Abstract
Background: Health clinic design varies from country to country. The layout of a general practitioner’s (GP’s) consulting room may influence the physician’s or patient’s experience. The aim of this study is to explore and investigate the layout of GP’s consulting rooms around the world and to describe any significant differences.
Methods: Between 3rd July and 2nd August 2018, an internet-based questionnaire on Google Docs was distributed by email, social media and WhatsApp platforms to several worldwide rural medicine groups. Analysis of an internet-based questionnaire to explore possible layouts of consultation rooms within practices was performed. The questionnaire was designed with three distinct sections: first, a GP demographic profile including gender, year of graduation from medical school, country of graduation, and type of practice (private or public); second, questions relating to the office layout; third, a section for questionnaire feedback.
Results: 502 responses to the questionnaire were received; 65.3% women and 34.7% men. The most common layout in Europe and America was where the physician and the patient were separated by a desk. The layout where the physician and the patient had a 90º angle facing each other was the most commonly used layout in Asia-Australia and Africa. For GPs who graduated before 1990 and between 1990-2010, the layout where the table was between the patient and physician was preferred. However, physicians graduating after 2010 preferred a layout with the physician and the patient with a 90º angle facing each other.
Conclusion: The position of the GP’s desk differs between and within countries as well as the gender of the physician and year of graduation. Next steps should focus on gathering an even greater breadth of GP input, as well as comparing and contrasting those to the preferences of our patients and communities.
Keywords: primary health care, health facilities, facility design and construction, doctor-patient relations, health communication, family medicine
Introduction
General practitioner’s (GP’s) consulting rooms differ from country to country, not only in language and cultural influences, but also in architectural design and placement of exam tables, desks, and chairs. Communication proves integral for GPs 1. The incorporation of computers and electronic medical records has further changed the physical environment and the way communication occurs. A GP consultation is one of the central experiences of the patient-physician interaction with both the location of the GP’s desk and the furniture arrangement impacting that encounter 2.
A clinical encounter requires a doctor, a patient, and two chairs at a minimum. Additionally, most practices will also have an office desk as well as a computer. These elements (two chairs and a desk) can be placed in various arrangements. Dannenberg & Burpee argue that the design focusing solely on safety regulations, such as following building codes and avoiding fire hazards, lose all the possibilities of improving the doctor and patient experience 3. Though these safety aspects are extremely important, engineers should not forego consideration of the medical encounter itself. For example, the physician’s desk can compartmentalize the physician and patient in opposite spaces - effectively serving as a “barrier” and interfering with communication 4. Furthermore, the power relationship can be directly affected by the GP’s desk position, including the computer 5, 6 and furniture arrangement that can negatively influence the physician-patient relationship. In some cases, the introduction of the computer in the consultation room has led patients and physicians to make comparisons with the past and the “two players” consultation where computers - the third party - was not present 7. In one study that included a focus group, patients preferred to sit beside the physician with a clear view of the computer screen 8.
The question of where the GP should sit to promote optimal patient-centered care was raised in a Google Group discussion of the World Organization of Family Doctors (WONCA) Rural Working Party. After several email exchanges, the authors decided to develop a questionnaire-based survey. The aim of this study was to explore and investigate the layout of GP’s consulting rooms around the world and to describe any significant differences.
Methods
A specific questionnaire exploring this topic was not found and the authors decided to develop one. This was an exploratory questionnaire intended to examine the possible layouts of consultation rooms within practices.
Between July 3rd and August 2nd 2018, an internet-based questionnaire on Google Docs ( Extended data) was distributed by email to several worldwide rural medicine social media and WhatsApp groups. The communities form a part of the WONCA Rural Working Party network and contain approximately 1200 GPs and trainees.
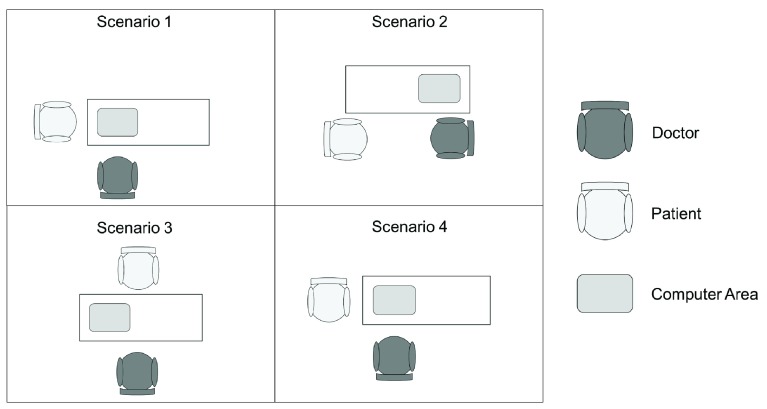
The questionnaire was designed with three distinct sections. First, the GP demographic profile was collected including gender, year of graduation from medical school, country of graduation, type of practice (private or public), if they were in a rural/remote or urban area, and if there was a computer in their practice. The second part included questions relating to the office layout ( Figure 1). We proposed four scenarios as suggested in the Google group discussions. If the practice design was not represented in the scenarios proposed, the participants had the option to describe their own set up. Finally, there was a section for questionnaire feedback in order to allow for future improvements. This included a free text section and a question about satisfaction of the questionnaire (ranked from extremely dissatisfied to extremely satisfied).
Figure 1. Proposed scenarios of practice with a computer.
Participants could opt to describe their own practice if none of the scenarios matched.
The four scenarios proposed with a computer were ( Figure 1):
Scenario 1: GP and patient with a 90° angle facing the desk with the computer on the corner.
Scenario 2: GP and patient directly facing each other with the computer at the desk.
Scenario 3: GP and patient separated by a desk with a computer in the middle/corner
Scenario 4: GP and patient with a 90° angle facing each other with the computer on the corner.
Other scenarios: Describe your own consulting room design
We analyzed the results of the study questionnaire using Chi-squared tests. The results were considered significant with p<0.05. The statistical programs Epi Info v7.2.2.1 and SPSS v23 were used for the statistical analyses. We did not analyze the qualitative responses in this study as they were intended to improve the design of a future questionnaire.
Results
In total, 502 responses were collected during the 30-day period the questionnaire was active; 328 of the respondents (65.3%) were women and 174 (34.7%) were men. The country of practice with the most respondents was Romania with 199 responses (39.6%), followed by Spain with 140 (27.9%), Brazil with 51 (10.2%), Mexico with 32 (6.4%) and India with 16 (3.2%). We asked respondents to describe their practice area as rural/remote or urban; 114 respondents described their area as rural/remote (22.7%) and 379 as urban (75.5%). A total of 296 respondents described their practice as public (59%) and 184 as private (36.7%).
Regarding computers at the practice, 482 out of 502 (96%) respondents had a computer at their practice and 20 (4%) did not. All except one of the respondents who didn’t have a computer were from developing countries - mainly Nigeria (40%), India (15%), and Brazil (15%).
We analyzed the countries of practice in four main geographical regions: Europe, Asia-Australia, the Americas (North and South America), and Africa.
In relation to practice layout, the most common setup in Europe was scenario 3, with the doctor and the patient separated by a desk (66%). This is also the most widely used layout in the Americas (46%), closely followed by scenario 4, with the GP and the patient with a 90° angle facing each other (41%). Scenario 4 was also the most common layout in Asia-Australia (80%) and Africa (56%).
When comparing geographical regions, scenario 3 was used significantly more often in Europe than in the Americas (p=0.0003), whereas scenario 4 is used significantly more often (p<0.0005) in the Americas than in Europe. We did not analyze differences in the layouts between Asia-Australia and Africa as we had so few responses. Layouts of practice by geographical are reported in Table 1.
Table 1. Layout of practice by geographical area.
| Scenario | Total | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||
| Zone | Europe | Count | 20 | 65 | 232 | 33 | 350 |
| % within Zone | 6% | 19% | 66% | 9% | 100% | ||
| Asia-Australia | Count | 0 | 1 | 0 | 4 | 5 | |
| % within Zone | 0% | 20% | 0% | 80% | 100% | ||
| America | Count | 3 | 9 | 41 | 37 | 90 | |
| % within Zone | 3% | 10% | 46% | 41% | 100% | ||
| Africa | Count | 3 | 1 | 0 | 5 | 9 | |
| % within Zone | 33% | 11% | 0% | 56% | 100% | ||
| Total | Count | 26 | 76 | 273 | 79 | 454 | |
| % within Zone | 6% | 17% | 60% | 17% | 100% | ||
There were no statistically significant differences in the layout of the practice depending upon whether the practice was rural or urban (scenario 1, p=0.411; scenario 2, p=0.627; scenario 3, p=0.953; scenario 4, p=0.360).
We analyzed responses according to the respondents’ year of medical school graduation and established three cohorts: before 1990, between 1990 and 2010 and after 2010. Amongst those who graduated before 1990, the most common scenario was number 3 (54%), followed by scenario 2 (27%). Amongst those who graduated between 1990 and 2010, the most common scenario was number 3 (71 %). Amongst those who graduated after 2010, the most common layout was scenario 4 (55%), followed by scenario 3 (31%). Scenario 2 was used significantly more often by respondents who graduated before 1990 than by respondents who graduated between 1990 and 2010 (p=0.003) and those who graduated after 2010 (p=0.003). Scenario 3 was used significantly more often by respondents who graduated between 1990 and 2010 than respondents who graduated before 1990 (p=0.0002) and those who graduated after 2010 (p<0.0005). Finally, Scenario 4 was used significantly more often by respondents who graduated after 2010 than by respondents who graduated before 1990 (p=0.0002) and respondents who graduated between 1990 and 2010 (p=0.0002). Layouts of practice by year of graduation are reported in Table 2.
Table 2. Practice layout by year of graduation of the GP.
| Scenario | Total | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||
| Graduation | <1990 | Count | 13 | 52 | 104 | 25 | 194 |
| % within grad3 | 7% | 27% | 54% | 13% | 100% | ||
| 1990–2010 | Count | 14 | 21 | 153 | 27 | 215 | |
| % within grad3 | 7% | 10% | 71% | 13% | 100% | ||
| >2010 | Count | 3 | 6 | 20 | 36 | 65 | |
| % within grad3 | 5% | 9% | 31% | 55% | 100% | ||
| Total | Count | 30 | 79 | 277 | 88 | 474 | |
| % within grad3 | 6% | 17% | 58% | 19% | 100% | ||
Most female GPs reported using scenario 3 (66%), followed by scenario 2 (16%). Male GPs also used scenario 3 most often (44%), but scenario 4 (28%) was the second most popular layout. Scenario 1 was used statistically significantly more often by male rather than female respondents (p=0.01), while scenario 3 was used statistically significantly more often by female than male respondents (p<0.0005). In contrast, scenario 4 was used more often by male than female respondents (p=0.0002). Layouts of practice by gender are reported in Table 3.
Table 3. Exam room layout by gender of GP.
| Scenario | Total | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||
| Gender | Female | Count | 14 | 51 | 207 | 44 | 316 |
| % within Gender | 4% | 16% | 66% | 14% | 100% | ||
| Male | Count | 16 | 28 | 69 | 44 | 157 | |
| % within Gender | 10% | 18% | 44% | 28% | 100% | ||
| Total | Count | 30 | 79 | 277 | 88 | 474 | |
| % within Gender | 6% | 17% | 58% | 19% | 100% | ||
Finally, the participants rated the questionnaire with 104 (20.9%) extremely satisfied, 187 (38.6%) moderately satisfied, 185 (37.1%) neither satisfied or nor dissatisfied, 16 (3.2%) moderately dissatisfied and 6 (1.2%) extremely dissatisfied. In addition, the participants’ main feedback of how to improve the questionnaire was to allow participants to design their own consultation room and/or to have picture illustrations.
Discussion
This study found that the position of the GP’s desk differs internationally, within countries, and according to year of graduation as well as the gender of the GP. Each approach has a social and cultural context ( Figure 2).
Figure 2. Real examples of practice layouts.
All images were authorized for use by the general PR actioners who sent in the pictures.
The position of the chairs and desk can directly affect the doctor-patient relationship. Jacobs has previously described that arranging chairs perpendicularly (e.g. Scenario 1) implies teamwork and support, chairs placed side-by-side augments education and instruction, while chairs arranged face-to-face (e.g. Scenario 2) show expertise and can be used to gain compliance 9. Scenario 3 was the setup most widely used in Europe. Because of the computer interference and the table in between, this layout does not necessarily support ‘expertise’ of the physician while simultaneously distancing the patient 9.
In this study, women preferred scenario 3 (66%), followed by scenario 2 (16%). Generally, female GPs reassure and encourage patients more compared to their male counterparts 1 who most often used scenario 3 (44%) - noting that scenario 4 (28%) was the second most popular. The choice of a more “protective” layout with the desk separating physician and patient could be a gender-related as GPs are increasingly facing violence, harassment, and threatening behavior 10.
Computers can increase the accuracy of the patient record and enhance physician efficiency but can also negatively interfere with the physician-patient interaction . The majority of GP’s (96%) in this study reported having a computer in the room. Frankel et al. listed the possible aspects in which a computer may interfere with a consultation: organization of the visit, verbal and nonverbal behavior, computer navigation and spatial navigation of the consulting room. Frankel also stated that “computering” could affect communication, which is the most powerful instrument available to the physician 11. Sinsky and Beasley compared the risk of texting while driving to the risk of “texting while doctoring”; physicians should not practice “computer-centered medicine” 12. Therefore, consulting rooms must be designed so that the computer is not the center of care but so that it is convenient and suited to the ergonomics of the physician. The multi-tasking involved in using a computer and the flow of the patient-physician-computer interaction can be complex and stressful 11. A study conducted in Belfast examining the content of consultations with a significant psychological component showed that when the patient had a psychological complaint, physicians focused more on the patient rather than the computer and balanced their use of the computer and communication 13. Moreover, it has been shown that changing the layout of a consultation room has the potential to improve communications between patients and doctors 14. Clinicians who have more barriers integrating the computer in the consulting room could have more difficulties dealing with multi-tasking and this could have a negative effect on the physician-patient relationship 11, 15.
The patient experience is constructed consciously and unconsciously, and design affects patient perception 4, 9. Why is design layout in Europe different from the Americas? Why is scenario 3 preferred in Europe but scenario 4 preferred in the Americas? Although there is no definitive answer for these questions, it is interesting to reflect on the learning matrix from different countries and experiences.
Also note the dynamic reflected by the year of graduation. For those who graduated before 1990, the table between the patient and general practitioner is preferred (54%), and this increases to 70% for graduates between 1990–2010, and then decreases to 55% for younger GPs (graduating after 2010) who prefer scenario 4. This may reflect the emphasis on a more patient-centered approach the authors have noticed in recent years.
It has been suggested that consultation spaces need to be more adaptable so that additional family members can be included when necessary 9 and - when using the computer - preferably the patient should be able to see the computer screen 16. However, the need to understand each community and cultural competency are linked to the consulting room design. Modifying current consulting room designs should open-up new opportunities of interaction between the GP and patients.
This study has several limitations. First, the number of scenarios was limited and it was difficult to determine patient and GP locations from participants’ descriptions. This cohort of respondents represents those who have access to the Internet or knowledge of this survey - noting limited numbers of respondents from Africa, North America, and Northern Europe. The results were concentrated in some countries and continents more than others where a broader representation would likely offer better data. Furthermore, other factors such as different designs to those in the proposed scenarios, satisfaction of doctors and patients in the chosen design for the consulting room and cultural differences were not covered by this research could influence consulting room design. The studies that exist have focused mainly on the developed world experience and we were unable to expand the scope much into developing countries. Lastly, the patient’s viewpoint and preferences were not taken into consideration. Nevertheless, this study serves as an interesting starting point for further investigations to understand consulting room design worldwide and reflect upon it.
Conclusions
The position of the patient’s chair differs between and within countries in addition to distinctions based on gender and year of graduation. Modifying current consulting room designs opens up new opportunities for interaction between GPs and their patients, while continuing to remain conscious of both community and cultural differences during planning. Next steps should focus on gathering an even greater breadth of GP input as well as comparing and contrasting those to the preferences of our patients and communities.
Ethical approval
The study protocol has been approved by the Catalan Institute in Primary Care Research (IDIAP Jordi Gol) Health Care Ethics Committee (code P18/202). Prior to starting the questionnaire, participants read the following: “Dear Participant: This pilot questionnaire aims to collect data for a study about consulting room from all around the world in Family Medicine/General Practice offices. The participation and engagement in this questionnaire is free, voluntary and anonymous. Thank you for participating. -Research Team.” Participant consent was therefore obtained if the participant continued with the questionnaire.
To ensure confidentiality, all data has been anonymized.
Data availability
Underlying data
Open Science Framework: Where is the Doctor’s Chair, https://doi.org/10.17605/OSF.IO/9FWU7 17.
This project contains the following underlying data:
Spreadsheet containing anonymized questionnaire responses
Extended data
Open Science Framework: Where is the Doctor’s Chair, https://doi.org/10.17605/OSF.IO/9FWU7 17.
This project contains the following extended data:
Questionnaire
Data are available under the terms of the Creative Commons Zero “No rights reserved” data waiver (CC0 1.0 Public domain dedication).
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 1; peer review: 2 approved with reservations]
References
- 1. van den Brink-Muinen A, Verhaak PF, Bensing JM, et al. : Communication in general practice: differences between European countries. Fam Pract. 2003;20(4):478–85. 10.1093/fampra/cmg426 [DOI] [PubMed] [Google Scholar]
- 2. Almquist JR, Kelly C, Bromberg J, et al. : Consultation room design and the clinical encounter: the space and interaction randomized trial. HERD. 2009;3(1):41–78. 10.1177/193758670900300106 [DOI] [PubMed] [Google Scholar]
- 3. Dannenberg AL, Burpee H: Architecture for Health Is Not Just for Healthcare Architects. HERD. 2018;11(2):8–12. 10.1177/1937586718772955 [DOI] [PubMed] [Google Scholar]
- 4. Sheldon H, Sinayuk L, Donovan S: Designing GP buildings. Staff and patient priorities for the design of community healthcare facilities in lambeth. Oxford;2007. Reference Source [Google Scholar]
- 5. Noordman J, Verhaak P, van Beljouw I, et al. : Consulting room computers and their effect on general practitioner-patient communication. Fam Pract. 2010;27(6):644–51. 10.1093/fampra/cmq058 [DOI] [PubMed] [Google Scholar]
- 6. Rouf E, Whittle J, Lu N, et al. : Computers in the exam room: differences in physician-patient interaction may be due to physician experience. J Gen Intern Med. 2007;22(1):43–8. 10.1007/s11606-007-0112-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pearce C, Arnold M, Phillips C, et al. : The patient and the computer in the primary care consultation. J Am Med Inform Assoc. 2011;18(2):138–42. 10.1136/jamia.2010.006486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rose D, Richter LT, Kapustin J: Patient experiences with electronic medical records: lessons learned. J Am Assoc Nurse Pract. 2014;26(12):674–80. 10.1002/2327-6924.12170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jacobs K: Patient Satisfaction by Design. Semin Hear. 2016;37(4):316–24. 10.1055/s-0036-1593999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Iacobucci G: Violent crime at GP surgeries is on the rise, figures show. BMJ. 2017;358:j4236. 10.1136/bmj.j4236 [DOI] [PubMed] [Google Scholar]
- 11. Frankel R, Altschuler A, George S, et al. : Effects of exam-room computing on clinician-patient communication: a longitudinal qualitative study. J Gen Intern Med. 2005;20(8):677–82. 10.1111/j.1525-1497.2005.0163.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sinsky CA, Beasley JW: Texting while doctoring: a patient safety hazard. Ann Intern Med. 2013;159(11):782–3. 10.7326/0003-4819-159-11-201312030-00012 [DOI] [PubMed] [Google Scholar]
- 13. Chan WS, Stevenson M, McGlade K: Do general practitioners change how they use the computer during consultations with a significant psychological component? Int J Med Inform. 2008;77(8):534–8. 10.1016/j.ijmedinf.2007.10.005 [DOI] [PubMed] [Google Scholar]
- 14. Ajiboye F, Dong F, Moore J, et al. : Effects of revised consultation room design on patient-physician communication. HERD. 2015;8(2):8–17. 10.1177/1937586714565604 [DOI] [PubMed] [Google Scholar]
- 15. Kazmi Z: Effects of exam room EHR use on doctor-patient communication: A systematic literature review. Inform Prim Care. 2013;21(1):30–9. 10.14236/jhi.v21i1.37 [DOI] [PubMed] [Google Scholar]
- 16. Als AB: The desk-top computer as a magic box: patterns of behaviour connected with the desk-top computer; GPs' and patients' perceptions. Fam Pract. 1997;14(1):17–23. 10.1093/fampra/14.1.17 [DOI] [PubMed] [Google Scholar]
- 17. Hoedebecke K: Where Is the Doctor’s Chair. OSF. 2019. 10.17605/OSF.IO/9FWU7 [DOI] [Google Scholar]