Using a multicenter ED visit registry, we demonstrate racial and ethnic differences in process and outcome measures of pain management for children with long-bone fractures.
Abstract
OBJECTIVES:
To test the hypotheses that minority children with long-bone fractures are less likely to (1) receive analgesics, (2) receive opioid analgesics, and (3) achieve pain reduction.
METHODS:
We performed a 3-year retrospective cross-sectional study of children <18 years old with long-bone fractures using the Pediatric Emergency Care Applied Research Network Registry (7 emergency departments). We performed bivariable and multivariable logistic regression to measure the association between patient race and ethnicity and (1) any analgesic, (2) opioid analgesic, (3) ≥2-point pain score reduction, and (4) optimal pain reduction (ie, to mild or no pain).
RESULTS:
In 21 069 visits with moderate-to-severe pain, 86.1% received an analgesic and 45.4% received opioids. Of 8533 patients with reassessment of pain, 89.2% experienced ≥2-point reduction in pain score and 62.2% experienced optimal pain reduction. In multivariable analyses, minority children, compared with non-Hispanic (NH) white children, were more likely to receive any analgesics (NH African American: adjusted odds ratio [aOR] 1.72 [95% confidence interval 1.51–1.95]; Hispanic: 1.32 [1.16–1.51]) and achieve ≥2-point reduction in pain (NH African American: 1.42 [1.14–1.76]; Hispanic: 1.38 [1.04–1.83]) but were less likely to receive opioids (NH African American: aOR 0.86 [0.77–0.95]; Hispanic: aOR 0.86 [0.76–0.96]) or achieve optimal pain reduction (NH African American: aOR 0.78 [0.67–0.90]; Hispanic: aOR 0.80 [0.67–0.95]).
CONCLUSIONS:
There are differences in process and outcome measures by race and ethnicity in the emergency department management of pain among children with long-bone fractures. Although minority children are more likely to receive analgesics and achieve ≥2-point reduction in pain, they are less likely to receive opioids and achieve optimal pain reduction.
What’s Known on This Subject:
Previous reports have revealed racial and ethnic disparities in process measures of pain management among children seeking care in emergency departments.
What This Study Adds:
We demonstrated differences in process and outcome measures of pain management by race and ethnicity. Although minority children were more likely to receive analgesics and achieve ≥2-point reduction in pain, they were less likely to receive opioids and achieve optimal pain reduction.
Pain is the most common reason for seeking emergency department (ED) care1 yet is poorly assessed and treated in the ED setting.2–4 Although the Joint Commission spurred national efforts to improve assessment and treatment of pain since 2000,5 inadequate and disparate pain management continues to remain a problem in the ED.2,6,7 Furthermore, compared with adults, children are more likely to be undertreated for pain.4,6,8,9
Racial and ethnic disparities in administration of analgesics, and specifically opioid analgesics, have been reported in the ED setting.10–16 Our investigative team has previously identified racial and ethnic differences in analgesic administration for pediatric patients presenting to the ED with acute abdominal pain.12 We have also demonstrated racial differences in opioid analgesic administration in pediatric patients diagnosed with appendicitis in the ED, even after adjustment for pain score and severity.10
Long-bone fractures are among the most common presenting complaints among children who present to the ED in acute pain.17 Racial and ethnic disparities in the ED management of pain among adults with long-bone fractures have been previously documented,15 but other studies have found no racial or ethnic differences in analgesic administration among patients treated for long-bone fractures in the ED.18–20 However, these studies were either conducted in adults,18,19 represented only single-center data,18 and/or only assessed analgesic provision rather than clinical outcomes.18,20 Therefore, we performed this multicenter study to investigate whether there are racial and ethnic differences in both process measures and clinical outcomes with respect to the management of pain in children with long-bone fractures. We hypothesized that minority children would be less likely to receive an analgesic and achieve pain reduction when compared with non-Hispanic (NH) white children.
Methods
Study Design
This was a retrospective cohort study in which we analyzed visits in the Pediatric Emergency Care Applied Research Network (PECARN) Registry21 from July 1, 2014, through June 30, 2017. The study was approved by the institutional review boards of all study sites and the data coordinating center.
Data Source and Study Population
The PECARN Registry is a validated, deidentified electronic health registry of all encounters at 7 pediatric EDs.21 Through automated processes, the registry extracts and transforms visit data from the sites’ electronic health records and harmonizes the data elements for monthly submission to the data coordinating center. The sites are geographically diverse and are composed of 4 large tertiary-care children’s hospital health systems with 4 pediatric EDs and 3 affiliated satellite pediatric EDs, representing a total of 7 separate EDs.21
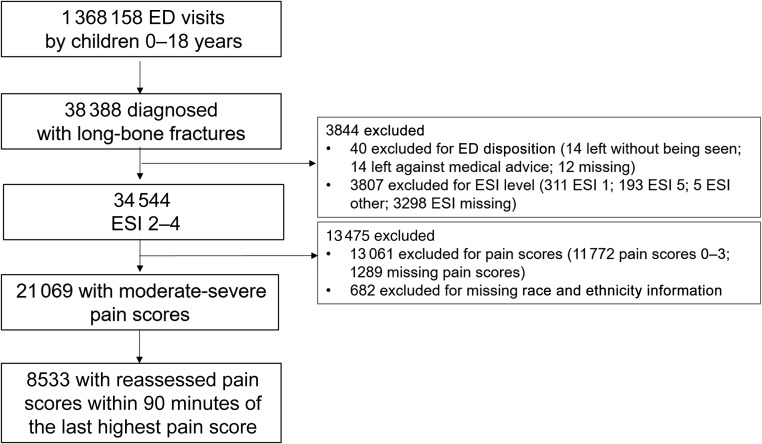
The eligible study population included all patients <18 years of age who presented to the ED with a long-bone fracture, defined as a fracture of the clavicle, humerus, ulna, radius, femur, tibia, or fibula. Visits were included if they had an International Classification of Diseases, Ninth Revision, and/or International Classification of Diseases, 10th Revision, diagnosis code for one of the aforementioned long-bone fractures or long-bone fracture identified by radiologic studies performed in the ED. For the latter, natural language processing identified patients with radiology reports indicating long-bone fractures using previously described methods.22 We excluded visits that were missing the patient’s race and ethnicity data. We excluded patient encounters during which no pain scores were documented or all documented pain scores were in the mild or no pain categories because patients with no or mild pain would not necessarily warrant analgesics for pain management. We also excluded patient encounters with an emergency severity index (ESI) level23 of 1 (critically ill) or 5 (no-urgent) and those for which ED disposition data were either missing or recorded as “left without being seen” or “left against medical advice” (Fig 1).
FIGURE 1.
Study population.
Outcomes
Outcomes included both process measures and clinical outcomes. Process measures included the following: (1) receipt of any analgesic and (2) receipt of an opioid analgesic. These included enteral and parenteral (intravenous, intramuscular, intranasal) routes of administration. Clinical outcome measures included (1) pain reduction of ≥2 points within 90 minutes of the last recorded highest pain score and (2) optimal pain reduction within 90 minutes of the maximum pain score, defined as pain reduction to mild or no pain. We used pain reduction within 90 minutes of the last recorded highest pain score as the clinical outcome measure because this is an identified quality metric in pediatric emergency medicine. This quality metric recommends reassessing and reducing pain for children with acute fractures within 90 minutes of ED arrival.24 Because we acknowledge that not all patients will experience their highest levels of pain after ED arrival, we expanded this metric to the last recorded highest reported pain score during the entire ED visit. Pain scores were recorded by using 10-point scales, including the Wong-Baker FACES Pain Rating Scale; Face, Legs, Activity, Cry, and Consolability Behavioral Scale; visual analog; and numeric rating scales. Because these scales show high levels of correlation,25,26 pain scores for each patient visit were combined into one pain score category. On a 10-point scale, pain was categorized as mild if between 1 and 3, moderate if between 4 and 6, and severe if between 7 and 10.27 At least a 2-point reduction in pain score was considered a minimally clinically significant change.28
Exposure
The primary exposure was the patient’s race and ethnicity. Consistent with other studies,10,29,30 the race and ethnicity variable was created by collapsing race and ethnicity, which are 2 discrete variables in the PECARN Registry, into 1 race and ethnicity variable. The race and ethnicity variable was categorized as NH African American, NH white, Hispanic, or other.
Potential confounding variables included patient-level characteristics, injury severity, and visit-level characteristics. Patient characteristics included age, sex, and insurance status. Markers of injury severity included triage acuity level, need for reduction as indicated by the use of procedural sedation, and location of fracture.31 Visit characteristics included year of visit, ED disposition, ED site, ED type, ED clinician, and provider type. Patient age was analyzed as a continuous variable. Insurance status was categorized as private, government (eg, Medicaid, Medicare), self-pay, or other. Triage level was categorized by using the 5-level ESI at each of the sites.23 Fracture location was categorized as upper extremity, lower extremity, or multiple trauma locations. ED disposition was categorized as admission, observation, or transfer or discharge. ED type was categorized as main pediatric ED or satellite ED. Provider type (ie, the most senior clinician of record providing care during the visit) was categorized as attending physician, multiple attending physicians, fellow, resident, or nurse practitioner (NP) or physician assistant (PA).
Statistical Analysis
We used descriptive statistics to describe our study population and measure, by race and ethnicity, proportions of (1) any analgesic provision, (2) opioid analgesic provision; (3) achievement of ≥2-point reduction in pain score within 90 minutes of the last highest recorded pain score, and (4) optimal pain reduction within 90 minutes of the maximum pain score. The eligible patient population for each analysis varied by outcome (eg, process measure versus clinical outcome measure). All patients were assessed for analgesia and opioid provision. For the pain reduction outcomes, we used the subpopulation of patients with reassessed pain scores within 90 minutes of the last highest documented pain score (Fig 1). To test for possible sample bias, we also measured whether there were any racial and ethnic differences in pain score documentation and reassessment of all children presenting to the ED with long-bone fractures. We used bivariable and multivariable logistic regression to develop unadjusted and adjusted odds ratios (aORs), respectively, to measure the strength of association of race and ethnicity with the outcome measures. Potential predictor variables for the model were predetermined on the basis of biological plausibility. As an initial screen, to provide a conservative consideration of all potentially related variables, predictors with a P value <.2 in bivariable analysis were included in our multivariable models.32 We adjusted for clustering by clinician and by site using a random-effects model with random effects for ED site and most senior clinician during the visit. To test for possible site effects, sites were dichotomized as to whether >30% of the pediatric population seeking ED care was of NH white race and ethnicity. We also explored the interaction of race and ethnicity with sites that served a higher proportion of NH white children in the multivariable model to assess whether distribution of race and ethnicity modifies the estimated differences in medication administration. This interaction was not significant and was therefore excluded from the model. Furthermore, we excluded the disposition and highest pain score covariables from the models because of collinearity with other variables. All analyses were conducted by using SAS version 9.4 (SAS Institute, Inc, Cary, NC). Full models are provided in supplemental tables.
Results
Characteristics of Study Population
There were 1 368 158 ED visits by children, of which 34 544 (2.5%) visits were for treatment of long-bone fractures with ESI levels of 2 to 4. Of these, 1289 (3.7%) encounters were excluded because they had no pain scores documented; there were no racial and ethnic differences with respect to documentation of a pain score (P value = .28). Of the 21 069 encounters with moderate-to-severe pain scores, 8533 (40.5%) had reassessed pain scores within 90 minutes of the last highest pain score. (Fig 1). There were no racial and ethnic differences with respect to reassessment of pain score (P value = .33). The median age was 10.0 (interquartile range 6.5–13.0) years, and approximately half (47.0%) of the study population was of NH white race and ethnicity (Table 1). The racial and ethnic composition across sites ranged from an NH African American proportion of 0.4% to 94.9% and a Hispanic proportion of 3.4% to 44.6% (Supplemental Table 3).
TABLE 1.
Demographics of Study Population
| Overall (N = 21 069) | NH White (n = 9910) | NH African American (n = 5416) | Hispanic (n = 3981) | Other (n = 1762) | |
|---|---|---|---|---|---|
| Age categories, n (%) | |||||
| 0 – <2 y | 746 (3.5) | 352 (3.6) | 149 (2.8) | 160 (4.0) | 85 (4.8) |
| 2 – <5 y | 2338 (11.1) | 1068 (10.8) | 493 (9.1) | 534 (13.4) | 243 (13.8) |
| 5 – <10 y | 7433 (35.3) | 3455 (34.9) | 1721 (31.8) | 1587 (39.9) | 670 (38.0) |
| 10 – <18 y | 10 552 (50.1) | 5036 (50.8) | 3053 (56.4) | 1700 (42.7) | 764 (43.4) |
| Male sex, n (%) | 13 050 (61.9) | 5931 (59.8) | 3543 (65.4) | 2525 (63.4) | 1051 (59.6) |
| Insurance status | |||||
| Private, n (%) | 9688 (46.0) | 7060 (71.2) | 1160 (21.4) | 638 (16.0) | 830 (47.1) |
| Government | 9990 (47.4) | 2494 (25.2) | 3720 (68.7) | 2965 (74.5) | 811 (46.0) |
| Self-pay | 857 (4.1) | 272 (2.7) | 253 (4.7) | 255 (6.4) | 77 (4.4) |
| Other or unknown | 534 (2.5) | 84 (0.8) | 283 (5.2) | 123 (3.1) | 44 (2.5) |
| ESI, n (%) | |||||
| ESI 2 | 4295 (20.4) | 2718 (27.4) | 694 (12.8) | 539 (13.5) | 344 (19.5) |
| ESI 3 | 9747 (46.3) | 4607 (46.5) | 2392 (44.2) | 1855 (46.6) | 893 (50.7) |
| ESI 4 | 7027 (33.4) | 2585 (26.1) | 2330 (43.0) | 1587 (39.9) | 525 (29.8) |
| Procedural sedation, n (%) | 4729 (22.4) | 2573 (26.0) | 1066 (19.7) | 675 (17.0) | 415 (23.6) |
| Injury location, n (%) | |||||
| Lower extremity only | 4777 (22.7) | 2052 (20.7) | 1558 (28.8) | 785 (19.7) | 382 (21.7) |
| Upper extremity only | 14 267 (67.7) | 6962 (70.2) | 3223 (59.5) | 2840 (71.3) | 1242 (70.5) |
| Multiple locations | 1129 (5.4) | 594 (6.0) | 272 (5.0) | 193 (4.8) | 70 (4.0) |
| Unknown | 896 (4.3) | 302 (3.0) | 363 (6.7) | 163 (4.1) | 68 (3.9) |
| Visit year, n (%) | |||||
| July 2014–June 2015 | 6524 (31.0) | 3014 (30.4) | 1726 (31.9) | 1255 (31.5) | 529 (30.0) |
| July 2015–June 2016 | 7127 (33.8) | 3348 (33.8) | 1850 (34.2) | 1325 (33.3) | 604 (34.3) |
| July 2016–June 2017 | 7418 (35.2) | 3548 (35.8) | 1840 (34.0) | 1401 (35.2) | 629 (35.7) |
| ED disposition, n (%) | |||||
| Admission, observation, or transfer | 4244 (20.1) | 2487 (25.1) | 793 (14.6) | 556 (14.0) | 408 (23.2) |
| Discharge | 16 825 (79.9) | 7423 (74.9) | 4623 (85.4) | 3425 (86.0) | 1354 (76.8) |
| ED site, n (%) | |||||
| A | 2194 (10.4) | 1478 (14.9) | 8 (0.1) | 529 (13.3) | 179 (10.2) |
| B | 1985 (9.4) | 1546 (15.6) | 146 (2.7) | 127 (3.2) | 166 (9.4) |
| C | 4390 (20.8) | 2058 (20.8) | 1595 (29.4) | 302 (7.6) | 435 (24.7) |
| D | 3871 (18.4) | 2569 (25.9) | 893 (16.5) | 133 (3.3) | 276 (15.7) |
| E | 4203 (19.9) | 1529 (15.4) | 408 (7.5) | 1875 (47.1) | 391 (22.2) |
| F | 3701 (17.6) | 724 (7.3) | 1678 (31.0) | 990 (24.9) | 309 (17.5) |
| G | 725 (3.4) | 6 (0.1) | 688 (12.7) | 25 (0.6) | 6 (0.3) |
| ED type, n (%) | |||||
| Primary | 16 165 (76.7) | 6880 (69.4) | 4574 (84.5) | 3300 (82.9) | 1411 (80.1) |
| Satellite | 4904 (23.3) | 3030 (30.6) | 842 (15.5) | 681 (17.1) | 351 (19.9) |
| Provider type, n (%) | |||||
| Attending | 13 442 (63.8) | 6449 (65.1) | 3556 (65.7) | 2337 (58.7) | 1100 (62.4) |
| Fellow | 767 (3.6) | 135 (1.4) | 383 (7.1) | 191 (4.8) | 58 (3.3) |
| Resident | 269 (1.3) | 45 (0.5) | 147 (2.7) | 54 (1.4) | 23 (1.3) |
| NP or PA | 2255 (10.7) | 1004 (10.1) | 340 (6.3) | 709 (17.8) | 202 (11.5) |
| Multiple attending | 4336 (20.6) | 2277 (23.0) | 990 (18.3) | 690 (17.3) | 379 (21.5) |
| Initial pain score, median (IQR) | 6.0 (5.0–8.0) | 6.0 (4.0–8.0) | 7.0 (5.0–9.0) | 6.0 (5.0–8.0) | 6.0 (4.0–8.0) |
| Initial pain score categories, n (%) | |||||
| No pain | 850 (4.0) | 397 (4.0) | 212 (3.9) | 155 (3.9) | 86 (4.9) |
| Mild pain, 1–3 | 1013 (4.8) | 567 (5.7) | 205 (3.8) | 141 (3.5) | 100 (5.7) |
| Moderate pain, 4–6 | 9286 (44.1) | 4797 (48.4) | 1935 (35.7) | 1741 (43.7) | 813 (46.1) |
| Severe pain, 7–10 | 9920 (47.1) | 4149 (41.9) | 3064 (56.6) | 1944 (48.8) | 763 (43.3) |
| Highest pain score, median (IQR) | 7.0 (5.0–9.0) | 6.0 (5.0–8.0) | 8.0 (6.0–10.0) | 7.0 (5.0–9.0) | 7.0 (5.0–8.0) |
| Highest pain score, n (%) | |||||
| Moderate pain, 4–6 | 9705 (46.1) | 5007 (50.5) | 2033 (37.5) | 1789 (44.9) | 876 (49.7) |
| Severe pain, 7–10 | 11 364 (53.9) | 4903 (49.5) | 3383 (62.5) | 2192 (55.1) | 886 (50.3) |
| Lowest pain score after highest pain score, median (IQR) | 2.0 (0.0–5.0) | 2.0 (0.0–4.0) | 2.0 (0.0–5.0) | 2.0 (0.0–4.0) | 2.0 (0.0–5.0) |
| Lowest pain score after highest pain score, n (%) | |||||
| No pain | 2934 (13.9) | 1648 (16.6) | 689 (12.7) | 352 (8.8) | 245 (13.9) |
| Mild pain, 1–3 | 2376 (11.3) | 1486 (15.0) | 459 (8.5) | 267 (6.7) | 164 (9.3) |
| Moderate pain, 4–6 | 2414 (11.5) | 1326 (13.4) | 579 (10.7) | 310 (7.8) | 199 (11.3) |
| Severe pain, 7–10 | 809 (3.8) | 396 (4.0) | 269 (5.0) | 87 (2.2) | 57 (3.2) |
| Not documented | 12 536 (59.5) | 5054 (51.0) | 3420 (63.1) | 2965 (74.5) | 1097 (62.3) |
IQR, interquartile range.
Process Measures
Of the 21 069 children with documented moderate-to-severe pain scores, 18 129 (86.0%) received at least 1 dose of an analgesic. After adjusting for confounding, in comparison with NH white children, minority children were more likely to receive any analgesics (NH African American: aOR 1.72 [95% confidence interval (CI) 1.51–1.95]; Hispanic: aOR 1.32 [95% CI 1.16–1.51]) (Table 2).
TABLE 2.
Management of Pain by Race and Ethnicity
| Race and Ethnicity | Process Measures | Clinical Outcomes | ||||||
|---|---|---|---|---|---|---|---|---|
| Any Analgesic | Opioid Analgesic | ≥2-Point Pain Reduction | Optimal Pain Reductiona | |||||
| % | aORb (95% CI) | % | aORb (95% CI) | % | aORb (95% CI) | % | aORb (95% CI) | |
| NH white | 84.6 | Referent | 53.2 | Referent | 88.4 | Referent | 64.8 | Referent |
| NH African American | 89.7 | 1.72 (1.51–1.95) | 39.5 | 0.86 (0.77–0.95) | 90.3 | 1.42 (1.14–1.76) | 57.2 | 0.78 (0.67–0.90) |
| Hispanic | 86.3 | 1.32 (1.16–1.51) | 36.4 | 0.86 (0.76–0.96) | 92.0 | 1.38 (1.04–1.83) | 60.4 | 0.80 (0.67–0.95) |
| Other | 85.2 | 1.06 (0.95–1.29) | 46.5 | 0.90 (0.79–1.02) | 89.5 | 1.09 (0.82–1.43) | 62.2 | 084 (0.70–1.01) |
Optimal pain reduction is defined as reduction of pain into the mild or no pain categories within 90 min of maximum pain score.
Adjusted for age, sex, insurance status, triage level, procedural sedation, fracture location, visit year, visit site, ED type, ED clinician, and provider type.
Approximately half (45.4%) of all children with moderate-to-severe pain received an opioid analgesic. After multivariable adjustment, minority children were less likely to receive an opioid analgesic (NH African American: aOR 0.86 [95% CI 0.77–0.95]; Hispanic: aOR 0.86 [95% CI 0.76–0.96]) in comparison with NH white children (Table 2).
Clinical Outcome Measures
Among the 8533 children who had documented reassessment of pain after their last highest documented pain score, 7614 (89.2%) achieved ≥2-point reduction in pain score within 90 minutes. After adjusting for confounding, in comparison with NH white children, minority children were more likely to achieve ≥2-point reduction in pain (NH African American: 1.42 [95% CI 1.14–1.76]; Hispanic: 1.38 [95% CI 1.04–1.83]) (Table 2).
With respect to optimal pain reduction, 5310 (62.2%) of visits had pain documented as mild or none within 90 minutes of the highest pain score. After multivariable adjustment, in comparison with NH white children, minority children (NH African American: aOR 0.78 [95% CI 0.67–0.90]; Hispanic: aOR 0.80 [95% CI 0.67–0.95]) were less likely to achieve optimal pain reduction (Table 2).
Discussion
In this multicenter study of children diagnosed with long-bone fractures in the pediatric ED, we found racial and ethnic disparities in both process measures and clinical outcomes of pain management. Although almost all children received some form of an analgesic, NH African American and Hispanic children were less likely to receive opioids in comparison with NH white children, even after severity adjustment. Similarly, although almost all children achieved at least a 2-point reduction in pain score within 90 minutes of highest recorded pain score, minority children were less likely to have a pain score in the mild–no pain categories in comparison with NH white children.
Our results reinforce the need for considering both process and outcome measures and adjusting for clinical severity because disparities may be missed if such a nuanced approach to investigation is not undertaken. Although we found that minority children, in comparison with NH white children, were more likely to receive analgesia, we identified that minority patients are less likely to receive opioid medications. Similarly, although we found that minority children are more likely to achieve at least a 2-point pain reduction, minority patients are more likely to continue to have persistent pain beyond the no pain to mild pain category. The reasons for these seemingly contradictory results are unclear. One explanation for the difference in opioid administration rates might be that minority children may have been less likely to receive analgesics before hospital arrival and therefore received a trial of acetaminophen or ibuprofen before receiving opioids. Unfortunately, analgesic use before ED arrival was not reliably captured. However, this postulated explanation would not explain the differences noted in lack of reduction of pain score to the mild–no pain category in minority children. A trial of early nonopioid medications should still have led to subsequent treatment to relieve pain if needed. These findings provide additional support to the notion that the elucidation of disparities in care may be nuanced; thus, it is important to critically consider the choice of outcome measures when conducting research related to health disparities and equity.
Unlike other studies in which authors have found rates of analgesia administration in EDs to range between 30% and 65%,4,6,9 we found that almost all children in this cohort with moderate-to-severe pain received some form of an analgesic.4,6 Furthermore, <5% of children with long-bone fractures in our cohort were missing documented pain scores, whereas other studies have found missing pain score documentation rates of almost 50%.6 One explanation for our findings may be attributed to our study population. We included patients who were cared for in pediatric EDs that were either located in, or affiliated with, large, urban, tertiary-care academic pediatric centers. Petrack et al4 previously reported that pediatric EDs are more likely to administer analgesics to children when compared to general or community EDs. Furthermore, our findings of higher rates of pain score documentation and analgesic administration may be a result of secular trends, as there has been increasing attention to pain management in EDs in recent years.5
Previous literature focusing on racial and ethnic differences in analgesic administration for long-bone fractures have demonstrated conflicting results. In a single-center study, Todd et al15 found that Hispanic adolescents and adults with long-bone fractures were less than half as likely as NH white patients to receive pain medication and were also less likely to receive opioids. In another study conducted at a different single-center institution, Todd et al33 demonstrated that African American adult patients with long-bone fractures were less likely to receive analgesics, and specifically opioids, when compared with their white counterparts. However, more recent studies have found no racial or ethnic associations with differences in pain management. For instance, in 2 studies of adults with long-bone fractures, there were no racial differences in analgesic administration.18,19 Using a national database, Yen et al20 also found no association of race and ethnicity with any analgesia or opioid administration among children with long-bone fractures. All of these studies are more than a decade old; thus, our results may be more reflective of current practice, including likely more judicious use of opioids as a consequence of the recent opioid epidemic. It is concerning, however, that our results demonstrate racial and ethnic differences in opioid administration. These results parallel recent reports of the management of pain for children with other conditions, such as abdominal pain and appendicitis, which have revealed lower rates of analgesia and opioid administration in minority patients, even after severity adjustment.10,12
Unique to our study is that in addition to analgesic administration, we also assessed clinical outcomes of pain reduction. Although almost all children achieved at least a 2-point reduction in pain within 90 minutes after the highest recorded pain score, minority patients were less likely to report optimal pain reduction (eg, reduction to mild or no pain). This may be attributed to lower rates of opioid administration among minority children. Thus, these results suggest that although the administration of analgesics may have improved over time, undertreatment of pain is still a concern among minority children.
Our findings contribute to the body of literature that demonstrates racial and ethnic disparities in health care. The fact that these findings are demonstrated in the ED setting is particularly concerning because the ED often functions as a safety net for underserved communities. Minority patients are generally more likely to be underinsured and less likely to have access to primary care,34 and EDs disproportionately care for these groups. Thus, it is concerning that our results suggest differential treatment of children associated with their race and ethnicity. Although it was beyond the scope of this study to explore the causes for these disparities, factors such as patient, clinician, and health system characteristics have all been suggested as both individual and interrelated factors that may contribute to racial and ethnic disparities in health care.35 Despite increased attention to the ED management of pain in recent years, with resultant quality improvement initiatives to improve pain score documentation and response to pain, racial and ethnic disparities continue to persist.
There are some important limitations to consider in this study. First, there is the possibility for selection bias with respect to cohort identification. However, we used both International Classification of Diseases codes and natural language processing of radiology reports, and it would be unlikely that such identification would differ by race and ethnicity. Second, it is possible that patients of different racial and ethnic groups differentially declined analgesics. Data regarding patient refusal of pain medication are not systematically collected in the electronic health record. Therefore, we cannot determine the effects that these may have had on our study results. Third, reassessments of pain were not documented in the entire study population. However, it is reassuring that there were no racial and ethnic differences in reassessment of pain score. Therefore, we believe that the impact of this potential ascertainment bias is minimal. Fourth, although this study was conducted across 7 pediatric EDs, these results may not be generalizable to all pediatric EDs or general EDs, potentially limiting the external validity of this study. However, on the basis of previous data, our findings may be even more pronounced at nonpediatric EDs where lower rates of analgesic administration have been found among general or nonpediatric EDs.4 Fifth, patients may be misclassified by race and ethnicity because some sites have patients self-identify race and ethnicity, whereas others assign race and ethnicity on the basis of other mechanisms, such as the perception of the registration staff. However, given that the goal of this study was to understand how race and ethnicity may affect clinical care, perceived race and ethnicity may be a better indicator than self-reported race and ethnicity; thus, the results may be minimally impacted by this potential misclassification bias. Finally, we did not evaluate medications administered before the ED visit. It is possible that this potential selection bias may have affected some of our findings, especially if there were differential rates of pretreatment across racial and ethnic groups.
Conclusions
We observed racial and ethnic differences in both the management and clinical outcomes of pain among children with long-bone fractures across 7 pediatric EDs. Although minority children were more likely to receive analgesics and achieve ≥2-point reduction in pain, even after severity adjustment, minority children were less likely to receive opioids and achieve optimal pain reduction. Further investigation is warranted to explore the reasons for such racial and ethnic disparities and to standardize care so that all children receive optimal pain treatment.
Glossary
- aOR
adjusted odds ratio
- CI
confidence interval
- ED
emergency department
- ESI
emergency severity index
- NH
non-Hispanic
- NP
nurse practitioner
- PA
physician assistant
- PECARN
Pediatric Emergency Care Applied Research Network
Footnotes
Dr Goyal conceptualized and designed the study and drafted the initial manuscript; Drs Johnson, Drendal, and Lorch helped conceptualize and design the study and reviewed and revised the manuscript; Drs Alpern, Chamberlain, and Cook helped conceptualize and design the study, coordinated and supervised data collection, and reviewed and revised the manuscript; Mr Webb performed data analysis and reviewed and revised the manuscript; Drs Alessandrini, Bajaj, and Grundmeier coordinated and supervised data collection and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institute of Minority Health and Disparities grant R03MD011654 to Dr Goyal and Agency for Healthcare Research and Quality grant R01HS020270 to Dr Alpern. The Pediatric Emergency Care Applied Research Network infrastructure was supported by the Health Resources and Services Administration, Maternal and Child Health Bureau, and Emergency Medical Services for Children Network Development Demonstration Program under cooperative agreements U03MC00008, U03MC00001, U03MC00003, U03MC00006, U03MC00007, U03MC22684, and U03MC22685. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of nor should any endorsements be inferred by the Health Resources and Services Administration, US Department of Health and Human Services, or US Government. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-0512.
References
- 1.Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20(3):165–169 [DOI] [PubMed] [Google Scholar]
- 2.Todd KH, Ducharme J, Choiniere M, et al. ; PEMI Study Group . Pain in the emergency department: results of the Pain and Emergency Medicine Initiative (PEMI) multicenter study. J Pain. 2007;8(6):460–466 [DOI] [PubMed] [Google Scholar]
- 3.Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med. 1989;7(6):620–623 [DOI] [PubMed] [Google Scholar]
- 4.Petrack EM, Christopher NC, Kriwinsky J. Pain management in the emergency department: patterns of analgesic utilization. Pediatrics. 1997;99(5):711–714 [DOI] [PubMed] [Google Scholar]
- 5.Phillips DM; Joint Commission on Accreditation of Healthcare Organizations . JCAHO pain management standards are unveiled. JAMA. 2000;284(4):428–429 [DOI] [PubMed] [Google Scholar]
- 6.Brown JC, Klein EJ, Lewis CW, Johnston BD, Cummings P. Emergency department analgesia for fracture pain. Ann Emerg Med. 2003;42(2):197–205 [DOI] [PubMed] [Google Scholar]
- 7.Drendel AL, Brousseau DC, Gorelick MH. Pain assessment for pediatric patients in the emergency department. Pediatrics. 2006;117(5):1511–1518 [DOI] [PubMed] [Google Scholar]
- 8.Furyk J, Sumner M. Pain score documentation and analgesia: a comparison of children and adults with appendicitis. Emerg Med Australas. 2008;20(6):482–487 [DOI] [PubMed] [Google Scholar]
- 9.Selbst SM, Clark M. Analgesic use in the emergency department. Ann Emerg Med. 1990;19(9):1010–1013 [DOI] [PubMed] [Google Scholar]
- 10.Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr. 2015;169(11):996–1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hostetler MA, Auinger P, Szilagyi PG. Parenteral analgesic and sedative use among ED patients in the United States: combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. Am J Emerg Med. 2002;20(3):139–143 [DOI] [PubMed] [Google Scholar]
- 12.Johnson TJ, Weaver MD, Borrero S, et al. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics. 2013;132(4). Available at: www.pediatrics.org/cgi/content/full/132/4/e851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78 [DOI] [PubMed] [Google Scholar]
- 14.Mills AM, Shofer FS, Boulis AK, Holena DN, Abbuhl SB. Racial disparity in analgesic treatment for ED patients with abdominal or back pain. Am J Emerg Med. 2011;29(7):752–756 [DOI] [PubMed] [Google Scholar]
- 15.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269(12):1537–1539 [PubMed] [Google Scholar]
- 16.Kipping EM, Chamberlain JM. The complex association of race/ethnicity with pain treatment quality in an urban medical center with 2 pediatric emergency departments. Pediatr Emerg Care. 2019;35(12):815–820 [DOI] [PubMed] [Google Scholar]
- 17.Burt CW, Fingerhut LA. Injury visits to hospital emergency departments: United States, 1992–95. Vital Health Stat 13. 1998;13(131):1–76 [PubMed] [Google Scholar]
- 18.Fuentes EF, Kohn MA, Neighbor ML. Lack of association between patient ethnicity or race and fracture analgesia. Acad Emerg Med. 2002;9(9):910–915 [DOI] [PubMed] [Google Scholar]
- 19.Bijur P, Bérard A, Nestor J, Calderon Y, Davitt M, Gallagher EJ. No racial or ethnic disparity in treatment of long-bone fractures. Am J Emerg Med. 2008;26(3):270–274 [DOI] [PubMed] [Google Scholar]
- 20.Yen K, Kim M, Stremski ES, Gorelick MH. Effect of ethnicity and race on the use of pain medications in children with long bone fractures in the emergency department. Ann Emerg Med. 2003;42(1):41–47 [DOI] [PubMed] [Google Scholar]
- 21.Deakyne SJD, Grundmeier RW, Campos DA, et al. ; Pediatric Emergency Care Applied Research Network . The Pediatric Emergency Care Applied Research Network Registry: a multicenter electronic health record registry of pediatric emergency care. Appl Clin Inform. 2018;9(2):366–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grundmeier RW, Masino AJ, Casper TC, et al. ; Pediatric Emergency Care Applied Research Network . Identification of long bone fractures in radiology reports using natural language processing to support healthcare quality improvement. Appl Clin Inform. 2016;7(4):1051–1068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gillboy NTT, Travers D, Rosenau AM. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook 2012 Edition. Rockville, MD: Agency for Healthcare Research and Quality; 2011 [Google Scholar]
- 24.Emergency Medical Services for Children Emergency department pediatric performance measures toolkit. Available at: https://emscimprovement.center/education-and-resources/toolkits/emergency-department-pediatric-performance-measures-toolbox/. Accessed March 4, 2019
- 25.Castarlenas E, Jensen MP, von Baeyer CL, Miró J. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents: a systematic review. Clin J Pain. 2017;33(4):376–383 [DOI] [PubMed] [Google Scholar]
- 26.Tomlinson D, von Baeyer CL, Stinson JN, Sung L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics. 2010;126(5). Available at: www.pediatrics.org/cgi/content/full/126/5/e1168 [DOI] [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services Acute Pain Management: Operative or Medical Procedures and Trauma. Clinical Practice Guideline No 1. Washington, DC: US Department of Health and Human Services; 1992 [Google Scholar]
- 28.Tsze DS, Hirschfeld G, von Baeyer CL, Suarez LE, Dayan PS. Changes in pain score associated with clinically meaningful outcomes in children with acute pain. Acad Emerg Med. 2019;26(9):1002–1013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Institute of Medicine Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 30.Goyal MK, Johnson TJ, Chamberlain JM, et al. ; Pediatric Care Applied Research Network (PECARN) . Racial and ethnic differences in antibiotic use for viral illness in emergency departments. Pediatrics. 2017;140(4):e20170203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dong L, Donaldson A, Metzger R, Keenan H. Analgesic administration in the emergency department for children requiring hospitalization for long-bone fracture. Pediatr Emerg Care. 2012;28(2):109–114 [DOI] [PubMed] [Google Scholar]
- 32.Hosmer DWLS, Sturdivant RX. Applied Logistic Regression, 3rd ed Hoboken, NJ: John Wiley & Sons; 2013 [Google Scholar]
- 33.Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11–16 [DOI] [PubMed] [Google Scholar]
- 34.Kirby JB, Taliaferro G, Zuvekas SH. Explaining racial and ethnic disparities in health care. Med Care. 2006;44(5 s uppl):I64–I72 [DOI] [PubMed] [Google Scholar]
- 35.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113–2121 [DOI] [PMC free article] [PubMed] [Google Scholar]