Abstract
PURPOSE
The burden of cancer is increasing globally, with poor outcomes in terms of morbidity and mortality in patients, especially in low- and middle-income countries. Lack of awareness of the risk factors, symptoms, and signs of common cancers in addition to inadequate cancer prevention programs at the community level are a major hindrance to the early detection of cancer.
METHODS
A cross-sectional study was conducted in the North East Region (NER) of India, with a sample population of 1,400 participants from Assam (n = 1,000), Meghalaya (n = 200), and Nagaland (n = 200). The questionnaire developed for the study consisted of sociodemographic profile, knowledge about cancer (oral, breast, and cervical), its warning signs, risk factors, and attitude toward cancer screening. Statistical analysis was performed using STATA version 13.0.
RESULTS
Among all the participants, 59% had heard about oral cancer, 50% about breast cancer, and 31% about cervical cancer. A limited understanding of risk factors, symptoms, and signs was reported for oral cancer (45%), breast cancer (54%), and cervical cancer (63%). A total of 34% of participants were aware of cancer screening. Among those who were aware of cancer screening, only six people had undergone any form of cancer screening, and 71% cited media as the major source of information.
CONCLUSION
The level of cancer awareness is low in the NER. A multipronged approach is needed with assistance from government and nongovernment organizations for training, providing adequate human resources and equipment, and developing cancer screening infrastructure. This needs to be coupled with mass media communication and interpersonal communication through frontline health workers.
INTRODUCTION
Cancer is the second leading cause of death, causing one in six deaths globally.1 A report from the Global Cancer Incidence, Mortality, and Prevalence database (GLOBOCAN, 2018) estimated 18.1 million new cases and 9.6 million cancer deaths worldwide in 2018.2 In India, the incidence of cancer is estimated to be 1.15 million, and deaths related to cancer are estimated to be 0.78 million in 2018. The most common cancer site among males was oral cancer (16%), and in females it was breast (28%) followed by cervical cancer (16%).2
The Indian Council of Medical Research, under its National Cancer Registry Program, reported that the rate of cancer was highest in the North East Region (NER) of India for the period of 2012-2014. It reported an age-adjusted rate (AAR) of cancer incidence of 271 cancer cases in males per 100,000 in Aizawl, Mizoram, and 249 cancer cases in females per 100,000 in Pampumpare, Arunachal Pradesh. AAR incidence of 206 per 100,000 males and 174 per 100,000 females was reported in the Kamrup district of Assam. This is much higher than the national average of 80-100 cases per 100,000 persons.3,4
The three most common cancer types in India (oral, breast, and cervical) are far more lethal in NER compared with the rest of India, primarily because of late presentation, delay in diagnosis, and subsequent treatment, which is often inadequate. This can be inferred from the fact that the 5-year survival rate of head and neck cancer in the NER is just 40%, compared with 74% for the rest of India.4
In addition to better primary health care and better-trained local doctors, knowing the causes of cancer provides a basis for understanding the potential for prevention or early detection of the disease. Older age, genetic mutations, early menarche, late pregnancy, nulliparity, late menopause, lack of physical activity, dense breasts, use of oral contraceptives, family history, and alcohol intake are risk factors for breast cancer.5 Human papillomavirus infection, smoking, use of oral contraceptives, and low immunity are risk factors for cervical cancer.6 Tobacco and alcohol consumption are major risk factors for oral cancer.7 In India, most patients with cancer present with advanced-stage disease, resulting in high mortality rates. Seventy percent of women with breast cancer present at advanced stage.8 The 5-year survival rate of patients with oral cancer decreases from 80% for those diagnosed with early-stage cancer to 20% for those diagnosed at advanced stages, underscoring the need for early detection and comprehensive treatment.9 The high mortality rate can be drastically reduced if nationwide screening programs for oral, breast, and cervical cancer are implemented for early detection.8,10 Currently, there is limited information about the public’s knowledge and understanding of common cancers and existing cancer screening programs in the NER of India.
CONTEXT
Key Objective
To determine the level of knowledge in cancer prevention; risk factors; and symptoms and signs of oral, breast, and cervical cancer in a cohort of the population eligible for cancer screening in the North East Region of India.
Knowledge Generated
The overall level of knowledge and participation in the cancer screening program amongst subjects are very low.
Relevance
The current findings provide insight into the gaps in provision of information and in the knowledge and awareness level of cancer and the cancer screening program. To address this, it is essential to create an infrastructure which includes active participation of government and nongovernment organizations; education and dissemination of information in the community; and the provision of adequate facilities and trained human resource to ensure participation in the oral, breast, and cervical cancer screening program by the population eligible for cancer screening in the North East Region in order to improve cancer outcomes.
The aim of the study is to understand public knowledge regarding oral, breast, and cervical cancer as well as cancer screening in the population of the NER. The objectives are to understand the association between sociodemographic characteristics and knowledge of the population with regard to risk factors, symptoms, signs, prevention, and screening for oral, breast and cervical cancer in the NER of India.
METHODS
Design and Settings
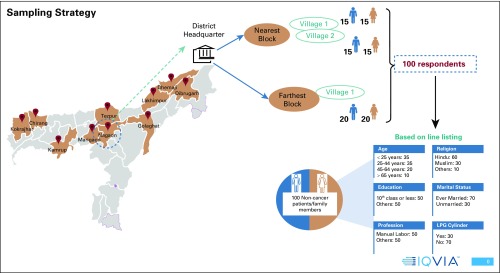
A cross-sectional study was designed across three states—Assam, Nagaland, and Meghalaya—in the NER of India. Overall, 1,400 participants were selected, with 1,000 from 10 districts of Assam, 200 from two districts of Meghalaya, and 200 from two districts of Nagaland. The participants were recruited based on the sampling plan depicted in Figure 1 and described in detail hereafter. The enrollment was through a selection of the nearest and the farthest blocks to the district headquarters as per the data available from the Government of India Census 2011. Nearest and farthest blocks were selected to ensure good representation of the population. Subsequently, two villages in the nearest block and one village in the farthest block were randomly selected from the list of villages as per data from the Government of India Census 2011. For recruiting participants for the study, line listing was carried out in the selected villages, on the basis of basic information, mainly related to age, educational status, marital status, profession, and income, as shown in Figure 1. Line listing is a process where information of each household member eligible for the study is collected. One hundred subjects who fulfilled the selection criteria were selected in each district. In each village, 30 participants from each of the two nearest blocks and 40 participants from the farthest block were interviewed for the study. The study was explained in detail to the participants, and informed consent was obtained before interviewing the participants.
FIG 1.
Sampling plan with the selection criteria for the participants to be included under community awareness and preventive survey.
Sample Size Calculation
The sample size was calculated using the equation11 N = ; with a confidence interval of 95%, with prevalence P = 50%, estimated error (D) of 6%, assuming a nonresponse rate of 25%, the total number of subjects was 1,400.
Data Collection
Questionnaire.
The questionnaire developed for the study had two sections (Data Supplement). The first section detailed the sociodemographic profile of the participants. The second section assessed the knowledge regarding risk factors, symptoms, and signs for oral, breast, and cervical cancers as well as cancer screening. The study questionnaire was adopted from the previously published literature in the Indian context on assessing the knowledge level of cancer among the population in community-based and hospital-based setting.12-17
After the design, the questionnaire was tested internally among the team members to understand its sequence, language, and time taken to conduct the interview. The pilot version was also tested in Assam among the general population (n = 35), with equal representation of sexes, across all age groups. The questionnaire was revised on the inputs received. The SurveyCTO application (Dobility, Cambridge, MA) was used to develop online and offline versions of the questionnaire tool. Android tablets running 4.0 and higher versions were used to conduct the survey. The data collectors and supervisors were trained over 3 days on the data collection process, research tools, study protocols, ethical considerations, quality assurance, and data reporting. The tool was translated into Hindi and Assamese (regional languages) and was made available in all three languages (English, Hindi, and Assamese) for the participants to choose from. The interviews were then administered by the trained data collectors in the language in which the participant was most comfortable responding.
Data analysis.
The analysis was done using STATA version 13.0. Univariate analysis was done to study the sample characteristics. Univariate and multivariate analyses were done for knowledge variables. Multivariate analysis was done to understand sociodemographic predictors of knowledge. The net bearing effect of different independent variables was explained in terms of odds ratio, with P value < .05 considered as statistically significant with a 95% CI. The dependent variables in the analysis were knowledge scores. The independent variables were age, education, economic status (on the basis of household income), and occupation.
Scoring.
Participants were asked specifically if they had ever heard about oral, breast, and cervical cancer. Those who answered in the affirmative were probed further to understand their knowledge and awareness levels. The score for overall knowledge of cancer, its prevention, and the warning symptoms and signs and risk factors of oral, breast, and cervix cancers were assessed using several predetermined statements. For every “yes” response, a score of 1 was assigned, while the remaining responses (“no/don’t know”) were assigned a score of 0. The overall knowledge of cancer and prevention was assessed by seven questions. An overall score < 4 was graded as less knowledge, and a score ≥ 4 was graded as good knowledge. The knowledge of specific cancers was assessed using predetermined statements: oral (17 questions), breast (10 questions), and cervical cancer (15 questions), respectively. Scores of < 9, < 5, and < 8 were graded as poor knowledge for oral, breast, and cervical cancers respectively.
RESULTS
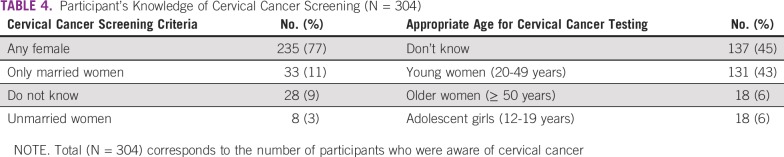
A total of 1,400 participants fulfilled the inclusion criteria and were enrolled in this study. Table 1 lists the demographic characteristics of the participants included in the survey.
TABLE 1.
Sociodemographic Characteristics of the Study Participants (N = 1,400)
Overall Knowledge of Cancer, Risk Factors, Symptoms, Signs, and Cancer Screening
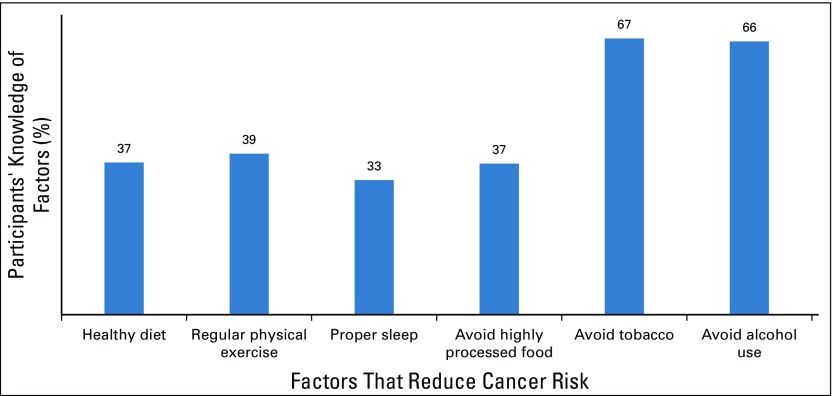
Knowledge among participants about the factors that can reduce the risk of cancer is shown in Figure 2. More than half of the participants agreed that avoiding tobacco or alcohol consumption reduces the risk of developing cancer, whereas knowledge regarding other factors was comparatively low among the study participants.
FIG 2.
Knowledge of participants on factors to reduce chances of cancer (N = 1,400).
Only 34% of the participants were aware of cancer screening. Among those who were aware of cancer screening, media was cited as the major source of information (71%). The second most common source of information was friends/relatives (47%) followed by health workers/nurses/doctors (31%). Overall, the percentage of Accredited Social Health Activist (ASHA)/Auxiliary Nurse Midwife (ANM) as a source of information for cancer screening awareness was found to be low (8%). Other sources assessed were public and social events (19%), schools/colleges (17%), and religious institutions (14%). Of all the eligible participants (n = 910) in the study, only six participants had undergone cancer screening. As per the Government of India Guidelines for screening of cancer, all people in the age group of 30 to 65 years are eligible for screening of common cancer (oral, breast, and cervical cancer).18
Knowledge of Oral, Breast, and Cervical Cancer
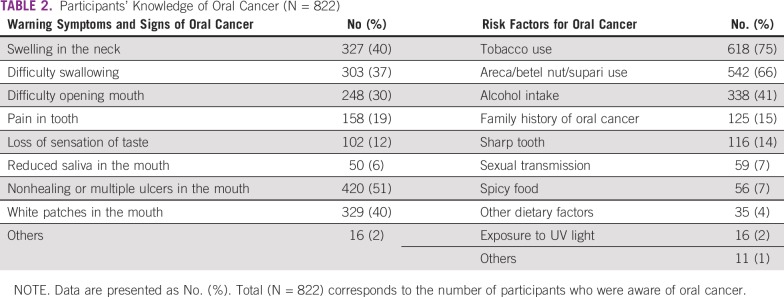
Knowledge of oral cancer.
Tobacco use was the most common risk factor cited for oral cancer (75%), followed by areca/betel nut/supari (66%) and alcohol intake (41%; Table 2). It was noted that despite oral cancer being highly prevalent in the NER, only 59% of participants had heard of mouth, tongue, or oral cancer. Knowledge of warning signs were as follows: most people (51%) described nonhealing or multiple ulcers as warning signs for oral cancer; 39% mentioned swelling in the neck, 37% mentioned difficulty in swallowing, and 30% mentioned difficulty in opening the mouth as warning signs of oral cancer.
TABLE 2.
Participants’ Knowledge of Oral Cancer (N = 822)
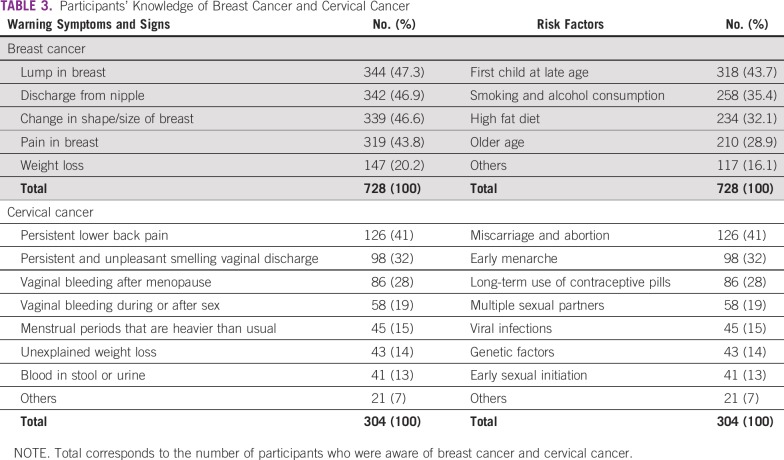
Knowledge of breast cancer.
It was observed that only half of the participants had heard about breast cancer. Out of these, knowledge about a lump in the breast (47%) followed by discharge from the nipple (47%) and change in shape and size of the breast (46%) were identified as common warning signs for breast cancer among the female participants (Table 3). Subjects stated that first child at a late age (43%) and high-fat diet (32%) were the most common risk factors for breast cancer.
TABLE 3.
Participants’ Knowledge of Breast Cancer and Cervical Cancer
Knowledge of cervical cancer.
It was found that only 21% of the participants had heard about cervical cancer. Out of these, nearly 37% cited persistent lower back pain and 35% cited persistent and unpleasant smelly vaginal discharge as warning symptoms of cervical cancer (Table 3). In this study, 41% of participants described miscarriage and abortion followed by early menarche (32%) and long-term use of contraceptive pill (28%) as risk factors for developing cervical cancer (Table 3).
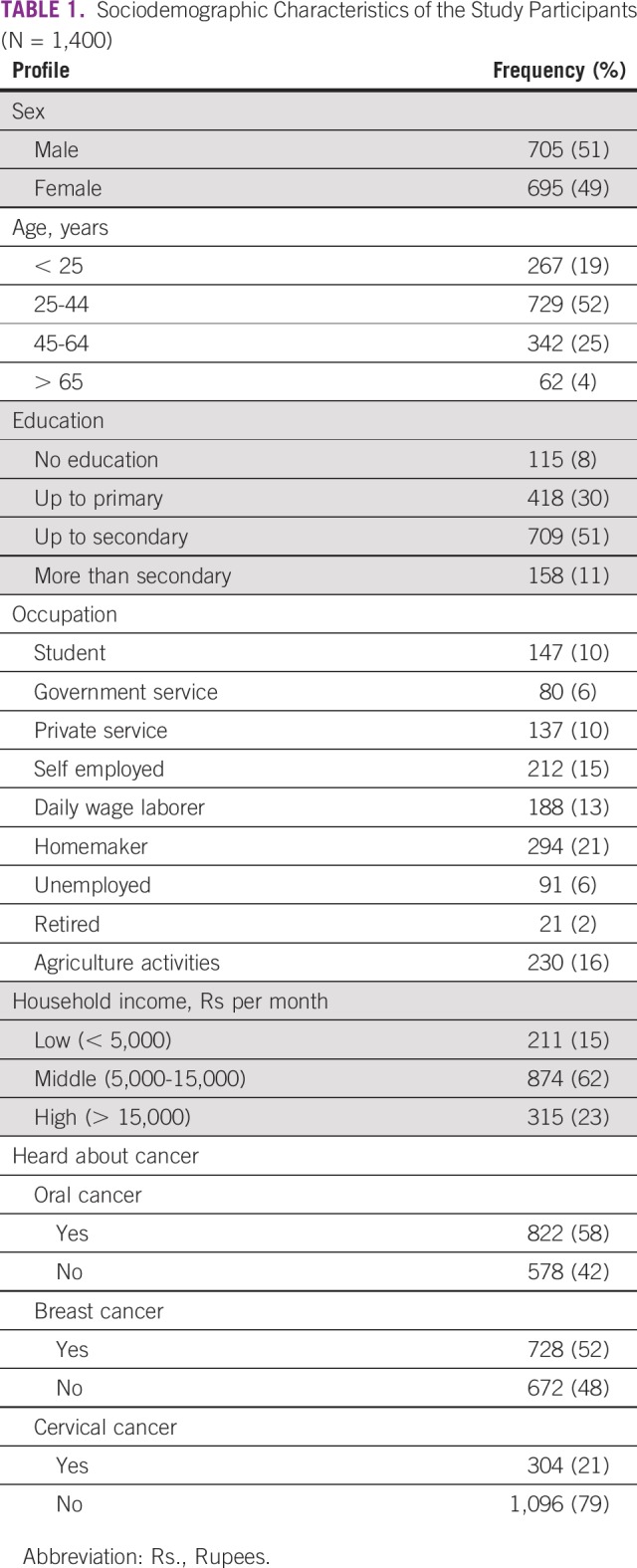
Of participants who had heard about cervical cancer, more than three-quarters (77%) were aware that any woman can get tested for cervical cancer; however, nearly 9% had no information about where to go for it. When questioned about the appropriate age for being tested for cervical cancer, 45% were unaware of this, and 43% participants mentioned 20-49 years (Table 4).
TABLE 4.
Participant’s Knowledge of Cervical Cancer Screening (N = 304)
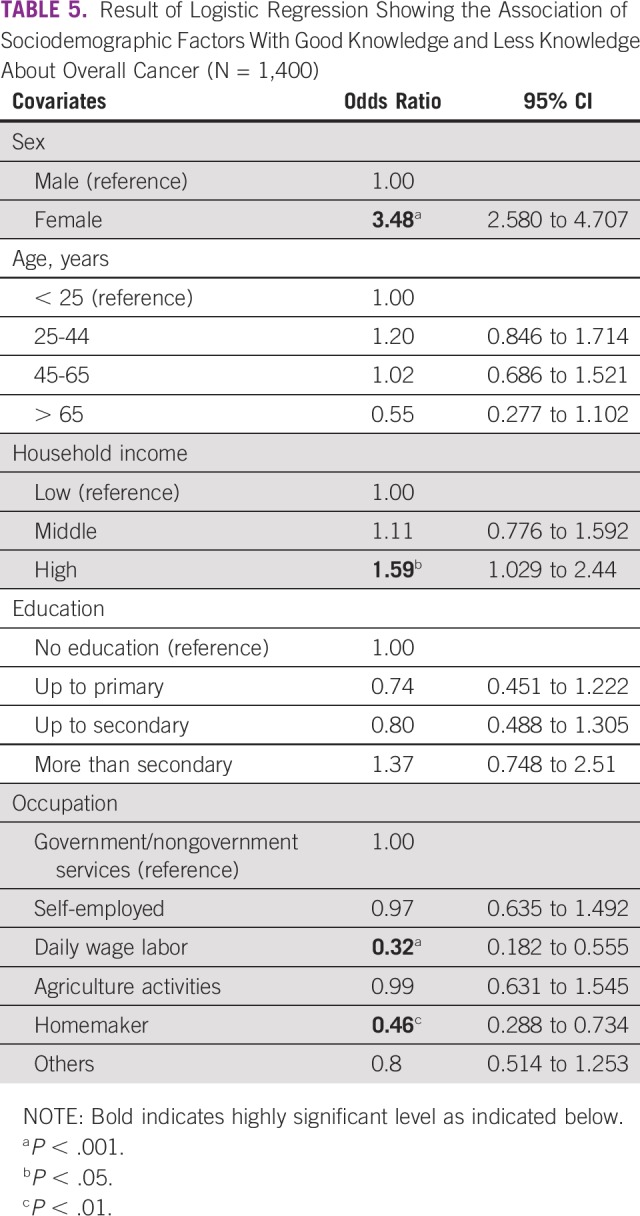
Logistic Regression Analysis
Table 5 lists the analysis of predictors of the level of knowledge among participants versus their sociodemographic characteristics. Females exhibited significantly better knowledge than males; those belonging to higher-income groups (more than Rupees 15,000 per month) showed greater knowledge compared with those belonging to lower-income groups. Of the several occupations of the participants studied, the daily wage workers and homemakers were noted to have significantly poorer knowledge.
TABLE 5.
Result of Logistic Regression Showing the Association of Sociodemographic Factors With Good Knowledge and Less Knowledge About Overall Cancer (N = 1,400)
DISCUSSION
The overall knowledge about cancer prevention, risk factors, symptoms, and signs was determined in the current study population. There were limited health communication campaigns about the importance of screening for common cancers, eligible age groups for screening, access to screening centers, and the government screening program. There was a significant correlation between the gender, education status, and income level and the knowledge and attitude toward oral, breast, and cervical cancer. The health-seeking behavior of the community and understanding of the need to undertake cancer screening among the participants was low. There could be several reasons for low participation of population in the screening program, some of which may be access to health care facilities, lack of availability of skilled manpower, and poor overall infrastructure of health facilities to conduct the screening program.
These results can be attributed to a significant lack of awareness and lack of cancer prevention programs in the NER.19 Only one-third of the population was aware of cancer screening, and the source of information was mainly mainstream media. The study highlights that there is a gap in health communication, which can be met through leveraging health workers and traditional health care professionals like doctors and nurses as a medium for information dissemination. In a country like India, where women are hesitant to freely discuss issues related to breast and cervical cancer, ASHA/ANM workers can facilitate communication, leading to potentially effective acceptance of the subject.
Engaging women in conversations around their cervical/breast health through effective interpersonal communication done by ASHA/ANMs is likely to lead to an increase in women accessing health care facilities for screening. In this study, women were found to have better knowledge regarding cancer risk factors, prevention, symptoms, and signs compared with males. This suggests that women can be an important source of generating awareness in the community and for mobilizing other women for screening and early detection. Furthermore, raising awareness about cancer prevention and screening can help reduce stigma typically associated with screening and help promote a community’s awareness of cancer prevention and health-seeking behavior.20 Personalized messaging also plays a crucial role in the prevention of developing positive health seeking among an underserved population.21,22
Participants were reasonably aware of the risk factors for oral cancer. It was mainly attributed to tobacco use, followed by areca nut and alcohol use. Despite this, the majority of people in the NER use tobacco, with the prevalence of tobacco use in Assam, Meghalaya, and Nagaland occurring in almost half of the adult population. Data from the Global Adult Tobacco Survey 2017 showed that even though the awareness level of harms from tobacco use was reported to be as high as 85% in all three states, tobacco use is high compared with the other states in India.23
Only half of the study participants had heard about breast cancer and its risk factors and symptoms, which was similar to other cross-sectional studies done in Puducherry, Maharashtra, and Gujarat in India.12-15 The strong association between increased literacy and better socioeconomic status with increased cancer awareness noted in this study was comparable to other studies conducted in Delhi and Madhya Pradesh.16,17
Only one-third of the population had heard about cervical (greva) cancer. Among those who were aware, the level of awareness was not uniform across the risk factors and warning symptoms and signs of cervical cancer. The knowledge level among participants in the study was less than that identified in a study conducted in Perambalur district, Tamil Nadu, which reported a reasonable knowledge (70%) about symptoms and signs of cervical cancer.17 Information about screening for cervical cancer, age of screening, and vaccination for prevention of cervical cancer was limited among the participants.
Only six out of the 1,400 participants (eligible for screening, n = 910) had undergone screening for oral, breast, and cervical cancer. This demonstrates the lack of knowledge and health-seeking behavior in the community. The low participation can also be attributed to the lack of infrastructure in terms of skilled manpower, equipment, and consumables as well as the fact that regular screening camps are not being conducted as part of a health care delivery system.
In a resource-constrained setting, some studies suggest an opportunistic, low-cost population-level screening with a referral system to affordable tertiary cancer centers as a strategy for primary and secondary prevention24-28 and a practical alternative to the current screening approach of mass-level population-based screening because of constraints of skilled human resources, lack of referral pathways, and poor follow-up.
Finally, the participants in this study are a good representation of the NER and therefore can be generalizable in the states of that region. The Human Development Report 2003, undertaken by Government of Assam, reported that the male population is 51.76% and the female population is 48.24%. The distribution of the population is across the state, with selection of 10 out of 33 districts. The education distribution as per the report is 64% literacy, and unemployment in the year 1999-2000 was at 9.8%.29 The study therefore provides a good baseline measure of key unmet needs for cancer control and highlights the need for targeted intervention in these communities.
One limitation of the study is the design of the questionnaire, which mainly elicited a yes or no response, with additional probing of those who answered in the affirmative. One challenge with this approach is that participants with low education and low confidence may be more likely to say they know nothing, fearing that if they say they know something they might be questioned further and might say incorrect things.
The study highlights a range of issues in the knowledge gap about oral, breast, and cervical cancer. The current baseline data provide a strong basis for developing effective communication strategies to be implemented in the northeast region of India. Furthermore, barriers in terms of social and cultural beliefs and perceptions about cancer, prevention, and screening need to be eliminated through developing comprehensive strategies of health communication and mobilizing the community to attend cancer screening at the nearest health facility.
A health communication strategy with consistent messaging, addressing a specific target group, should be designed and implemented. In terms of a health system for screening, we suggest that packaging cancer screening efforts into a comprehensive noncommunicable disease service (diabetes and hypertension) is more cost effective and increases community participation.
ACKNOWLEDGMENT
Data were collected by IMS Health (Delhi) as a part of the Tata Trusts Cancer Care Program.
AUTHOR CONTRIBUTIONS
Conception and design: Kunal Oswal, Akash Pradhan, Mahendra Avhad, Ramachandran Venkataramanan, Lakshman Sethuraman, Arnie Purushotham
Administrative support: Mahendra Avhad, Lakshman Sethuraman
Collection and assembly of data: Rishav Kanodia, Umakant Nadkar, Mahendra Avhad, Arnie Purushotham
Data analysis and interpretation: Kunal Oswal, Akash Pradhan, Umakant Nadkar, Carlo Caduff
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.World Health Organization (WHO) Global Health Observatory. Geneva: 2018. https://apps.who.int/gho/data/node.main.A908?lang=en [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Indian Council of Medical Research . Three-year report of Population Based Cancer Registries, 2009–2011. Bangalore, India: National Centre for Disease Informatics and Research/National Cancer Registry Programme; 2013. [Google Scholar]
- 4. Indian Council of Medical Research (ICMR): A report on cancer burden in north eastern states of India: National Centre for Disease Informatics and Research. http://www.ncdirindia.org/Reports_NE/NE2012_2014/Files/NE_2012_14.pdf.
- 5.Division of Cancer Prevention and Control, Centers for Disease Control and Prevention (CDC) What are the risk factors for breast cancer? 2018 https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
- 6. Mustafa M, Ajaz NA, Illzam El, et al: Risk factors for cervical cancer: Diagnosis and management. IOSR-JDMS 15:104-110, 2016. [Google Scholar]
- 7.Ram H, Sarkar J, Kumar H, et al. Oral cancer: Risk factors and molecular pathogenesis. J Maxillofac Oral Surg. 2011;10:132–137. doi: 10.1007/s12663-011-0195-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh S, Shrivastava JP, Dwivedi A. Breast cancer screening existence in India: A nonexisting reality. Indian J Med Paediatr Oncol. 2015;36:207–209. doi: 10.4103/0971-5851.171539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lingen MW, Abt E, Agrawal N, et al. Evidence-based clinical practice guideline for the evaluation of potentially malignant disorders in the oral cavity: A report of the American Dental Association. J Am Dent Assoc. 2017;148:712–727.e10. doi: 10.1016/j.adaj.2017.07.032. [DOI] [PubMed] [Google Scholar]
- 10.Bobdey S, Sathwara J, Jain A, et al. Burden of cervical cancer and role of screening in India. Indian J Med Paediatr Oncol. 2016;37:278–285. doi: 10.4103/0971-5851.195751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hulley SB, Cummings SR, Browner WS, et al. Designing Clinical Research: An Epidemiologic Approach (ed 4) Philadelphia, PA: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 12.Sharma KP, Ganguly E, Nagda D, et al. Knowledge, attitude and preventive practices of South Indian women towards breast cancer. Health Agenda. 2013;1:16–22. [Google Scholar]
- 13. Shaista A, Madhavi M, Pradeep S, et al: A study to assess knowledge, attitude of breast cancer & practice of breast self-examination in females of self help groups (SHGs) in tribal area of Raigad District. International Journal of Current Medical and Applied Sciences 11:86-93, 2016. [Google Scholar]
- 14.Siddharth R, Gupta D, Narang R, et al. Knowledge, attitude and practice about breast cancer and breast self-examination among women seeking out-patient care in a teaching hospital in central India. Indian J Cancer. 2016;53:226–229. doi: 10.4103/0019-509X.197710. [DOI] [PubMed] [Google Scholar]
- 15. Gandhi PH, Trivedi M, Ganguly P, et al: KAP Study on early diagnostic signs of risk factors for cancer. Natl J Integr Res Med 4:16-21, 2013. [Google Scholar]
- 16.Somdatta P, Baridalyne N. Awareness of breast cancer in women of an urban resettlement colony. Indian J Cancer. 2008;45:149–153. doi: 10.4103/0019-509x.44662. [DOI] [PubMed] [Google Scholar]
- 17.Varadheswari T, Dandekar HR, Sharanya T. A study on the prevalence and KAP regarding cervical cancer among women attending a tertiary care hospital in Perambalur. International Journal of Preventive Medicine Research. 2015;1:71–78. [Google Scholar]
- 18. Ministry of Health and Family Welfare, Government of India: Operational guidelines on prevention screening and control of common non communicable diseases. http://www.nhm.gov.in/images/pdf/NPCDCS.pdf.
- 19.Krishnatreya M, Kataki AC. A way forward to address the cancer burden in North-East India. Int J Health Allied Sci. 2016;5:61–62. [Google Scholar]
- 20.Sivaram S, Majumdar G, Perin D, et al. Population-based cancer screening programmes in low-income and middle-income countries: Regional consultation of the International Cancer Screening Network in India. Lancet Oncol. 2018;19:e113–e122. doi: 10.1016/S1470-2045(18)30003-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jibaja-Weiss ML, Volk RJ, Kingery P, et al. Tailored messages for breast and cervical cancer screening of low-income and minority women using medical records data. Patient Educ Couns. 2003;50:123–132. doi: 10.1016/s0738-3991(02)00119-2. [DOI] [PubMed] [Google Scholar]
- 22.Harrison RV, Janz NK, Wolfe RA, et al. Personalized targeted mailing increases mammography among long-term noncompliant medicare beneficiaries: A randomized trial. Med Care. 2003;41:375–385. doi: 10.1097/01.MLR.0000053020.30060.F2. [DOI] [PubMed] [Google Scholar]
- 23. https://www.who.int/tobacco/surveillance/survey/gats/GATS_India_2016-17_FactSheet.pdf Ministry of Health and Family Welfare: Global Adult Tobacco Survey (GATS 2), Delhi, India.
- 24.Palència L, Espelt A, Rodríguez-Sanz M, et al. Socio-economic inequalities in breast and cervical cancer screening practices in Europe: Influence of the type of screening program. Int J Epidemiol. 2010;39:757–765. doi: 10.1093/ije/dyq003. [DOI] [PubMed] [Google Scholar]
- 25.Lee HY, Park EC, Jun JK, et al. Trends in socioeconomic disparities in organized and opportunistic gastric cancer screening in Korea (2005-2009) Cancer Epidemiol Biomarkers Prev. 2010;19:1919–1926. doi: 10.1158/1055-9965.EPI-09-1308. [DOI] [PubMed] [Google Scholar]
- 26.Madlensky L, Goel V, Polzer J, et al. Assessing the evidence for organised cancer screening programmes. Eur J Cancer. 2003;39:1648–1653. doi: 10.1016/s0959-8049(03)00315-0. [DOI] [PubMed] [Google Scholar]
- 27.Mallath MK, Taylor DG, Badwe RA, et al. The growing burden of cancer in India: Epidemiology and social context. Lancet Oncol. 2014;15:e205–e212. doi: 10.1016/S1470-2045(14)70115-9. [DOI] [PubMed] [Google Scholar]
- 28. https://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report-2014 Samiei M: Health system strengthening for cancer control, in Stewart BW, Wild, CP (ed): World Cancer Report 2014.
- 29. https://www.undp.org/content/dam/india/docs/highlights_of_the_assam_full_report_2003.pdf Government of Assam: Assam Human Development Report.