The ongoing coronavirus disease 2019 (COVID-19) pandemic is a challenge for patients, health care professionals, and populations worldwide. Endoscopy units and their staff are at high risk to be exposed to and distribute the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Therefore, guidance on endoscopic activity in this pandemic is urgently needed. Recommendations must balance safety issues and practicability and, therefore, need to be cross validated by real-world data and updated as new findings emerge.
To address the need for guidance in this situation, the European Society for Gastrointestinal Endoscopy (ESGE) and the German Respiratory Society (DGP) have published recommendations for endoscopy units to mitigate infection risks. To date, it is unclear whether these recommendations can be implemented in the majority of endoscopy units, because data are scarce and limited to few centers.1 We conducted this survey to explore the ability to implement these recommendations. As such, our data provide a basic framework for future recommendations.
Methods
Based on the ESGE and DGP recommendations, we developed 33 questions to assess the adherence to and practicability of the guidelines in an Internet-based survey. Completion of the survey was possible for 7 days from April 1 to April 7. Further details of the methodology are described in the supplementary material.
Results
Overall, 676 complete questionnaires were retrieved, of which 20 were identified as duplicates or from outside Germany and excluded. In total, 393 endoscopy units were from hospitals, and 263 were from outpatient clinics and practices from all parts of Germany (Supplementary Figure 1). Overall, 145 (22.1%) responses did not include the postal code. Supplementary Table 1 summarizes the results in detail.
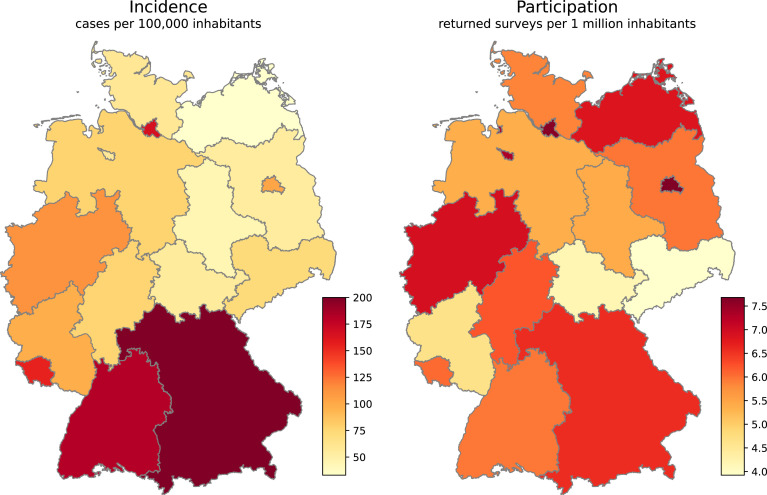
Supplementary Figure 1.
Geographic heatmap of COVID-19 incidence rates in federal states on April 7, 2020, and participating endoscopy units. Nationwide incidence was 119 of 100,000 inhabitants on April 7. Of note, 145 anonymous responses (22.1% of all responses) are not plotted. COVID-19 data were retrieved from the Robert Koch Institute, Germany.
Cancellations of Interventions
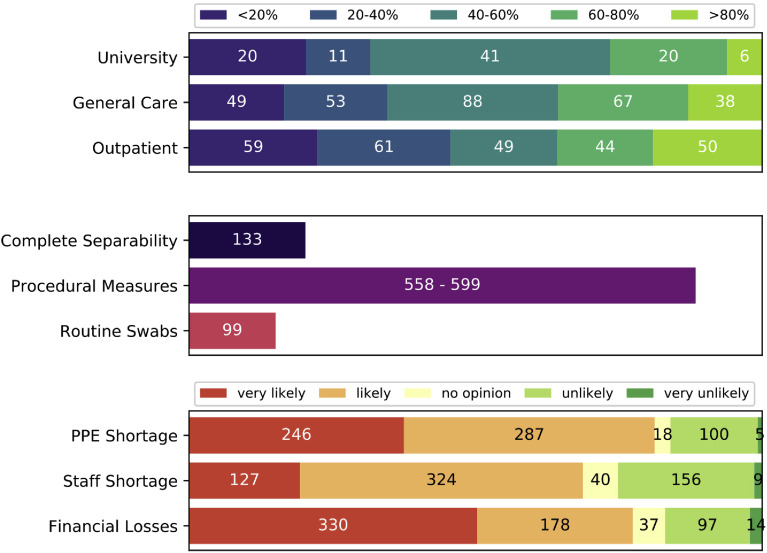
A total of 253 (38.6%) endoscopy units cancelled less than 40%, whereas 225 (34.3%) cancelled more than 60% of their procedures (Figure 1 ). Interestingly, 45.6% of private practices cancelled less than 40% of their procedures, compared to 33.8% of hospital-based units.
Figure 1.
Survey results of 656 responses. (A) Cancelled procedures by level of care. University hospitals and maximum care facilities (n = 98), general and basic care hospitals (n = 295), and outpatient clinics and private practices (n = 263). (B) Realization of endoscopic societies’ recommendations. A mean is given for procedural measures consisting of the structured risk assessment for patients (n = 599), risk-adapted use of PPE (n = 558), and training of staff to treat patients with COVID-19 (n = 584). (C) Expectations of endoscopy unit heads for the future concerning shortages in PPE and staff as well as financial losses threatening the economic survival of the unit.
Separation of Patients at Risk
Ideal conditions for the separation of infectious patients were achieved in only 2.3% of endoscopies (n = 15), where a complete spatial separation and a negative pressure endoscopy suite were available. A complete or ideal separation was possible in 20.3% of the investigated endoscopy units (Figure 1). In general, most units were not able to separate well: 47% could separate only partially (peri-interventional area or endoscopy room), and 32.8% could not separate high-risk patients or those with proven COVID-19 at all.
Procedural Measures
Most endoscopy units (91.6%) identified patients at risk of infection in a structured manner. To mitigate risk of infection, most endoscopy units (>85%) issued new instructions on risk-adapted personal protective equipment (PPE) use and trained their staff in the treatment of patients with COVID-19.
Swabs
Routine swabs for personnel were performed in 5.5% of endoscopy units. Also, the overall rate of preinterventional swabs for patients was low (15.1%). Bronchoscopy units had a considerably higher rate of preinterventional swabs (32.4%) compared to gastrointestinal (GI) units (8.4%).
Expectations
The majority of endoscopy units (81.3%) perceived shortages in PPE as likely or very likely (Figure 1). Overall, 68.8% of endoscopy units expected staff shortages during the pandemic. In total, 77.4% of endoscopy units anticipated substantial financial losses that could threaten the economic survival to be likely or very likely.
Discussion
To our knowledge, this is the first nationwide survey to obtain real-world data on how endoscopy units cope with the current COVID-19 pandemic and the measures taken to ensure continued balanced patient care. The framework of this survey relied on the ESGE and DGP recommendations, both of which were published 14 days before the survey was conducted.
In recent reports, the prevalence of GI symptoms in patients with SARS-CoV-2 infection was higher than previously estimated, ranging from 11.4% to 61.1% in a series with a special focus on GI symptoms.2 , 3 Moreover, there is emerging evidence that SARS-CoV-2 is excreted in the feces, even after it becomes undetectable in the pharynx and lung.4 Furthermore, live virus was detected in the stool of patients.5 , 6 As a consequence of the current knowledge, endoscopy societies have recommended postponing or cancelling all but emergency and urgent endoscopic interventions.7
Our results show that approximately one third of the participating endoscopy units followed these recommendations, because more than 60% of all procedures were cancelled. However, approximately 40% of the endoscopy units still performed more than 60% of their procedures. Interestingly, units performing >60% of procedures were more likely to be private practices (Figure 1). In their comments, heads of outpatient GI units repeatedly pointed out the ethical dilemma because their economic survival is threatened by cancellations. Therefore, strategies to substitute for financial losses endangering economic survival need to be discussed and implemented, particularly for privately owned endoscopy units worldwide.
Of note, the British Society of Gastroenterology published a list of specific interventions and indications to guide planning and cancellations, as did the American Gastroenterological Association, which might serve as a model in this context.7 , 8
It is important to note that only 20.3% of all endoscopy units had the capability to conduct interventions of high-risk patients in a spatially separated endoscopy ward. Ideal conditions, with a negative pressure endoscopy room, were an exception. Because pandemics are irregularly recurring events, these observations should be taken into consideration when new endoscopy units are planned in the future and when emergency plans are updated.
Procedural measures were implemented well, such as risk stratification of patients, risk-adapted use of PPE, and training of staff to treat patients with suspected or proven COVID-19. In contrast, routine follow-up to inquire about symptoms and swabs on patients was rarely conducted. Again, all of these measurements need to be evaluated for their effectiveness in the future.
Finally, fear is evident among many endoscopists that a lack of PPE might further complicate endoscopic activity in the future. Reprocessing of masks is possible and, as such, is warranted in the current situation. Although many practices and outpatient clinics do not have the necessary tools to provide safe reprocessing, cooperation with nearby hospitals and laboratories might be an option to reduce the impact of current PPE scarcity.
Acknowledgments
The authors thank all participating heads of endoscopy units for their responses, trust, and insightful comments. The authors especially thank Clara Heidemann, Marko Damm, Sebastian Krug, and Patrick Michl for their substantial support with performing the survey and writing the manuscript.
CRediT Authorship Contributions
Jakob Garbe, Dr Med (Conceptualization: Lead; Data curation: Lead; Formal analysis: Lead; Methodology: Lead; Project administration: Lead; Writing – original draft: Lead). Stephan Eisenmann, Dr Med (Conceptualization: Equal; Data curation: Equal; Formal analysis: Equal; Methodology: Equal; Project administration: Equal; Visualization: Supporting; Writing – original draft: Equal). Steffen Walter, Dr (Conceptualization: Equal; Formal analysis: Supporting; Methodology: Lead; Writing – review & editing: Supporting). Frank Lammert, Prof Dr (Conceptualization: Supporting; Investigation: Equal; Resources: Lead; Writing – review & editing: Lead). Kaid Darwiche, Prof Dr (Conceptualization: Supporting; Methodology: Supporting; Resources: Lead; Writing – review & editing: Supporting). Jonas Rosendahl, Prof Dr med (Data curation: Equal; Formal analysis: Equal; Methodology: Equal; Supervision: Lead; Validation: Equal; Writing – original draft: Lead).
Footnotes
Conflicts of interest The authors disclose no conflicts.
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at https://doi.org/10.1053/j.gastro.2020.04.061.
Supplemental Material
Methods
Ethical approval was obtained from the local ethical review committee (title: “Versorgungsrealität in deutschen Endoskopiezentren in Zeiten der COVID-19-Pandemie,” 2020-044; March 30, 2020). Based on the ESGE and DGP recommendations, we developed 33 questions to assess the adherence to and practicability of the guidelines in an Internet-based survey. Relevant questions were developed to cover structure-related, personnel-related, and procedure-related measures. Where appropriate, we added additional items to better understand the local situation.
In a fourth category, expectations for the future of endoscopy units were investigated. Answers for questions on measures were yes/no questions or multiple choice; few allowed for answers or specifications in free text. Expectations for the future were requested on a 5-step Likert-type scale (highly probable to highly improbable). The survey was constructed the following expert recommendations of Steffen Walter. It was addressed to the heads of endoscopy units, who were in addition asked to provide basic information on the characteristics and care levels of their units.
The software LimeSurvey (LimeSurvey GmbH, Germany) was used to conduct the survey online. The survey was distributed via the German Society of Gastroenterology, Digestive, and Metabolic Diseases and the DGP. Completion of the survey was possible for 7 days, from April 1 to April 7. Descriptive statistics were calculated using Office Excel 2016 (Microsoft, Redmond, WA).
Duplicates were identified by using the provided postal code and answer patterns as well as cross-referencing in the databases for hospitals, practices, and outpatient clinics.
Data Sources
British Society of Gastroenterology. Endoscopy activity and COVID-19: BSG and JAG guidance. https://www.bsg.org.uk/covid-19-advice/endoscopy-activity-and-covid-19-bsg-and-jag-guidance/. Updated April 3, 2020.
European Society of Gastrointestinal Endoscopy. ESGE and ESGENA position statement on gastrointestinal endoscopy and the COVID-19 pandemic. https://www.esge.com/esge-and-esgena-position-statement-on-gastrointestinal-endoscopy-and-the-covid-19-pandemic/. Published April 17, 2020.
German Hospital Register. https://www.deutsches-krankenhaus-verzeichnis.de/. Accessed April 2020.
Register of respiratory medicine private practices. https://lungenatlas.de/index.aspx. Accessed April 2020.
Register of gastrointestinal private practices and outpatient clinics. https://www.bng-gastro.de/. April 2020.
Robert Koch Institute. Coronavirus disease 2019 (COVID-19): daily situation report of the Robert Koch Institute. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-04-07-en.pdf?__blob=publicationFile. Updated April 7, 2020.
Supplementary Table 1.
Condensed Survey Results by Type of Endoscopy Unit
| n (%) | Type of endoscopy, n (%) |
|||
|---|---|---|---|---|
| Interdisciplinary | Bronchoscopy | Gastrointestinal | ||
| Responses | 656 (100) | 113 (17.2) | 105 (16) | 438 (66.7) |
| Cancellations | ||||
| None or <20% | 128 (19.5) | 15 (13.3) | 34 (32.3) | 79 (18.1) |
| >20% to <40% | 125 (19.1) | 16 (14.2) | 17 (16.2) | 92 (21) |
| >40% to <60% | 177 (27) | 43 (38.1) | 25 (23.8) | 109 (24.9) |
| >60% to 100% | 225 (34.3) | 39 (34.5) | 29 (27.6) | 157 (35.8) |
| Measures applied | ||||
| Separation and structural conditionsa | ||||
| Ideal | 15 (2.3) | 5 (4.4) | 5 (4.8) | 5 (1.1) |
| Complete | 118 (18) | 25 (22.1) | 23 (21.9) | 70 (16) |
| Partial | 308 (47) | 62 (54.9) | 44 (41.9) | 202 (46.1) |
| None | 215 (32.8) | 21 (18.6) | 33 (31.4) | 161 (36.8) |
| Staff | ||||
| Availability of second team | 261 (39.8) | 57 (50.4) | 57 (54.3) | 147 (33.6) |
| Routine staff swabs | 36 (5.5) | 9 (8) | 10 (9.5) | 17 (3.9) |
| Identification of staff at risk | 299 (45.6) | 70 (61.9) | 52 (49.5) | 177 (40.4) |
| Special deployment of staff at risk | 252 (84.3) | 56 (80) | 40 (76.9) | 156 (88.1) |
| Infectiology consultation | 404 (61.6) | 94 (83.2) | 85 (81) | 225 (51.4) |
| Procedural measures | ||||
| Patient risk assessment | 599 (91.3) | 104 (92) | 100 (95.2) | 395 (90.2) |
| Swabs on patients | 99 (15.1) | 28 (24.8) | 34 (32.4) | 37 (8.4) |
| Risk adapted PPE use | 558 (85.1) | 107 (94.7) | 89 (84.8) | 362 (82.6) |
| COVID-19 staff training | 584 (89) | 105 (92.9) | 96 (91.4) | 383 (87.4) |
| Structured follow-up | 59 (9) | 11 (9.7) | 11 (10.5) | 37 (8.4) |
| Expectations for the future | ||||
| Shortages of PPE | ||||
| (Highly) probable | 533 (81.3) | 86 (76.1) | 78 (74.2) | 369 (84.3) |
| No opinion | 18 (2.7) | 7 (6.2) | 4 (3.8) | 7 (1.6) |
| (Highly) improbable | 105 (16) | 20 (17.7) | 23 (21.9) | 62 (14.2) |
| Shortages of staff | ||||
| (Highly) probable | 451 (68.8) | 73 (64.6) | 71 (67.7) | 307 (70.1) |
| No opinion | 40 (6.1) | 4 (3.5) | 8 (7.6) | 28 (6.4) |
| (Highly) improbable | 165 (25.2) | 36 (31.9) | 26 (24.8) | 103 (23.5) |
| Financial losses threatening economic survival | ||||
| (Highly) probable | 508 (77.4) | 85 (75.2) | 66 (62.8) | 357 (81.5) |
| No opinion | 37 (5.6) | 7 (6.2) | 9 (8.6) | 21 (4.8) |
| (Highly) improbable | 111 (16.9) | 21 (18.6) | 30 (28.6) | 60 (13.7) |
Ideal separation was given when, aside from full spatial separability, endoscopic procedures were performed in a separated negative pressure room.
References
- 1.Repici A. Gastroenterology. 2020;159:363–366. doi: 10.1053/j.gastro.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nobel Y.R. Gastroenterology. 2020;159:373–375. doi: 10.1053/j.gastro.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng S.C. Gut. 2020;69:973–974. doi: 10.1136/gutjnl-2020-321195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xiao F. Gastroenterology. 2020;158:1831–1833. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wölfel R. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 6.Wang W. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.British Society of Gastroenterology https://www.bsg.org.uk/covid-19-advice/endoscopy-activity-and-covid-19-bsg-and-jag-guidance/ Published April 3, 2020.
- 8.American Gastroenterological Association https://www.gastro.org/practice-guidance/practice-updates/covid-19/gastroenterology-professional-society-guidance-on-endoscopic-procedures-during-the-covid-19-pandemic Updated March 31, 2020.