To the Editor:
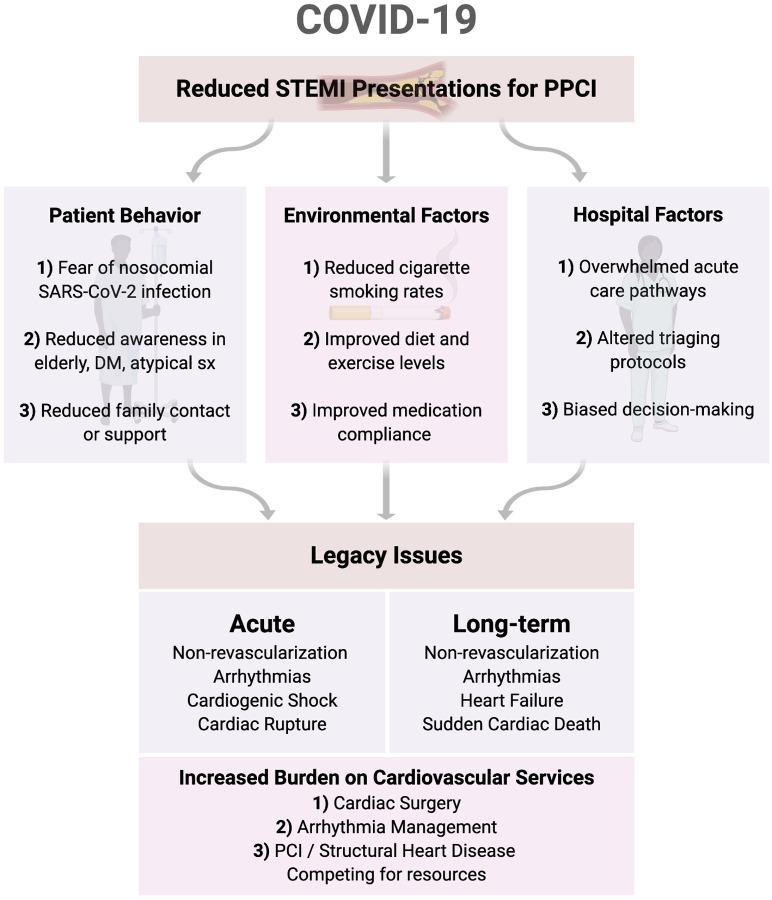
The COVID-19 pandemic has required acute and long-term services to accommodate surges in hospital admissions. Cardiovascular care has experienced challenges to primary percutaneous coronary intervention (PPCI) from safety (personal protective equipment), staffing (health care worker infection rates), and patient welfare perspectives. Recently, an approximately 40% reduction in ST-segment-elevation myocardial infarction (STEMI) presentations for PPCI has been reported during the COVID-19 crisis.1 Reduced STEMI admissions could relate to altered patient behaviour, disrupted care pathways, or altered cardiovascular risk factors pertaining to partial or complete lockdown conditions during the pandemic (Fig. 1 ).
Figure 1.
Potential contributory factors and legacy issues which may arise from decreased PPCI presentations during the COVID-19 pandemic. DM, diabetes mellitus; PPCI, primary percutaneous coronary intervention; STEMI, ST-segment-elevation myocardial infarction. Figure created with Biorender.com.
Human psychologic responses to STEMI symptoms are well known, with around 20% of patients ignoring symptoms or presenting late (>12 hours) despite chest pain,2 a proportion that has not changed since the 1980s. Moreover, a proportion of STEMIs, including in elderly, female, and diabetic patients, present silently or atypically, delaying acute diagnosis. COVID-19 public health warnings may have inadvertently contributed to reduced STEMI patient contact with emergency medical services (EMS) or primary care physicians. Cocooned elderly patients through reduced family contact may also have impaired ability to raise the alarm. Thus, altered patient behaviour is one likely contributing factor to reduced STEMI presentations.
Moreover, early COVID-19 advice to smokers worldwide suggested cessation would reduce hand-to-face contact and thus virus transmission and if implemented this could have affected STEMI event rates.3 In addition, altered stress levels in home-bound subjects may have reduced blood pressure and increased exercise and compliance with medication, with the latter effect likely to be beneficial within a 2-month time window.4 At-risk subjects may also have improved lifestyle given public health warnings regarding cardiovascular risk and poor COVID-19 outcomes. Additional factors include disruption to acute triage and in-hospital care as EMS, emergency rooms, and in-hospital services became overwhelmed by the number and severity of COVID-19 cases to the relative exclusion of other acute medical admissions.
To confirm if this trend of reduced STEMI presentation is real, a comprehensive analysis of STEMI registries worldwide is required. In the short term, STEMI underdetection is likely to presage more acute deaths from underrevascularization, including by lethal arrhythmias, cardiogenic shock, and cardiac rupture, at rates unheralded in recent PPCI history. Medium- and long-term complications, such as heart failure, sudden cardiac death, and postinfarct angina, are also likely to increase. Dealing with the legacy of this unrevascularized cohort will present challenges to multiple cardiology services from structural heart disease to arrhythmia management and to cardiac surgery.
Funding Sources
N.M.C. has received funding from Science Foundation Ireland (grant no. 12/RC/2273_P2).
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [e-pub ahead of print]. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed]
- 2.Eagle K.A., Goodman S.G., Avezum A., et al. Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE) Lancet. 2002;359:373–377. doi: 10.1016/S0140-6736(02)07595-5. [DOI] [PubMed] [Google Scholar]
- 3.Rakowski T., Siudak Z., Dziewierz A., Dubiel J.S., Dudek D. Impact of smoking status on outcome in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. J Thromb Thrombolysis. 2012;34:397–403. doi: 10.1007/s11239-012-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halliday B.P., Wassall R., Lota A.S., et al. Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomised trial. Lancet. 2019;393:61–73. doi: 10.1016/S0140-6736(18)32484-X. [DOI] [PMC free article] [PubMed] [Google Scholar]