Abstract
E-cigarettes have dramatically increased in popularity among youth. Coincident with expanded legalization, young adults’ use of cannabis (marijuana) has also steadily increased in recent years. Use of tobacco products can increase the chances of later cannabis initiation among youth. However, most longitudinal investigations of tobacco and cannabis use patterns have focused on tobacco cigarettes, included adolescents as opposed to young adults, and have only employed two timepoints. The current study examined prospective associations between e-cigarette and cannabis use in a large, diverse college sample assessed over four timepoints (freshman – senior year; N = 4,670). E-cigarette use and cannabis use were modelled in a four-wave cross-lagged model. The results showed significant bidirectional associations between both substances, even after controlling for time-varying levels of depressive symptoms, alcohol use, and polysubstance use, sensation seeking, demographic variables, concurrent associations and previous levels of use. Moreover, the significance of the predictive path from e-cigarette use to later cannabis use remained unchanged when we ran the same model, but restricted the sample to e-cigarette-only users (i.e., never cigarette smokers), whereas only one prospective path from cannabis to e-cigarette use was significant in this subsample. The current findings suggest that the association of e-cigarette use and cannabis use is likely bidirectional, with stronger support for the link from e-cigarette use to later cannabis use, above and beyond cigarette use. As e-cigarettes gain further hold of the tobacco product market share and cannabis legalization continues to expand, data such as these will be critical for informing regulatory decisions for e-cigarettes and cannabis, particularly involving their accessibility to youth and young adults.
Keywords: e-cigarettes, cannabis, cross-lagged model, college students
1. Introduction
Electronic cigarettes (e-cigarettes) are a broad class of products that enable users to inhale an aerosol (or “vapor”) that often contains nicotine, flavorants, and other constituents (Breland et al., 2014). E-cigarettes are one of the most polarizing issues in public health. Though e-cigarettes show some promise as a cessation aid and appear to be less harmful than combustible forms of tobacco by some metrics, there is uncertainty regarding the long-term harms of these products (National Academies of Sciences and Medicine, 2018). Moreover, e-cigarettes have become extremely popular among youth (Cullen et al., 2018), including among those who had never used tobacco products (Bunnell et al., 2015), and a growing body of evidence suggests that adolescents and young adults who use e-cigarettes are more likely to begin smoking tobacco cigarettes (Barrington-Trimis et al., 2016; Berry et al., 2019; Leventhal et al., 2015; Soneji et al., 2017; Spindle et al., 2017; Watkins et al., 2018; Wills et al., 2017).
In parallel with the rise in popularity of e-cigarettes, cannabis (marijuana) legalization has expanded across the U.S. Indeed, as of this writing, 34 U.S. states permit cannabis use for medicinal purposes while 11 states allow for non-medicinal (i.e., “recreational”) cannabis use. Beyond traditional instruments used to smoke cannabis (e.g., joints, blunts, bowls, etc.), cannabis vaporizers that are functionally similar to e-cigarettes have emerged that aerosolize cannabis plant material or concentrated cannabis extracts for user inhalation (Spindle, Bonn-Miller, & Vandrey, 2019). Notably, the recent expansion in cannabis legalization has coincided with an increase in cannabis use rates among young adults (McCance-Katz, 2018), which is concerning for myriad reasons. For instance, young adults often engage in risky cannabis-related behaviors such as driving while intoxicated and are prone to use cannabis products high in Δ−9-tetrahydrocannabinol (THC), the primary psychoactive constituent of cannabis that can foster dependence and produce other negative effects (e.g., acute impairment of cognitive functioning and motor skills; Huestis, 2007; Montoya and Weiss, 2018).
Understanding the relationship between e-cigarette use and cannabis use among young adults is key to discerning the net public health effects of each individual product and for informing decisions regarding their accessibility. Of particular importance is elucidating tobacco and cannabis associations among college students, as these individuals use cannabis at higher rates than their age-similar counterparts who are not in college (McCance-Katz, 2018). Numerous cross-sectional studies have demonstrated that young adults who use tobacco products (including e-cigarettes) are far more likely to use cannabis compared to non-tobacco users (Cohn et al., 2015; Ramo et al., 2012; Richter et al., 2004; Schauer et al., 2017). Concurrent use of cannabis and tobacco/nicotine can increase dependence and make cessation more difficult for each substance (Peters et al., 2012), and is associated with increased risk taking and greater psychosocial problems among youth, compared with the use of either substance alone (Pulvers et al., 2018). Though informative, these cross-sectional studies are unable to shed light on whether tobacco product use facilitates subsequent initiation of cannabis, or vice versa.
Several longitudinal studies have demonstrated that the use of tobacco/nicotine or cannabis increases the chances of uptake of the other substance, but the majority of these studies have focused on tobacco cigarettes (Ramo et al., 2012). Overall, the few prior longitudinal investigations of e-cigarette and cannabis use trajectories have shown that e-cigarette use predicts later initiation of cannabis (Dai et al., 2018; Silveira et al., 2018; Unger et al., 2016). For example, e-cigarette use among previously nicotine and cannabis-naïve adolescents in the Population Assessment of Tobacco and Health (PATH) survey significantly increased these individuals’ odds of having initiated cannabis use one year later (Dai et al., 2018; Silveira et al., 2018). Importantly, however, extant longitudinal e-cigarette and cannabis use studies have been limited by the inclusion of only adolescents (under age 18), examination of only 2 time points (e.g., baseline and one-year follow-up; Dai et al., 2018; Silveira et al., 2018), and in some cases, non-diverse samples (e.g., only Hispanic youth; Lozano et al., 2017; Unger et al., 2016). Assessing e-cigarette and cannabis use for more than 2 timepoints would facilitate exploration of bi-directional associations between these two substances, which ultimately could improve interventions intended to deter initiation and escalation of each substance among adolescents and young adults. Should e-cigarette use also increase risk of cannabis initiation in young adults, policies may need to be implemented to reduce e-cigarette accessibility among this age group (e.g., increasing the minimum purchasing age for all tobacco products).
The present study sought to extend prior research by examining whether e-cigarette use leads to cannabis use in a large, ethnically-diverse sample of young adult college students, followed for a total of 4 years (i.e., from their freshman to senior years). Studying transition behaviors for this length of time allows for more nuanced exploration of bi-directional associations between cannabis and nicotine than has been possible in prior studies which only included 2 assessment time points. That is, we could better determine in this study whether initiation of one product was more strongly associated with the other.
Using a complex four-wave cross-lagged model with time-dependent and time-varying covariates, our goal was to isolate the hypothesized prospective effects of e-cigarettes on cannabis and vice versa. Moreover, we also assessed whether e-cigarette use was prospectively associated with subsequent cannabis use among individuals who were not cigarette smokers in order to determine whether the use of e-cigarettes alone, as opposed to multiple tobacco products, would confer risk for later use of cannabis.
We had the following research question:
Does e-cigarette use lead to cannabis use?
We have developed the following hypotheses:
Hypothesis 1: E-cigarette use will be prospectively associated with higher cannabis use.
Hypothesis 2: E-cigarette use will be uniquely associated with higher cannabis use even when controlling for cigarette use.
2. Method
2.1. Sample
The Spit for Science (S4S) project is an ongoing, longitudinal, university-wide project at a large, urban university focused on genetic and environmental influences on college students’ substance use and behavioral health outcomes (Dick et al., 2014). S4S invites incoming students aged 18 or older to participate in an online survey at the beginning of the fall semester of their freshman year and provide a saliva sample for genotyping. Participants subsequently complete a follow-up online survey each spring while attending college. Data collection for S4S began in the fall of 2011, and five cohorts of incoming freshman students have been enrolled in the study (incoming students in 2011–2014 and 2017). Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools (Harris et al., 2009). The full S4S sample consists of over 12,000 participants assessed at baseline, with 48.70% who completed the survey in year 2, 38.62% completed the survey in year 3, and 30.25% completed the survey in year 4. The sample size for the present study was narrowed down using the following inclusion criteria: given that the baseline measure of e-cigarette use (freshman fall assessment) was only available for cohort 4, we decided to use freshman spring assessment, assessed among cohorts 3 and 4, as a baseline to maximize the number of timepoints and the available sample. In total, we used four timepoints: freshman spring (Y1), sophomore spring (Y2), junior spring (Y3), and senior spring (Y4), with time-invariant covariates assessed at baseline – freshman fall (Y0). The final analytic sample was N = 4,670 at Y1 spring. Our sample was similar to the overall university population: 49% White, 17% Black/African American, 13% Asian, 8% Hispanic, 13% other, majority female and mostly between the ages of 18–24 (U.S. Department of Education, 2018). Looking at attrition across time using logistic regression predicting completion status, we found that females were statistically significantly more likely than males to remain in the study (across all timepoints). Further, as compared to White participants, Black participants were more likely to complete (across all timepoints), Asian participants were more likely to complete at Y2, Y3, and Y4, and Hispanic were more likely to complete at Y3 and Y4.
2.2. Measures
2.1.1. E-cigarette use (assessed Y1, Y2, Y3, Y4).
Participants were first asked a question related to how many e-cigarettes they used in their lifetime with the following options: 0 = none, 1 = 1–9, 2 = 10–99, 3 = 100–200, 4 = more than 200. Then, participants who indicated ever using e-cigarettes (answers 1–4) were asked about the number of days they used e-cigarettes in the past month, with the following options: 0 = I didn’t use e-cigarettes in the past month, 1 = once or twice, 2 = a few days (3 to four days a month), 3 = a couple of days a week (5 to 11 days a month), 4 = three times a week (12 to 14 days a month), 5 = most days of the week (15 to 25 days a month), 6 = daily or almost daily (26 to 30 days a month). Because our main interest was in ever use of e-cigarettes, we decided to combine the two items (i.e., ever and past-month use) as using only the past month measure would have limited the sample to individuals with prior e-cigarette experience only, and thus filtered out never-e-cigarette users. We combined the items into a single measure in the following way: 0 = individuals who never used e-cigarettes (0 use lifetime), 1 = individuals who used e-cigarettes but not in the current month, 2 = individuals who used e-cigarettes once or twice in the past month (2 in the past month item), 3 = individuals who used e-cigarettes 3 to four days a month (3 in the past month item), 4 = individuals who used three times or more a week (4–6 in the past month item).
2.1.2. Cigarette use (assessed Y1, Y2, Y3, Y4).
Similar to the e-cigarette use measure, we computed whether participants ever used cigarettes by combining analogous item asking about lifetime cigarette use across the four waves. This was recoded into 0 = never used cigarettes across the four waves, 1 = ever used cigarettes.
2.1.3. Cannabis use (assessed Y1, Y2, Y3, Y4).
Past 12-month cannabis use was measured by asking participants whether they consumed cannabis in the past 12 months and if so, how many times they used cannabis in the past 12 months. This was recoded as 0 = never used cannabis, 1 = 1–5 times in the past 12 months, 2 = 6 or more times in the past 12 months.
2.1.4. Control variables.
2.1.4.1. Depressive symptoms (assessed Y1, Y2, Y3, Y4).
Internalizing symptoms have been found to be predictive of higher substance use in many previous studies (e.g., Dawson, Goldstein, Moss, Li, & Grant, 2010; Farmer et al., 2015). Four items asking related to experiences with depressive symptoms (Likert-type scale, range 1–5) were asked during every wave. The internal reliability was α = .84 (Y1), α = .86 (Y2), α = .87 (Y3), and α = .87 (Y4). These items are listed in Appendix A.
2.1.4.2. Polysubstance use (assessed Y1, Y2, Y3, Y4).
Previous studies suggested that e-cigarette use might be associated with higher risk for polysubstance use (Miech et al., 2015; Morean et al., 2016). An index of polysubstance use (“polysubstance use” afterwards) was created as average of response to three items, asking about the past 12 months consumption of opiods, stimulants, or cocaine, with response options 0 = never used the substance, 1 = 1–5 times in the past 12 months, 2 = 6 or more times in the past 12 months.
2.1.4.3. Alcohol use (assessed Y1, Y2, Y3, Y4).
Among young adults, alcohol use often co-occurs with cannabis (e.g., Mohler-Kuo et al., 2003; Primack et al., 2012; Simons et al., 2005), as well as tobacco use (Nichter et al., 2010; Reed et al., 2007). Alcohol use was assessed as the combination of two questions: one asking participants about the number of drinks they had in the past 30 days, and the other asking about the number of drinks they had on a typical day. Then, the number of days participants were drinking was multiplied by the number of drinks per occasion, and this was multiplied by 14 (reflecting 14 grams of ethanol per standard drink). The resulting scale reflects average alcohol consumption per month as grams of ethanol. For more detailed information about the scale, please see Salvatore et al. (2016).
2.1.4.4. Sensation seeking (assessed at baseline).
High sensation seeking has been found to be associated with higher substance use in a number of previous studies (Crawford et al., 2003; Martin et al., 2002), including e-cigarettes (Dai et al., 2018). Three sensation seeking items (Likert-type scale, range 1–4) from an abbreviated version of UPPS-P (Lynam et al., 2007) were asked during the freshman year only. The reliability was α = .63. These items are listed in Appendix A.
2.1.4.5. Ethnicity/Race (assessed at baseline).
The selected sample included the following self-reported ethnic/racial breakdown: African American = 889 (19.1%), American Indian/Alaskan Native = 27 (.6%), Asian = 789 (17.0%), Hawaiian/Pacific Islander = 28 (.6%), Hispanic/Latino = 281 (6.1%), More than one race = 316 (6.8%), Unknown = 45 (1%), White = 2,295 (49.4%). This was dummy-coded into Asian, Black, Other (collapsing American Indian/Alaskan Native, Hawaiian/Pacific Islander, Hispanic/Latino, More than one race, and Unknown) with reference group being White.
2.1.4.6. Age (assessed at baseline).
The age at baseline (M = 18.58, SD = 0.52).
2.1.4.7. Sex (assessed at baseline).
There was a total 1,730 males (37%) and 2,940 females (63%).
2.3. Data Analysis
First, descriptive statistics and zero-order correlations were computed for all variables. Then, a cross-lagged model of e-cigarette and cannabis use was estimated in a structural equation modeling framework, with use of e-cigarette or cannabis regressed on previous year’s use of e-cigarette or cannabis. Along with that, depressive symptoms, alcohol use, and polysubstance use were also modeled in a similar fashion, that is, using four-wave autoregressive model, with e-cigarette use and cannabis use regressed on previous year’s level of depressive symptoms, alcohol use, and polysubstance use (and vice versa). Furthermore, the concurrent timepoints were also allowed to covary. In effect, we estimated a 4-wave cross-lagged model for five constructs, with the main focus being the prospective cross-lagged paths between e-cigarette and cannabis use, with depressive symptoms, alcohol use and polysubstance use modelled as time-varying covariates. This model is shown in Figure 1. Regressing on previous levels of the same substance while controlling for concurrent associations with the other substance enabled evaluation of the support for cross-lagged effects, where previous levels of substance use lead to causal change in the other substance use, controlling for concurrent and previous year’s levels of depressive symptoms, alcohol use, and polysubstance use. Finally, the same cross-lagged model was estimated for the subset of participants that indicated never using cigarettes throughout four years of college.
Figure 1.
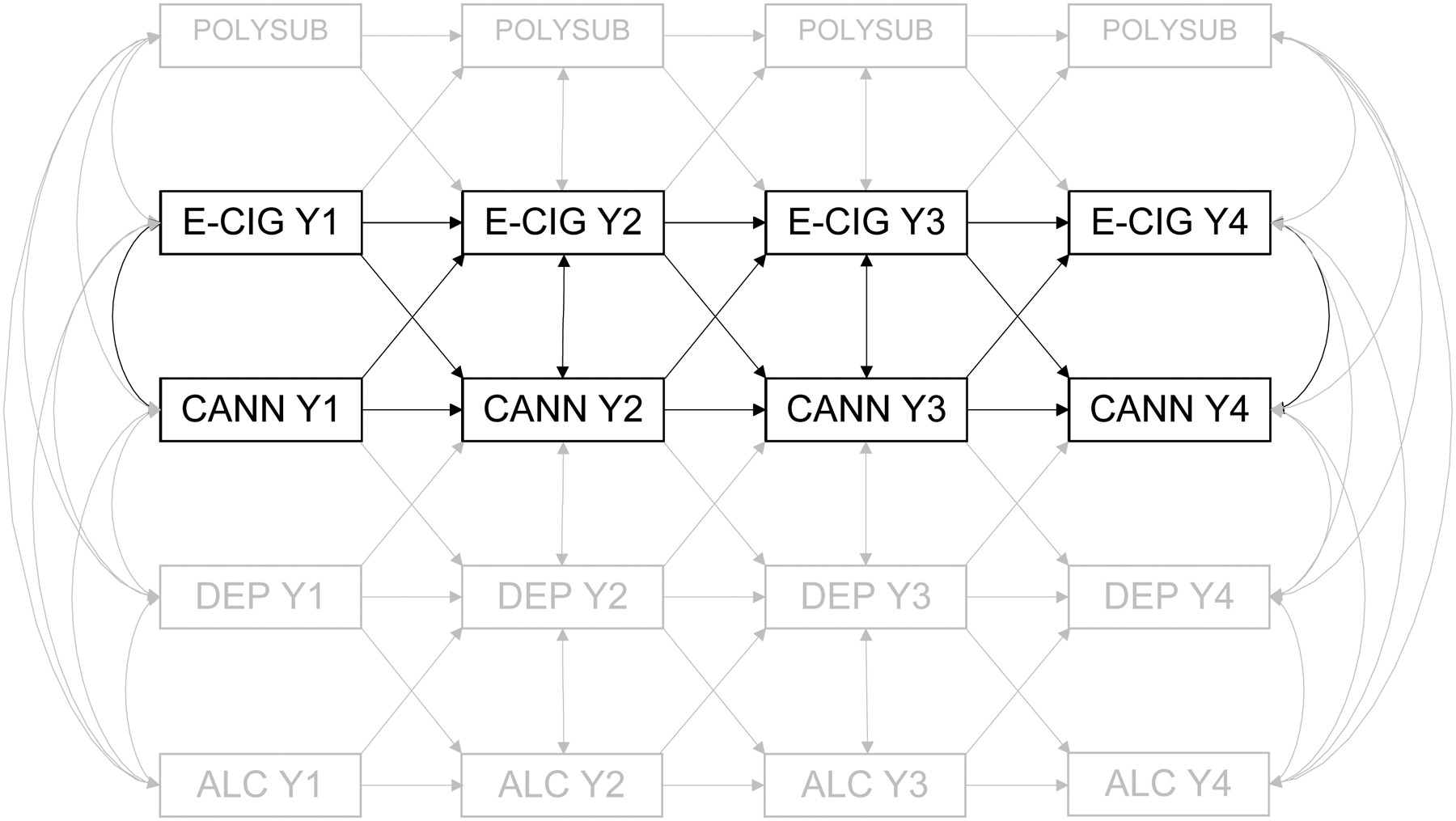
Note. Y1 = year 1, Y2 = year 2, Y3 = year 3, Y4 = year 4. POLYSUB = polysubstance use, E-CIG = e-cigarette use, CANN = cannabis use, DEP = depressive symptoms, ALC = alcohol use. For clarity, paths POLYSUB → CANN/DEP/ALC, E-CIG → DEP/ALC, CANN → POLYSUB/ALC, DEP →E-CIG/POLYSUB, and ALC → CANN/E-CIG/POLYSUB are not shown but were estimated.
All variables in the cross-lagged model were residualized on background variables (sensation seeking at baseline, age, sex, dummy-coded ethnicity variables) prior to analyses. All models were estimated in Mplus 8 (Muthén & Muthén, 1998–2017). Full information maximum likelihood (FIML) was used to handle missing data. Auxiliary variables (depressive symptoms at baseline, polysubstance use at baseline, cannabis use at baseline) were used to increase precision in estimating missing data. To handle non-normality of data and provide more robust estimates, a bootstrapping method with 5,000 resamples was used to estimate standard errors.
3. Results
Mean levels of e-cigarette use and cannabis use were largely similar across the four years, with the highest reported levels for both in the fourth year (Table 1). E-cigarette use (E-CIG) showed moderate stability across waves (rs .55 – .61). Similarly, cannabis use (CANN) showed high stability across waves (rs. .70–.73). Polysubstance use, alcohol use, and depressive symptoms showed moderate stability across time. Depressive symptoms were found to be concurrently, and, with few exceptions, prospectively associated with higher levels of e-cigarette and cannabis use. Polysubstance use and alcohol use were found to be associated with higher levels of both e-cigarette and cannabis use, concurrently and prospectively. Similarly, higher levels of sensation seeking were associated with higher levels of both substances in each wave. Women were found to show significantly lower levels of e-cigarette and cannabis use across all four timepoints.
Table 1.
Means, Standard Deviations, and Correlations of Study Variables
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. E-cig Y1 | 0.50 | 0.91 | |||||||||||||||||||||||
| 2. E-cig Y2 | 0.43 | 0.80 | .55** | ||||||||||||||||||||||
| 3. E-cig Y3 | 0.43 | 0.81 | .47** | .59** | |||||||||||||||||||||
| 4. E-cig Y4 | 0.52 | 0.93 | .46** | .52** | .61** | ||||||||||||||||||||
| 5. Cannabis Y1 | 0.71 | 0.85 | .34** | .32** | .29** | .31** | |||||||||||||||||||
| 6. Cannabis Y2 | 0.72 | 0.88 | .32** | .34** | .32** | .29** | .70** | ||||||||||||||||||
| 7. Cannabis Y3 | 0.71 | 0.87 | .32** | .34** | .32** | .31** | .63** | .73** | |||||||||||||||||
| 8. Cannabis Y4 | 0.91 | 0.89 | .28** | .28** | .29** | .36** | .54** | .64** | .75** | ||||||||||||||||
| 9. D. symptoms Y1 | 2.48 | 1.00 | .13** | .10** | .09** | .04 | .12** | .12** | .15** | .14** | |||||||||||||||
| 10. D. symptoms Y2 | 2.37 | 1.02 | .11** | .13** | .10** | .04 | .07** | .10** | .12** | .13** | .57** | ||||||||||||||
| 11. D. symptoms Y3 | 2.43 | 1.02 | .09** | .05* | .10** | .06* | .09** | .11** | .19** | .17** | .52** | .59** | |||||||||||||
| 12. D. symptoms Y4 | 2.35 | 1.00 | .09* | .05 | .11** | .11** | .08 | .10* | .12** | .17** | 1.52** | .55** | .64** | ||||||||||||
| 13. Polysub Y1 | 0.12 | 0.31 | .34** | .31** | .30** | .32** | .44** | .36** | .32** | .23** | .15** | .11** | .09** | .08* | |||||||||||
| 14. Polysub Y2 | 0.12 | 0.31 | .32** | .32** | .33** | .28** | .41** | .47** | .39** | .34** | .09** | .13** | .12** | .13** | .61** | ||||||||||
| 15. Polysub Y3 | 0.15 | 0.36 | .30** | .38** | .38** | .35** | .40** | .42** | .48** | .38** | .11** | .09** | .15** | .13** | .49** | .61** | |||||||||
| 16. Polysub Y4 | 0.20 | 0.48 | .24** | .35** | .34** | .46** | .26** | .36** | .36** | .45** | .13** | .13** | .17** | .12** | .35** | .48** | .55** | ||||||||
| 17. Alcohol Y1 | 229.5 | 517.5 | .27** | .22** | .25** | .26** | .31** | .33** | .28** | .20** | .03 | .00 | −.01 | .02 | .37** | .38** | .33** | .24** | |||||||
| 18. Alcohol Y2 | 212.4 | 446.5 | .23** | .25** | .33** | .29** | .27** | .33** | .32** | .25** | .01 | .00 | .00 | .05 | .25** | .38** | .37** | .31** | .42** | ||||||
| 19. Alcohol Y3 | 244.0 | 464.2 | .21** | .30** | .27** | .32** | .31** | .32** | .30** | .24** | .02 | −.02 | .00 | −.01 | .21** | .23** | .36** | .31** | .35** | .50** | |||||
| 20. Alcohol Y4 | 270.1 | 441.3 | .23** | .31** | .30** | .30** | .32** | .28** | .28** | .35** | .03 | .04 | .03 | .02 | .19** | .30** | .37** | .2* | .31** | .4* | .58* | ||||
| 21. Sen. Seeking Y0 | 2.84 | 0.71 | .19** | .17** | .13** | .10** | .22** | .19** | .15** | .12** | −.05* | −.05 | −.02 | −.03 | .18** | .16** | .15** | .10** | .20** | .15** | .14** | .14** | |||
| 22. Female | 0.63 | 0.48 | −.23** | −.17** | −.18** | −.24** | −.12** | −.09** | −.08** | −.03 | .10** | .11** | .09** | .13** | −.14** | −.07** | −.09** | −.03 | −.17** | −.16** | −.20** | −.15** | −.21** | ||
| 23. Age | 18.58 | 0.52 | .07** | .04* | .04 | .06* | −.04* | −.01 | −.02 | .03 | .02 | .00 | −.02 | −.02 | .02 | .02 | .03 | .05 | .04* | .01 | .08** | .02 | .06** | −.07** |
Note. M andSD are used to represent mean and standard deviation, respectively. Y1–Y4 indicate first to fourth year of data collection, Y0 = freshman baseline. D. symptoms = depressive symptoms, Polysub = polysubstance use, Alcohol = alcohol use, Sen. seeking = sensation seeking.
indicates p < .05.
indicates p < .01.
The cross-lagged model yielded an adequate fit to the data, χ2 (75) = 283.293, p < .001, CFI = .964, RMSEA = .024, 90% RMSEA CI [.022, .027]. The standardized results from the model are shown in Figure 2 as the first estimates. They showed that with the exception of Y4, e-cigarette use and cannabis use were significantly positively correlated at the same timepoint, showing that individuals who are more likely to use e-cigarettes are also more likely to use cannabis. More importantly, e-cigarette use was found to predict cannabis use one year later at two out of three timepoints (the exception being E-CIG Y2 → CANN Y3 β =.01, p = .698), above and beyond other predictors (E-CIG Y1 → CANN Y2 β = .09, p =.002, E-CIG Y3 → CANN Y4 β = .09, p = .031), showing that using e-cigarettes leads to later increased use of cannabis. Interestingly, previous levels of cannabis use were also found to predict later increased e-cigarette use (CANN Y1 → E-CIG Y2 β = .07, p = .017, CANN Y3 → E-CIG Y4 β = .09, p = .011), suggesting that the association between e-cigarette use and cannabis is bidirectional (again, with the exception of sophomore year predicting junior year levels, CANN Y2 → E-CIG Y3 β = −.01, p =.771).
Figure 2.
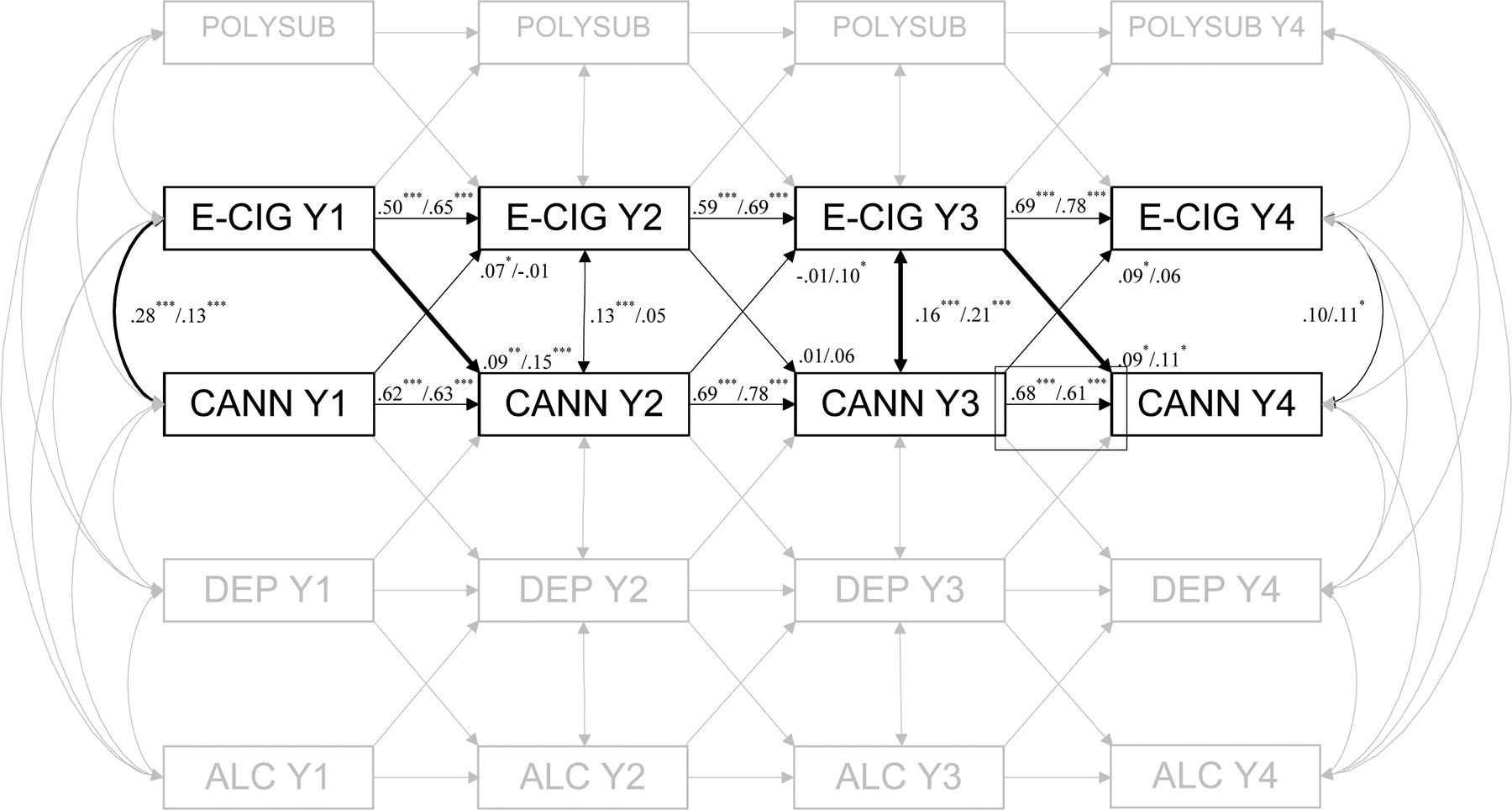
Note. Y1 = year 1, Y2 = year 2, Y3 = year 3, Y4 = year 4. POLYSUB = polysubstance use, E-CIG = e-cigarette use, CANN = cannabis use, DEP = depressive symptoms, ALC = alcohol use. * indicates p < .05. ** indicates p < .01, *** indicates p < .001. The first value refers to estimate in the full sample, the second value is estimate in the sample of non-cigarette smokers. Paths in bold reflect significant cross-substance paths in both models. For clarity, paths POLYSUB → CANN/DEP/ALC, E-CIG → DEP/ALC, CANN → POLYSUB/ALC, DEP → E-CIG/POLYSUB, and ALC → CANN/E-CIG/POLYSUB are not shown but were estimated.
Lastly, in order to evaluate whether the effect of e-cigarette use on cannabis is unique to e-cigarettes or whether it is associated with tobacco product use in general, we restricted the sample to only participants who indicated that they never used cigarettes across all four timepoints, essentially focusing on e-cigarette monousers (N = 2,380) and applied the same cross-lagged model. The results from these analyses are the second estimates in Figure 2. Interestingly, the significant predictive paths from E-CIG to later CANN remained significant and increased in size, ECIG Y1 → CANN Y2 β = .15, p <.001, ECIG Y3 → CANN Y4 β = .11, p =.042. On the other hand, both the CANN Y1 → E-CIG Y2 path (β = −.01, p = .983) and the CANN Y3 → E-CIG Y4 (β = .06, p =.199) path became statistically non-significant, whereas the CANN Y2 → E-CIG Y3 became significant (β = .10, p =.048) These results indicate that the longitudinal bidirectional association of e-cigarette use and cannabis use cannot be explained by cigarette use.
4. Discussion
The current study examined the hypotheses that e-cigarette use will be associated prospectively with higher cannabis use in college students and that this association will remain significant after controlling for cigarette use. Both of these hypotheses were supported. E-cigarette use was found to predict higher cannabis use at later time points after adjusting for the concurrent association between cannabis use and e-cigarette use. Cannabis use also predicted higher e-cigarette use at later time points after adjusting for the concurrent association between cannabis use and e-cigarette use. These associations emerged even when controlling for concurrent and preceding rates of depressive symptoms, alcohol use, and polysubstance use, as well as sensation seeking, sex, age, and race/ethnicity. Moreover, after removing subjects who used cigarettes from the sample, the paths from e-cigarette use to cannabis use (freshman to sophomore, junior to senior) remained significant, while the previously significant predictive paths from cannabis use to later e-cigarette use were non-significant in this subset. Even though the observed effects are modest in size, the complexity of the analytic model used provides strong evidence of unique associations between e-cigarettes and cannabis, especially emphasizing the link from e-cigarette to later cannabis use.
These results align with previous findings that e-cigarette use is associated prospectively with later initiation of cannabis use (Dai et al., 2018; Silveira et al., 2018; Unger et al., 2016). This previous literature is limited by the inclusion of only adolescents, analysis of only 2 time points (Dai et al., 2018; Silveira et al., 2018), and a lack of diverse samples (Lozano et al., 2017; Unger et al., 2016). We expand upon these results by demonstrating that e-cigarette use is associated prospectively with cannabis use in a diverse sample of emerging adult college students, followed across four years. Furthermore, the identification of a bi-directional association between e-cigarette use and cannabis use is a novel addition to the literature and should be examined in future analyses. The levels of e-cigarette use and cannabis use were generally quite low in the current sample, as majority of the students did not regularly use e-cigarettes or cannabis. Thus, it is possible that the observed associations would have been stronger in a sample with higher e-cigarette or cannabis use rates.
Cannabis and e-cigarette use are high-priority public health issues in emerging adult populations. Changes in the recreational legality of cannabis use are likely to lead to increases in cannabis use among emerging adults (Hall & Weier, 2015; McCance-Katz, 2018) and the prevalence of e-cigarette use in this group has increased rapidly with the advent of more novel e-cigarette products (National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health [NCCDPHP], 2016). A clear understanding of the relationship between cannabis use and e-cigarette use is critical to understanding the potential population-level harm associated with these novel trends in substance use. The bi-directional association between cannabis use and e-cigarette use suggests that the conditions that specifically increase the use of one substance have implications for the broader landscape of emerging adult substance use. The risk associated with the rising popularity of novel e-cigarette products is compounded by subsequent increases in cannabis use. Similarly, the risk associated with the legalization of recreational cannabis use is compounded by subsequent increases in e-cigarette use. The interrelationship between the use of these two substances should be considered when weighing the benefits and consequences of policies which would regulate either of them.
Although the prevalence of cigarette use has declined in recent years, this trend has been accompanied by a striking increase in the prevalence of e-cigarette use (Levy et al., 2018). As e-cigarette use becomes more common, and cigarette use less common, it will become increasingly important to differentiate the negative outcomes that are specifically associated with each behavior to better predict the consequences of these trends to public health. The prospective association between e-cigarette use and cannabis use then represents an emergent public health concern, particularly when legislative and cultural factors are poised to increase the prevalence of each behavior independently. Future research should continue to examine interrelationships between e-cigarette use and patterns of illicit substance use to better inform future efforts that may aim to regulate the distribution of these e-cigarette products.
We speculate that the observed bi-directional associations between e-cigarettes and cannabis could be caused by several factors. First, inhalation is the most common route of administration for cannabis, and cannabis vaporizers, which are similar in design and appearance to e-cigarettes, are an increasingly popular means to inhale ground cannabis or cannabis extracts (Spindle et al., 2019). Thus, when individuals start using one inhaled substance (e.g., nicotine-containing e-cigarettes), this may serve as a catalyst to trying other substances (e.g., cannabis) that can be administered through the same route and/or with a similar device. Second, co-users of cannabis and nicotine report that these two substances can have interactive effects. For example, nicotine/tobacco can purportedly intensify and extend the “high” from cannabis (Schauer et al., 2017). In addition, co-use of cannabis and nicotine produces enhanced reinforcing effects compared to those produced by either substance alone (Rabin & George, 2015). Thus, the individuals in this study may have started with one product (cannabis or e-cigarettes) and later transitioned to using the other product to experience these interactive drug effects. Lastly, use of both e-cigarettes and cannabis may be the result of young adults having a general propensity to experiment with drugs as opposed to cannabis or e-cigarettes having a direct influence on subsequent initiation of the other. Future research should consider obtaining qualitative reports from co-users of cannabis and e-cigarettes which describe their specific reasons for transitioning between these two substances in order to provide a more in-depth understanding of the longitudinal associations we detected in this study.
This study has some limitations. First, our measure of cannabis use is limited in scope and only differentiates between no use, using 1–5 times, and using 6+ times. It is possible that higher thresholds of cannabis use may be uniquely associated with negative outcomes. Another limitation of the study is the different timeframe of the e-cigarette (combination of ever use and past-month use) and the cannabis use (past 12 months). Although we believe that the differences become less salient when used in a repeated-measures longitudinal model, future studies in this area would benefit from using consistent timeframe for both measures. Furthermore, e-cigarette and cannabis use questions were non-specific in nature. It is possible that some participants might have been using e-cigarettes with marijuana in it, thus inflating the associations. However, the e-cigarette items were part of survey section related to nicotine use broadly (including cigarettes, smokeless tobacco, little cigars, etc.) and thus we believe that the placement of the item in this context implied e-cigarettes with nicotine. Nevertheless, future studies might benefit from explicitly describing e-cigarette use as inhaling aerosol with nicotine. Lastly, all measures used in this study were based on self-reports. Obtaining objective measures of use, e.g., through biomarkers of nicotine/cannabis exposure, might be an improvement in obtaining more valid measures of substance use for future studies.
The current study found support for a bi-directional association between cannabis use and e-cigarette use over time in emerging adults: cannabis use increases future e-cigarette use and e-cigarette use increases future cannabis use. However, when limiting the sample to participants who do not smoke cigarettes, there was more evidence for e-cigarette to later cannabis use link than vice versa. Recent increases in the prevalence of e-cigarette use and loosening of legal restrictions on cannabis use mark this association as an emerging public health concern. The increase in the prevalence of e-cigarette use has been met with a concurrent decrease in the prevalence of cigarette use. Shifting trends in emerging adult substance use suggest that identification of the causes and consequences of novel forms of substance use will be an important public health pursuit in the coming years.
Tested longitudinal association of e-cigarette and cannabis use
Large, diverse college sample (N = 4,670) assessed over four years
Bidirectional effects for e-cigarette and cannabis use were found
E-cigarettes showed effects on later cannabis use even among cigarette nonsmokers
Appendix A
Depressive symptoms
The next questions ask about some problems and feelings which people sometimes have. Please give the answer which best describes how much discomfort that problem has caused you during the last 30 days, including today.
| 1 | 2 | 3 | 4 | 5 | NA |
|---|---|---|---|---|---|
| Not at all | A little bit | Moderately | Quite a bit | Extremely | I choose not to answer |
Feeling blue
Worrying too much about things
Feeling no interest in things
Feeling hopeless about the future
Sensation seeking
Below are a number of statements that describe ways in which people act and think. For each statement, please indicate how much you agree or disagree with the statement.
| 1 | 2 | 3 | 4 | NA |
|---|---|---|---|---|
| Disagree strongly | Disagree a little | Agree a little | Agree strongly | I choose not to answer |
I quite enjoy taking risks.
I welcome new and exciting experiences and sensations, even if they are a little frightening and unconventional.
I would enjoy the sensation of skiing very fast down a high mountain slope.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
Dr. Eissenberg is a paid consultant in litigation against the tobacco industry and the electronic cigarette industry and is named on a patent application for a device that measures the puffing behavior of electronic cigarette users.
All remaining authors declare that there are no conflicts of interest.
References
- Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, … McConnell R (2016). E-cigarettes and future cigarette use. Pediatrics, 138, e20160379. doi: 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry KM, Fetterman JL, Benjamin EJ, Bhatnagar A, Barrington-Trimis JL, Leventhal AM, & Stokes A (2019). Association of electronic cigarette use with subsequent initiation of tobacco cigarettes in US youths. JAMA Network Open, 2, e187794–e187794. doi: 10.1001/jamanetworkopen.2018.7794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breland AB, Spindle T, Weaver M, & Eissenberg T (2014). Science and electronic cigarettes: current data, future needs. Journal of Addiction Medicine, 8, 223–233. doi: 10.1097/ADM.0000000000000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunnell RE, Agaku IT, Arrazola RA, Apelberg BJ, Caraballo RS, Corey CG, … King BA (2015). Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine & Tobacco Research, 17, 228–235. doi: 10.1093/ntr/ntu166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn A, Villanti A, Richardson A, Rath JM, Williams V, Stanton C, & Mermelstein R (2015). The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addictive Behaviors, 48, 79–88. doi: 10.1016/j.addbeh.2015.02.005 [DOI] [PubMed] [Google Scholar]
- Crawford AM, Pentz MA, Chou C-P, Li C, & Dwyer JH (2003). Parallel developmental trajectories of sensation seeking and regular substance use in adolescents. Psychology of Addictive Behaviors, 17, 179. doi: 10/d3b6tc [DOI] [PubMed] [Google Scholar]
- Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, & King BA (2018). Notes from the field: Use of electronic cigarettes and any tobacco product among middle and high school students—United States, 2011–2018. Morbidity and Mortality Weekly Report, 67, 1276–77. doi: 10.15585/mmwr.mm6745a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Catley D, Richter KP, Goggin K, & Ellerbeck EF (2018). Electronic cigarettes and future marijuana use: A longitudinal study. Pediatrics, 14, e20173787. doi: 10/gdjgdz [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Moss HB, Li T-K, & Grant BF (2010). Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: Likelihood, expression and course. Drug and Alcohol Dependence, 112, 9–17. doi: 10/b2j229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Nasim A, Edwards AC, Salvatore JE, Cho SB, Adkins A, Meyers J, Yan J, Cooke M, Clifford J, Goyal N, Halberstadt L, Ailstock K, Neale Z, Opalesky J, Hancock L, Donovan KK, Sun C, Riley B, & Kendler KS (2014). Spit for Science: Launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Frontiers in Genetics, 5, 47. doi: 10/gfv8d6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer RF, Seeley JR, Kosty DB, Gau JM, Duncan SC, Lynskey MT, & Lewinsohn PM (2015). Internalizing and externalizing psychopathology as predictors of cannabis use disorder onset during adolescence and early adulthood. Psychology of Addictive Behaviors, 29, 541–551. doi: 10/f7r583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, & Weier M (2015). Assessing the public health impacts of legalizing recreational cannabis use in the USA. Clinical Pharmacology and Therapeutics, 97(6), 607–615. doi: 10.1002/cpt.110 [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. doi: 10/cksdbv [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, Warner KE, Cummings KM, Hammond D, Kuo C, Fong GT, Thrasher JF, Goniewicz ML, & Borland R (2018). Examining the relationship of vaping to smoking initiation among US youth and young adults: A reality check. Tobacco Control, tobaccocontrol-2018–054446. doi: 10.1136/tobaccocontrol-2018-054446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano P, Barrientos-Gutierrez I, Arillo-Santillan E, Morello P, Mejia R, Sargent JD, & Thrasher JF (2017). A longitudinal study of electronic cigarette use and onset of conventional cigarette smoking and marijuana use among Mexican adolescents. Drug and Alcohol Dependence, 180, 427–430. doi: 10.1016/j.drugalcdep.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam D, Smith GT, Cyders MA, Fischer S, & Whiteside SA (2007). The UPPS-P: A multidimensional measure of risk for impulsive behavior. Unpublished Technical Report. [Google Scholar]
- Martin CA, Kelly TH, Rayens MK, Brogli BR, Brenzel A, Smith WJ, & Omar HA (2002). Sensation seeking, puberty, and nicotine, alcohol, and marijuana use in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 1495–1502. doi: 10/c2j7bh [DOI] [PubMed] [Google Scholar]
- McCance-Katz EF (2018). The National Survey on Drug Use and Health: 2017. Retrieved from https://www.samhsa.gov/data/sites/default/files/nsduh-ppt-09-2018.pdf.
- Miech RA, O’Malley PM, Johnston LD, & Patrick ME (2015). E-cigarettes and the drug use patterns of adolescents. Nicotine & Tobacco Research, 18(5), 654–659. doi: 10/f8pwdz [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohler-Kuo M, Lee JE, & Wechsler H (2003). Trends in marijuana and other illicit drug use among college students: Results from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal of American College Health, 52, 17–24. doi: 10/b4292h [DOI] [PubMed] [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, Simon P, & Krishnan-Sarin S (2016). Latent class analysis of current e-cigarette and other substance use in high school students. Drug and Alcohol Dependence, 161, 292–297. doi: 10/f8gzc6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montoya ID, & Weiss SR (2018). Cannabis Use Disorders. Cham, Switzerland: Springer. [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition Los Angeles, CA: Muthén and Muthén. [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. (2016). Patterns of E-Cigarette Use Among U.S. Youth and Young Adults. Centers for Disease Control and Prevention (US) https://www.ncbi.nlm.nih.gov/books/NBK538687/ [Google Scholar]
- Nichter M, Nichter M, Carkoglu A, & Lloyd-Richardson E (2010). Smoking and drinking among college students: “It’s a package deal.” Drug and Alcohol Dependence, 106, 16–20. doi: 10/c675z6 [DOI] [PubMed] [Google Scholar]
- Peters EN, Budney AJ, & Carroll KM (2012). Clinical correlates of co‐occurring cannabis and tobacco use: A systematic review. Addiction, 107, 1404–1417. doi: 10.1111/j.1360-0443.2012.03843.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Kim KH, Shensa A, Sidani JE, Barnett TE, & Switzer GE (2012). Tobacco, marijuana, and alcohol use in university students: A cluster analysis. Journal of American College Health, 60, 374–386. doi: 10/gdz3xp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulvers K, Ridenour C, Woodcock A, Savin MJ, Holguin G, Hamill S, & Romero DR (2018). Marijuana use among adolescent multiple tobacco product users and unique risks of dual tobacco and marijuana use. Drug and Alcohol Dependence, 189, 80–89. doi: 10.1016/j.drugalcdep.2018.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin RA, & George TP (2015). A review of co-morbid tobacco and cannabis use disorders: Possible mechanisms to explain high rates of co-use. The American Journal on Addictions, 24(2), 105–116. doi: 10/ggd6t5 [DOI] [PubMed] [Google Scholar]
- Ramo DE, Liu H, & Prochaska JJ (2012). Tobacco and marijuana use among adolescents and young adults: A systematic review of their co-use. Clinical Psychology Review, 32, 105–121. doi: 10.1016/j.cpr.2011.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed MB, Wang R, Shillington AM, Clapp JD, & Lange JE (2007). The relationship between alcohol use and cigarette smoking in a sample of undergraduate college students. Addictive Behaviors, 32, 449–464. doi: 10/cmfng2 [DOI] [PubMed] [Google Scholar]
- Richter KP, Kaur H, Resnicow K, Nazir N, Mosier MC, & Ahluwalia JS (2004). Cigarette smoking among marijuana users in the United States. Substance Abuse, 25, 35–43. doi: 10.1300/J465v25n02_06 [DOI] [PubMed] [Google Scholar]
- Salvatore JE, Thomas NS, Cho SB, Adkins A, Kendler KS, & Dick DM (2016). The role of romantic relationship status in pathways of risk for emerging adult alcohol use. Psychology of Addictive Behaviors, 30, 335–344. doi: 10/f8p263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer GL, Rosenberry ZR, & Peters EN (2017). Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addictive Behaviors, 64, 200–211. doi: 10/ggd6t6 [DOI] [PubMed] [Google Scholar]
- Silveira ML, Conway KP, Green VR, Kasza KA, Sargent JD, Borek N, … Cummings KM (2018). Longitudinal associations between youth tobacco and substance use in waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study. Drug and Alcohol Dependence, 191, 25–36. doi: 10.1016/j.drugalcdep.2018.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Correia CJ, Hansen CL, & Christopher MS (2005). An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors, 19, 326–334. doi: 10/bvfr6q [DOI] [PubMed] [Google Scholar]
- Spindle TR, Bonn-Miller MO, & Vandrey R (2019). Changing landscape of cannabis: Novel products, formulations, and methods of administration. Current Opinion in Psychology, 30, 98–102. doi: 10/gf4qrx [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindle TR, Hiler MM, Cooke ME, Eissenberg T, Kendler KS, & Dick DM (2017). Electronic cigarette use and uptake of cigarette smoking: A longitudinal examination of US college students. Addictive Behaviors, 67, 66–72. doi: 10.1016/j.addbeh.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, … Miech RA (2017). Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: A systematic review and meta-analysis. JAMA Pediatrics, 171, 788–797. doi: 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger JB, Soto DW, & Leventhal A (2016). E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug and Alcohol Dependence, 163, 261–264. doi: 10.1016/j.drugalcdep.2016.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Education. (2018). Institute of Education Sciences, National Center for Education Statistics.
- Watkins SL, Glantz SA, & Chaffee BW (2018). Association of noncigarette tobacco product use with future cigarette smoking among youth in the Population Assessment of Tobacco and Health (PATH) study, 2013–2015. JAMA Pediatrics, 172, 181–187. doi: 10.1001/jamapediatrics.2017.4173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, & Williams RJ (2017). Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tobacco Control, 26, 34–39. doi: 10.1136/tobaccocontrol-2015-052705 [DOI] [PMC free article] [PubMed] [Google Scholar]


