Highlights
-
•
The Behavioral Immune System (BIS) contributes to pandemics anxiety.
-
•
A community sample in China (N = 908) was surveyed during the COVID-19 health crisis.
-
•
Disgust propensity and sensitivity was a moderator in fear of contracting COVID-19.
Keywords: COVID-19, Coronavirus, Behavioral immune system, Disgust propensity, Disgust sensitivity, Anxiety sensitivity
Abstract
The COVID-19 public health crisis has led to extensive recommendations by officials to contain its spread. Anxiety regarding contracting the virus is prominent in the public. Specific routes to anxiety over disease contraction are under studied. It is expected that a contributory feature of fear of contracting COVID-19 involve disgust propensity and sensitivity, emotional reactions that are part of a broader behavioral immune system (BIS). A total of N = 908 Chinese adults (mean age = 40.37 years, SD = 9.27; n = 752 female) participated in a survey distributed between February 24 and March 15, 2020. Participants completed measures of anxiety sensitivity, disgust propensity and sensitivity, and fear of contracting COVID-19. Results support a moderating relationship between both disgust propensity and sensitivity in the relationship between physical concerns associated with anxiety sensitivity and fear of contracting COVID-19. These results lend support for individual variation in the activation of the BIS. Recommendations for public education to target individuals who may experience mental health consequences from pandemics are provided.
1. Introduction
The international health crisis prompted by COVID-19 (also known as coronavirus) has led to recommendations from public health officials to contain the spread of this highly contagious virus. Among the methods of containment have been maintaining physical distances of at least six feet when encountering others, wearing face masks, and more frequent and vigorous hand washing (Centers for Disease Control & Prevention, 2020; World Health Organization, 2020). The primary symptoms of COVID-19 are fever, tiredness and dry cough. The virus typically incubates for one to 14 days, with the sufferer experiencing few or no symptoms before full disease expression, and is highly contagious (Lauer et al., 2020). Emerging evidence suggests that COVID-19 has a higher mortality rate than other similar viruses, such as Severe Acute Respiratory Syndrome (SARS) or Middle East Respiratory Syndrome (MERS) (Mahase, 2020). It is highly likely that anxiety about contracting COVID-19 is prominent (Qiu et al., 2020; Wang et al., 2020), and thus the study of psychological risk factors is important as part of developing comprehensive approaches for management.
There has been extensive reporting on the nature, symptoms, and fatality rate of COVID-19. It has been anticipated that the unpredictability of the spread and dangerousness of the virus would have additional mental health impact. Anticipated increases in anxiety and depression due to increased uncertainty have been predicted (Zandifar & Badrfam, 2020), and recent findings have shown actual spikes in these negative mood states (Gao et al., in press; Li, Guan et al., in press; Li, Wang et al., in press).
The availability of detailed information about the illness can contribute to psychological reactions in the public, particularly among individuals with elevated levels of health anxiety (Asmundson & Taylor, 2020), anxiety sensitivity and disgust proneness. Responses to past pandemics are instructive on evaluating how anxiety sensitivity and disgust proneness influence broader anxiety reactions to illness risk. For example, in a college student sample (N = 315) disgust sensitivity was a significant predictor of fear of contracting H1N1 (swine flu) in data collected during times of peak media attention to the pandemic in 2009–2010 (Wheaton, Abramowitz, Berman, Fabricant, & Olatunji, 2012). In a student sample (N = 107) gathered during the peak period of concern over contracting Ebola in the United States in late 2014, the physical concerns subscale of the Anxiety Sensitivity Index (ASI-3; Taylor et al., 2007) and disgust sensitivity (assessed with the Disgust Scale-Revised; DS-R, Olatunji et al., 2007) were correlated with fear of contracting the illness, although neither were significant in regression analyses (Blakey, Reuman, Jacoby, & Abramowitz, 2015). Similar findings were observed in a sample of students and other members of a university community (N = 216) during the time of the Zika outbreak, in 2015–2016, where the ASI-3 physical concerns subscale and the DS-R were significantly correlated with fear of contracting the illness, but were not significant predictors in regression analyses (Blakey & Abramowitz, 2017).
Research on anxiety and disgust reactions from prior pandemics suggest associations with fear of contracting illnesses during pandemics, although the unique variance each accounts for has not been found significant in several recent studies. The nature of COVID-19, with particularly significant respiratory symptoms, and respiratory failure as one of the ways in which the virus can be fatal, increases the relevance of anxiety sensitivity. Reviews of the literature have shown that a general fear of respiratory symptoms is associated with anxiety sensitivity (Horenstein, Potter, & Heimberg, 2018). Additional research has demonstrated a significant role for disgust in health-related concerns, such as hypochondriasis (Weck, Esch, & Rohrmann, 2014). Further, considering that recommended public health measures emphasize potential risks for contracting COVID-19 from surfaces and objects, disgust would be expected to additionally contribute to avoidance given its established role in contamination fear (McKay, 2017), particularly disgust sensitivity (Olatunji, Ebesutani, Haidt, & Sawchuk, 2014).
Disgust sensitivity is the extent that one interprets physical sensations as resulting from disgust and the potential of a contaminant being present. Disgust propensity is the extent that one is likely to experience disgust for a range of putative disgust elicitors (van Overveld, de Jong, Peters, Cavanagh, & Davey, 2006). These emotional experiences form a part of the behavioral immune system (BIS; discussed in Taylor, 2019); in short, the BIS is a system of psychological mechanisms that detect cues to the presence of infectious pathogens in the immediate environment and trigger disease-relevant emotional (e.g., fear, anxiety, disgust) and cognitive responses that promote the avoidance of disease cues (Schaller & Duncan, 2007). Disgust propensity and sensitivity should moderate the relationship between anxiety sensitivity and COVID-19 anxiety. The rationale for a moderating relationship is that both anxiety sensitivity and disgust have health relevant components. Activation of the BIS increases the disgust salience for objects and situations that were not previously found disgusting. As pandemics such as COVID-19 arouse heightened physical monitoring, when present in conjunction with disgust propensity and sensitivity, it is expected that fear of contracting COVID-19 would be heightened.
The conjoint roles of anxiety sensitivity and disgust propensity and sensitivity reflect an environmental activation of the BIS (Schaller & Duncan, 2007). The BIS is activated as an additional safeguard against infection when the risk is not visible to the naked eye. Therefore, anxiety sensitivity, which activates appraisals of changes in physiological reactions as signs of potential danger, along with disgust propensity and sensitivity which appraises specific infection risks, would be expected to be marshaled in protecting against infection when information about increased risks become known (discussed in Taylor, 2019). What is less clear is the extent that disgust propensity and sensitivity, and anxiety sensitivity, might work together. On the one hand, these could operate concurrently. On the other, since disgust is activated for more specific situations as compared to anxiety sensitivity, which is activated more frequently due to the ongoing daily changes in physical reactivity, disgust would be expected to be a moderator in relation to anxiety sensitivity and anxiety regarding potential infection. As the BIS is activated to detect cues related to potential pathogen infection (Schaller & Park, 2011), this would specifically implicate physical detection via anxiety sensitivity. It would also be expected to heighten disgust awareness, given the role of emotion in protecting against potential harm from pathogens. This potential harm includes pathogen contact that is not oral, such as through the skin (i.e., Tolin, Worhunsky, & Maltby, 2004). This study is the first of its kind to test the relationship between these two disgust-related variables in predicting fear of contracting a pandemic-based infection, such as the one represented in COVID-19.
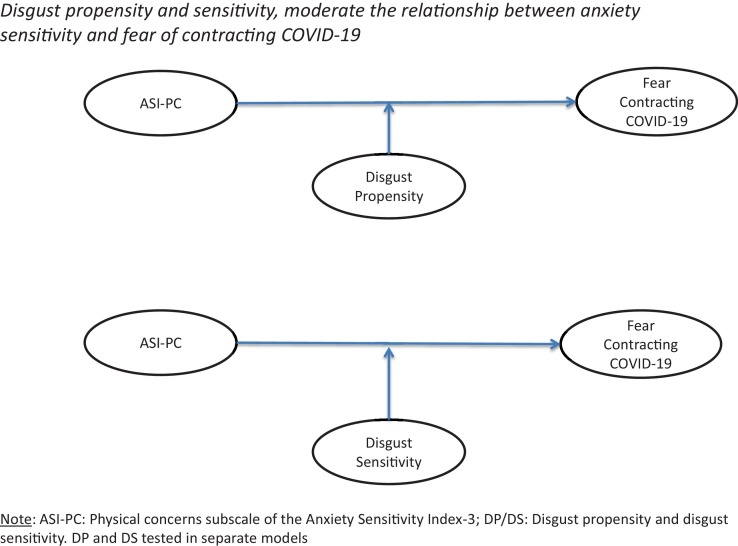
This study sampled individuals living in China during the COVID-19 outbreak, which first appeared in Wuhan province at the end of 2019 (Li, Guan et al., 2020; Li, Wang et al., 2020). The aims of the study were to investigate the predictive and moderating effects of disgust on anxiety sensitivity and fear of contracting COVID-19. Based on the above review, the following hypotheses were tested, with the moderator models tested illustrated in Fig. 1 :
Fig. 1.
Moderation Model Tested.
H1: Disgust propensity and sensitivity, and the physical concerns associated with anxiety sensitivity, predict anxiety regarding contracting COVID-19.
H2: Disgust propensity and sensitivity moderate the relationship between physical concerns associated with anxiety sensitivity and anxiety regarding contracting COVID-19.
2. Methods
2.1. Participants and procedure
A cross-sectional online survey of Chinese adults between February 24-March 15, 2020 was conducted. We invited participants using the commonly-used Chinese social media app “WeChat” (Montag, Becker, & Gan, 2018). WeChat has location-based online groups, and it was arranged for WeChat group moderators from localities within a large urban city in Eastern China (Tianjin, population = 12 million) to invite their residents to participate. Interested participants were shown an online informed consent statement and, for those agreeing, a Chinese language online survey. The survey was hosted on Survey Star, offering features to prevent automated participation by bots. Individuals completing the survey received compensation, randomly allotting a digital payment or voucher, from 3 to 10 Chinese RMB (roughly equivalent to 0.50-$1.50 USD). Our project was approved by the Tianjin Normal University ethics committee, following the Declaration of Helsinki.
The online survey reminded individuals to complete skipped items; therefore, we had no missing data. After deleting participants entering the same response consecutively across dozens of items, 908 participants remained. Mean age was 40.37 years (SD = 9.27), ranging from 17 to 64 years, most participants were women (n = 752, 82.82 %), and a majority of participants were of Chinese Han ethnicity (n = 875, 96.37 %).
2.2. Instruments
In addition to surveying demographic characteristics including sex, age and ethnicity the following measures were administered:
2.2.1. Depression Anxiety Stress Scale-21 (DASS-21)
The DASS-21 is a 21-item self-report instrument, with symptom ratings over the past week. The instrument employs a Likert-type scale from “0 = Did not apply to me at all” to “3 = Applied to me very much, or most of the time.” We analyzed only depression and anxiety items (7 items each) and used these as covariates in the regression and moderator tests. The depression and anxiety subscales have adequate reliability and validity (Zanon et al., in press). We used the Chinese instrument version, validated previously (Wang et al., 2016). Internal consistency (coefficient alpha) in our sample was .82 for depression, and .76 for anxiety.
2.2.2. Generalized Anxiety Disorder Scale-7 for COVID-19 Anxiety (CoVGAD-7)
The GAD-7 is a 7-item self-report measure of anxiety and worry symptoms (originally in English), with past two-week rating instructions. The scale uses a Likert-type frequency scale from “0 = Not at all” to “3 = Nearly every day.” Total scores are considered valid and reliable (Plummer, Manea, Trepel, & McMillan, 2016). The measure is widely adopted, including as part of the Mental and Behavioral Health Registry of the American Psychological Association (Wright et al., in press). We used the Chinese version, validated by He, Li, Qian, Cui, and Wu (2010). We tailored instructions to inquire about COVID-19 anxiety, asking “Over the last 2 weeks, how often have you been bothered by the following problems because of the Coronavirus outbreak?” The internal consistency for the present sample was .90.
2.2.3. Anxiety Sensitivity Index-3rd edition (ASI-3) edition (ASI-3)
The ASI-3 (originally in English) is an 18-item measure that assesses anxiety sensitivity along three dimensions—physical concerns, social concerns, and cognitive concerns—with six items for each subscale (Taylor et al., 2007). There is also a valid total score. Items are rated along a five point scale from “0=very little” to “4=very much.” The Chinese version was employed in this study, which has comparable factor structure (Wang et al., 2014). The internal consistency for the present sample was 0.95 for the total scale, and 0.90 for the physical concerns subscale.
2.2.4. Disgust Propensity and Sensitivity Scale-Revised (DPSS-R)
The DPSS-R (van Overveld et al., 2006) is a 16-item scale (originally in English) that assesses disgust propensity and sensitivity in separate 8-item factor analytically derived scales. Each scale of the measure has been shown to predict avoidance of disgust-evoking behavioral avoidance tasks, including tasks associated with pathogens (touching a bandage with a red spot, wiping face with unwashed towel, combing hair with a used brush, using a finger to stir a cup purported to contain someone else’s saliva) (van Overveld, de Jong, & Peters, 2010). Items are rated from “0=never” to “4=always.” For the present study, the original scale was translated to Chinese and back-translated to English, verified and refined, to ensure proper use in the Chinese language. The disgust propensity subscale in the current study had an internal consistency of 0.84, and for disgust sensitivity it was 0.87.
2.3. Analysis
Analyses were conducted using the SPSS software package (v. 25.0 for Mac; IBM Corporation, 2017). Moderator tests (displayed in Fig. 1) were conducted using the additional PROCESS v.3.4 macro (Hayes, 2018). Scales used in the primary analyses were summed, as recommended in the development of the measures. It was assumed that the DPSS-R, which was not previously published in Chinese and translated here to Chinese but not subject to additional tests of validity, retained the two-factor structure originally found in van Overveld et al. (2006). We conducted a confirmatory factor analysis (CFA) of the two-factor disgust sensitivity/propensity model. We treated items as ordinal, using a polychoric covariance matrix, probit factor loadings, and weighted least-squares estimation with a mean- and variance- adjusted chi-square test. The model fit well, robust χ2(103, N = 908) = 830.857, p < .001, CFI = .96, TLI = .96, RMSEA = .09 (90 % CI: .08–.09), SRMR = .04. Given that the predictions were related specifically to disgust sensitivity and propensity, no additional analyses were conducted on the total score. Similarly, as the measure for anxiety regarding contracting CoV-19 was adapted from the GAD-7, a CFA was conducted. A single factor was found that fit the data well, robust χ2(14, N = 908) = 114.90, p < .001, CFI = .99, TLI = .98, RMSEA = .09 (90 % CI: .07–.11), SRMR = .03. As a result of these analyses, the total score of the CoVGAD-7 was used.
3. Results
3.1. Descriptive information
Table 1 displays the correlation matrix and descriptive information on the sample and the measures used in the primary analyses for this study. Using prior benchmarks, no variables were significantly skewed or kurtotic.
Table 1.
Correlation Matrix and Descriptive Statistics for Age and Study Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
|
– | ||||||
|
0.02 | – | |||||
|
0.06 | 0.78 | – | ||||
|
0.06 | 0.59 | 0.67 | – | |||
|
−0.06 | 0.48 | 0.39 | 0.41 | – | ||
|
−0.06 | 0.49 | 0.49 | 0.56 | 0.68 | – | |
|
−0.01 | 0.52 | 0.52 | 0.52 | 0.54 | 0.45 | – |
| Mean | 40.37 | 16.49 | 13.59 | 4.90 | 2.77 | 3.93 | 4.32 |
| SD | 9.27 | 5.46 | 5.44 | 4.90 | 3.21 | 3.17 | 3.88 |
Note: DPSS-R is Disgust Propensity and Sensitivity Scale-Revised; ASI-3 is the Anxiety Sensitivity Index-3rd edition; CoVGAD-7 is the Generalized Anxiety Disorder scale modified for CoV-19.
Correlations greater than |0.12| were significant at p<.05.
3.2. H1: Disgust propensity and sensitivity, and the physical concerns associated with anxiety sensitivity predict anxiety regarding contracting COVID-19
Multiple regression analyses were conducted, with age, gender, anxiety and depression as covariates and with CoVGAD-7 as the criterion and the subscales of the DPSS-R and ASI-3 as predictors. The total model when examining the predictive value of the ASI-3 physical concerns and DPSS-R propensity was F(6,901) = 151.98, p < .001, with Adjusted R2 change = 0.50. The DPSS-R propensity subscale had β = 0.16 (t(901) = 5.24, p < .001) and the ASI-3 physical concerns subscale had β = 0.14 (t(901) = 4.48, p < .001). The total model when examining the predictive value of the ASI-3 physical concerns and DPSS-R sensitivity was F(6,901) = 153.97 p < .001, with Adjusted R2 change = 0.51. The DPSS-R sensitivity subscale had β = 0.19 (t(901) = 5.78, p < .001) and the ASI-3 physical concerns subscale had β = 0.11 (t(901) = 3.28, p < .001). As the hypothesis centered on the physical concerns subscale of the ASI-3 in conjunction with either the propensity or sensitivity subscales of the DPSS-R, the same pattern of significance was found for the cognitive concerns and social concerns subscales of the ASI-3. For brevity, these results are not reported here, but are available upon request.
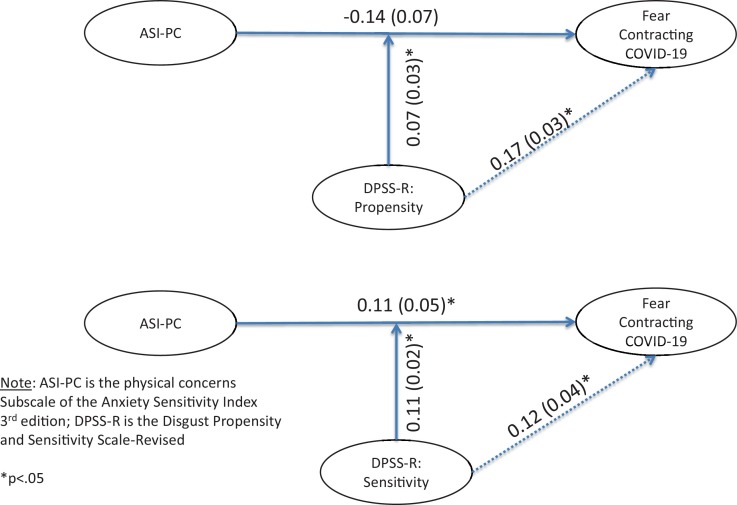
3.3. H2: Disgust propensity and sensitivity moderate the relationship between physical concerns associated with anxiety sensitivity and anxiety regarding contracting COVID-19
Moderator tests using PROCESS were conducted, with age, gender, anxiety, and depression as covariates. As with the regression analyses in Hypothesis 1, a total of six moderator analyses were conducted. Specifically, each subscale of the DPSS-R was designated a moderator, with each subscale of the ASI-3 as predictors (2 subscales of DPSS-R by 3 subscales of ASI-3 equals 6 sets of regression analyses) of the CoVGAD-7. In these analyses, only the moderator tests involving both subscales of the DPSS-R, individually, in conjunction with the ASI-3 physical concerns subscale, were significant in predicting the CoVGAD-7. The model test statistics for each predictor weight are presented in Fig. 2 . The total model for DPSS-R propensity moderating the relationship between ASI-3 physical concerns and CoVGAD-7 was R2 = 0.51 (F(7,900) = 132.13, p < .001). The total model for DPSS-R sensitivity moderating the relationship between ASI-3 physical concerns and CoVGAD-7 was R2 = 0.55 (F(7,900) = 183.80, p < .001).
Fig. 2.
Disgust Propensity and Sensitivity Moderator Tests.
4. Discussion
The results from these analyses show that, taken individually, anxiety sensitivity and both disgust propensity and sensitivity predict fear of contracting COVID-19. From the regression analyses, anxiety sensitivity, which denotes a tendency to interpret changes in physical sensations as potentially harmful and has associated implications for apprehensions in appearing anxious and loss of cognitive functioning, each individually predict fear of contracting COVID-19. However, the findings from the moderator hypotheses provide a more nuanced understanding of the association among these variables.
Moderator analyses that address the anticipated relationship between anxiety sensitivity and disgust propensity and sensitivity show a more specific relationship, one expected based on the BIS model of disease avoidance. This suggests that public health approaches to managing anxiety would emphasize that individuals who might be prone to monitoring physical sensations (i.e., respiration, in the case of CoV-19 concerns; Xu et al., 2020) would benefit from education regarding the potential for false alarms regarding these interpretations. Complicating this further in relation to COVID-19 is the long incubation period of the virus, with a carrier potentially being infected for up to 14 days before symptom expression (Lauer et al., 2020). As a result, individuals at risk for significantly heightened anxiety due to COVID-19 may suffer disabling anxiety for up to two weeks following any incidental contact with others whom they believe are hosts for the virus. Further, public information about the contributory factors involved in anxiety regarding contracting COVID-19 is further influenced by one’s propensity to experiencing disgust, and the sensitivity one has to interpreting sensations as emanating from disgust. This is consistent with basic research on the transmissibility of disgust (discussed in McKay, 2017); that is, the degree that an individual is inclined to have an active BIS even in times that are not marked by higher risk of infection will interact with their pre-existing tendency to monitor their physical state for potential changes.
The importance of these findings is that when developing treatment for individuals fearful about contracting COVID-19, specific consideration for disgust reactions is necessary. This is central given that disgust is not currently part of any systematic treatment programs (McKay, 2017). Some models of intervention have been proposed that include counterconditioning, habituation methods, and conceptual reorientation (discussed in Mason & Richardson, 2012). These approaches have not been carefully investigated in the context of addressing disgust reactions, but given its role as a moderator in the BIS, intervention may serve to alleviate the physical sensations associated with anxiety sensitivity that in turn contributes to fear of contracting COVID-19.
This study had several important limitations. First, the research reported was based on a community convenience sample. As individual participants were not interviewed, more detailed evaluations of specific manifestations of the emotional reactions to COVID-19 could be examined. This limitation emerged from active quarantine conditions, and hence in-person questionnaire administration or interviews could not be conducted. Additionally, it is possible that participants self-selected based on their concerns over COVID-19, and thus may not be fully representative of the population affected, such as through quarantine or other closures, by the pandemic. Further, as these data are cross-sectional in nature, we cannot make causal statements regarding the relationship among the study variables. It is expected that the findings from this study can be used as a basis for future investigations either as part of the COVID-19 pandemic, or future pandemics. For example, interview based examinations could further probe the relationship among the variables here, and additional evaluate factors underlying the BIS. Pre-existing concerns with pathogens might be also further evaluated for it’s potential role in activating the BIS and contributing the relationships identified in this study. Prior research has suggested that obsessive-compulsive symptoms may play a role in anxiety sensitivity when considered in the context of prior pandemic fears (i.e., H1N1; Brand, McKay, Wheaton, & Abramowitz, 2013) and thus may serve as an additional focus of investigation. For example, longitudinal studies are needed to determine whether premorbid disgust propensity and sensitivity, anxiety sensitivity, and fear of death, or levels of these traits measured during early periods in the viral outbreak, are associated with fear of contracting COVID-19 infection measured at later periods in the pandemic.
Footnotes
Dr. Meredith Coles served as Action Editor.
References
- Asmundson G.J.G., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020;71 doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey S.M., Abramowitz J.S. Psychological predictors of health anxiety in response to the Zika virus. Journal of Clinical Psychology in Medical Settings. 2017;24:270–278. doi: 10.1007/s10880-017-9514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey S.M., Reuman L., Jacoby R.J., Abramowitz J.S. Tracing “fearbola”: Psychological predictors of anxious responding to the threat of Ebola. Cognitive Therapy and Research. 2015;39:816–825. doi: 10.1007/s10608-015-9701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand J., McKay D., Wheaton M.G., Abramowitz J.S. The relationship between obsessive compulsive beliefs and symptoms, anxiety and disgust sensitivity, and Swine Flu fears. Journal of Obsessive-compulsive and Related Disorders. 2013;2:200–206. doi: 10.1016/j.jocrd.2013.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Author; Washington, DC: 2020. Coronavirus disease 2019 (COVID-19)https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html [Accessed 4 April 2020] [Google Scholar]
- Gao, J., Dai, J., Zheng, P., Chen, H., Mao, Y., Chen, S., Wang, Y., … Jia, Y. (in press). Mental health problems and social media exposure during COVID-19 outbreak. Lancet. [DOI] [PMC free article] [PubMed]
- Hayes A.F. Guilford; New York, NY: 2018. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- He X.Y., Li C.B., Qian J., Cui H.S., Wu W.Y. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatient. Shanghai Archives of Psychiatry. 2010;22:200–203. [Google Scholar]
- Horenstein A., Potter C.M., Heimberg R.G. How does anxiety sensitivity increase risk of chronic medical conditions? Clinical Psychology Science and Practice. 2018;25 doi: 10.1111/cpsp.12248. [DOI] [Google Scholar]
- IBM Corporation . Vol. 25.0. IBM Corportation; Armonk, NY: 2017. (IBM SPSS for Macintosh). [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredity H.R., Azman A.S.…Lessler J. The incubation period of coronavirus 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Annals of Internal Medicine. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Q., Guan, X., Wu, P., Wang, X., Zhou, L., Tong, Y., Ren, R., … Feng, Z. (in press). Early transmission dynamics in Wuhan, China, of novel coronavirus –infected pneumonia. New England Journal of Medicine. DOI: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed]
- Li, S., Wang, Y., Xue, J., Zhao, N., & Zhu, T. (in press). The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. International Journal of Environmental Research and Public Health. 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed]
- Mahase E. Coronavirus: COVID-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. British Medical Journal. 2020;368:m641. doi: 10.1136/bmj.m641. [DOI] [PubMed] [Google Scholar]
- Mason E.C., Richardson R. Treating disgust in anxiety disorders. Clinical Psychology Science and Practice. 2012;19:180–194. [Google Scholar]
- McKay D. Presidential address: Embracing the repulsive: The case for disgust as a functionally central emotion in the theory, practice, and dissemination of cognitive-behavior therapy. Behavior Therapy. 2017;48:731–738. doi: 10.1016/j.beth.2017.08.006. [DOI] [PubMed] [Google Scholar]
- Montag C., Becker B., Gan C. The multipurpose application WeChat: A review on recent research. Frontiers in Psychology. 2018;9:2247. doi: 10.3389/fpsyg.2018.02247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanon, C., Brenner, R. E., Baptista, M. N., Vogel, D. L., Rubin, M., Al-Darmaki, F. R.,. . . Topkaya, N. (in press). Examining the dimensionality, reliability, and invariance of the Depression, Anxiety, and Stress Scale–21 (DASS-21) across eight countries. Assessment. doi: 10.1177/1073191119887449. [DOI] [PubMed]
- Olatunji B.O., Cisler J.M., Deacon B.J., Connolly K., Lohr J.M. The Disgust Propensity and Sensitivity Scale-Revised: Psychometric properties and specificity in relation to anxiety disorder symptoms. Journal of Anxiety Disorders. 2007;21:918–930. doi: 10.1016/j.janxdis.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Ebesutani C., Haidt J., Sawchuk C.N. Specificity of disgust domains in the prediction of contamination anxiety and avoidance: A multimodal examination. Behavior Therapy. 2014;45:469–481. doi: 10.1016/j.beth.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller M., Duncan L.A. The behavioral immune system: Its evolution and social psychological implications. In: Forgas J.P., Haselton M.G., von Hippel W., editors. Sydney symposium of social psychology: Evolution and the social mind: Evolutionary psychology and social cognition. Routledge/Taylor & Francis Group; 2007. pp. 293–307. [Google Scholar]
- Schaller M., Park J.H. The behavioral immune system (and why it matters) Current Directions in Psychological Science. 2011;20:99–103. doi: 10.1177/0963721411402596. [DOI] [Google Scholar]
- Taylor S., Zvolensky M.J., Cox B.J., Deacon B., Heimberg R.G., Ledley D.R., Abramowitz J.S., Cardenas S.J. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Taylor S. Cambridge Scholars Publishing; Newcastle upon Tyne: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. [Google Scholar]
- Tolin D.F., Worhunsky P., Maltby N. Sympathetic magic in contamination-related OCD. Journal of Behavior Therapy and Experimental Psychiatry. 2004;35:193–205. doi: 10.1016/j.jbtep.2004.04.009. [DOI] [PubMed] [Google Scholar]
- van Overveld W.J.M., de Jong P.J., Peters M.L., Cavanagh K., Davey G.C.L. Disgust propensity and disgust sensitivity: Separate constructs that are differentially related to specific fear. Personality and Individual Differenes. 2006;41:1241–1252. doi: 10.1016/j.paid.2006.04.021. [DOI] [Google Scholar]
- van Overveld M., de Jong P.J., Peters M.L. The disgust propensity and sensitivity scale – Revised: Its predictive value for avoidance behavior. Personality and Individual Differences. 2010;49:706–711. doi: 10.1016/j.paid.2010.06.008. [DOI] [Google Scholar]
- Wang L., Liu W., Zhu X., Wang Y., Li L., Yang Y. Validity and reliability of the Chinese Version of the Anxiety Sensitivity Index-3 in healthy adult women. Chinese Mental Health Journal. 2014;28:767–771. [Google Scholar]
- Wang K., Shi H.S., Geng F.L., Zou L.Q., Tan S.P., Wang Y., Chan R.C. Cross-cultural validation of the Depression Anxiety Stress Scale-21 in China. Psychological Assessment. 2016;28(5):e88–e100. doi: 10.1037/pas0000207. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weck F., Esch S., Rohrmann S. The role of disgust in patients with hypochondriasis. Anxiety, Stress, and Coping. 2014;27:576–586. doi: 10.1080/10615806.2013.873793. [DOI] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (Swine Flu) pandemic. Cognitive Therapy and Research. 2012;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- World Health Organization . 2020. Rolling update on the coronavirus disease (COVID-19) April 2, 2020 update. Geneva, Switzerland. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. [Accessed 4 April 2020] [Google Scholar]
- Wright, C.V., Bard, D., Bobbitt, B., Butt, Z., Goodheart, C., Lysell, K., McKay, D., & Stephens, K. (in press). Promoting measurement-based care and quality measure development: The APA Mental and Behavioral Health Registry Initiative. Psychological Services. [DOI] [PubMed]
- Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C.…Wang F.S. Pathological findings of COVID-19 associated with acute respiratory syndrome. The Lancet Respiratory Medicine. 2020 doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]