Clinical Implications.
-
•
Patients with asthma and chronic obstructive pulmonary disease are advised to closely adhere to their prescribed inhaler medication therapy due to the coronavirus disease 2019 pandemic. Using electronic medication data, we examined controller medication use and found positive increases in medication adherence.
The appropriate use of adherence to daily controller medications is important for patients with respiratory illnesses during the coronavirus disease 2019 (COVID-19) pandemic.1 The recommended use of daily controller therapy for asthma and chronic obstructive pulmonary disease (COPD) has been associated with improved disease outcomes and decreased risk of respiratory exacerbations.1, 2, 3 Increased adherence to daily medications is multifactorial and during the present pandemic may be driven by a patient's concern of his or her respiratory symptoms being associated or confused with COVID-19. Patients with well-managed symptoms are also less likely to seek acute respiratory care at health care facilities and emergency departments, which decreases the risk of incidental exposure to SARS-CoV-2 and allows health care providers to focus attention on patients with other critical needs.1
To understand how patients with asthma and COPD were responding to the recommendation of respiratory societies to follow daily medication regimens during the COVID-19 pandemic, we analyzed patient adherence to controller medication. Data were collected from Propeller Health (Madison, WI), a digital platform that tracks inhaler use through electronic medication monitors and sends alerts to patients for missed doses. This analysis was determined to be exempt by the Copernicus IRB (PRH1-18-132).
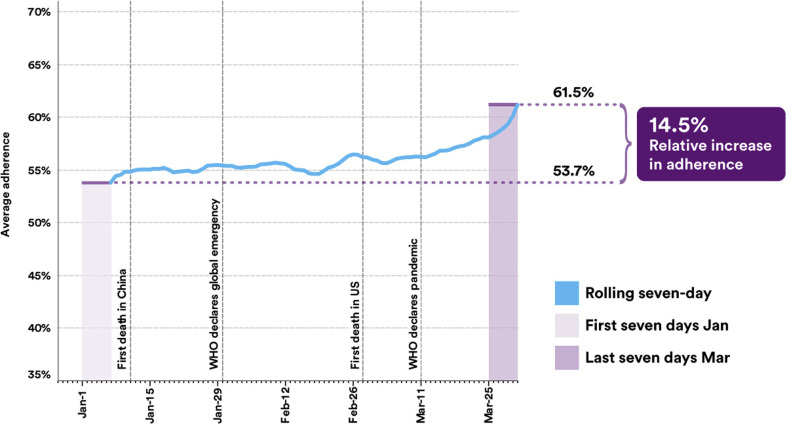
We analyzed adherence to controller inhaler use for 7578 patients (77% asthma, 67% females) with a median (interquartile range) age of 40.0 (26.0-55.0) years. From the first 7 days of January 2020 to the last 7 days of March 2020, there was a 14.5% increase (53.7% to 61.5%) in mean daily controller medication adherence, previously defined4 (Figure 1 ). We noted similar increases in adherence across age groups with older patients having higher levels of adherence. When adjusted for age, there were no clinically meaningful differences in adherence for patients with asthma or COPD. In addition, during the last week of March, over 53% of patients achieved ≥75% adherence to controller medications, a 14.9% increase from the first week of January. We have previously reported changes in adherence by month.5 In children, 4-17 years of age, there is a peak noted in September-October that has been temporally associated with seasonal rhinovirus6 and in adults a peak noted in November-February with both age groups showing a decline in adherence in March and April.5
Figure 1.
Mean daily controller adherence in asthma and chronic obstructive pulmonary disease before and during the coronavirus disease 2019 pandemic.
Although we cannot definitively state the cause of the improvement in adherence, the trend may be reflective of patients responding to national COVID-19 guidelines7 and to patient concern about controlling their primary respiratory illness with their controller medications. Furthermore, patients with asthma and COPD who track their adherence to their controller medications may be more motivated and achieve higher use of these medicines, and therefore the findings may not be generalizable to all patients.8 Future analyses should also explore if medication adherence changed during other recent pandemics like H1N1. This initial evidence on adherence is encouraging during the first weeks of COVID-19 and hopefully will have a positive effect on improving control of asthma and COPD and minimize the need for acute care for their primary respiratory disease.
Footnotes
This study was funded by Propeller Health, Madison, WI, an affiliate of ResMed.
Conflicts of interest: B. Theye, I. Smeenk, and D. A. Stempel are paid employees of Propeller Health, and L. Kaye, R. Gondalia, and M. A. Barrett are paid employees of ResMed.
References
- 1.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E.W.Y. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bengtson L.G., DePietro M., McPheeters J., Fox K.M. Real-world outcomes in patients with chronic obstructive pulmonary disease initiating long-acting mono bronchodilator therapy. Ther Adv Respir Dis. 2018;12 doi: 10.1177/1753466618772750. 1753466618772750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Engelkes M., Janssens H.M., de Jongste J.C., Sturkenboom M.C., Verhamme K.M. Medication adherence and the risk of severe asthma exacerbations: a systematic review. Eur Respir J. 2015;45:396–407. doi: 10.1183/09031936.00075614. [DOI] [PubMed] [Google Scholar]
- 4.De Keyser H.E., Kaye L., Anderson W.C., Gondalia R., Theye B., Szefler S.J. Electronic medication monitors help determine adherence subgroups in asthma. Resp Med. 2020;164:105914. doi: 10.1016/j.rmed.2020.105914. [DOI] [PubMed] [Google Scholar]
- 5.Kaye L., Hoch H., Szefler S.J., Anderson W., Barrett M., Van Sickle D. Real-life patterns of asthma controller use vary by age, time of day and season. J Allergy Clin Immunol. 2018;141:AB61. [Google Scholar]
- 6.Sears M.R., Johnston N.W. Understanding the September asthma epidemic. J Allergy Clin Immunol. 2007;120:526–529. doi: 10.1016/j.jaci.2007.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) Situation Summary. https://www.cdc.gov/coronavirus/2019-ncov/index.html Available from: Accessed April 2, 2020.
- 8.Blakey J.D., Bender B.G., Dima A.L., Weinman J., Safioti G., Costello R.W. Digital technologies and adherence in respiratory diseases: the road ahead. Eur Respir J. 2018;52:1801147. doi: 10.1183/13993003.01147-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]