977 [DOI] [PMC free article] [PubMed]
- Desfrere L, Jarreau PH, Dommergues M, Brunhes A, Hubert P, Nihoul-Fekete C, et al. Impact of delayed repair and elective high-frequency oscillatory ventilation on survival of antenatally diagnosed congenital diaphragmatic hernia: first application of these strategies in the more “severe” subgroup of antenatally diagnosed newborns. Intensive Care Med. 2000;26(7):934–941. doi: 10.1007/s001340051284. [DOI] [PubMed] [Google Scholar]
- Dessens AB, Haas HS, Koppe JG. Twenty-year follow-up of antenatal corticosteroid treatment. Pediatrics. 2000;105(6):E77. doi: 10.1542/peds.105.6.e77. [DOI] [PubMed] [Google Scholar]
- Dhanireddy R, Smith YF, Hamosh M, Mullon DK, Scanlon JW, Hamosh P. Respiratory distress syndrome in the newborn: relationship to serum prolactin, thyroxine, and sex. Biol Neonate. 1983;43(1–2):9–15. doi: 10.1159/000241631. [DOI] [PubMed] [Google Scholar]
- Dillon PW, Cilley RE, Hudome SM, Ozkan EN, Krummel TM. Nitric oxide reversal of recurrent pulmonary hypertension and respiratory failure in an infant with CDH after successful ECMO therapy. J Pediatr Surg. 1995;30(5):743–744. doi: 10.1016/0022-3468(95)90706-8. [DOI] [PubMed] [Google Scholar]
- Dillon PW, Cilley RE, Mauger D, Zachary C, Meier A. The relationship of pulmonary artery pressure and survival in congenital diaphragmatic hernia. J Pediatr Surg. 2004;39(3):307–312. doi: 10.1016/j.jpedsurg.2003.11.010. [DOI] [PubMed] [Google Scholar]
- Dimitriou G, Greenough A. Measurement of lung volume and optimal oxygenation during high frequency oscillation. Arch Dis Child Fetal Neonatal Ed. 1995;72:F180–F183. doi: 10.1136/fn.72.3.f180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitriou G, Greenough A, Griffin F, Chan V. Synchronous intermittent mandatory ventilation modes compared with patient triggered ventilation during weaning. Arch Dis Child Fetal Neonatal Ed. 1995;72(3):F188–F190. doi: 10.1136/fn.72.3.f188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitriou G, Greenough A, Laubscher B, Yamaguchi N. Comparison of airway pressure-triggered and airflow-triggered ventilation in very immature infants. Acta Paediatr. 1998;87(12):1256–1260. doi: 10.1080/080352598750030942. [DOI] [PubMed] [Google Scholar]
- Dimitriou G, Greenough A, Cherian S. Comparison of airway pressure and airflow triggering systems using a single type of neonatal ventilator. Acta Paediatr. 2001;90(4):445–447. [PubMed] [Google Scholar]
- Dimmitt RA, Moss RL, Rhine WD, Benitz WE, Henry MC, Vanmeurs KP. Venoarterial versus venovenous extracorporeal membrane oxygenation in congenital diaphragmatic hernia: the Extracorporeal Life Support Organization Registry, 1990–1999. J Pediatr Surg. 2001;36(8):1199–1204. doi: 10.1053/jpsu.2001.25762. [DOI] [PubMed] [Google Scholar]
- Donn SM, Sinha SK. Invasive and noninvasive neonatal mechanical ventilation. Respir Care. 2003;48:426–439. [PubMed] [Google Scholar]
- Donn SM, Sinha SK. Minimising ventilator induced lung injury in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2006;91(3):F226–F230. doi: 10.1136/adc.2005.082271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downard CD, Jaksic T, Garza JJ, Dzakovic A, Nemes L, Jennings RW, et al. Analysis of an improved survival rate for congenital diaphragmatic hernia. J Pediatr Surg. 2003;38(5):729–732. doi: 10.1016/jpsu.2003.50194. [DOI] [PubMed] [Google Scholar]
- Dreyfuss D, Saumon G. Barotrauma is volutrauma, but which volume is the one responsible? Intensive Care Med. 1992;18(3):139–141. doi: 10.1007/BF01709236. [DOI] [PubMed] [Google Scholar]
- Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med. 1998;157(1):294–323. doi: 10.1164/ajrccm.157.1.9604014. [DOI] [PubMed] [Google Scholar]
- Drummond WH, Gregory GA, Heymann MA, Phibbs RA. The independent effects of hyperventilation, tolazoline, and dopamine on infants with persistent pulmonary hypertension. J Pediatr. 1981;98(4):603–611. doi: 10.1016/s0022-3476(81)80775-5. [DOI] [PubMed] [Google Scholar]
- Duenhoelter JH, Pritchard JA. Fetal respiration. A review. Am J Obstet Gynecol. 1977;129:326–338. doi: 10.1016/0002-9378(77)90793-1. [DOI] [PubMed] [Google Scholar]
- Duke T. Neonatal pneumonia in developing countries. Arch Dis Child Fetal Neonatal Ed. 2005;90:F211–F219. doi: 10.1136/adc.2003.048108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunser MW, Mayr AJ, Ulmer H, Ritsch N, Knotzer H, Pajk W, et al. The effects of vasopressin on systemic hemodynamics in catecholamine-resistant septic and postcardiotomy shock: a retrospective analysis. Anesth Analg. 2001;93(1):7–13. doi: 10.1097/00000539-200107000-00003. [DOI] [PubMed] [Google Scholar]
- Duran R, Ulfet V, Mustafa Y, Betul A. An unusual complication of nasopharyngeal CPAP in a premature infant. Paediatr Anaesth. 2005;15(10):903–905. doi: 10.1111/j.1460-9592.2005.01670.x. [DOI] [PubMed] [Google Scholar]
- Durand M, McCann E, Brady JP. Effect of continuous positive airway pressure on the ventilatory response to CO2 in preterm infants. Pediatrics. 1983;71(4):634–638. [PubMed] [Google Scholar]
- Early versus delayed neonatal administration of a synthetic surfactant – the judgment of OSIRIS. The OSIRIS Collaborative Group (open study of infants at high risk of or with respiratory insufficiency – the role of surfactant (1992) Lancet 340(8832):1363–1369 [PubMed]
- Edberg KE, Ekstrom-Jodal B, Hallman M, Hjalmarson O, Sandberg K, Silberberg A. Immediate effects on lung function of instilled human surfactant in mechanically ventilated newborn infants with IRDS. Acta Paediatr Scand. 1990;79(8–9):750–755. doi: 10.1111/j.1651-2227.1990.tb11550.x. [DOI] [PubMed] [Google Scholar]
- Eden RD, Seifert LS, Winegar A, Spellacy WN. Perinatal characteristics of uncomplicated postdate pregnancies. Obstet Gynecol. 1987;69:296–299. [PubMed] [Google Scholar]
- Egan EA, Dillon WP, Zorn S. Fetal lung liquid absorption and alveolar epithelial solute permeability in surfactant deficient, breathing fetal lambs. Pediatr Res. 1984;18(6):566–570. doi: 10.1203/00006450-198406000-00018. [DOI] [PubMed] [Google Scholar]
- Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116(6):1353–1360. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- Eichenwald EC, Ungarelli RA, Stark AR. Hypercapnia increases expiratory braking in preterm infants. J Appl Physiol. 1993;75:2665–2670. doi: 10.1152/jappl.1993.75.6.2665. [DOI] [PubMed] [Google Scholar]
- Eichenwald EC, Aina A, Stark AR. Apnea frequently persists beyond term gestation in infants delivered at 24 to 28 weeks. Pediatrics. 1997;100:354–359. doi: 10.1542/peds.100.3.354. [DOI] [PubMed] [Google Scholar]
- El Shahed AI, Dargaville P, Ohlsson A, Soll RF (2007) Surfactant for meconium aspiration syndrome in full term/near term infants. Cochrane Database Syst Rev (3):CD002054 [DOI] [PubMed]
- Elbourne D, Field D, Mugford M (2002) Extracorporeal membrane oxygenation for severe respiratory failure in newborn infants (Cochrane Review). Cochrane Database Syst Rev (1):CD001340 [DOI] [PubMed]
- Elgellab A, Riou Y, Abbazine A, Truffert P, Matran R, Lequien P, et al. Effects of nasal continuous positive airway pressure (NCPAP) on breathing pattern in spontaneously breathing premature newborn infants. Intensive Care Med. 2001;27(11):1782–1787. doi: 10.1007/s00134-001-1117-1. [DOI] [PubMed] [Google Scholar]
- Engle WD, Arant BS, Jr, Wiriyathian S, Rosenfeld CR. Diuresis and respiratory distress syndrome: physiologic mechanisms and therapeutic implications. J Pediatr. 1983;102(6):912–917. doi: 10.1016/s0022-3476(83)80024-9. [DOI] [PubMed] [Google Scholar]
- Engle WA, Yoder MC, Andreoli SP, Darragh RK, Langefeld CD, Hui SL. Controlled prospective randomized comparison of high-frequency jet ventilation and conventional ventilation in neonates with respiratory failure and persistent pulmonary hypertension. J Perinatol. 1997;17:3–9. [PubMed] [Google Scholar]
- Evans NJ, Archer LN. Doppler assessment of pulmonary artery pressure during recovery from hyaline membrane disease. Arch Dis Child. 1991;66(7 Spec No):802–804. doi: 10.1136/adc.66.7_spec_no.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell PM, Avery ME. Hyaline membrane disease. Am Rev Respir Dis. 1975;111(5):657–688. doi: 10.1164/arrd.1975.111.5.657. [DOI] [PubMed] [Google Scholar]
- Fauza DO, Wilson JM. Congenital diaphragmatic hernia and associated anomalies: their incidence, identification, and impact on prognosis. J Pediatr Surg. 1994;29(8):1113–1117. doi: 10.1016/0022-3468(94)90290-9. [DOI] [PubMed] [Google Scholar]
- Feldman JL, Del Negro CA. Looking for inspiration: new perspectives on respiratory rhythm. Nat Rev. 2006;7:232–242. doi: 10.1038/nrn1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueras-Aloy J, Quero J, Carbonell-Estrany X, Ginovart G, Perez-Rodriguez J, Raspall F, et al. Early administration of the second dose of surfactant (beractant) in the treatment of severe hyaline membrane disease. Acta Paediatr. 2001;90(3):296–301. doi: 10.1080/080352501300067631. [DOI] [PubMed] [Google Scholar]
- Findlay RD, Taeusch HW, Walther FJ. Surfactant replacement therapy for meconium aspiration syndrome. Pediatrics. 1996;97:48–52. [PubMed] [Google Scholar]
- Finer NN, Barrington KJ (2006) Nitric oxide for respiratory failure in infants born at or near term. Cochrane Database Syst Rev (4):CD000399 [DOI] [PubMed]
- Finer NN, Moriartey RR, Boyd J, Phillips HJ, Stewart AR, Ulan O. Postextubation atelectasis: a retrospective review and a prospective controlled study. J Pediatr. 1979;94(1):110–113. doi: 10.1016/s0022-3476(79)80371-6. [DOI] [PubMed] [Google Scholar]
- Finer NN, Carlo WA, Duara S, Fanaroff AA, Donovan EF, Wright LL, et al. Delivery room continuous positive airway pressure/positive end-expiratory pressure in extremely low birth weight infants: a feasibility trial. Pediatrics. 2004;114(3):651–657. doi: 10.1542/peds.2004-0394. [DOI] [PubMed] [Google Scholar]
- Finer NN, Merritt TA, Bernstein G, et al. A multicenter, pilot study of Aerosurf delivered via nasal CPAP to prevent RDS in pre-term neonates. Eur Pediatr Acad Soc. 2006;59:4840. [Google Scholar]
- Fleming PJ, Bryan AC, Bryan MH. Functional immaturity of pulmonary irritant receptors and apnea in newborn preterm infants. Pediatrics. 1978;61:515–518. [PubMed] [Google Scholar]
- Fliman PJ, deRegnier RA, Kinsella JP, Reynolds M, Rankin LL, Steinhorn RH. Neonatal extracorporeal life support: impact of new therapies on survival. J Pediatr. 2006;148:595–599. doi: 10.1016/j.jpeds.2005.12.024. [DOI] [PubMed] [Google Scholar]
- Fowlie PW. Prophylactic indomethacin: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 1996;74(2):F81–F87. doi: 10.1136/fn.74.2.f81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowlie PW, Davis PG. Prophylactic indomethacin for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2003;88(6):F464–F466. doi: 10.1136/fn.88.6.F464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox WW, Berman LS, Downes JJJ, Peckham GJ. The therapeutic application of end-expiratory pressure in the meconium aspiration syndrome. Pediatrics. 1975;56:214–217. [PubMed] [Google Scholar]
- Fox WW, Schwartz JG, Shaffer TH. Successful extubation of neonates: clinical and physiological factors. Crit Care Med. 1981;9(12):823–826. doi: 10.1097/00003246-198112000-00003. [DOI] [PubMed] [Google Scholar]
- Frenckner B, Ehren H, Granholm T, Linden V, Palmer K. Improved results in patients who have congenital diaphragmatic hernia using preoperative stabilization, extracorporeal membrane oxygenation, and delayed surgery. J Pediatr Surg. 1997;32(8):1185–1189. doi: 10.1016/s0022-3468(97)90679-5. [DOI] [PubMed] [Google Scholar]
- Frenckner B, Broome M, Lindstrom M, Radell P. Platelet-derived growth factor inhibition – a new treatment of pulmonary hypertension in congenital diaphragmatic hernia? J Pediatr Surg. 2008;43(10):1928–1931. doi: 10.1016/j.jpedsurg.2008.07.022. [DOI] [PubMed] [Google Scholar]
- Frerichs I, Dargaville PA, Dudykevych T, Rimensberger PC. Electrical impedance tomography: a method for monitoring regional lung aeration and tidal volume distribution? Intensive Care Med. 2003;29(12):2312–2316. doi: 10.1007/s00134-003-2029-z. [DOI] [PubMed] [Google Scholar]
- Frey P, Glanzmann R, Nars P, Herzog B. Familial congenital diaphragmatic defect: transmission from father to daughter. J Pediatr Surg. 1991;26(12):1396–1398. doi: 10.1016/0022-3468(91)91044-y. [DOI] [PubMed] [Google Scholar]
- Friedlich P, Lecart C, Posen R, Ramicone E, Chan L, Ramanathan R. A randomized trial of nasopharyngeal-synchronized intermittent mandatory ventilation versus nasopharyngeal continuous positive airway pressure in very low birth weight infants after extubation. J Perinatol. 1999;19(6 Pt 1):413–418. doi: 10.1038/sj.jp.7200205. [DOI] [PubMed] [Google Scholar]
- Froese AB, Kinsella JP. High-frequency oscillatory ventilation: lessons from the neonatal/pediatric experience. Crit Care Med. 2005;33(3 Suppl):S115–S121. doi: 10.1097/01.ccm.0000155923.97849.6d. [DOI] [PubMed] [Google Scholar]
- Froese AB, McCulloch PR, Sugiura M, Vaclavik S, Possmayer F, Moller F. Optimizing alveolar expansion prolongs the effectiveness of exogenous surfactant therapy in the adult rabbit. Am Rev Respir Dis. 1993;148(3):569–577. doi: 10.1164/ajrccm/148.3.569. [DOI] [PubMed] [Google Scholar]
- Fuchimukai T, Fujiwara T, Takahashi A, Enhorning G. Artificial pulmonary surfactant inhibited by proteins. J Appl Physiol. 1987;62:429–437. doi: 10.1152/jappl.1987.62.2.429. [DOI] [PubMed] [Google Scholar]
- Fujikura T, Froehlich LA. Intrauterine pneumonia in relation to birth weight and race. Am J Obstet Gynecol. 1967;97:81–84. doi: 10.1016/0002-9378(67)90596-0. [DOI] [PubMed] [Google Scholar]
- Gaillard EA, Cooke RW, Shaw NJ. Improved survival and neurodevelopmental outcome after prolonged ventilation in preterm neonates who have received antenatal steroids and surfactant. Arch Dis Child Fetal Neonatal Ed. 2001;84(3):F194–F196. doi: 10.1136/fn.84.3.F194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaon P, Lee S, Hannan S, Ingram D, Milner AD. Assessment of effect of nasal continuous positive pressure on laryngeal opening using fibre optic laryngoscopy. Arch Dis Child Fetal Neonatal Ed. 1999;80(3):F230–F232. doi: 10.1136/fn.80.3.f230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garite TJ, Rumney PJ, Briggs GG, Harding JA, Nageotte MP, Towers CV, et al. A randomized, placebo-controlled trial of betamethasone for the prevention of respiratory distress syndrome at 24 to 28 weeks’ gestation. Am J Obstet Gynecol. 1992;166(2):646–651. doi: 10.1016/0002-9378(92)91691-3. [DOI] [PubMed] [Google Scholar]
- Garland JS, Nelson DB, Rice T, Neu J. Increased risk of gastrointestinal perforations in neonates mechanically ventilated with either face mask or nasal prongs. Pediatrics. 1985;76(3):406–410. [PubMed] [Google Scholar]
- Garland JS, Buck RK, Allred EN, Leviton A. Hypocarbia before surfactant therapy appears to increase bronchopulmonary dysplasia risk in infants with respiratory distress syndrome. Arch Pediatr Adolesc Med. 1995;149(6):617–622. doi: 10.1001/archpedi.1995.02170190027005. [DOI] [PubMed] [Google Scholar]
- Gaston B, Drazen JM, Loscalzo J, Stamler JS. The biology of nitrogen oxides in the airways. Am J Respir Crit Care Med. 1994;149(2 Pt 1):538–551. doi: 10.1164/ajrccm.149.2.7508323. [DOI] [PubMed] [Google Scholar]
- Gauda EB, McLemore GL, Tolosa J, Marston-Nelson J, Kwak D. Maturation of peripheral arterial chemoreceptors in relation to neonatal apnoea. Semin Neonatol. 2004;9:181–194. doi: 10.1016/j.siny.2003.11.002. [DOI] [PubMed] [Google Scholar]
- Gerhardt T, Bancalari E. Apnea of prematurity: I. Lung function and regulation of breathing. Pediatrics. 1984;74:58–62. [PubMed] [Google Scholar]
- Gerstmann DR, Minton SD, Stoddard RA, Meredith KS, Monaco F, Bertrand JM, et al. The Provo multicenter early high-frequency oscillatory ventilation trial: improved pulmonary and clinical outcome in respiratory distress syndrome. Pediatrics. 1996;98(6 Pt 1):1044–1057. [PubMed] [Google Scholar]
- Gibbs DL, Rice HE, Farrell JA, Adzick NS, Harrison MR. Familial diaphragmatic agenesis: an autosomal-recessive syndrome with a poor prognosis. J Pediatr Surg. 1997;32(2):366–368. doi: 10.1016/s0022-3468(97)90212-8. [DOI] [PubMed] [Google Scholar]
- Gibson RL, Nizet V, Rubens CE. Group B streptococcal beta-hemolysin promotes injury of lung microvascular endothelial cells. Pediatr Res. 1999;45:626–634. doi: 10.1203/00006450-199905010-00003. [DOI] [PubMed] [Google Scholar]
- Gluck L, Kulovich MV, Eidelman AI, Cordero L, Khazin AF. Biochemical development of surface activity in mammalian lung. IV. Pulmonary lecithin synthesis in the human fetus and newborn and etiology of the respiratory distress syndrome. Pediatr Res. 1972;6(2):81–99. doi: 10.1203/00006450-197202000-00002. [DOI] [PubMed] [Google Scholar]
- Goldsmith JP. Continuous positive airway pressure and conventional mechanical ventilation in the treatment of meconium aspiration syndrome. J Perinatol. 2008;28(Suppl 3):S49–S55. doi: 10.1038/jp.2008.156. [DOI] [PubMed] [Google Scholar]
- Goldsmith LS, Greenspan JS, Rubenstein SD, Wolfson MR, Shaffer TH. Immediate improvement in lung volume after exogenous surfactant: alveolar recruitment versus increased distention. J Pediatr. 1991;119(3):424–428. doi: 10.1016/s0022-3476(05)82057-8. [DOI] [PubMed] [Google Scholar]
- Goldstein RF, Brazy JE. Fluctuations of arterial blood pressure decrease with mechanical ventilation in premature infants with respiratory distress syndrome. J Perinatol. 1990;10:267–271. [PubMed] [Google Scholar]
- Gomez R, Ghezzi F, Romero R, Munoz H, Tolosa JE, Rojas I. Premature labor and intra-amniotic infection. Clinical aspects and role of the cytokines in diagnosis and pathophysiology. Clin Perinatol. 1995;22(2):281–342. [PubMed] [Google Scholar]
- Gooding CA, Gregory GA, Taber P, Wright RR. An experimental model for the study of meconium aspiration of the newborn. Radiology. 1971;100:137–140. doi: 10.1148/100.1.137. [DOI] [PubMed] [Google Scholar]
- Gounaris A, Costalos C, Varchalama L, Kokori P, Kolovou E, Alexiou N. Gastric emptying in very-low-birth-weight infants treated with nasal continuous positive airway pressure. J Pediatr. 2004;145(4):508–510. doi: 10.1016/j.jpeds.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Gouyon JB, Ribakovsky C, Ferdynus C, Quantin C, Sagot P, Gouyon B. Severe respiratory disorders in term neonates. Paediatr Perinat Epidemiol. 2008;22:22–30. doi: 10.1111/j.1365-3016.2007.00875.x. [DOI] [PubMed] [Google Scholar]
- Graham PL, 3rd, Begg MD, Larson E, Della-Latta P, Allen A, Saiman L. Risk factors for late onset gram-negative sepsis in low birth weight infants hospitalized in the neonatal intensive care unit. Pediatr Infect Dis J. 2006;25(2):113–117. doi: 10.1097/01.inf.0000199310.52875.10. [DOI] [PubMed] [Google Scholar]
- Greenough A, Sharma A. Optimal strategies for newborn ventilation – a synthesis of the evidence. Early Hum Dev. 2005;81(12):957–964. doi: 10.1016/j.earlhumdev.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Greenough A, Morley C, Davis J. Interaction of spontaneous respiration with artificial ventilation in preterm babies. J Pediatr. 1983;103(5):769–773. doi: 10.1016/s0022-3476(83)80483-1. [DOI] [PubMed] [Google Scholar]
- Greenough A, Greenall F, Gamsu H. Synchronous respiration: which ventilator rate is best? Acta Paediatr Scand. 1987;76(5):713–718. doi: 10.1111/j.1651-2227.1987.tb10554.x. [DOI] [PubMed] [Google Scholar]
- Greenough A, Dimitriou G, Prendergast M, Milner AD (2008) Synchronized mechanical ventilation for respiratory support in newborn infants. Cochrane Database Syst Rev (1):CD000456 [DOI] [PubMed]
- Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971;284(24):1333–1340. doi: 10.1056/NEJM197106172842401. [DOI] [PubMed] [Google Scholar]
- Greisen G, Munck H, Lou H. Severe hypocarbia in preterm infants and neurodevelopmental deficit. Acta Paediatr Scand. 1987;76(3):401–404. doi: 10.1111/j.1651-2227.1987.tb10489.x. [DOI] [PubMed] [Google Scholar]
- Gross RE. Congenital hernia of the diaphragm. Am J Dis Child. 1946;71(6):579–592. doi: 10.1001/archpedi.1946.02020290002001. [DOI] [PubMed] [Google Scholar]
- Gross I, Smith GJ, Wilson CM, Maniscalco WM, Ingleson LD, Brehier A, et al. The influence of hormones on the biochemical development of fetal rat lung in organ culture. II. Insulin. Pediatr Res. 1980;14(6):834–838. doi: 10.1203/00006450-198006000-00012. [DOI] [PubMed] [Google Scholar]
- Guner YS, Chokshi N, Aranda A, Ochoa C, Qureshi FG, Nguyen NX, et al. Thoracoscopic repair of neonatal diaphragmatic hernia. J Laparoendosc Adv Surg Tech A. 2008;18(6):875–880. doi: 10.1089/lap.2007.0239. [DOI] [PubMed] [Google Scholar]
- Gupta A, Rastogi S, Sahni R, et al. Inhaled nitric oxide and gentle ventilation in the treatment of pulmonary hypertension of the newborn – a single-center, 5-year experience. J Perinatol. 2002;22:435–441. doi: 10.1038/sj.jp.7210761. [DOI] [PubMed] [Google Scholar]
- Gupta S, Sinha SK, Tin W, Donn SM. A randomized controlled trial of post-extubation bubble continuous positive airway pressure versus Infant Flow Driver continuous positive airway pressure in preterm infants with respiratory distress syndrome. J Pediatr. 2009;154(5):645–650. doi: 10.1016/j.jpeds.2008.12.034. [DOI] [PubMed] [Google Scholar]
- Guthrie SO, Walsh WF, Auten K, Clark RH. Initial dosing of inhaled nitric oxide in infants with hypoxic respiratory failure. J Perinatol. 2004;24:290–294. doi: 10.1038/sj.jp.7211087. [DOI] [PubMed] [Google Scholar]
- Hachey WE, Eyal FG, Curtet-Eyal NL, Kellum FE. High-frequency oscillatory ventilation versus conventional ventilation in a piglet model of early meconium aspiration. Crit Care Med. 1998;26:556–561. doi: 10.1097/00003246-199803000-00031. [DOI] [PubMed] [Google Scholar]
- Hajer GF, vd Staak FH, de Haan AF, Festen C. Recurrent congenital diaphragmatic hernia; which factors are involved? Eur J Pediatr Surg. 1998;8(6):329–333. doi: 10.1055/s-2008-1071226. [DOI] [PubMed] [Google Scholar]
- Hall GL, Hantos Z, Wildhaber JH, Sly PD. Contribution of nasal pathways to low frequency respiratory impedance in infants. Thorax. 2002;57(5):396–399. doi: 10.1136/thorax.57.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliday HL. History of surfactant from 1980. Biol Neonate. 2005;87(4):317–322. doi: 10.1159/000084879. [DOI] [PubMed] [Google Scholar]
- Halliday HL. Recent clinical trials of surfactant treatment for neonates. Biol Neonate. 2006;89(4):323–329. doi: 10.1159/000092869. [DOI] [PubMed] [Google Scholar]
- Halliday HL, McClure G, Reid MM, Lappin TR, Meban C, Thomas PS. Controlled trial of artificial surfactant to prevent respiratory distress syndrome. Lancet. 1984;1:476–478. doi: 10.1016/s0140-6736(84)92849-6. [DOI] [PubMed] [Google Scholar]
- Halliday HL, Tarnow-Mordi WO, Corcoran JD, Patterson CC. Multicentre randomised trial comparing high and low dose surfactant regimens for the treatment of respiratory distress syndrome (the Curosurf 4 trial) Arch Dis Child. 1993;69(3 Spec No):276–280. doi: 10.1136/adc.69.3_spec_no.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliday HL, Speer CP, Robertson B. Treatment of severe meconium aspiration syndrome with porcine surfactant. Collaborative Surfactant Study Group. Eur J Pediatr. 1996;155:1047–1051. doi: 10.1007/BF02532529. [DOI] [PubMed] [Google Scholar]
- Hamilton PP, Onayemi A, Smyth JA, Gillan JE, Cutz E, Froese AB, et al. Comparison of conventional and high-frequency ventilation: oxygenation and lung pathology. J Appl Physiol. 1983;55(1 Pt 1):131–138. doi: 10.1152/jappl.1983.55.1.131. [DOI] [PubMed] [Google Scholar]
- Han VK, Beverley DW, Clarson C, Sumabat WO, Shaheed WA, Brabyn DG, et al. Randomized controlled trial of very early continuous distending pressure in the management of preterm infants. Early Hum Dev. 1987;15(1):21–32. doi: 10.1016/0378-3782(87)90097-1. [DOI] [PubMed] [Google Scholar]
- Hand IL, Noble L, Geiss D. The effects of positioning on the Hering-Breuer reflex in the preterm infant. Pediatr Pulmonol. 2007;42(1):37–40. doi: 10.1002/ppul.20531. [DOI] [PubMed] [Google Scholar]
- Hannam S, Ingram DM, Milner AD. A possible role for the Hering-Breuer deflation reflex in apnea of prematurity. J Pediatr. 1998;132:35–39. doi: 10.1016/s0022-3476(98)70481-0. [DOI] [PubMed] [Google Scholar]
- Harbarth S, Sudre P, Dharan S, Cadenas M, Pittet D. Outbreak of Enterobacter cloacae related to understaffing, overcrowding, and poor hygiene practices. Infect Control Hosp Epidemiol. 1999;20:598–603. doi: 10.1086/501677. [DOI] [PubMed] [Google Scholar]
- Hardart GE, Fackler JC. Predictors of intracranial hemorrhage during neonatal extracorporeal membrane oxygenation. J Pediatr. 1999;134(2):156–159. doi: 10.1016/s0022-3476(99)70408-7. [DOI] [PubMed] [Google Scholar]
- Harding R. Development of the respiratory system. In: Thorburn GD, Harding R, editors. Textbook of fetal physiology. Oxford: Oxford Medical Publications; 1994. pp. 140–167. [Google Scholar]
- Harris H, Wilson S, Brans Y, Wirtschafter D, Cassady G. Nasal continuous positive airway pressure. Improvement in arterial oxygenation in hyaline membrane disease. Biol Neonate. 1976;29(3–4):231–237. doi: 10.1159/000240868. [DOI] [PubMed] [Google Scholar]
- Harrison VC, Heese Hde V, Klein M. The significance of grunting in hyaline membrane disease. Pediatrics. 1968;41(3):549–559. [PubMed] [Google Scholar]
- Hascoet JM, Espagne S, Hamon I. CPAP and the preterm infant: lessons from the COIN trial and other studies. Early Hum Dev. 2008;84(12):791–793. doi: 10.1016/j.earlhumdev.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Heimler R, Hoffmann RG, Starshak RJ, Sasidharan P, Grausz JP. Chronic lung disease in premature infants: a retrospective evaluation of underlying factors. Crit Care Med. 1988;16(12):1213–1217. doi: 10.1097/00003246-198812000-00007. [DOI] [PubMed] [Google Scholar]
- Heiss K, Manning P, Oldham KT, Coran AG, Polley TZ, Jr, Wesley JR, et al. Reversal of mortality for congenital diaphragmatic hernia with ECMO. Ann Surg. 1989;209(2):225–230. doi: 10.1097/00000658-198902000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiss KF, Clark RH, Cornish JD, Stovroff M, Ricketts R, Kesser K, et al. Preferential use of venovenous extracorporeal membrane oxygenation for congenital diaphragmatic hernia. J Pediatr Surg. 1995;30(3):416–419. doi: 10.1016/0022-3468(95)90045-4. [DOI] [PubMed] [Google Scholar]
- Hellstrom-Westas L, Bell AH, Skov L, Greisen G, Svenningsen NW. Cerebroelectrical depression following surfactant treatment in preterm neonates. Pediatrics. 1992;89(4 Pt 1):643–647. [PubMed] [Google Scholar]
- Henderson-Smart D. The effect of gestational age on the incidence and duration of recurrent apnoea in newborn babies. Aust J Paediatr. 1981;17:273–276. doi: 10.1111/j.1440-1754.1981.tb01957.x. [DOI] [PubMed] [Google Scholar]
- Henderson-Smart DJ, Wilkinson A, Raynes-Greenow CH (2002) Mechanical ventilation for newborn infants with respiratory failure due to pulmonary disease. Cochrane Database Syst Rev (4):CD002770 [DOI] [PMC free article] [PubMed]
- Henderson-Smart DJ, Cools F, Bhuta T, Offringa M (2007) Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev (3):CD000104 [DOI] [PubMed]
- Henderson-Smart DJ, De Paoli AG, Clark RH, Bhuta T (2009) High frequency oscillatory ventilation versus conventional ventilation for infants with severe pulmonary dysfunction born at or near term. Cochrane Database Syst Rev (3):CD002974 [DOI] [PMC free article] [PubMed]
- Hendricks-Munoz KD, Walton JP. Hearing loss in infants with persistent fetal circulation. Pediatrics. 1988;81:650–656. [PubMed] [Google Scholar]
- Hernandez LA, Peevy KJ, Moise AA, Parker JC. Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. J Appl Physiol. 1989;66(5):2364–2368. doi: 10.1152/jappl.1989.66.5.2364. [DOI] [PubMed] [Google Scholar]
- Hernandez C, Little BB, Dax JS, Gilstrap LC, Rosenfeld CR. Prediction of the severity of meconium aspiration syndrome. Am J Obstet Gynecol. 1993;169:61–70. doi: 10.1016/0002-9378(93)90132-3. [DOI] [PubMed] [Google Scholar]
- Herting E, Sun B, Jarstrand C, Curstedt T, Robertson B. Surfactant improves lung function and mitigates bacterial growth in immature ventilated rabbits with experimentally induced neonatal group B streptococcal pneumonia. Arch Dis Child Fetal Neonatal Ed. 1997;76:F3–F8. doi: 10.1136/fn.76.1.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herting E, Rauprich P, Stichtenoth G, Walter G, Johansson J, Robertson B. Resistance of different surfactant preparations to inactivation by meconium. Pediatr Res. 2001;50:44–49. doi: 10.1203/00006450-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Hey Ee . Neonatal formulary. 4. London: BMJ Books; 2003. [Google Scholar]
- Higgins RD, Richter SE, Davis JM. Nasal continuous positive airway pressure facilitates extubation of very low birth weight neonates. Pediatrics. 1991;88(5):999–1003. [PubMed] [Google Scholar]
- Higgins ST, Wu AM, Sen N, Spitzer AR, Chander A. Meconium increases surfactant secretion in isolated rat alveolar type II cells. Pediatr Res. 1996;39:443–447. doi: 10.1203/00006450-199603000-00011. [DOI] [PubMed] [Google Scholar]
- High-frequency oscillatory ventilation compared with conventional mechanical ventilation in the treatment of respiratory failure in preterm infants. The HIFI Study Group (1989) N Engl J Med 320(2):88–93 [DOI] [PubMed]
- Hill HR. Biochemical, structural, and functional abnormalities of polymorphonuclear leukocytes in the neonate. Pediatr Res. 1987;22:375–382. doi: 10.1203/00006450-198710000-00001. [DOI] [PubMed] [Google Scholar]
- Hintz SR, Suttner DM, Sheehan AM, Rhine WD, Van Meurs KP. Decreased use of neonatal extracorporeal membrane oxygenation (ECMO): how new treatment modalities have affected ECMO utilization. Pediatrics. 2000;106(6):1339–1343. doi: 10.1542/peds.106.6.1339. [DOI] [PubMed] [Google Scholar]
- Hintz SR, Poole WK, Wright LL, Fanaroff AA, Kendrick DE, Laptook AR, et al. Changes in mortality and morbidities among infants born at less than 25 weeks during the post-surfactant era. Arch Dis Child Fetal Neonatal Ed. 2005;90(2):F128–F133. doi: 10.1136/adc.2003.046268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschl RB, Schumacher RE, Snedecor SN, Bui KC, Bartlett RH. The efficacy of extracorporeal life support in premature and low birth weight newborns. J Pediatr Surg. 1993;28(10):1336–1340. doi: 10.1016/s0022-3468(05)80324-0. [DOI] [PubMed] [Google Scholar]
- Hislop AA, Wigglesworth JS, Desai R. Alveolar development in the human fetus and infant. Early Hum Dev. 1986;13(1):1–11. doi: 10.1016/0378-3782(86)90092-7. [DOI] [PubMed] [Google Scholar]
- Hjalmarson O. Epidemiology and classification of acute, neonatal respiratory disorders. A prospective study. Acta Paediatr Scand. 1981;70(6):773–783. doi: 10.1111/j.1651-2227.1981.tb06228.x. [DOI] [PubMed] [Google Scholar]
- Hjalmarson O, Olsson T., IV Work of breathing. Acta Paediatr Scand Suppl. 1974;247:49–60. [PubMed] [Google Scholar]
- Ho JJ, Subramaniam P, Henderson-Smart DJ, Davis PG (2002) Continuous distending pressure for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev (2):CD002271 [DOI] [PubMed]
- Holcberg G, Huleihel M, Katz M, et al. Vasoconstrictive activity of meconium stained amniotic fluid in the human placental vasculature. Eur J Obstet Gynecol Reprod Biol. 1999;87:147–150. doi: 10.1016/s0301-2115(99)00099-8. [DOI] [PubMed] [Google Scholar]
- Holleman-Duray D, Kaupie D, Weiss MG. Heated humidified high-flow nasal cannula: use and a neonatal early extubation protocol. J Perinatol. 2007;27(12):776–781. doi: 10.1038/sj.jp.7211825. [DOI] [PubMed] [Google Scholar]
- Holm BA, Notter RH. Effects of hemoglobin and cell membrane lipids on pulmonary surfactant activity. J Appl Physiol. 1987;63:1434–1442. doi: 10.1152/jappl.1987.63.4.1434. [DOI] [PubMed] [Google Scholar]
- Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M, et al. Trends in mortality and morbidity for very low birth weight infants, 1991–1999. Pediatrics. 2002;110(1 Pt 1):143–151. doi: 10.1542/peds.110.1.143. [DOI] [PubMed] [Google Scholar]
- Huckstadt T, Foitzik B, Wauer RR, Schmalisch G. Comparison of two different CPAP systems by tidal breathing parameters. Intensive Care Med. 2003;29(7):1134–1140. doi: 10.1007/s00134-003-1785-0. [DOI] [PubMed] [Google Scholar]
- Hulsey TC, Alexander GR, Robillard PY, Annibale DJ, Keenan A. Hyaline membrane disease: the role of ethnicity and maternal risk characteristics. Am J Obstet Gynecol. 1993;168(2):572–576. doi: 10.1016/0002-9378(93)90496-6. [DOI] [PubMed] [Google Scholar]
- Hummler H, Schulze A. New and alternative modes of mechanical ventilation in neonates. Semin Fetal Neonatal Med. 2009;14(1):42–48. doi: 10.1016/j.siny.2008.08.006. [DOI] [PubMed] [Google Scholar]
- Hunt RW, Kean MJ, Stewart MJ, Inder TE. Patterns of cerebral injury in a series of infants with congenital diaphragmatic hernia utilizing magnetic resonance imaging. J Pediatr Surg. 2004;39(1):31–36. doi: 10.1016/j.jpedsurg.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Hutchison AA (2007) Essentials of airway physiology. In: 5th world congress on Pediatric Critical Care, World Federation of Pediatric Intensive Critical Care Societies, Geneva, June 24–28; follow Research and Education at www.wfpiccs.org
- Hutchison AA, Bignall S. Non-invasive positive pressure ventilation in the preterm neonate: reducing endotrauma and the incidence of bronchopulmonary dysplasia. Arch Dis Child Fetal Neonatal Ed. 2008;93:F64–F68. doi: 10.1136/adc.2006.103770. [DOI] [PubMed] [Google Scholar]
- Hutchison AA, Speck DF. Laryngeal and diaphragmatic muscle activities after central nervous system lesions in cats. Acta Paediatr. 2003;92:1297–1307. [PubMed] [Google Scholar]
- Hutchison AA, Burchfield DJ, Wozniak JA, Mohrman SJ. Laryngeal muscle activities with cerebral hypoxia-ischemia in newborn lambs. Am J Respir Crit Care Med. 2002;166:85–91. doi: 10.1164/rccm.2101024. [DOI] [PubMed] [Google Scholar]
- Huxtable KA, Tucker AS, Wedgwood RJ. Staphylococcal pneumonia in childhood; long-term follow-up. Am J Dis Child. 1964;108:262–269. doi: 10.1001/archpedi.1964.02090010264007. [DOI] [PubMed] [Google Scholar]
- Idiong N, Lemke RP, Lin YJ, Kwiatkowski K, Cates DB, Rigatto H. Airway closure during mixed apneas in preterm infants: is respiratory effort necessary? J Pediatr. 1998;133:509–512. doi: 10.1016/s0022-3476(98)70058-7. [DOI] [PubMed] [Google Scholar]
- Ijsselstijn H, Tibboel D, Hop WJ, Molenaar JC, de Jongste JC. Long-term pulmonary sequelae in children with congenital diaphragmatic hernia. Am J Respir Crit Care Med. 1997;155(1):174–180. doi: 10.1164/ajrccm.155.1.9001308. [DOI] [PubMed] [Google Scholar]
- Ikegami M, Jacobs H, Jobe A. Surfactant function in respiratory distress syndrome. J Pediatr. 1983;102(3):443–447. doi: 10.1016/s0022-3476(83)80673-8. [DOI] [PubMed] [Google Scholar]
- Ikegami M, Jobe AH, Yamada T, Seidner S. Relationship between alveolar saturated phosphatidylcholine pool sizes and compliance of preterm rabbit lungs. The effect of maternal corticosteroid treatment. Am Rev Respir Dis. 1989;139(2):367–369. doi: 10.1164/ajrccm/139.2.367. [DOI] [PubMed] [Google Scholar]
- Ikegami M, Jobe AH, Tabor BL, Rider ED, Lewis JF. Lung albumin recovery in surfactant-treated preterm ventilated lambs. Am Rev Respir Dis. 1992;145(5):1005–1008. doi: 10.1164/ajrccm/145.5.1005. [DOI] [PubMed] [Google Scholar]
- Inamura N, Kubota A, Nakajima T, Kayatani F, Okuyama H, Oue T, et al. A proposal of new therapeutic strategy for antenatally diagnosed congenital diaphragmatic hernia. J Pediatr Surg. 2005;40(8):1315–1319. doi: 10.1016/j.jpedsurg.2005.05.018. [DOI] [PubMed] [Google Scholar]
- Inhaled nitric oxide and hypoxic respiratory failure in infants with congenital diaphragmatic hernia. The Neonatal Inhaled Nitric Oxide Study Group (NINOS) (1997) Pediatrics 99(6):838–845 [DOI] [PubMed]
- Iocono JA, Cilley RE, Mauger DT, Krummel TM, Dillon PW. Postnatal pulmonary hypertension after repair of congenital diaphragmatic hernia: predicting risk and outcome. J Pediatr Surg. 1999;34(2):349–353. doi: 10.1016/s0022-3468(99)90207-5. [DOI] [PubMed] [Google Scholar]
- Ioffe S, Chernick V. Maternal alcohol ingestion and the incidence of respiratory distress syndrome. Am J Obstet Gynecol. 1987;156(5):1231–1235. doi: 10.1016/0002-9378(87)90152-9. [DOI] [PubMed] [Google Scholar]
- Jackson JC, Palmer S, Truog WE, Standaert TA, Murphy JH, Hodson WA. Surfactant quantity and composition during recovery from hyaline membrane disease. Pediatr Res. 1986;20(12):1243–1247. doi: 10.1203/00006450-198612000-00011. [DOI] [PubMed] [Google Scholar]
- Jackson JK, Vellucci J, Johnson P, Kilbride HW. Evidence-based approach to change in clinical practice: introduction of expanded nasal continuous positive airway pressure use in an intensive care nursery. Pediatrics. 2003;111(4 Pt 2):e542–e547. [PubMed] [Google Scholar]
- Jacobsen T, Gronvall J, Petersen S, Andersen GE. “Minitouch” treatment of very low-birth-weight infants. Acta Paediatr. 1993;82(11):934–938. doi: 10.1111/j.1651-2227.1993.tb12603.x. [DOI] [PubMed] [Google Scholar]
- Jaillard SM, Pierrat V, Dubois A, Truffert P, Lequien P, Wurtz AJ, et al. Outcome at 2 years of infants with congenital diaphragmatic hernia: a population-based study. Ann Thorac Surg. 2003;75(1):250–256. doi: 10.1016/s0003-4975(02)04278-9. [DOI] [PubMed] [Google Scholar]
- Jakobson LS, Frisk V, Trachsel D, O’Brien K. Visual and fine-motor outcomes in adolescent survivors of high-risk congenital diaphragmatic hernia who did not receive extracorporeal membrane oxygenation. J Perinatol. 2009;29(9):630–636. doi: 10.1038/jp.2009.61. [DOI] [PubMed] [Google Scholar]
- Jasin LR, Kern S, Thompson S, Walter C, Rone JM, Yohannan MD. Subcutaneous scalp emphysema, pneumo-orbitis and pneumocephalus in a neonate on high humidity high flow nasal cannula. J Perinatol. 2008;28(11):779–781. doi: 10.1038/jp.2008.99. [DOI] [PubMed] [Google Scholar]
- Jasnosz KM, Hermansen MC, Snider C, Sang K. Congenital complete absence (bilateral agenesis) of the diaphragm: a rare variant of congenital diaphragmatic hernia. Am J Perinatol. 1994;11(5):340–343. doi: 10.1055/s-2007-994549. [DOI] [PubMed] [Google Scholar]
- Javid PJ, Jaksic T, Skarsgard ED, Lee S. Survival rate in congenital diaphragmatic hernia: the experience of the Canadian Neonatal Network. J Pediatr Surg. 2004;39(5):657–660. doi: 10.1016/j.jpedsurg.2004.01.022. [DOI] [PubMed] [Google Scholar]
- Jefferies AL, Coates G, O’Brodovich H. Pulmonary epithelial permeability in hyaline-membrane disease. N Engl J Med. 1984;311(17):1075–1080. doi: 10.1056/NEJM198410253111703. [DOI] [PubMed] [Google Scholar]
- Jobe AH. Commentary on surfactant treatment of neonates with respiratory failure and group B streptococcal infection. Pediatrics. 2000;106:1135. doi: 10.1542/peds.106.5.1135. [DOI] [PubMed] [Google Scholar]
- Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163(7):1723–1729. doi: 10.1164/ajrccm.163.7.2011060. [DOI] [PubMed] [Google Scholar]
- Jobe AH, Kramer BW, Moss TJ, Newnham JP, Ikegami M. Decreased indicators of lung injury with continuous positive expiratory pressure in preterm lambs. Pediatr Res. 2002;52(3):387–392. doi: 10.1203/00006450-200209000-00014. [DOI] [PubMed] [Google Scholar]
- Johnson P. Comparative aspects of the control of breathing during development. In: von Euler C, Lagercrantz H, editors. Central nervous control mechanisms in breathing. Oxford: Permagon Press; 1979. pp. 337–352. [Google Scholar]
- Jones CA, Cayabyab RG, Kwong KY, et al. Undetectable interleukin (IL)-10 and persistent IL-8 expression early in hyaline membrane disease: a possible developmental basis for the predisposition to chronic lung inflammation in preterm newborns. Pediatr Res. 1996;39:966–975. doi: 10.1203/00006450-199606000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorch G, Hartl H, Roth B, Kribs A, Gortner L, Schaible T, et al. Surfactant aerosol treatment of respiratory distress syndrome in spontaneously breathing premature infants. Pediatr Pulmonol. 1997;24(3):222–224. doi: 10.1002/(sici)1099-0496(199709)24:3<222::aid-ppul9>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Jounieaux V, Aubert G, Dury M, Delguste P, Rodenstein D. Effects of nasal positive-pressure hyperventilation on the glottis in normal awake subjects. J Appl Physiol. 1995;79:176–185. doi: 10.1152/jappl.1995.79.1.176. [DOI] [PubMed] [Google Scholar]
- Kahn DJ, Courtney SE, Steele AM, Habib RH. Unpredictability of delivered bubble nasal continuous positive airway pressure: role of bias flow magnitude and nares-prong air leaks. Pediatr Res. 2007;62(3):343–347. doi: 10.1203/PDR.0b013e318123f702. [DOI] [PubMed] [Google Scholar]
- Kamata S, Usui N, Ishikawa S, Okuyama H, Kitayama Y, Sawai T, et al. Prolonged preoperative stabilization using high-frequency oscillatory ventilation does not improve the outcome in neonates with congenital diaphragmatic hernia. Pediatr Surg Int. 1998;13(8):542–546. doi: 10.1007/s003830050398. [DOI] [PubMed] [Google Scholar]
- Kamper J, Wulff K, Larsen C, Lindequist S. Early treatment with nasal continuous positive airway pressure in very low-birth-weight infants. Acta Paediatr. 1993;82(2):193–197. doi: 10.1111/j.1651-2227.1993.tb12637.x. [DOI] [PubMed] [Google Scholar]
- Kanto WP, Jr, Borer RC, Jr, Barr M, Jr, Roloff DW. Tracheal aspirate lecithin/sphingomyelin ratios as predictors of recovery from respiratory distress syndrome. J Pediatr. 1976;89(4):612–616. doi: 10.1016/s0022-3476(76)80402-7. [DOI] [PubMed] [Google Scholar]
- Kanto WP, Jr, Kuhns LP, Borer RC, Jr, Roloff DW. Failure of serial chest radiographs to predict recovery from respiratory distress syndrome. Am J Obstet Gynecol. 1978;131(7):757–760. doi: 10.1016/0002-9378(78)90241-7. [DOI] [PubMed] [Google Scholar]
- Kassim Z, Greenough A. Patient-triggered ventilation. Minerva Pediatr. 2006;58(4):327–332. [PubMed] [Google Scholar]
- Kattwinkel J, Nearman HS, Fanaroff AA, Katona PG, Klaus MH. Apnea of prematurity. Comparative therapeutic effects of cutaneous stimulation and nasal continuous positive airway pressure. J Pediatr. 1975;86(4):588–592. doi: 10.1016/s0022-3476(75)80158-2. [DOI] [PubMed] [Google Scholar]
- Kattwinkel J, Robinson M, Bloom BT, Delmore P, Ferguson JE. Technique for intrapartum administration of surfactant without requirement for an endotracheal tube. J Perinatol. 2004;24(6):360–365. doi: 10.1038/sj.jp.7211103. [DOI] [PubMed] [Google Scholar]
- Kavvadia V, Greenough A, Dimitriou G, Hooper R. Influence of ethnic origin on respiratory distress syndrome in very premature infants. Arch Dis Child Fetal Neonatal Ed. 1998;78(1):F25–F28. doi: 10.1136/fn.78.1.f25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kays DW, Langham MR, Jr, Ledbetter DJ, Talbert JL. Detrimental effects of standard medical therapy in congenital diaphragmatic hernia. Ann Surg. 1999;230(3):340–348. doi: 10.1097/00000658-199909000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller RL, Hamrick SE, Kitterman JA, Fineman JR, Hawgood S. Treatment of rebound and chronic pulmonary hypertension with oral sildenafil in an infant with congenital diaphragmatic hernia. Pediatr Crit Care Med. 2004;5(2):184–187. doi: 10.1097/01.pcc.0000113266.26638.ad. [DOI] [PubMed] [Google Scholar]
- Kendig JW, Ryan RM, Sinkin RA, Maniscalco WM, Notter RH, Guillet R, et al. Comparison of two strategies for surfactant prophylaxis in very premature infants: a multicenter randomized trial. Pediatrics. 1998;101(6):1006–1012. doi: 10.1542/peds.101.6.1006. [DOI] [PubMed] [Google Scholar]
- Keszler M. Volume-targeted ventilation. J Perinatol. 2005;25(Suppl 2):S19–S22. doi: 10.1038/sj.jp.7211313. [DOI] [PubMed] [Google Scholar]
- Keszler M, Molina B, Butterfield AB, Subramanian KN. Combined high-frequency jet ventilation in a meconium aspiration model. Crit Care Med. 1986;14:34–38. doi: 10.1097/00003246-198601000-00009. [DOI] [PubMed] [Google Scholar]
- Keszler M, Modanlou HD, Brudno DS, Clark FI, Cohen RS, Ryan RM, et al. Multicenter controlled clinical trial of high-frequency jet ventilation in preterm infants with uncomplicated respiratory distress syndrome. Pediatrics. 1997;100(4):593–599. doi: 10.1542/peds.100.4.593. [DOI] [PubMed] [Google Scholar]
- Khalaf MN, Brodsky N, Hurley J, Bhandari V. A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics. 2001;108(1):13–17. doi: 10.1542/peds.108.1.13. [DOI] [PubMed] [Google Scholar]
- Khammash H, Perlman M, Wojtulewicz J, Dunn M. Surfactant therapy in full-term neonates with severe respiratory failure [see comments] Pediatrics. 1993;92:135–139. [PubMed] [Google Scholar]
- Khan A, Qurashi M, Kwiatkowski K, Cates D, Rigatto H. Measurement of the CO2 apneic threshold in newborn infants: possible relevance for periodic breathing and apnea. J Appl Physiol. 2005;98:1171–1176. doi: 10.1152/japplphysiol.00574.2003. [DOI] [PubMed] [Google Scholar]
- Khorana M, Paradeevisut H, Sangtawesin V, Kanjanapatanakul W, Chotigeat U, Ayutthaya JK. A randomized trial of non-synchronized Nasopharyngeal Intermittent Mandatory Ventilation (nsNIMV) vs. Nasal Continuous Positive Airway Pressure (NCPAP) in the prevention of extubation failure in pre-term < 1,500 grams. J Med Assoc Thai. 2008;91(Suppl 3):S136–S142. [PubMed] [Google Scholar]
- Kiciman NM, Andreasson B, Bernstein G, Mannino FL, Rich W, Henderson C, et al. Thoracoabdominal motion in newborns during ventilation delivered by endotracheal tube or nasal prongs. Pediatr Pulmonol. 1998;25(3):175–181. doi: 10.1002/(sici)1099-0496(199803)25:3<175::aid-ppul7>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Kim EH. Successful extubation of newborn infants without preextubation trial of continuous positive airway pressure. J Perinatol. 1989;9(1):72–76. [PubMed] [Google Scholar]
- Kinsella JP, Abman SH. Inhaled nitric oxide and high frequency oscillatory ventilation in persistent pulmonary hypertension of the newborn. Eur J Pediatr. 1998;157(Suppl 1):S28–S30. doi: 10.1007/pl00014288. [DOI] [PubMed] [Google Scholar]
- Kinsella JP, Truog WE, Walsh WF, et al. Randomized, multicenter trial of inhaled nitric oxide and high-frequency oscillatory ventilation in severe, persistent pulmonary hypertension of the newborn. J Pediatr. 1997;131:55–62. doi: 10.1016/s0022-3476(97)70124-0. [DOI] [PubMed] [Google Scholar]
- Kinsella JP, Ivy DD, Abman SH. Pulmonary vasodilator therapy in congenital diaphragmatic hernia: acute, late, and chronic pulmonary hypertension. Semin Perinatol. 2005;29(2):123–128. doi: 10.1053/j.semperi.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Kirpalani H (2007) NIPPV in premature infants: Hamilton Health Sciences Canadian Institutes of Health Research (CIHR). http://clinicaltrials.gov/ct2/show/NCT00433212
- Koivusalo AI, Pakarinen MP, Lindahl HG, Rintala RJ. The cumulative incidence of significant gastroesophageal reflux in patients with congenital diaphragmatic hernia-a systematic clinical, pH-metric, and endoscopic follow-up study. J Pediatr Surg. 2008;43(2):279–282. doi: 10.1016/j.jpedsurg.2007.10.014. [DOI] [PubMed] [Google Scholar]
- Konishi M, Fujiwara T, Naito T, Takeuchi Y, Ogawa Y, Inukai K, et al. Surfactant replacement therapy in neonatal respiratory distress syndrome. A multi-centre, randomized clinical trial: comparison of high- versus low-dose of surfactant TA. Eur J Pediatr. 1988;147(1):20–25. doi: 10.1007/BF00442605. [DOI] [PubMed] [Google Scholar]
- Kopelman AE, Holbert D. Use of oxygen cannulas in extremely low birthweight infants is associated with mucosal trauma and bleeding, and possibly with coagulase-negative staphylococcal sepsis. J Perinatol. 2003;23(2):94–97. doi: 10.1038/sj.jp.7210865. [DOI] [PubMed] [Google Scholar]
- Kribs A, Vierzig A, Hunseler C, Eifinger F, Welzing L, Stutzer H, et al. Early surfactant in spontaneously breathing with nCPAP in ELBW infants – a single centre four year experience. Acta Paediatr. 2008;97(3):293–298. doi: 10.1111/j.1651-2227.2007.00617.x. [DOI] [PubMed] [Google Scholar]
- Kubicka ZJ, Limauro J, Darnall RA. Heated, humidified high-flow nasal cannula therapy: yet another way to deliver continuous positive airway pressure? Pediatrics. 2008;121(1):82–88. doi: 10.1542/peds.2007-0957. [DOI] [PubMed] [Google Scholar]
- Kugelman A, Saiki K, Platzker AC, Garg M. Measurement of lung volumes and pulmonary mechanics during weaning of newborn infants with intractable respiratory failure from extracorporeal membrane oxygenation. Pediatr Pulmonol. 1995;20:145–151. doi: 10.1002/ppul.1950200304. [DOI] [PubMed] [Google Scholar]
- Kugelman A, Gangitano E, Pincros J, Tantivit P, Taschuk R, Durand M. Venovenous versus venoarterial extracorporeal membrane oxygenation in congenital diaphragmatic hernia. J Pediatr Surg. 2003;38(8):1131–1136. doi: 10.1016/s0022-3468(03)00256-2. [DOI] [PubMed] [Google Scholar]
- Kugelman A, Feferkorn I, Riskin A, Chistyakov I, Kaufman B, Bader D. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure for respiratory distress syndrome: a randomized, controlled, prospective study. J Pediatr. 2007;150(5):521–526. doi: 10.1016/j.jpeds.2007.01.032. [DOI] [PubMed] [Google Scholar]
- Kuint J, Reichman B, Neumann L, Shinwell ES. Prognostic value of the immediate response to surfactant. Arch Dis Child Fetal Neonatal Ed. 1994;71(3):F170–F173. doi: 10.1136/fn.71.3.f170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni A, Ehrenkranz RA, Bhandari V. Effect of introduction of synchronized nasal intermittent positive-pressure ventilation in a neonatal intensive care unit on bronchopulmonary dysplasia and growth in preterm infants. Am J Perinatol. 2006;23(4):233–240. doi: 10.1055/s-2006-939536. [DOI] [PubMed] [Google Scholar]
- Kuna ST, McCarthy MP, Smickley JS. Laryngeal response to passively induced hypocapnia during NREM sleep in normal adult humans. J Appl Physiol. 1993;75:1088–1096. doi: 10.1152/jappl.1993.75.3.1088. [DOI] [PubMed] [Google Scholar]
- Kunisaki SM, Barnewolt CE, Estroff JA, Myers LB, Fauza DO, Wilkins-Haug LE, et al. Ex utero intrapartum treatment with extracorporeal membrane oxygenation for severe congenital diaphragmatic hernia. J Pediatr Surg. 2007;42(1):98–104. doi: 10.1016/j.jpedsurg.2006.09.009. [DOI] [PubMed] [Google Scholar]
- Kyzer S, Sirota L, Chaimoff C. Abdominal wall closure with a silastic patch after repair of congenital diaphragmatic hernia. Arch Surg. 2004;139(3):296–298. doi: 10.1001/archsurg.139.3.296. [DOI] [PubMed] [Google Scholar]
- Lachmann RA, van Kaam AH, Haitsma JJ, Lachmann B. High positive end-expiratory pressure levels promote bacterial translocation in experimental pneumonia. Intensive Care Med. 2007;33:1800–1804. doi: 10.1007/s00134-007-0749-1. [DOI] [PubMed] [Google Scholar]
- Lally KP, Engle W. Postdischarge follow-up of infants with congenital diaphragmatic hernia. Pediatrics. 2008;121(3):627–632. doi: 10.1542/peds.2007-3282. [DOI] [PubMed] [Google Scholar]
- Lally KP, Lally PA, Lasky RE, Tibboel D, Jaksic T, Wilson JM, et al. Defect size determines survival in infants with congenital diaphragmatic hernia. Pediatrics. 2007;120(3):e651–e657. doi: 10.1542/peds.2006-3040. [DOI] [PubMed] [Google Scholar]
- Lamont RF, Dunlop PD, Levene MI, Elder MG. Use of glucocorticoids in pregnancies complicated by severe hypertension and proteinuria. Br J Obstet Gynaecol. 1983;90(3):199–202. doi: 10.1111/j.1471-0528.1983.tb08608.x. [DOI] [PubMed] [Google Scholar]
- Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Observational study of humidified high-flow nasal cannula compared with nasal continuous positive airway pressure. J Pediatr. 2009;154(2):177–182. doi: 10.1016/j.jpeds.2008.07.021. [DOI] [PubMed] [Google Scholar]
- Langham MR, Jr, Kays DW, Ledbetter DJ, Frentzen B, Sanford LL, Richards DS. Congenital diaphragmatic hernia. Epidemiology and outcome. Clin Perinatol. 1996;23(4):671–688. [PubMed] [Google Scholar]
- Lanteri CJ, Willet KE, Kano S, Jobe AH, Ikegami M, Polk DH, et al. Time course of changes in lung mechanics following fetal steroid treatment. Am J Respir Crit Care Med. 1994;150(3):759–765. doi: 10.1164/ajrccm.150.3.8087349. [DOI] [PubMed] [Google Scholar]
- Leach CL, Greenspan JS, Rubenstein SD, Shaffer TH, Wolfson MR, Jackson JC, et al. Partial liquid ventilation with perflubron in premature infants with severe respiratory distress syndrome. The LiquiVent Study Group. N Engl J Med. 1996;335(11):761–767. doi: 10.1056/NEJM199609123351101. [DOI] [PubMed] [Google Scholar]
- Lee KS, Dunn MS, Fenwick M, Shennan AT. A comparison of underwater bubble continuous positive airway pressure with ventilator-derived continuous positive airway pressure in premature neonates ready for extubation. Biol Neonate. 1998;73(2):69–75. doi: 10.1159/000013962. [DOI] [PubMed] [Google Scholar]
- Leipala JA, Bhat RY, Rafferty GF, Hannam S, Greenough A. Effect of posture on respiratory function and drive in preterm infants prior to discharge. Pediatr Pulmonol. 2003;36(4):295–300. doi: 10.1002/ppul.10316. [DOI] [PubMed] [Google Scholar]
- Lemons JA, Bauer CR, Oh W, Korones SB, Papile LA, Stoll BJ, et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics. 2001;107(1):E1. doi: 10.1542/peds.107.1.e1. [DOI] [PubMed] [Google Scholar]
- Leon AE, Michienzi K, Ma CX, Hutchison AA. Serum caffeine concentrations in preterm neonates. Am J Perinatol. 2007;24:39–47. doi: 10.1055/s-2006-958163. [DOI] [PubMed] [Google Scholar]
- Leone TA, Rich W, Finer NN. Neonatal intubation: success of pediatric trainees. J Pediatr. 2005;146(5):638–641. doi: 10.1016/j.jpeds.2005.01.029. [DOI] [PubMed] [Google Scholar]
- LeSouef PN, England SJ, Bryan AC. Total resistance of the respiratory system in preterm infants with and without an endotracheal tube. J Pediatr. 1984;104(1):108–111. doi: 10.1016/s0022-3476(84)80605-8. [DOI] [PubMed] [Google Scholar]
- Lewis JF, Ikegami M, Jobe AH, Tabor B. Aerosolized surfactant treatment of preterm lambs. J Appl Physiol. 1991;70(2):869–876. doi: 10.1152/jappl.1991.70.2.869. [DOI] [PubMed] [Google Scholar]
- Lewis DF, Futayyeh S, Towers CV, Asrat T, Edwards MS, Brooks GG. Preterm delivery from 34 to 37 weeks of gestation: is respiratory distress syndrome a problem? Am J Obstet Gynecol. 1996;174(2):525–528. doi: 10.1016/s0002-9378(96)70421-0. [DOI] [PubMed] [Google Scholar]
- Lieberman E, Torday J, Barbieri R, Cohen A, Van Vunakis H, Weiss ST. Association of intrauterine cigarette smoke exposure with indices of fetal lung maturation. Obstet Gynecol. 1992;79(4):564–570. [PubMed] [Google Scholar]
- Liechty EA, Donovan E, Purohit D, Gilhooly J, Feldman B, Noguchi A, et al. Reduction of neonatal mortality after multiple doses of bovine surfactant in low birth weight neonates with respiratory distress syndrome. Pediatrics. 1991;88(1):19–28. [PubMed] [Google Scholar]
- Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972;50(4):515–525. [PubMed] [Google Scholar]
- Lin CH, Wang ST, Lin YJ, Yeh TF. Efficacy of nasal intermittent positive pressure ventilation in treating apnea of prematurity. Pediatr Pulmonol. 1998;26(5):349–353. doi: 10.1002/(sici)1099-0496(199811)26:5<349::aid-ppul8>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Lin CY, Zhang H, Cheng KC, Slutsky AS. Mechanical ventilation may increase susceptibility to the development of bacteremia. Crit Care Med. 2003;31:1429–1434. doi: 10.1097/01.CCM.0000063449.58029.81. [DOI] [PubMed] [Google Scholar]
- Lin HC, Su BH, Lin TW, Peng CT, Tsai CH. Risk factors of mortality in meconium aspiration syndrome: review of 314 cases. Acta Paediatr Taiwan. 2004;45:30–34. [PubMed] [Google Scholar]
- Lin AE, Pober BR, Adatia I. Congenital diaphragmatic hernia and associated cardiovascular malformations: type, frequency, and impact on management. Am J Med Genet C Semin Med Genet. 2007;145(2):201–216. doi: 10.1002/ajmg.c.30131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linderkamp O, Versmold HT, Fendel H, Riegel KP, Betke K. Association of neonatal respiratory distress with birth asphyxia and deficiency of red cell mass in premature infants. Eur J Pediatr. 1978;129(3):167–173. doi: 10.1007/BF00442160. [DOI] [PubMed] [Google Scholar]
- Lindner W, Vossbeck S, Hummler H, Pohlandt F. Delivery room management of extremely low birth weight infants: spontaneous breathing or intubation? Pediatrics. 1999;103(5 Pt 1):961–967. doi: 10.1542/peds.103.5.961. [DOI] [PubMed] [Google Scholar]
- Lindwall R, Blennow M, Svensson M, Jonsson B, Berggren-Bostrom E, Flanby M, et al. A pilot study of inhaled nitric oxide in preterm infants treated with nasal continuous positive airway pressure for respiratory distress syndrome. Intensive Care Med. 2005;31(7):959–964. doi: 10.1007/s00134-005-2593-5. [DOI] [PubMed] [Google Scholar]
- Liptsen E, Aghai ZH, Pyon KH, Saslow JG, Nakhla T, Long J, et al. Work of breathing during nasal continuous positive airway pressure in preterm infants: a comparison of bubble vs variable-flow devices. J Perinatol. 2005;25(7):453–458. doi: 10.1038/sj.jp.7211325. [DOI] [PubMed] [Google Scholar]
- Lista G, Colnaghi M, Castoldi F, Condo V, Reali R, Compagnoni G, et al. Impact of targeted-volume ventilation on lung inflammatory response in preterm infants with respiratory distress syndrome (RDS) Pediatr Pulmonol. 2004;37(6):510–514. doi: 10.1002/ppul.10458. [DOI] [PubMed] [Google Scholar]
- Locke R, Greenspan JS, Shaffer TH, Rubenstein SD, Wolfson MR. Effect of nasal CPAP on thoracoabdominal motion in neonates with respiratory insufficiency. Pediatr Pulmonol. 1991;11(3):259–264. doi: 10.1002/ppul.1950110313. [DOI] [PubMed] [Google Scholar]
- Logan JW, Rice HE, Goldberg RN, Cotten CM. Congenital diaphragmatic hernia: a systematic review and summary of best-evidence practice strategies. J Perinatol. 2007;27(9):535–549. doi: 10.1038/sj.jp.7211794. [DOI] [PubMed] [Google Scholar]
- Lotze A, Mitchell BR, Bulas DI, Zola EM, Shalwitz RA, Gunkel JH. Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. Survanta in Term Infants Study Group. J Pediatr. 1998;132:40–47. doi: 10.1016/s0022-3476(98)70482-2. [DOI] [PubMed] [Google Scholar]
- Lund DP, Mitchell J, Kharasch V, Quigley S, Kuehn M, Wilson JM. Congenital diaphragmatic hernia: the hidden morbidity. J Pediatr Surg. 1994;29(2):258–262. doi: 10.1016/0022-3468(94)90329-8. [DOI] [PubMed] [Google Scholar]
- Lundstrom KE. Early nasal continuous positive airway pressure for preterm neonates: the need for randomized trials. Acta Paediatr. 2003;92(10):1124–1126. [PubMed] [Google Scholar]
- Makri V, Hospes B, Stoll-Becker S, Borkhardt A, Gortner L. Polymorphisms of surfactant protein B encoding gene: modifiers of the course of neonatal respiratory distress syndrome? Eur J Pediatr. 2002;161(11):604–608. doi: 10.1007/s00431-002-1046-1. [DOI] [PubMed] [Google Scholar]
- Masuda T, Kazama T, Ikeda K, Ohba S. Tension pneumomediastinum secondary to meconium aspiration syndrome. Crit Care Med. 1984;12:1009. doi: 10.1097/00003246-198411000-00022. [DOI] [PubMed] [Google Scholar]
- Maturana A, Torres-Pereyra J, Salinas R, Astudillo P, Moya FR, The Chile Surf Group A randomized trial of natural surfactant for moderate to severe meconium aspiration syndrome. Pediatr Res. 2005;57:1545A. [Google Scholar]
- Mazela J, Merritt TA, Finer NN. Aerosolized surfactants. Curr Opin Pediatr. 2007;19(2):155–162. doi: 10.1097/MOP.0b013e32807fb013. [DOI] [PubMed] [Google Scholar]
- Mazzella M, Bellini C, Calevo MG, Campone F, Massocco D, Mezzano P, et al. A randomised control study comparing the Infant Flow Driver with nasal continuous positive airway pressure in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2001;85(2):F86–F90. doi: 10.1136/fn.85.2.F86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCallion N, Davis PG, Morley CJ (2005) Volume-targeted versus pressure-limited ventilation in the neonate. Cochrane Database Syst Rev (3):CD003666 [DOI] [PubMed]
- McCann EM, Goldman SL, Brady JP. Pulmonary function in the sick newborn infant. Pediatr Res. 1987;21(4):313–325. doi: 10.1203/00006450-198704000-00001. [DOI] [PubMed] [Google Scholar]
- McCormick MC, Workman-Daniels K, Brooks-Gunn J, Peckham GJ. Hospitalization of very low birth weight children at school age. J Pediatr. 1993;122(3):360–365. doi: 10.1016/s0022-3476(05)83417-1. [DOI] [PubMed] [Google Scholar]
- McGahren ED, Mallik K, Rodgers BM. Neurological outcome is diminished in survivors of congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation. J Pediatr Surg. 1997;32(8):1216–1220. doi: 10.1016/s0022-3468(97)90685-0. [DOI] [PubMed] [Google Scholar]
- Mendelson CR, Alcorn JL, Gao E. The pulmonary surfactant protein genes and their regulation in fetal lung. Semin Perinatol. 1993;17(4):223–232. [PubMed] [Google Scholar]
- Menon G, Boyle EM, Bergqvist LL, McIntosh N, Barton BA, Anand KJ. Morphine analgesia and gastrointestinal morbidity in preterm infants: secondary results from the NEOPAIN trial. Arch Dis Child Fetal Neonatal Ed. 2008;93(5):F362–F367. doi: 10.1136/adc.2007.119297. [DOI] [PubMed] [Google Scholar]
- Mercier JC, Hummler H, Durrmeyer X, Sanchez-Luna M, Carnielli VP, Field D, Greenough A, Van Overmeire B, Jonsson B, Hallman M, Baldassarre J (2009) Inhaled nitric oxide for the prevention of bronchopulmonary dysplasia in preterm infants. Pediatric Academic Society, Baltimore
- Metkus AP, Esserman L, Sola A, Harrison MR, Adzick NS. Cost per anomaly: what does a diaphragmatic hernia cost? J Pediatr Surg. 1995;30(2):226–230. doi: 10.1016/0022-3468(95)90565-0. [DOI] [PubMed] [Google Scholar]
- Mettauer NL, Pierce CM, Cassidy JV, Kiely EM, Petros AJ. One-year survival in congenital diaphragmatic hernia, 1995–2006. Arch Dis Child. 2009;94(5):407. doi: 10.1136/adc.2008.147827. [DOI] [PubMed] [Google Scholar]
- Michna J, Jobe AH, Ikegami M. Positive end-expiratory pressure preserves surfactant function in preterm lambs. Am J Respir Crit Care Med. 1999;160(2):634–639. doi: 10.1164/ajrccm.160.2.9902016. [DOI] [PubMed] [Google Scholar]
- Migliazza L, Bellan C, Alberti D, Auriemma A, Burgio G, Locatelli G, et al. Retrospective study of 111 cases of congenital diaphragmatic hernia treated with early high-frequency oscillatory ventilation and presurgical stabilization. J Pediatr Surg. 2007;42(9):1526–1532. doi: 10.1016/j.jpedsurg.2007.04.015. [DOI] [PubMed] [Google Scholar]
- Migliori C, Motta M, Angeli A, Chirico G. Nasal bilevel vs. continuous positive airway pressure in preterm infants. Pediatr Pulmonol. 2005;40(5):426–430. doi: 10.1002/ppul.20276. [DOI] [PubMed] [Google Scholar]
- Migliori C, Gancia P, Garzoli E, Spinoni V, Chirico G. The Effects of helium/oxygen mixture (heliox) before and after extubation in long-term mechanically ventilated very low birth weight infants. Pediatrics. 2009;123(6):1524–1528. doi: 10.1542/peds.2008-0937. [DOI] [PubMed] [Google Scholar]
- Miguet D, Claris O, Lapillonne A, Bakr A, Chappuis JP, Salle BL. Preoperative stabilization using high-frequency oscillatory ventilation in the management of congenital diaphragmatic hernia. Crit Care Med. 1994;22(9 Suppl):S77–S82. doi: 10.1097/00003246-199422091-00008. [DOI] [PubMed] [Google Scholar]
- Miller JD, Carlo WA. Safety and effectiveness of permissive hypercapnia in the preterm infant. Curr Opin Pediatr. 2007;19(2):142–144. doi: 10.1097/MOP.0b013e3280895e12. [DOI] [PubMed] [Google Scholar]
- Miller MJ, Martin RJ. Pathophysiology of apnea of prematurity. In: Polin RA, Fox WW, Abman SH, editors. Fetal and neonatal physiology. 3. Philadelphia: Saunders; 2004. p. 905. [Google Scholar]
- Miller MJ, Carlo WA, Martin RJ. Continuous positive airway pressure selectively reduces obstructive apnea in preterm infants. J Pediatr. 1985;106(1):91–94. doi: 10.1016/s0022-3476(85)80475-3. [DOI] [PubMed] [Google Scholar]
- Miller MJ, DiFiore JM, Strohl KP, Martin RJ. Effects of nasal CPAP on supraglottic and total pulmonary resistance in preterm infants. J Appl Physiol. 1990;68(1):141–146. doi: 10.1152/jappl.1990.68.1.141. [DOI] [PubMed] [Google Scholar]
- Moa G, Nilsson K, Zetterstrom H, Jonsson LO. A new device for administration of nasal continuous positive airway pressure in the newborn: an experimental study. Crit Care Med. 1988;16(12):1238–1242. doi: 10.1097/00003246-198812000-00013. [DOI] [PubMed] [Google Scholar]
- Moretti C, Gizzi C, Papoff P, Lampariello S, Capoferri M, Calcagnini G, et al. Comparing the effects of nasal synchronized intermittent positive pressure ventilation (nSIPPV) and nasal continuous positive airway pressure (nCPAP) after extubation in very low birth weight infants. Early Hum Dev. 1999;56(2–3):167–177. doi: 10.1016/s0378-3782(99)00046-8. [DOI] [PubMed] [Google Scholar]
- Morini F, Capolupo I, Masi R, Ronchetti MP, Locatelli M, Corchia C, et al. Hearing impairment in congenital diaphragmatic hernia: the inaudible and noiseless foot of time. J Pediatr Surg. 2008;43(2):380–384. doi: 10.1016/j.jpedsurg.2007.10.048. [DOI] [PubMed] [Google Scholar]
- Morley CJ, Lau R, De Paoli A, Davis PG. Nasal continuous positive airway pressure: does bubbling improve gas exchange? Arch Dis Child Fetal Neonatal Ed. 2005;90(4):F343–F344. doi: 10.1136/adc.2004.062588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358(7):700–708. doi: 10.1056/NEJMoa072788. [DOI] [PubMed] [Google Scholar]
- Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995;102(2):101–106. doi: 10.1111/j.1471-0528.1995.tb09060.x. [DOI] [PubMed] [Google Scholar]
- Moses D, Holm BA, Spitale P, Liu MY, Enhorning G. Inhibition of pulmonary surfactant function by meconium. Am J Obstet Gynecol. 1991;164:477–481. doi: 10.1016/s0002-9378(11)80003-7. [DOI] [PubMed] [Google Scholar]
- Moss RL, Chen CM, Harrison MR. Prosthetic patch durability in congenital diaphragmatic hernia: a long-term follow-up study. J Pediatr Surg. 2001;36(1):152–154. doi: 10.1053/jpsu.2001.20037. [DOI] [PubMed] [Google Scholar]
- Moya FR, Gadzinowski J, Bancalari E, Salinas V, Kopelman B, Bancalari A, et al. A multicenter, randomized, masked, comparison trial of lucinactant, colfosceril palmitate, and beractant for the prevention of respiratory distress syndrome among very preterm infants. Pediatrics. 2005;115(4):1018–1029. doi: 10.1542/peds.2004-2183. [DOI] [PubMed] [Google Scholar]
- Moya F, Sinha S, Gadzinowski J, D’Agostino R, Segal R, Guardia C, et al. One-year follow-up of very preterm infants who received lucinactant for prevention of respiratory distress syndrome: results from 2 multicenter randomized, controlled trials. Pediatrics. 2007;119(6):e1361–e1370. doi: 10.1542/peds.2006-0149. [DOI] [PubMed] [Google Scholar]
- Muratore CS, Wilson JM. Congenital diaphragmatic hernia: where are we and where do we go from here? Semin Perinatol. 2000;24(6):418–428. doi: 10.1053/sper.2000.21111. [DOI] [PubMed] [Google Scholar]
- Muratore CS, Kharasch V, Lund DP, Sheils C, Friedman S, Brown C, et al. Pulmonary morbidity in 100 survivors of congenital diaphragmatic hernia monitored in a multidisciplinary clinic. J Pediatr Surg. 2001;36(1):133–140. doi: 10.1053/jpsu.2001.20031. [DOI] [PubMed] [Google Scholar]
- Muratore CS, Utter S, Jaksic T, Lund DP, Wilson JM. Nutritional morbidity in survivors of congenital diaphragmatic hernia. J Pediatr Surg. 2001;36(8):1171–1176. doi: 10.1053/jpsu.2001.25746. [DOI] [PubMed] [Google Scholar]
- Musante G, Schulze A, Gerhardt T, Everett R, Claure N, Schaller P, et al. Proportional assist ventilation decreases thoracoabdominal asynchrony and chest wall distortion in preterm infants. Pediatr Res. 2001;49(2):175–180. doi: 10.1203/00006450-200102000-00008. [DOI] [PubMed] [Google Scholar]
- Mutch L, Newdick M, Lodwick A, Chalmers I. Secular changes in rehospitalization of very low birth weight infants. Pediatrics. 1986;78(1):164–171. [PubMed] [Google Scholar]
- Myers TR. AARC Clinical Practice Guideline: selection of an oxygen delivery device for neonatal and pediatric patients – 2002 revision & update. Respir Care. 2002;47(6):707–716. [PubMed] [Google Scholar]
- Naeye RL, Dellinger WS, Blanc WA. Fetal and maternal features of antenatal bacterial infections. J Pediatr. 1971;79:733–739. doi: 10.1016/s0022-3476(71)80383-9. [DOI] [PubMed] [Google Scholar]
- Nafday SM, Green RS, Lin J, Brion LP, Ochshorn I, Holzman IR. Is there an advantage of using pressure support ventilation with volume guarantee in the initial management of premature infants with respiratory distress syndrome? A pilot study. J Perinatol. 2005;25(3):193–197. doi: 10.1038/sj.jp.7211233. [DOI] [PubMed] [Google Scholar]
- Neonatal acute respiratory failure outcome data. The Extracorporeal Life Support Organisation (2009)
- Neonatal ECMO Registry of the Extracorporeal Life Support Organisation (2004) Neonatal ECMO. Ann Arbor
- Newnham JP, Jobe AH. Should we be prescribing repeated courses of antenatal corticosteroids? Semin Fetal Neonatal Med. 2009;14(3):157–163. doi: 10.1016/j.siny.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Ng E, Taddio A, Ohlsson A (2003) Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev (1):CD002052 [DOI] [PMC free article] [PubMed]
- Ng GY, Derry C, Marston L, Choudhury M, Holmes K, Calvert SA. Reduction in ventilator-induced lung injury improves outcome in congenital diaphragmatic hernia? Pediatr Surg Int. 2008;24(2):145–150. doi: 10.1007/s00383-007-2051-2. [DOI] [PubMed] [Google Scholar]
- Niblett DJ, Sandhar BK, Dunnill MS, Sykes MK. Comparison of the effects of high frequency oscillation and controlled mechanical ventilation on hyaline membrane formation in a rabbit model of the neonatal respiratory distress syndrome. Br J Anaesth. 1989;62(6):628–636. doi: 10.1093/bja/62.6.628. [DOI] [PubMed] [Google Scholar]
- Nijhuis-van der Sanden MW, van der Cammen-van Zijp MH, Janssen AJ, Reuser JJ, Mazer P, van Heijst AF, et al. Motor performance in five-year-old extracorporeal membrane oxygenation survivors: a population-based study. Crit Care. 2009;13(2):R47. doi: 10.1186/cc7770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson R, Grossmann G, Robertson B. Artificial ventilation of premature newborn rabbits: effects of positive end-expiratory pressure on lung mechanics and lung morphology. Acta Paediatr Scand. 1980;69(5):597–602. doi: 10.1111/j.1651-2227.1980.tb07328.x. [DOI] [PubMed] [Google Scholar]
- Nissen MD. Congenital and neonatal pneumonia. Paediatr Respir Rev. 2007;8:195–203. doi: 10.1016/j.prrv.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Nobuhara KK, Lund DP, Mitchell J, Kharasch V, Wilson JM. Long-term outlook for survivors of congenital diaphragmatic hernia. Clin Perinatol. 1996;23(4):873–887. [PubMed] [Google Scholar]
- Nock ML, Difiore JM, Arko MK, Martin RJ. Relationship of the ventilatory response to hypoxia with neonatal apnea in preterm infants. J Pediatr. 2004;144:291–295. doi: 10.1016/j.jpeds.2003.11.035. [DOI] [PubMed] [Google Scholar]
- Nolent P, Hallalel F, Chevalier JY, Flamant C, Renolleau S. Meconium aspiration syndrome requiring mechanical ventilation: incidence and respiratory management in France (2000–2001) Arch Pediatr. 2004;11:417–422. doi: 10.1016/j.arcped.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Noori S, Friedlich P, Wong P, Garingo A, Seri I. Cardiovascular effects of sildenafil in neonates and infants with congenital diaphragmatic hernia and pulmonary hypertension. Neonatology. 2007;91(2):92–100. doi: 10.1159/000097125. [DOI] [PubMed] [Google Scholar]
- Northway WH, Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967;276(7):357–368. doi: 10.1056/NEJM196702162760701. [DOI] [PubMed] [Google Scholar]
- O’Donnell CP, Kamlin CO, Davis PG, Morley CJ. Endotracheal intubation attempts during neonatal resuscitation: success rates, duration, and adverse effects. Pediatrics. 2006;117(1):e16–e21. doi: 10.1542/peds.2005-0901. [DOI] [PubMed] [Google Scholar]
- Oelberg DG, Downey SA, Flynn MM. Bile salt-induced intracellular Ca++ accumulation in type II pneumocytes. Lung. 1990;168:297–308. doi: 10.1007/BF02719707. [DOI] [PubMed] [Google Scholar]
- Ojomo EO, Coustan DR. Absence of evidence of pulmonary maturity at amniocentesis in term infants of diabetic mothers. Am J Obstet Gynecol. 1990;163(3):954–957. doi: 10.1016/0002-9378(90)91103-j. [DOI] [PubMed] [Google Scholar]
- Olsen SL, Thibeault DW, Truog WE. Crossover trial comparing pressure support with synchronized intermittent mandatory ventilation. J Perinatol. 2002;22(6):461–466. doi: 10.1038/sj.jp.7210772. [DOI] [PubMed] [Google Scholar]
- Onrust SV, Dooley M, Goa KL. Calfactant: a review of its use in neonatal respiratory distress syndrome. Paediatr Drugs. 1999;1(3):219–243. doi: 10.2165/00128072-199901030-00006. [DOI] [PubMed] [Google Scholar]
- Ostrea EMJ, Naqvi M. The influence of gestational age on the ability of the fetus to pass meconium in utero. Clinical implications. Acta Obstet Gynecol Scand. 1982;61:275–277. doi: 10.3109/00016348209156571. [DOI] [PubMed] [Google Scholar]
- Owen LS, Morley CJ, Davis PG. Neonatal nasal intermittent positive pressure ventilation: what do we know in 2007? Arch Dis Child Fetal Neonatal Ed. 2007;92(5):F414–F418. doi: 10.1136/adc.2007.117614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen LS, Morley CJ, Davis PG. Neonatal nasal intermittent positive pressure ventilation: a survey of practice in England. Arch Dis Child Fetal Neonatal Ed. 2008;93(2):F148–F150. doi: 10.1136/adc.2007.118109. [DOI] [PubMed] [Google Scholar]
- Pandit PB, Courtney SE, Pyon KH, Saslow JG, Habib RH. Work of breathing during constant- and variable-flow nasal continuous positive airway pressure in preterm neonates. Pediatrics. 2001;108(3):682–685. doi: 10.1542/peds.108.3.682. [DOI] [PubMed] [Google Scholar]
- Pandya HC, Kotecha S. Chronic lung disease of prematurity: clinical and pathophysiological correlates. Monaldi Arch Chest Dis. 2001;56(3):270–275. [PubMed] [Google Scholar]
- Pantalitschka T, Sievers J, Urschitz MS, Herberts T, Reher C, Poets CF. Randomized crossover trial of four nasal respiratory support systems on apnoea of prematurity in very low birth weight infants. Arch Dis Child Fetal Neonatal Ed. 2009;94:F245–F248. doi: 10.1136/adc.2008.148981. [DOI] [PubMed] [Google Scholar]
- Pape KE, Armstrong DL, Fitzhardinge PM. Central nervous system pathology associated with mask ventilation in the very low birthweight infant: a new etiology for intracerebellar hemorrhages. Pediatrics. 1976;58(4):473–483. [PubMed] [Google Scholar]
- Papoff P, Caresta E, Versacci P, Grossi R, Midulla F, Moretti C. The role of terlipressin in the management of severe pulmonary hypertension in congenital diaphragmatic hernia. Paediatr Anaesth. 2009;19(8):805–806. doi: 10.1111/j.1460-9592.2009.03078.x. [DOI] [PubMed] [Google Scholar]
- Paranka MS, Clark RH, Yoder BA, Null DM., Jr Predictors of failure of high-frequency oscillatory ventilation in term infants with severe respiratory failure. Pediatrics. 1995;95:400–404. [PubMed] [Google Scholar]
- Patel D, Greenough A. Does nasal CPAP reduce bronchopulmonary dysplasia (BPD)? Acta Paediatr. 2008;97(10):1314–1317. doi: 10.1111/j.1651-2227.2008.00931.x. [DOI] [PubMed] [Google Scholar]
- ATS-ERS Pediatrics Assembly Respiratory mechanics in infants: physiologic evaluation in health and disease. American Thoracic Society/European Respiratory Society. Am Rev Respir Dis. 1993;147:474–496. doi: 10.1164/ajrccm/147.2.474. [DOI] [PubMed] [Google Scholar]
- Pellicano A, Tingay DG, Mills JF, Fasulakis S, Morley CJ, Dargaville PA. Comparison of four methods of lung volume recruitment during high frequency oscillatory ventilation. Intensive Care Med. 2009;35:1990–1998. doi: 10.1007/s00134-009-1628-8. [DOI] [PubMed] [Google Scholar]
- Phatak RS, Pairaudeau CF, Smith CJ, Pairaudeau PW, Klonin H. Heliox with inhaled nitric oxide: a novel strategy for severe localized interstitial pulmonary emphysema in preterm neonatal ventilation. Respir Care. 2008;53(12):1731–1738. [PubMed] [Google Scholar]
- Pillow JJ, Hillman N, Moss TJ, Polglase G, Bold G, Beaumont C, et al. Bubble continuous positive airway pressure enhances lung volume and gas exchange in preterm lambs. Am J Respir Crit Care Med. 2007;176(1):63–69. doi: 10.1164/rccm.200609-1368OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piotrowski A, Sobala W, Kawczynski P. Patient-initiated, pressure-regulated, volume-controlled ventilation compared with intermittent mandatory ventilation in neonates: a prospective, randomised study. Intensive Care Med. 1997;23(9):975–981. doi: 10.1007/s001340050441. [DOI] [PubMed] [Google Scholar]
- Piper JM, Xenakis EM, McFarland M, Elliott BD, Berkus MD, Langer O. Do growth-retarded premature infants have different rates of perinatal morbidity and mortality than appropriately grown premature infants? Obstet Gynecol. 1996;87(2):169–174. doi: 10.1016/0029-7844(95)00400-9. [DOI] [PubMed] [Google Scholar]
- Poets CF. Pathophysiology of apnea of prematurity: implications from observational studies. In: Mathew OP, editor. Respiratory control and disorders in the newborn. New York: Marcel Dekker, Inc.; 2003. pp. 295–316. [Google Scholar]
- Possmayer F. Physicochemical aspects of pulmonary surfactant. In: Polin RA, Fox WW, Abman SH, editors. Fetal and neonatal physiology. 3. Philadelphia: W.B. Saunders; 2004. pp. 1014–1034. [Google Scholar]
- Praud JP, Reix P. Upper airways and neonatal respiration. Respir Physiol Neurobiol. 2005;149:131–141. doi: 10.1016/j.resp.2005.04.020. [DOI] [PubMed] [Google Scholar]
- Probyn ME, Hooper SB, Dargaville PA, McCallion N, Crossley K, Harding R, et al. Positive end expiratory pressure during resuscitation of premature lambs rapidly improves blood gases without adversely affecting arterial pressure. Pediatr Res. 2004;56(2):198–204. doi: 10.1203/01.PDR.0000132752.94155.13. [DOI] [PubMed] [Google Scholar]
- Quinteros A, Gonzalez AJ, Salinas JA, Luco M, Tapia JL (2009) Hypopharyngeal oxygen concentration and pressures delivered by nasal cannula in preterm infants. Relationship with flow, gas mixture and infant weight. Pediatric Academic Society, Baltimore [DOI] [PubMed]
- Ramanathan R. Optimal ventilatory strategies and surfactant to protect the preterm lungs. Neonatology. 2008;93(4):302–308. doi: 10.1159/000121456. [DOI] [PubMed] [Google Scholar]
- Ramanathan R, Sardesai S. Lung protective ventilatory strategies in very low birth weight infants. J Perinatol. 2008;28(Suppl 1):S41–S46. doi: 10.1038/jp.2008.49. [DOI] [PubMed] [Google Scholar]
- Ramanathan R, Rasmussen MR, Gerstmann DR, Finer N, Sekar K. A randomized, multicenter masked comparison trial of poractant alfa (Curosurf) versus beractant (Survanta) in the treatment of respiratory distress syndrome in preterm infants. Am J Perinatol. 2004;21(3):109–119. doi: 10.1055/s-2004-823779. [DOI] [PubMed] [Google Scholar]
- Ramsden CA, Reynolds EO. Ventilator settings for newborn infants. Arch Dis Child. 1987;62:529–538. doi: 10.1136/adc.62.5.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rana AR, Khouri JS, Teitelbaum DH, Drongowski RA, Hirschl RB, Mychaliska GB. Salvaging the severe congenital diaphragmatic hernia patient: is a silo the solution? J Pediatr Surg. 2008;43(5):788–791. doi: 10.1016/j.jpedsurg.2007.12.011. [DOI] [PubMed] [Google Scholar]
- Rasheed A, Tindall S, Cueny DL, Klein MD, Delaney-Black V. Neurodevelopmental outcome after congenital diaphragmatic hernia: extracorporeal membrane oxygenation before and after surgery. J Pediatr Surg. 2001;36(4):539–544. doi: 10.1053/jpsu.2001.22278. [DOI] [PubMed] [Google Scholar]
- Rennie JM. Roberton’s textbook of neonatology. 4. Philadelphia: Elsevier; 2005. [Google Scholar]
- Revenis ME, Glass P, Short BL. Mortality and morbidity rates among lower birth weight infants (2000 to 2500 grams) treated with extracorporeal membrane oxygenation. J Pediatr. 1992;121(3):452–458. doi: 10.1016/s0022-3476(05)81804-9. [DOI] [PubMed] [Google Scholar]
- Reyes C, Chang LK, Waffarn F, Mir H, Warden MJ, Sills J. Delayed repair of congenital diaphragmatic hernia with early high-frequency oscillatory ventilation during preoperative stabilization. J Pediatr Surg. 1998;33(7):1010–1016. doi: 10.1016/s0022-3468(98)90523-1. [DOI] [PubMed] [Google Scholar]
- Reynolds EO, Roberton NR, Wigglesworth JS. Hyaline membrane disease, respiratory distress, and surfactant deficiency. Pediatrics. 1968;42(5):758–768. [PubMed] [Google Scholar]
- Richardson CP, Jung AL. Effects of continuous positive airway pressure on pulmonary function and blood gases of infants with respiratory distress syndrome. Pediatr Res. 1978;12(7):771–774. doi: 10.1203/00006450-197807000-00006. [DOI] [PubMed] [Google Scholar]
- Richardson DK, Torday JS. Racial differences in predictive value of the lecithin/sphingomyelin ratio. Am J Obstet Gynecol. 1994;170(5 Pt 1):1273–1278. doi: 10.1016/s0002-9378(94)70141-5. [DOI] [PubMed] [Google Scholar]
- Richardson P, Wyman ML, Jung AL. Functional residual capacity and severity of respiratory distress syndrome in infants. Crit Care Med. 1980;8(11):637–640. doi: 10.1097/00003246-198011000-00008. [DOI] [PubMed] [Google Scholar]
- Rider ED, Ikegami M, Whitsett JA, Hull W, Absolom D, Jobe AH. Treatment responses to surfactants containing natural surfactant proteins in preterm rabbits. Am Rev Respir Dis. 1993;147(3):669–676. doi: 10.1164/ajrccm/147.3.669. [DOI] [PubMed] [Google Scholar]
- Rigatto H. Apnea. In: Thibeault DW, Gregory GA, editors. Neonatal pulmonary care. 2. Norwalk: Appleton Century-Crofts; 1986. pp. 641–656. [Google Scholar]
- Rishi A, Hatzis D, McAlmon K, Floros J. An allelic variant of the 6A gene for human surfactant protein A. Am J Physiol. 1992;262(5 Pt 1):L566–L573. doi: 10.1152/ajplung.1992.262.5.L566. [DOI] [PubMed] [Google Scholar]
- Robertson NJ, McCarthy LS, Hamilton PA, Moss AL. Nasal deformities resulting from flow driver continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 1996;75(3):F209–F212. doi: 10.1136/fn.75.3.f209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha GM, Bianchi RF, Severo M, Rodrigues MM, Baptista MJ, Correia-Pinto J, et al. Congenital diaphragmatic hernia – the neonatal period (part I) Eur J Pediatr Surg. 2008;18(4):219–223. doi: 10.1055/s-2008-1038502. [DOI] [PubMed] [Google Scholar]
- Rojas MA, Lozano JM, Rojas MX, Laughon M, Bose CL, Rondon MA, et al. Very early surfactant without mandatory ventilation in premature infants treated with early continuous positive airway pressure: a randomized, controlled trial. Pediatrics. 2009;123(1):137–142. doi: 10.1542/peds.2007-3501. [DOI] [PubMed] [Google Scholar]
- Ronnestad A, Abrahamsen TG, Medbo S, Reigstad H, Lossius K, Kaaresen PI, et al. Septicemia in the first week of life in a Norwegian national cohort of extremely premature infants. Pediatrics. 2005;115(3):e262–e268. doi: 10.1542/peds.2004-1834. [DOI] [PubMed] [Google Scholar]
- Roy BJ, Rycus P, Conrad SA, Clark RH. The changing demographics of neonatal extracorporeal membrane oxygenation patients reported to the Extracorporeal Life Support Organization (ELSO) Registry. Pediatrics. 2000;106(6):1334–1338. doi: 10.1542/peds.106.6.1334. [DOI] [PubMed] [Google Scholar]
- Roze JC, Chambille B, Fleury MA, Debillon T, Gaultier C. Oxygen cost of breathing in newborn infants with long-term ventilatory support. J Pediatr. 1995;127(6):984–987. doi: 10.1016/s0022-3476(95)70044-7. [DOI] [PubMed] [Google Scholar]
- Rubaltelli FF, Bonafe L, Tangucci M, Spagnolo A, Dani C. Epidemiology of neonatal acute respiratory disorders. A multicenter study on incidence and fatality rates of neonatal acute respiratory disorders according to gestational age, maternal age, pregnancy complications and type of delivery. Italian Group of Neonatal Pneumology. Biol Neonate. 1998;74(1):7–15. doi: 10.1159/000014005. [DOI] [PubMed] [Google Scholar]
- Rubin BK, Tomkiewicz RP, Patrinos ME, Easa D. The surface and transport properties of meconium and reconstituted meconium solutions. Pediatr Res. 1996;40:834–838. doi: 10.1203/00006450-199612000-00010. [DOI] [PubMed] [Google Scholar]
- Ryan CA, Finer NN, Peters KL. Nasal intermittent positive-pressure ventilation offers no advantages over nasal continuous positive airway pressure in apnea of prematurity. Am J Dis Child. 1989;143(10):1196–1198. doi: 10.1001/archpedi.1989.02150220094026. [DOI] [PubMed] [Google Scholar]
- Rybak IA, O’Connor R, Ross A, Shevtsova NA, Nuding SC, Segers LS, Shannon R, Dick TE, Dunin-Barkowski WL, Orem JM, Solomon IC, Morris KF, Lindsey BG. Reconfiguration of the pontomedullary respiratory network: a computational modeling study with coordinated in vivo experiments. J Neurophysiol. 2008;100:1770–1799. doi: 10.1152/jn.90416.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sai Sunil Kinshore M, Dutta S, Kumar P (2009) Early nasal intermittent positive pressure ventilation versus continuous positive airway pressure for respiratory distress syndrome. Acta Paediatr 98(9):1412–1415 [DOI] [PubMed]
- Sakai H, Tamura M, Hosokawa Y, Bryan AC, Barker GA, Bohn DJ. Effect of surgical repair on respiratory mechanics in congenital diaphragmatic hernia. J Pediatr. 1987;111(3):432–438. doi: 10.1016/s0022-3476(87)80475-4. [DOI] [PubMed] [Google Scholar]
- Sakai H, Bohn DJ, Bryan AC. Congenital diaphragmatic hernia: does surgical repair really improve respiratory mechanics. Jpn J Pediatr Surg. 1987;19:881. doi: 10.1016/s0022-3476(87)80475-4. [DOI] [PubMed] [Google Scholar]
- Sakurai Y, Azarow K, Cutz E, Messineo A, Pearl R, Bohn D. Pulmonary barotrauma in congenital diaphragmatic hernia: a clinicopathological correlation. J Pediatr Surg. 1999;34(12):1813–1817. doi: 10.1016/s0022-3468(99)90319-6. [DOI] [PubMed] [Google Scholar]
- Sandri F, Ancora G, Lanzoni A, Tagliabue P, Colnaghi M, Ventura ML, et al. Prophylactic nasal continuous positive airways pressure in newborns of 28–31 weeks gestation: multicentre randomised controlled clinical trial. Arch Dis Child Fetal Neonatal Ed. 2004;89(5):F394–F398. doi: 10.1136/adc.2003.037010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandri F, Plavka R, Simeoni U. The CURPAP study: an international randomized controlled trial to evaluate the efficacy of combining prophylactic surfactant and early nasal continuous positive airway pressure in very preterm infants. Neonatology. 2008;94(1):60–62. doi: 10.1159/000113060. [DOI] [PubMed] [Google Scholar]
- Sandri F, Plavka R, Simeoni U (2009) CURPAP study – an international randomised controlled trial to evaluate the efficacy of combining prophylactic surfactant and early nasal CPAP in very preterm infants. Pediatric Academic Society, Baltimore [DOI] [PubMed]
- Sant’Ambrogio FB, Sant’Ambrogio G, Chung K. Effect of HCl-Pepsin laryngeal instillations on upper airway patency-maintaining mechanisms. J Appl Physiol. 1998;84:1299–1304. doi: 10.1152/jappl.1998.84.4.1299. [DOI] [PubMed] [Google Scholar]
- Santin R, Brodsky N, Bhandari V. A prospective observational pilot study of synchronized nasal intermittent positive pressure ventilation (SNIPPV) as a primary mode of ventilation in infants > or = 28 weeks with respiratory distress syndrome (RDS) J Perinatol. 2004;24(8):487–493. doi: 10.1038/sj.jp.7211131. [DOI] [PubMed] [Google Scholar]
- Saslow JG, Aghai ZH, Nakhla TA, Hart JJ, Lawrysh R, Stahl GE, et al. Work of breathing using high-flow nasal cannula in preterm infants. J Perinatol. 2006;26(8):476–480. doi: 10.1038/sj.jp.7211530. [DOI] [PubMed] [Google Scholar]
- Saugstad OD, Ramji S, Soll RF, Vento M. Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology. 2008;94(3):176–182. doi: 10.1159/000143397. [DOI] [PubMed] [Google Scholar]
- Scheurer MA, Bradley SM, Atz AM. Vasopressin to attenuate pulmonary hypertension and improve systemic blood pressure after correction of obstructed total anomalous pulmonary venous return. J Thorac Cardiovasc Surg. 2005;129(2):464–466. doi: 10.1016/j.jtcvs.2004.06.043. [DOI] [PubMed] [Google Scholar]
- Schlessel JS, Susskind H, Joel DD, Bossuyt A, Harrold WH, Zanzi I, et al. Effect of PEEP on regional ventilation and perfusion in the mechanically ventilated preterm lamb. J Nucl Med. 1989;30(8):1342–1350. [PubMed] [Google Scholar]
- Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, et al. Caffeine therapy for apnea of prematurity. N Engl J Med. 2006;354(20):2112–2121. doi: 10.1056/NEJMoa054065. [DOI] [PubMed] [Google Scholar]
- Schmidt B, Roberts R, Davis P, Doyle L, Barrington K, Ohlsson A, Solimano A, Tin W, for the Caffeine for Apnea of Prematurity Trial Group Caffeine therapy for apnea of prematurity. N Engl J Med. 2006;354:2112–2121. doi: 10.1056/NEJMoa054065. [DOI] [PubMed] [Google Scholar]
- Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, et al. Long-term effects of caffeine therapy for apnea of prematurity. N Engl J Med. 2007;357(19):1893–1902. doi: 10.1056/NEJMoa073679. [DOI] [PubMed] [Google Scholar]
- Schmolzer GM, Kamlin OF, Dawson JA, Davis PG, Morley CJ. Respiratory monitoring of neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed. 2010;95(4):F295–F303. doi: 10.1136/adc.2009.165878. [DOI] [PubMed] [Google Scholar]
- Schneider J, Mitchell I, Singhal N, Kirk V, Hasan SU. Prenatal cigarette smoke exposure attenuates recovery from hypoxemic challenge in preterm infants. Am J Respir Crit Care Med. 2008;178:520–526. doi: 10.1164/rccm.200803-432OC. [DOI] [PubMed] [Google Scholar]
- Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P. Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med. 2003;349(22):2099–2107. doi: 10.1056/NEJMoa031154. [DOI] [PubMed] [Google Scholar]
- Schulze A, Jonzon A, Schaller P, Sedin G. Effects of ventilator resistance and compliance on phrenic nerve activity in spontaneously breathing cats. Am J Respir Crit Care Med. 1996;153(2):671–676. doi: 10.1164/ajrccm.153.2.8564116. [DOI] [PubMed] [Google Scholar]
- Schulze A, Gerhardt T, Musante G, Schaller P, Claure N, Everett R, et al. Proportional assist ventilation in low birth weight infants with acute respiratory disease: a comparison to assist/control and conventional mechanical ventilation. J Pediatr. 1999;135(3):339–344. doi: 10.1016/s0022-3476(99)70131-9. [DOI] [PubMed] [Google Scholar]
- Schulze A, Rieger-Fackeldey E, Gerhardt T, Claure N, Everett R, Bancalari E. Randomized crossover comparison of proportional assist ventilation and patient-triggered ventilation in extremely low birth weight infants with evolving chronic lung disease. Neonatology. 2007;92(1):1–7. doi: 10.1159/000098376. [DOI] [PubMed] [Google Scholar]
- Schwartz SM, Vermilion RP, Hirschl RB. Evaluation of left ventricular mass in children with left-sided congenital diaphragmatic hernia. J Pediatr. 1994;125(3):447–451. doi: 10.1016/s0022-3476(05)83293-7. [DOI] [PubMed] [Google Scholar]
- Schwartz IP, Bernbaum JC, Rychik J, Grunstein M, D’Agostino J, Polin RA. Pulmonary hypertension in children following extracorporeal membrane oxygenation therapy and repair of congenital diaphragmatic hernia. J Perinatol. 1999;19(3):220–226. doi: 10.1038/sj.jp.7200141. [DOI] [PubMed] [Google Scholar]
- Seidner S, Pettenazzo A, Ikegami M, Jobe A. Corticosteroid potentiation of surfactant dose response in preterm rabbits. J Appl Physiol. 1988;64(6):2366–2371. doi: 10.1152/jappl.1988.64.6.2366. [DOI] [PubMed] [Google Scholar]
- Semakula N, Stewart DL, Goldsmith LJ, Cook LN, Bond SJ. Survival of patients with congenital diaphragmatic hernia during the ECMO era: an 11-year experience. J Pediatr Surg. 1997;32(12):1683–1689. doi: 10.1016/s0022-3468(97)90506-6. [DOI] [PubMed] [Google Scholar]
- Sen S, Reghu A, Ferguson SD. Efficacy of a single dose of antenatal steroid in surfactant-treated babies under 31 weeks’ gestation. J Matern Fetal Neonatal Med. 2002;12(5):298–303. doi: 10.1080/jmf.12.5.298.303. [DOI] [PubMed] [Google Scholar]
- Seppanen MP, Kaapa PO, Kero PO, Saraste M. Doppler-derived systolic pulmonary artery pressure in acute neonatal respiratory distress syndrome. Pediatrics. 1994;93(5):769–773. [PubMed] [Google Scholar]
- Shaffer TH, Lowe CA, Bhutani VK, Douglas PR. Liquid ventilation: effects on pulmonary function in distressed meconium-stained lambs. Pediatr Res. 1984;18:47–52. [PubMed] [Google Scholar]
- Shanmugananda K, Rawal J. Nasal trauma due to nasal continuous positive airway pressure in newborns. Arch Dis Child Fetal Neonatal Ed. 2007;92(1):F18. doi: 10.1136/adc.2006.095034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82(4):527–532. [PubMed] [Google Scholar]
- Shoemaker MT, Pierce MR, Yoder BA, DiGeronimo RJ. High flow nasal cannula versus nasal CPAP for neonatal respiratory disease: a retrospective study. J Perinatol. 2007;27(2):85–91. doi: 10.1038/sj.jp.7211647. [DOI] [PubMed] [Google Scholar]
- Short BL. Extracorporeal membrane oxygenation: use in meconium aspiration syndrome. J Perinatol. 2008;28(Suppl 3):S79–S83. doi: 10.1038/jp.2008.152. [DOI] [PubMed] [Google Scholar]
- Siebert JR, Haas JE, Beckwith JB. Left ventricular hypoplasia in congenital diaphragmatic hernia. J Pediatr Surg. 1984;19(5):567–571. doi: 10.1016/s0022-3468(84)80105-0. [DOI] [PubMed] [Google Scholar]
- Siew ML, Te Pas AB, Wallace MJ, Kitchen MJ, Lewis RA, Fouras A, et al. Positive end-expiratory pressure enhances development of a functional residual capacity in preterm rabbits ventilated from birth. J Appl Physiol. 2009;106(5):1487–1493. doi: 10.1152/japplphysiol.91591.2008. [DOI] [PubMed] [Google Scholar]
- Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, et al. Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999;5(12):1433–1436. doi: 10.1038/71012. [DOI] [PubMed] [Google Scholar]
- Singh SD, Bowe L, Smith J, Clarke P, Glover K, Pasquill A et al (2006) Nasal CPAP weaning of VLBW infants: is decreasing CPAP pressure or increasing time off the better strategy – results of a randomised controlled trial. Pediatric Academic Society annual meeting, San Francisco, Abstract No. 2635.4
- Singh J, Sinha SK, Alsop E, Gupta S, Mishra A, Donn SM. Long term follow-up of very low birthweight infants from a neonatal volume versus pressure mechanical ventilation trial. Arch Dis Child Fetal Neonatal Ed. 2009;94(5):F360–F362. doi: 10.1136/adc.2008.150938. [DOI] [PubMed] [Google Scholar]
- Singh BS, Clark RH, Powers RJ, Spitzer AR. Meconium aspiration syndrome remains a significant problem in the NICU: outcomes and treatment patterns in term neonates admitted for intensive care during a ten-year period. J Perinatol. 2009;29:497–503. doi: 10.1038/jp.2008.241. [DOI] [PubMed] [Google Scholar]
- Sinha SK, Donn SM. Fetal-to-neonatal maladaptation. Semin Fetal Neonatal Med. 2006;11(3):166–173. doi: 10.1016/j.siny.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Sinha SK, Donn SM. Newer forms of conventional ventilation for preterm newborns. Acta Paediatr. 2008;97(10):1338–1343. doi: 10.1111/j.1651-2227.2008.00869.x. [DOI] [PubMed] [Google Scholar]
- Sinha A, Yokoe D, Platt R. Epidemiology of neonatal infections: experience during and after hospitalization. Pediatr Infect Dis J. 2003;22:244–251. doi: 10.1097/01.inf.0000055060.32226.8a. [DOI] [PubMed] [Google Scholar]
- Sinha SK, Gupta S, Donn SM. Immediate respiratory management of the preterm infant. Semin Fetal Neonatal Med. 2008;13(1):24–29. doi: 10.1016/j.siny.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Skari H, Bjornland K, Frenckner B, Friberg LG, Heikkinen M, Hurme T, et al. Congenital diaphragmatic hernia: a survey of practice in Scandinavia. Pediatr Surg Int. 2004;20(5):309–313. doi: 10.1007/s00383-004-1186-7. [DOI] [PubMed] [Google Scholar]
- Skelton R, Jeffery HE. Factors affecting the neonatal response to artificial surfactant. J Paediatr Child Health. 1996;32(3):236–241. doi: 10.1111/j.1440-1754.1996.tb01561.x. [DOI] [PubMed] [Google Scholar]
- So BH, Shibuya K, Tamura M, Watanabe H, Kamoshita S. Clinical experience in using a new type of nasal prong for administration of N-CPAP. Acta Paediatr Jpn. 1992;34(3):328–333. doi: 10.1111/j.1442-200x.1992.tb00967.x. [DOI] [PubMed] [Google Scholar]
- Soe A, Hodgkinson J, Jani B, Ducker D. Nasal continuous positive airway pressure weaning in preterm infants [abstract] Eur J Pediatr. 2006;165(suppl 1):50. [Google Scholar]
- Soll RF, Blanco F (2001) Natural surfactant extract versus synthetic surfactant for neonatal respiratory distress syndrome. Cochrane Database Syst Rev (2):CD000144 [DOI] [PubMed]
- Soll RF, Morley CJ (2001) Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev (2):CD000510 [DOI] [PubMed]
- Soll R, Ozek E (2009) Multiple versus single doses of exogenous surfactant for the prevention or treatment of neonatal respiratory distress syndrome. Cochrane Database Syst Rev (1):CD000141 [DOI] [PubMed]
- Somaschini M, Locatelli G, Salvoni L, Bellan C, Colombo A. Impact of new treatments for respiratory failure on outcome of infants with congenital diaphragmatic hernia. Eur J Pediatr. 1999;158(10):780–784. doi: 10.1007/s004310051203. [DOI] [PubMed] [Google Scholar]
- Sosenko IR. Antenatal cocaine exposure produces accelerated surfactant maturation without stimulation of antioxidant enzyme development in the late gestation rat. Pediatr Res. 1993;33(4 Pt 1):327–331. doi: 10.1203/00006450-199304000-00004. [DOI] [PubMed] [Google Scholar]
- Speer CP, Gefeller O, Groneck P, Laufkotter E, Roll C, Hanssler L, et al. Randomised clinical trial of two treatment regimens of natural surfactant preparations in neonatal respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed. 1995;72(1):F8–F13. doi: 10.1136/fn.72.1.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer A. Apnea and home cardiorespiratory monitoring. In: McConnell MS, Imaizumi SO, editors. Guidelines for pediatric home health care. Elk Grove Village: American Academy of Pediatrics; 2002. pp. 357–387. [Google Scholar]
- Sreenan C, Lemke RP, Hudson-Mason A, Osiovich H. High-flow nasal cannulae in the management of apnea of prematurity: a comparison with conventional nasal continuous positive airway pressure. Pediatrics. 2001;107(5):1081–1083. doi: 10.1542/peds.107.5.1081. [DOI] [PubMed] [Google Scholar]
- Sriram S, Wall SN, Khoshnood B, Singh JK, Hsieh HL, Lee KS. Racial disparity in meconium-stained amniotic fluid and meconium aspiration syndrome in the United States, 1989–2000. Obstet Gynecol. 2003;102:1262–1268. doi: 10.1016/j.obstetgynecol.2003.07.006. [DOI] [PubMed] [Google Scholar]
- St Peter SD, Valusek PA, Tsao K, Holcomb GW, 3rd, Ostlie DJ, Snyder CL. Abdominal complications related to type of repair for congenital diaphragmatic hernia. J Surg Res. 2007;140(2):234–236. doi: 10.1016/j.jss.2007.03.018. [DOI] [PubMed] [Google Scholar]
- Steer PA, Flenady VJ, Shearman A, Lee TC, Tudehope DI, Charles BG. Periextubation caffeine in preterm neonates: a randomized dose response trial. J Paediatr Child Health. 2003;39:511–515. doi: 10.1046/j.1440-1754.2003.00207.x. [DOI] [PubMed] [Google Scholar]
- Stefanescu BM, Murphy WP, Hansell BJ, Fuloria M, Morgan TM, Aschner JL. A randomized, controlled trial comparing two different continuous positive airway pressure systems for the successful extubation of extremely low birth weight infants. Pediatrics. 2003;112(5):1031–1038. doi: 10.1542/peds.112.5.1031. [DOI] [PubMed] [Google Scholar]
- Steinhorn RH, Kinsella JP, Pierce C, Butrous G, Dilleen M, Oakes M, et al. Intravenous sildenafil in the treatment of neonates with persistent pulmonary hypertension. J Pediatr. 2009;155(6):841–847. doi: 10.1016/j.jpeds.2009.06.012. [DOI] [PubMed] [Google Scholar]
- Stenson BJ, Glover RM, Parry GJ, Wilkie RA, Laing IA, Tarnow-Mordi WO. Static respiratory compliance in the newborn. III: early changes after exogenous surfactant treatment. Arch Dis Child Fetal Neonatal Ed. 1994;70(1):F19–F24. doi: 10.1136/fn.70.1.f19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens TP, Harrington EW, Blennow M, Soll RF (2007) Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev (4):CD003063 [DOI] [PMC free article] [PubMed]
- Stolar CJ. What do survivors of congenital diaphragmatic hernia look like when they grow up? Semin Pediatr Surg. 1996;5(4):275–279. [PubMed] [Google Scholar]
- Stolar C, Dillon P, Reyes C. Selective use of extracorporeal membrane oxygenation in the management of congenital diaphragmatic hernia. J Pediatr Surg. 1988;23(3):207–211. doi: 10.1016/s0022-3468(88)80723-1. [DOI] [PubMed] [Google Scholar]
- Stolar CJ, Levy JP, Dillon PW, Reyes C, Belamarich P, Berdon WE. Anatomic and functional abnormalities of the esophagus in infants surviving congenital diaphragmatic hernia. Am J Surg. 1990;159(2):204–207. doi: 10.1016/s0002-9610(05)80261-2. [DOI] [PubMed] [Google Scholar]
- Stolar CJ, Crisafi MA, Driscoll YT. Neurocognitive outcome for neonates treated with extracorporeal membrane oxygenation: are infants with congenital diaphragmatic hernia different? J Pediatr Surg. 1995;30(2):366–371. doi: 10.1016/0022-3468(95)90591-x. [DOI] [PubMed] [Google Scholar]
- Subhedar NV, Ryan SW, Shaw NJ. Open randomised controlled trial of inhaled nitric oxide and early dexamethasone in high risk preterm infants. Arch Dis Child Fetal Neonatal Ed. 1997;77(3):F185–F190. doi: 10.1136/fn.77.3.f185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam P, Henderson-Smart DJ, Davis PG (2005) Prophylactic nasal continuous positive airways pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev (3):CD001243 [DOI] [PubMed]
- Sun B, Curstedt T, Robertson B. Surfactant inhibition in experimental meconium aspiration. Acta Paediatr. 1993;82:182–189. doi: 10.1111/j.1651-2227.1993.tb12635.x. [DOI] [PubMed] [Google Scholar]
- Swaminathan S, Quinn J, Stabile MW, Bader D, Platzker AC, Keens TG. Long-term pulmonary sequelae of meconium aspiration syndrome. J Pediatr. 1989;114:356–361. doi: 10.1016/s0022-3476(89)80551-7. [DOI] [PubMed] [Google Scholar]
- Sweet D, Bevilacqua G, Carnielli V, Greisen G, Plavka R, Didrik Saugstad O, et al. European consensus guidelines on the management of neonatal respiratory distress syndrome. J Perinat Med. 2007;35(3):175–186. doi: 10.1515/JPM.2007.048. [DOI] [PubMed] [Google Scholar]
- Szymankiewicz M, Gadzinowski J, Kowalska K. Pulmonary function after surfactant lung lavage followed by surfactant administration in infants with severe meconium aspiration syndrome. J Matern Fetal Neonatal Med. 2004;16:125–130. doi: 10.1080/14767050400003777. [DOI] [PubMed] [Google Scholar]
- te Pas AB, Walther FJ. A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics. 2007;120(2):322–329. doi: 10.1542/peds.2007-0114. [DOI] [PubMed] [Google Scholar]
- te Pas AB, Siew M, Wallace MJ, Kitchen MJ, Fouras A, Lewis RA, et al. Effect of sustained inflation length on establishing functional residual capacity at birth in ventilated premature rabbits. Pediatr Res. 2009;66(3):295–300. doi: 10.1203/PDR.0b013e3181b1bca4. [DOI] [PubMed] [Google Scholar]
- te Pas AB, Kamlin CO, Dawson JA, O’Donnell C, Sokol J, Stewart M, et al. Ventilation and spontaneous breathing at birth of infants with congenital diaphragmatic hernia. J Pediatr. 2009;154(3):369–373. doi: 10.1016/j.jpeds.2008.09.029. [DOI] [PubMed] [Google Scholar]
- Thach B. Fast breaths, slow breaths, small breaths, big breaths: importance of vagal innervation in the newborn lung. J Appl Physiol. 2001;91:2298–2300. doi: 10.1152/jappl.2001.91.5.2298. [DOI] [PubMed] [Google Scholar]
- Thach BT, Stark AR. Spontaneous neck flexion and airway obstruction during apneic spells in preterm infants. J Pediatr. 1979;94:275–281. doi: 10.1016/s0022-3476(79)80843-4. [DOI] [PubMed] [Google Scholar]
- Thomas M, Greenough A, Morton M. Prolonged ventilation and intact survival in very low birth weight infants. Eur J Pediatr. 2003;162(2):65–67. doi: 10.1007/s00431-002-0914-z. [DOI] [PubMed] [Google Scholar]
- Thome UH, Ambalavanan N. Permissive hypercapnia to decrease lung injury in ventilated preterm neonates. Semin Fetal Neonatal Med. 2009;14(1):21–27. doi: 10.1016/j.siny.2008.08.005. [DOI] [PubMed] [Google Scholar]
- Thome U, Kossel H, Lipowsky G, Porz F, Furste HO, Genzel-Boroviczeny O, et al. Randomized comparison of high-frequency ventilation with high-rate intermittent positive pressure ventilation in preterm infants with respiratory failure. J Pediatr. 1999;135(1):39–46. doi: 10.1016/s0022-3476(99)70325-2. [DOI] [PubMed] [Google Scholar]
- Thomson MA. Continuous positive airway pressure and surfactant; combined data from animal experiments and clinical trials. Biol Neonate. 2002;81(Suppl 1):16–19. doi: 10.1159/000056766. [DOI] [PubMed] [Google Scholar]
- Tibboel D, Gaag AV. Etiologic and genetic factors in congenital diaphragmatic hernia. Clin Perinatol. 1996;23(4):689–699. [PubMed] [Google Scholar]
- Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA. Trends in use and outcome of newborn infants treated with high frequency ventilation in Australia and New Zealand, 1996–2003. J Paediatr Child Health. 2007;43:160–166. doi: 10.1111/j.1440-1754.2007.01036.x. [DOI] [PubMed] [Google Scholar]
- Torday J. Cellular timing of fetal lung development. Semin Perinatol. 1992;16(2):130–139. [PubMed] [Google Scholar]
- Torfs CP, Curry CJ, Bateson TF, Honore LH. A population-based study of congenital diaphragmatic hernia. Teratology. 1992;46(6):555–565. doi: 10.1002/tera.1420460605. [DOI] [PubMed] [Google Scholar]
- Trachsel D, Selvadurai H, Bohn D, Langer JC, Coates AL. Long-term pulmonary morbidity in survivors of congenital diaphragmatic hernia. Pediatr Pulmonol. 2005;39(5):433–439. doi: 10.1002/ppul.20193. [DOI] [PubMed] [Google Scholar]
- Trachsel D, Selvadurai H, Adatia I, Bohn D, Schneiderman-Walker J, Wilkes D, et al. Resting and exercise cardiorespiratory function in survivors of congenital diaphragmatic hernia. Pediatr Pulmonol. 2006;41(6):522–529. doi: 10.1002/ppul.20359. [DOI] [PubMed] [Google Scholar]
- Tracy M, Downe L, Holberton J. How safe is intermittent positive pressure ventilation in preterm babies ventilated from delivery to newborn intensive care unit? Arch Dis Child Fetal Neonatal Ed. 2004;89(1):F84–F87. doi: 10.1136/fn.89.1.F84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran N, Lowe C, Sivieri EM, Shaffer TH. Sequential effects of acute meconium obstruction on pulmonary function. Pediatr Res. 1980;14:34–38. doi: 10.1203/00006450-198001000-00009. [DOI] [PubMed] [Google Scholar]
- Trevisanuto D, Grazzina N, Ferrarese P, Micaglio M, Verghese C, Zanardo V. Laryngeal mask airway used as a delivery conduit for the administration of surfactant to preterm infants with respiratory distress syndrome. Biol Neonate. 2005;87(4):217–220. doi: 10.1159/000083370. [DOI] [PubMed] [Google Scholar]
- Tripathi S, Saili A, Dutta R. Inflammatory markers in meconium induced lung injury in neonates and effect of steroids on their levels: a randomized controlled trial. Indian J Med Microbiol. 2007;25:103–107. doi: 10.4103/0255-0857.32714. [DOI] [PubMed] [Google Scholar]
- Truffert P, Storme L, Fily A (2008) Randomised trial comparing nasal CPAP versus conventional ventilation in extremely preterm infants. Progres en Neonatologie 28eme Journees Nationales de Neonatologie. Societe Francaise de Neonatologie, Paris
- Turkbay D, Dilmen U, Altug N. Pneumopericardium in a term infant on nasal continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 2007;92(3):F168. doi: 10.1136/adc.2006.107458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler DC, Murphy J, Cheney FW. Mechanical and chemical damage to lung tissue caused by meconium aspiration. Pediatrics. 1978;62:454–459. [PubMed] [Google Scholar]
- Ueda T, Ikegami M, Polk D, Mizuno K, Jobe A. Effects of fetal corticosteroid treatments on postnatal surfactant function in preterm lambs. J Appl Physiol. 1995;79(3):846–851. doi: 10.1152/jappl.1995.79.3.846. [DOI] [PubMed] [Google Scholar]
- UK Collaborative ECMO Trial Group UK collaborative randomised trial of neonatal extracorporeal membrane oxygenation. Lancet. 1996;348:75–82. [PubMed] [Google Scholar]
- UK collaborative randomised trial of neonatal extracorporeal membrane oxygenation. UK Collaborative ECMO Trail Group (1996) Lancet 348(9020):75–82 [PubMed]
- Upton CJ, Milner AD, Stokes GM. Upper airway patency during apnoea of prematurity. Arch Dis Child. 1992;67:419–424. doi: 10.1136/adc.67.4_spec_no.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbaniak KJ, McCowan LM, Townend KM. Risk factors for meconium-aspiration syndrome. Aust N Z J Obstet Gynaecol. 1996;36:401–406. doi: 10.1111/j.1479-828x.1996.tb02180.x. [DOI] [PubMed] [Google Scholar]
- Vain NE, Szyld EG, Prudent LM, Wiswell TE, Aguilar AM, Vivas NI. Oropharyngeal and nasopharyngeal suctioning of meconium-stained neonates before delivery of their shoulders: multicentre, randomised controlled trial. Lancet. 2004;364:597–602. doi: 10.1016/S0140-6736(04)16852-9. [DOI] [PubMed] [Google Scholar]
- van de Berg E, Lemmers PM, Toet MC, Klaessens J, van Bel F. The effect of the “InSurE” procedure on cerebral oxygenation and electrical brain activity of the preterm infant. Arch Dis Child Fetal Neonatal Ed. 2010;95(1):F53–F58. doi: 10.1136/adc.2008.156414. [DOI] [PubMed] [Google Scholar]
- van Kaam AH, Rimensberger PC. Lung-protective ventilation strategies in neonatology: what do we know – what do we need to know? Crit Care Med. 2007;35(3):925–931. doi: 10.1097/01.CCM.0000256724.70601.3A. [DOI] [PubMed] [Google Scholar]
- van Kaam AH, Lachmann RA, Herting E, De Jaegere A, van Iwaarden F, Noorduyn LA, et al. Reducing atelectasis attenuates bacterial growth and translocation in experimental pneumonia. Am J Respir Crit Care Med. 2004;169:1046–1053. doi: 10.1164/rccm.200312-1779OC. [DOI] [PubMed] [Google Scholar]
- Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics. 2000;105(6):1194–1201. doi: 10.1542/peds.105.6.1194. [DOI] [PubMed] [Google Scholar]
- Van Marter LJ, Allred EN, Leviton A, Pagano M, Parad R, Moore M. Antenatal glucocorticoid treatment does not reduce chronic lung disease among surviving preterm infants. J Pediatr. 2001;138(2):198–204. doi: 10.1067/mpd.2001.110980. [DOI] [PubMed] [Google Scholar]
- Van Meurs K. Is surfactant therapy beneficial in the treatment of the term newborn infant with congenital diaphragmatic hernia? J Pediatr. 2004;145(3):312–316. doi: 10.1016/j.jpeds.2004.04.056. [DOI] [PubMed] [Google Scholar]
- Van Meurs KP, Robbins ST, Reed VL, Karr SS, Wagner AE, Glass P, et al. Congenital diaphragmatic hernia: long-term outcome in neonates treated with extracorporeal membrane oxygenation. J Pediatr. 1993;122(6):893–899. doi: 10.1016/s0022-3476(09)90013-0. [DOI] [PubMed] [Google Scholar]
- Van Meurs KP, Wright LL, Ehrenkranz RA, Lemons JA, Ball MB, Poole WK, et al. Inhaled nitric oxide for premature infants with severe respiratory failure. N Engl J Med. 2005;353(1):13–22. doi: 10.1056/NEJMoa043927. [DOI] [PubMed] [Google Scholar]
- Vanamo K, Peltonen J, Rintala R, Lindahl H, Jaaskelainen J, Louhimo I. Chest wall and spinal deformities in adults with congenital diaphragmatic defects. J Pediatr Surg. 1996;31(6):851–854. doi: 10.1016/s0022-3468(96)90152-9. [DOI] [PubMed] [Google Scholar]
- Vanamo K, Rintala R, Sovijarvi A, Jaaskelainen J, Turpeinen M, Lindahl H, et al. Long-term pulmonary sequelae in survivors of congenital diaphragmatic defects. J Pediatr Surg. 1996;31(8):1096–1099. doi: 10.1016/s0022-3468(96)90095-0. [DOI] [PubMed] [Google Scholar]
- Vanamo K, Rintala RJ, Lindahl H, Louhimo I. Long-term gastrointestinal morbidity in patients with congenital diaphragmatic defects. J Pediatr Surg. 1996;31(4):551–554. doi: 10.1016/s0022-3468(96)90494-7. [DOI] [PubMed] [Google Scholar]
- vd Staak FH, de Haan AF, Geven WB, Doesburg WH, Festen C. Improving survival for patients with high-risk congenital diaphragmatic hernia by using extracorporeal membrane oxygenation. J Pediatr Surg. 1995;30(10):1463–1467. doi: 10.1016/0022-3468(95)90408-5. [DOI] [PubMed] [Google Scholar]
- Velaphi S, Van Kwawegen A. Meconium aspiration syndrome requiring assisted ventilation: perspective in a setting with limited resources. J Perinatol. 2008;28(Suppl 3):S36–S42. doi: 10.1038/jp.2008.155. [DOI] [PubMed] [Google Scholar]
- Veldhuizen R, Nag K, Orgeig S, Possmayer F. The role of lipids in pulmonary surfactant. Biochim Biophys Acta. 1998;1408(2–3):90–108. doi: 10.1016/s0925-4439(98)00061-1. [DOI] [PubMed] [Google Scholar]
- Verder H. Nasal CPAP has become an indispensable part of the primary treatment of newborns with respiratory distress syndrome. Acta Paediatr. 2007;96(4):482–484. doi: 10.1111/j.1651-2227.2007.00263.x. [DOI] [PubMed] [Google Scholar]
- Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrom K, et al. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicenter Study Group. N Engl J Med. 1994;331(16):1051–1055. doi: 10.1056/NEJM199410203311603. [DOI] [PubMed] [Google Scholar]
- Verder H, Albertsen P, Ebbesen F, Greisen G, Robertson B, Bertelsen A, et al. Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns of less than 30 weeks’ gestation. Pediatrics. 1999;103(2):E24. doi: 10.1542/peds.103.2.e24. [DOI] [PubMed] [Google Scholar]
- Walsh MC, Morris BH, Wrage LA, Vohr BR, Poole WK, Tyson JE, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr. 2005;146(6):798–804. doi: 10.1016/j.jpeds.2005.01.047. [DOI] [PubMed] [Google Scholar]
- Walsh-Sukys MC, Tyson JE, Wright LL, et al. Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics. 2000;105:14–20. doi: 10.1542/peds.105.1.14. [DOI] [PubMed] [Google Scholar]
- Walstab JE, Bell RJ, Reddihough DS, Brennecke SP, Bessell CK, Beischer NA. Factors identified during the neonatal period associated with risk of cerebral palsy. Aust N Z J Obstet Gynaecol. 2004;44:342–346. doi: 10.1111/j.1479-828X.2004.00249.x. [DOI] [PubMed] [Google Scholar]
- Wapner RJ, Sorokin Y, Mele L, Johnson F, Dudley DJ, Spong CY, et al. Long-term outcomes after repeat doses of antenatal corticosteroids. N Engl J Med. 2007;357(12):1190–1198. doi: 10.1056/NEJMoa071453. [DOI] [PubMed] [Google Scholar]
- Ward RM. Pharmacologic enhancement of fetal lung maturation. Clin Perinatol. 1994;21(3):523–542. [PubMed] [Google Scholar]
- Webber S, Wilkinson AR, Lindsell D, Hope PL, Dobson SR, Isaacs D. Neonatal pneumonia. Arch Dis Child. 1990;65:207–211. doi: 10.1136/adc.65.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells DA, Gillies D, Fitzgerald DA (2005) Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database Syst Rev (2):CD003645 [DOI] [PMC free article] [PubMed]
- Wen SW, Smith G, Yang Q, Walker M. Epidemiology of preterm birth and neonatal outcome. Semin Fetal Neonatal Med. 2004;9(6):429–435. doi: 10.1016/j.siny.2004.04.002. [DOI] [PubMed] [Google Scholar]
- Wessel DL, Adatia I, Van Marter LJ, et al. Improved oxygenation in a randomized trial of inhaled nitric oxide for persistent pulmonary hypertension of the newborn. Pediatrics. 1997;100:E7. doi: 10.1542/peds.100.5.e7. [DOI] [PubMed] [Google Scholar]
- West KW, Bengston K, Rescorla FJ, Engle WA, Grosfeld JL. Delayed surgical repair and ECMO improves survival in congenital diaphragmatic hernia. Ann Surg. 1992;216(4):454–460. doi: 10.1097/00000658-199210000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler KI, Davis PG, Kamlin CO, Morley CJ. Assist control volume guarantee ventilation during surfactant administration. Arch Dis Child Fetal Neonatal Ed. 2009;94(5):F336–F338. doi: 10.1136/adc.2008.149583. [DOI] [PubMed] [Google Scholar]
- Wilkinson DJ, Andersen CC, Smith K, Holberton J. Pharyngeal pressure with high-flow nasal cannulae in premature infants. J Perinatol. 2008;28(1):42–47. doi: 10.1038/sj.jp.7211879. [DOI] [PubMed] [Google Scholar]
- Wilson JM, Lund DP, Lillehei CW, Vacanti JP. Congenital diaphragmatic hernia – a tale of two cities: the Boston experience. J Pediatr Surg. 1997;32(3):401–405. doi: 10.1016/s0022-3468(97)90590-x. [DOI] [PubMed] [Google Scholar]
- Wirbelauer J, Speer CP. The role of surfactant treatment in preterm infants and term newborns with acute respiratory distress syndrome. J Perinatol. 2009;29(Suppl 2):S18–S22. doi: 10.1038/jp.2009.30. [DOI] [PubMed] [Google Scholar]
- Wiswell TE, Bent RC. Meconium staining and the meconium aspiration syndrome. Unresolved issues. Pediatr Clin North Am. 1993;40:955–981. doi: 10.1016/s0031-3955(16)38618-7. [DOI] [PubMed] [Google Scholar]
- Wiswell TE, Henley MA. Intratracheal suctioning, systemic infection, and the meconium aspiration syndrome. Pediatrics. 1992;89:203–206. [PubMed] [Google Scholar]
- Wiswell TE, Tuggle JM, Turner BS. Meconium aspiration syndrome: have we made a difference? Pediatrics. 1990;85:715–721. [PubMed] [Google Scholar]
- Wiswell TE, Foster NH, Slayter MV, Hachey WE. Management of a piglet model of the meconium aspiration syndrome with high-frequency or conventional ventilation. Am J Dis Child. 1992;146:1287–1293. doi: 10.1001/archpedi.1992.02160230045013. [DOI] [PubMed] [Google Scholar]
- Wiswell TE, Peabody SS, Davis JM, Slayter MV, Bent RC, Merritt TA. Surfactant therapy and high-frequency jet ventilation in the management of a piglet model of the meconium aspiration syndrome. Pediatr Res. 1994;36:494–500. doi: 10.1203/00006450-199410000-00015. [DOI] [PubMed] [Google Scholar]
- Wiswell TE, Graziani LJ, Kornhauser MS, Cullen J, Merton DA, McKee L, et al. High-frequency jet ventilation in the early management of respiratory distress syndrome is associated with a greater risk for adverse outcomes. Pediatrics. 1996;98(6 Pt 1):1035–1043. [PubMed] [Google Scholar]
- Wiswell TE, Gannon CM, Jacob J, et al. Delivery room management of the apparently vigorous meconium-stained neonate: results of the multicenter, international collaborative trial. Pediatrics. 2000;105:1–7. doi: 10.1542/peds.105.1.1. [DOI] [PubMed] [Google Scholar]
- Wiswell TE, Knight GR, Finer NN, et al. A multicenter, randomized, controlled trial comparing Surfaxin (Lucinactant) lavage with standard care for treatment of meconium aspiration syndrome. Pediatrics. 2002;109:1081–1087. doi: 10.1542/peds.109.6.1081. [DOI] [PubMed] [Google Scholar]
- Wiswell TE, Tin W, Ohler K. Evidence-based use of adjunctive therapies to ventilation. Clin Perinatol. 2007;34(1):191–204. doi: 10.1016/j.clp.2006.12.006. [DOI] [PubMed] [Google Scholar]
- Wood BR. Physiologic principles. In: Goldsmith JP, Karotkin EH, editors. Assisted ventilation of the neonate. 4. Philadelphia: Saunders; 2003. pp. 15–40. [Google Scholar]
- Woodhead DD, Lambert DK, Clark JM, Christensen RD. Comparing two methods of delivering high-flow gas therapy by nasal cannula following endotracheal extubation: a prospective, randomized, masked, crossover trial. J Perinatol. 2006;26(8):481–485. doi: 10.1038/sj.jp.7211543. [DOI] [PubMed] [Google Scholar]
- Wung JT, James LS, Kilchevsky E, James E. Management of infants with severe respiratory failure and persistence of the fetal circulation, without hyperventilation. Pediatrics. 1985;76(4):488–494. [PubMed] [Google Scholar]
- Wung JT, Sahni R, Moffitt ST, Lipsitz E, Stolar CJ. Congenital diaphragmatic hernia: survival treated with very delayed surgery, spontaneous respiration, and no chest tube. J Pediatr Surg. 1995;30(3):406–409. doi: 10.1016/0022-3468(95)90042-x. [DOI] [PubMed] [Google Scholar]
- Yang EY, Allmendinger N, Johnson SM, Chen C, Wilson JM, Fishman SJ. Neonatal thoracoscopic repair of congenital diaphragmatic hernia: selection criteria for successful outcome. J Pediatr Surg. 2005;40(9):1369–1375. doi: 10.1016/j.jpedsurg.2005.05.036. [DOI] [PubMed] [Google Scholar]
- Yeh TF, Harris V, Srinivasan G, Lilien L, Pyati S, Pildes RS. Roentgenographic findings in infants with meconium aspiration syndrome. JAMA. 1979;242:60–63. [PubMed] [Google Scholar]
- Yeh TF, Lilien LD, Barathi A, Pildes RS. Lung volume, dynamic lung compliance, and blood gases during the first 3 days of postnatal life in infants with meconium aspiration syndrome. Crit Care Med. 1982;10:588–592. doi: 10.1097/00003246-198209000-00006. [DOI] [PubMed] [Google Scholar]
- Yoder BA, Kirsch EA, Barth WH, Gordon MC. Changing obstetric practices associated with decreasing incidence of meconium aspiration syndrome. Obstet Gynecol. 2002;99:731–739. doi: 10.1016/s0029-7844(02)01942-7. [DOI] [PubMed] [Google Scholar]
- Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associated with nasal prong versus nasal mask during continuous positive airway pressure treatment in very low birthweight infants: a randomised control study. Arch Dis Child Fetal Neonatal Ed. 2005;90(6):F480–F483. doi: 10.1136/adc.2004.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yost CC, Soll RF (2000). Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev (2):CD001456 [DOI] [PubMed]
- Yu VY, Rolfe P. Effect of continuous positive airway pressure breathing on cardiorespiratory function in infants with respiratory distress syndrome. Acta Paediatr Scand. 1977;66(1):59–64. doi: 10.1111/j.1651-2227.1977.tb07808.x. [DOI] [PubMed] [Google Scholar]
- Yuksel B, Greenough A, Gamsu HR. Neonatal meconium aspiration syndrome and respiratory morbidity during infancy. Pediatr Pulmonol. 1993;16:358–361. doi: 10.1002/ppul.1950160607. [DOI] [PubMed] [Google Scholar]
- Zola EM, Gunkel JH, Chan RK, Lim MO, Knox I, Feldman BH, et al. Comparison of three dosing procedures for administration of bovine surfactant to neonates with respiratory distress syndrome. J Pediatr. 1993;122(3):453–459. doi: 10.1016/s0022-3476(05)83440-7. [DOI] [PubMed] [Google Scholar]