Abstract
Background.
Mental disorders may emerge as the result of interactions between observable symptoms. Such interactions can be analyzed using network analysis. Several recent studies have used network analysis to examine eating disorders, indicating a core role of overvaluation of weight and shape. However, no studies to date have applied network models to binge-eating disorder (BED), the most prevalent eating disorder.
Methods.
We constructed a cross-sectional graphical LASSO network in a sample of 788 individuals with BED. Symptoms were assessed using the Eating Disorders Examination Interview. We identified core symptoms of BED using expected influence centrality.
Results.
Overvaluation of shape emerged as the symptom with the highest centrality. Dissatisfaction with weight and overvaluation of weight also emerged as highly central symptoms. On the other hand, behavioral symptoms such as binge eating, eating in secret, and dietary restraint/restriction were less central. The network was stable, allowing for reliable interpretations (centrality stability coefficient = 0.74).
Conclusions.
Overvaluation of shape and weight emerged as core symptoms of BED. This trend is consistent with past network analyses of eating disorders more broadly, as well as literature that suggests a primary role of shape and weight concerns in BED. Although DSM-5 diagnostic criteria for BED does not currently include a cognitive criterion related to body image or shape/weight overvaluation, our results provide support for including shape/weight overvaluation as a diagnostic specifier.
Keywords: Binge-eating disorder, eating disorders, network analysis, overvaluation of shape/weight, psychopathology
Traditional approaches to psychopathology have conceptualized symptoms of mental disorders as emerging from a latent common cause (Borsboom et al., 2003). This latent model theory posits that underlying latent variables representing psychological disorders produce symptoms that are experienced by individuals with these disorders. More recent theoretical approaches have described how these symptoms might influence one another in a dynamic and casual network, rather than existing independently. The network model has emerged as a novel way to conceptualize psychological disorders, replacing the notion that psychological disorders themselves are the underlying cause of symptoms, or that symptoms are implicitly reflective of certain psychological disorders (Borsboom and Cramer, 2013). Instead, the network approach views symptoms of mental disorders as distinct entities that can influence, maintain, and/or interact with other symptoms (McNally, 2016).
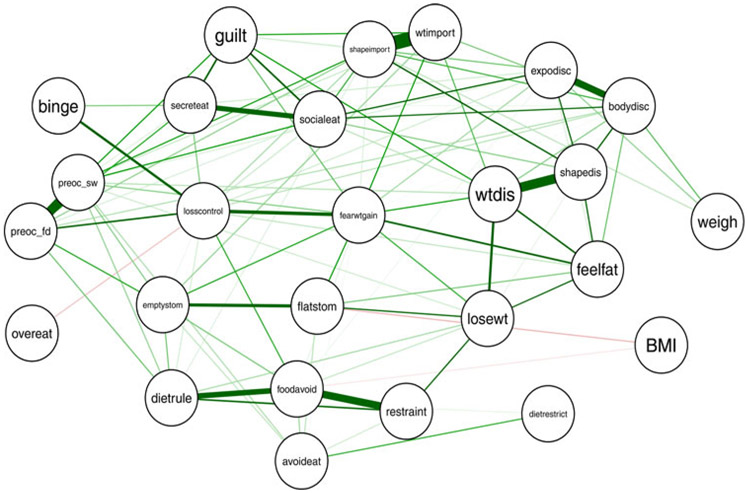
Network analysis allows for a depiction and quantification of the symptoms are most central to a disorder, as well as the strength by which symptoms react with and influence one another (Borsboom and Cramer, 2013; McNally, 2016; Fried et al., 2017). In a network model, symptoms are represented as individual nodes, connected by edges that depict the strength (e.g. strong correlation) and direction (e.g. positive correlation) between pairs of symptoms. Thicker edges indicate stronger associations between symptoms, with positive associations typically depicted in green and negative associations typically depicted in red. Central symptoms are nodes that demonstrate many strong connections to other nodes, a greater number of connections with other nodes, and nodes that serve as ‘hubs’ between other, disconnected, nodes (Freeman, 1978). Since its introduction to the study of psychopathology, clinical researchers have applied network analysis to examine psychopathology networks and to identify the core symptoms of many psychological disorders including depression (Fried et al., 2016; McNally et al., 2017), anxiety (Beard et al., 2016; Heeren and McNally, 2016), obsessive-compulsive disorder (Jones et al., 2018), and posttraumatic stress disorder (McNally et al., 2015; Armour et al., 2017).
More recent research has also begun to apply network analysis to eating disorders. Levinson et al. (2017) examined a psychopathology network of bulimia nervosa (BN) and found that fear of weight gain was central to the BN network. Other studies have examined eating-disorder psychopathology networks among mixed diagnostic groups comprised primarily of individuals with anorexia nervosa (AN), BN, and other specified feeding and eating disorders (OSFED; Forbush et al., 2016; Dubois et al., 2017; Forrest et al., 2018). Findings from these studies largely indicate that symptoms involving weight and shape concerns, including overvaluation of shape and weight and body checking, are central in networks of eating-disorder psychopathology. Thus, the emerging literature suggests that cognitive symptoms related to overvaluation and/or concerns with weight and shape appear to be core symptoms of eating disorders, at least among individuals with AN, BN, and OSFED. However, it is important to note that the majority of previous studies have relied on self-report questionnaires to assess eating disorder symptoms, which may not capture some of the symptoms as well as semi-structured investigator-based clinical interviews, particularly for some complex behavioral features (such as binge eating) and cognitive-evaluative features (such as overvaluation of shape/weight) as indicated by previous comparative research (Wilfley et al., 1997; Grilo et al., 2001a, 2001b).
To date, no studies have applied network models to examine the core psychopathology of binge-eating disorder (BED). BED, which is characterized by recurrent episodes of binge eating (i.e. eating objectively large amounts of food while experiencing a subjective loss of control over eating), marked distress about binge eating, and the absence of inappropriate compensatory behaviors (e.g. self-induced vomiting), is the most prevalent eating disorder and is associated with psychosocial impairment (Udo & Grilo, 2018).
Unlike other eating disorder diagnoses (e.g. AN, BN), the diagnostic criteria for BED does not include a cognitive criterion related to body image or shape/weight overvaluation (Grilo, 2013). Research has indicated that overvaluation of shape and weight is associated with significantly greater eating-disorder psychopathology and depression among individuals with BED (Grilo et al., 2008, 2010; Goldschmidt et al., 2010) and appears to be a better indicator of severity than the current DSM-5 severity specifier of binge-eating frequency (Grilo et al., 2015). Therefore, cognitive eating disorder symptoms involving overvaluation of shape and weight, or related constructs of body image, may also be critically important and core symptoms in BED. If cognitive symptoms relating to weight and shape are central to a BED network, this would refine approaches to assessment and diagnosis (Grilo, 2013) and inform efforts ability to design well-specified treatments to target key symptoms of this disorder.
Therefore, the current study aimed to apply network analysis to examine the psychopathology of BED among a large sample of treatment-seeking patients with BED, as well as to identify the most central and influential symptoms of BED. Given previous research demonstrating the importance of overvaluation of shape and weight in BED (Grilo et al., 2008, 2010; Goldschmidt et al., 2010) and emerging findings on the centrality of weight/shape overvaluation in other eating disorder networks (e.g. Forbush et al., 2016; Dubois et al., 2017; Forrest et al., 2018), we hypothesized that symptoms reflecting overvaluation of shape and weight, as well as dissatisfaction with shape and weight, would be central to the network.
Methods
Participants
Participants in the current study were 788 individuals (74.2% female, 73.8% White) between 18 and 65-years-old (M = 45.62, s.d. = 9.86) who responded to advertisements for psychosocial and medication treatment studies for BED at an urban, medical-school-based program. Participants met full DSM-IV criteria for BED, and had a mean body mass index (BMI) of 38.07 (s.d. = 6.80). Participants were excluded if they were receiving treatment for eating/weight concerns, had uncontrolled medical conditions that influenced eating/weight (e.g. diabetes), had a severe mental illness that could interfere with clinical assessment (e.g. psychosis), or were pregnant. This study received approval from the university’s ethical review board; all enrolled participants provided written informed consent.
Measures
Trained doctoral-level research clinicians, monitored to maintain reliability, evaluated participants. Research clinicians administered the Structured Clinical Interview for DSM-IV Axis I Disorders (First et al., 1997) to determine DSM-IV-based BED diagnosis and age of onset, and the semi-structured Eating Disorder Examination (EDE) (Fairburn & Cooper, 1993) to confirm the BED diagnosis and to characterize eating-disorder psychopathology used in this study.
Eating disorder examination
The EDE (Fairburn & Cooper, 1993) is an investigator-based interview that evaluates eating-disorder psychopathology in the past 28 days, and over longer intervals corresponding to diagnostic criteria. The EDE assesses three types of eating episodes: objective binge episodes (OBEs, eating an unusually large amount of food while perceiving a loss of control over eating; this is the DSM-IV definition of binge eating episodes), subjective binge episodes (SBEs, eating a small or typical amount of food while perceiving a loss of control) and objective overeating episodes (OOEs, eating an unusually large amount of food without perceiving a loss of control). Four subscales reflect eating-disorder features (Restraint, Eating Concern, Shape Concern, and Weight Concern), as well as a Global severity score. The EDE has demonstrated good inter-rater and test-retest reliability in BED (Grilo et al., 2004). In the present study, inter-rater reliability was examined in 113 cases; intraclass correlation coefficient for OBEs was 0.94, Global severity score was 0.92, Restraint was 0.92, Eating Concern was 0.78, Weight Concern was 0.91, and Shape Concern was 0.94.
Data analytic plan
Graphical lasso
We computed and visualized regularized partial correlation networks using a graphical LASSO (Least Absolute Shrinkage and Selection Operator) using the R packages glasso (Friedman et al., 2018) and qgraph (Epskamp et al., 2018). The graphical LASSO first computes a partial correlation network among all variables, which provides associations between pairs of symptoms while controlling for the influence of other variables. Next, the LASSO applies an L1 penalty to shrink trivially small correlations to zero, thereby removing potentially spurious correlations and returning a sparse network of only the largest, potentially causal, edges. Visual inspection of this network graph provides a preliminary identification of central nodes (i.e. symptoms), as well as the strength of associations between pairs of nodes.
We computed two graphical LASSO networks. The first network included symptoms assessed in the EDE that were plausible causal candidates in the etiology and maintenance of BED, including behavioral symptoms (e.g. binge eating) and cognitive symptoms (e.g. overvaluation of shape/weight). We did not include compensatory behaviors (e.g. self-induced vomiting) because these symptoms showed little variation at the individual level and are not part of the presentation of BED. In addition to running a network analysis with all symptoms included, we computed and visualized a second graphical LASSO network that did not include cognitive symptoms related to shape/weight overvaluation and dissatisfaction.
Expected influence
We identified the most central symptoms in the network by calculating the one-step expected influence (Robinaugh et al., 2015) using the networktools package (Jones, 2017). Compared with other measures of centrality, expected influence provides a more accurate measure of node centrality that takes negative edges (i.e. negative correlations between symptoms) into account. We conducted a 1000-sample bootstrap to estimate the stability of the expected influence values.
Results
Figure 1 displays the regularized partial correlation network for BED psychopathology; Table 1 provides a key for all node names included in the network analyses. In the network model, green edges represent positive regularized correlations between nodes and red edges represent negative regularized correlations between nodes. Edge thickness signifies correlation magnitude, such that thicker edges represent stronger regularized correlations.
Fig. 1.
Regularized partial correlation network for binge-eating disorder (BED). Each node represents a symptom; each edge represents the regularized partial correlation between symptoms. Green and red edges represent positive and regularized correlations, respectively; thicker edges represent stronger correlations.
Table 1.
Network node names for EDE symptoms
| Node name | EDE symptom |
|---|---|
| Avoideat | Avoidance of eating |
| Binge | OBE (past month) |
| Bodydisc | Discomfort seeing body |
| Bmi | Body mass index |
| Dietru le | Dietary rules |
| Dietrestrict | Dietary restriction outside of bulimic episodes |
| Emptystom | Empty stomach |
| Expodisc | Avoidance of exposure |
| Fearwtgain | Fear of weight gain |
| Feelfat | Feelings of fatness |
| Flatstom | Flat stomach |
| Foodavoid | Food avoidance |
| Guilt | Guilt about eating |
| Losewt | Desire to lose weight |
| Losscontrol | Fear of losing control over eating |
| Overeat | Objective overeating |
| preoc_sw | Preoccupation with shape or weight |
| Restraint | Restraint over eating |
| Secreteat | Eating in secret |
| Shapedis | Dissatisfaction with shape |
| Shapeimport | Importance of shape |
| Socialeat | Social eating |
| Weigh | Reaction to prescribed weighing |
| Wtdis | Dissatisfaction with weight |
| Wtimport | Importance of weight |
| preoc_fd | Preoccupation with food, eating, or calories |
EDE, eating disorders examination.
Overvaluation of shape and overvaluation of weight were strongly associated with each other, as were shape dissatisfaction and weight dissatisfaction, as well as preoccupation with shape/weight and preoccupation with food, eating, and calories (see Fig. 1). Binge eating was moderately associated with loss-of-control eating and weakly associated with eating in secret. BMI was negatively associated with the desire to have a flat stomach and avoidance of food.
Figure 2 shows the one-step expected influence values for all eating disorder symptoms. Overvaluation of shape (i.e. shape importance in self-evaluation) emerged as the symptom with the highest influence, as computed via associations with all adjacent nodes. Dissatisfaction with weight and overvaluation of weight also emerged as highly central symptoms in the network. On the other hand, behavioral symptoms such as binge eating, eating in secret, and dietary restraint/restriction were less central in the network. BMI was the least central node in the network, with minimal influence on adjacent nodes. Stability of the network was good, with a centrality stability coefficient of 0.74.
Fig. 2.
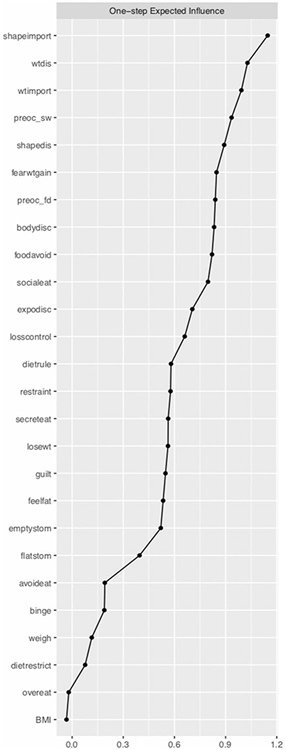
One-step expected influence values for each node in the binge-eating disorder (BED) network. Nodes with higher expected influence values are more central to the BED network. Nodes are listed in order of descending expected influence.
In addition, we computed a second regularized partial correlation network with all cognitive symptoms related to shape/weight overvaluation and dissatisfaction excluded (see online Supplementary Fig. S1). Results from this network indicated that food avoidance was strongly associated with restraint over eating and following dietary rules, and that concern/avoidance of social eating was strongly associated with eating in secret and guilt about eating. Online Supplementary Fig. S2 shows the one-step expected influence values for all nodes. Food avoidance emerged as the symptom with the highest influence. Preoccupation with food, eating, and calories, as well as concern/avoidance of social eating also emerged as highly central symptoms in the network. On the other hand, behavioral symptoms such as overeating, as well as BMI and reaction to prescribed weighing, were the least central nodes in the network. Online Supplementary Fig. S3 shows a comparison of expected influence between the fust network with all symptoms included, and the second network without cognitive symptoms related to shape/weight overvaluation and dissatisfaction.
Discussion
This study is the first to apply network analysis to examine the core psychopathology of BED. Consistent with our hypothesis, symptoms concerning shape and weight emerged as central to the BED network in a large, treatment-seeking sample. More specifically, overvaluation of shape emerged as the most central node in the network. On the other hand, behavioral features of BED (e.g. binge eating) were peripheral to the network, indicating that they had less coherence to the rest of the network as compared with other nodes. BMI was similarly peripheral to the network and had the lowest expected influence of all nodes, suggesting that BMI is not a central feature to the psychopathology of BED. Additionally, such results indicate that overvaluation of shape and weight, and other associated symptoms in BED, do not reflect concerns or distress about excess weight (Grilo, 2013). Findings from the current study provide further support for the importance of overvaluation of shape and weight in BED (Grilo, 2013) suggesting that these symptoms appear to constitute core symptoms for the disorder. Indeed, in a network model with cognitive symptoms related to weight/shape overvaluation and dissatisfaction excluded, no symptoms showed as a strong expected influence as overvaluation symptoms in the original network. More broadly, these results replicate previous findings in network analyses of AN (Forrest et al., et al., 2018), BN (Levinson et al., 2017), and mixed diagnostic groups (Dubois et al., 2017), which also identified shape and weight symptoms and overvaluation of shape and weight as core to eating-disorder psychopathology, and extends these findings to a clinical sample of treatment-seeking patients with BED assessed using reliably-administered investigator-based clinical interview. Collectively, this emerging literature provides empirical support for the transdiagnostic theory of eating disorders, which posits that overvaluation of shape/weight constitutes the core psychopathology of eating disorders (Fairburn et al., 2003).
In addition to identifying central features of disorders, findings from network analyses also have important clinical implications. Identification of core symptoms can inform more targeted clinical interventions. For example, certain empirically-supported psychological treatments for BED (Grilo, 2017), such as cognitive-behavioral therapy (CBT), and lifestyle behavioral weight loss therapy, assist patients in developing behavioral strategies to normalize and regulate eating patterns. CBT additionally assists patients in identifying and modifying relevant cognitive processes including weight/shape concerns. The added ‘cognitive’ focus of CBT might perhaps account for its longer-term advantages of over behavioral approaches for BED (Wilson et al., 2010; Grilo et al., 2011) and BN (Fairburn et al., 1993a, 1993b). Consistent with that speculation are findings that overvaluation of shape/weight predicts poorer treatment outcomes for BED (Grilo et al., 2013a, 2013b) and for BN (Fairburn et al. 1993a, 1993b), and, more importantly, has been found to moderate treatment outcomes such as those patients with BED with overvaluation derive substantially greater benefit from CBT than from pharmacotherapy (Grilo et al., 2013a, 2013b).
However, even with these ‘leading’ treatments, a substantial portion of patients do not achieve remission from binge-eating 0 (Grilo, 2017; Wilson et al., 2007). Our findings here (i.e. BMI and many behavioral symptoms had limited connections to the overall psychopathology network) might suggest that directly modifying behavioral patterns of binge eating or focusing on weight loss may not suffice over time because those changes might not extend to improvements in other aspects of BED symptoms. Indeed, evolving refinements of CBT (i.e. CBT-E; Fairburn, 2008) have included additional emphasis on overvaluation along with specific ‘modules’ to more directly target such cognitive features. The CBT-E model emphasizes overvaluation as a maintaining mechanism for eating disorders and outlines different methods to target it with patients. Our empirical findings here reinforce further those clinical views and the need to more closely target the ways in which overvaluation influences other behavioral and cognitive features of BED beyond just identifying and restructuring those cognitions. Our findings suggest that decreasing the strength of the associations between overvaluation with the other symptoms (i.e. not just reducing the severity of overvaluation) could further improve treatment outcomes.
Findings for the current study should be considered in the context of the limitations. Although our large, relatively diverse clinical sample assessed rigorously using interviews administered by trained and monitored doctoral research-clinicians, is a strength of the study, the generalizability of our results to non-treatment-seeking or community samples of individuals with BED is unknown. Future studies should include individuals with BED from non-treatment seeking and community samples to examine whether core symptoms differ across these populations. In addition, concerns have been raised regarding the generalizability of networks across samples. To address this concern, we used a graphical LASSO to minimize trivially small correlations. We also conducted a 1000-sample bootstrap to assess stability and accuracy of estimations included in the network, finding that expected influence was a stable index of centrality (Epskamp et al., 2018). Further research is needed to identify whether the group characteristics identified in this study extend to the individual level, and to elucidate the direction and causality of relationships between symptoms. Finally, the cross-sectional nature of this study limits our ability to distinguish temporal relationships between symptoms. Future research should use longitudinal designs to characterize naturalistic and treatment-based changes in BED networks over time. Such studies could allow us to identify prognostic variables for differential response to treatment in patients, as well as provide additional information to bolster the causal symptom relationships proposed by the network approach.
In summary, this study was the first to apply network analysis to examine the psychopathology of BED. Our findings suggest that overvaluation of shape and weight was central to the BED network, while behavioral features of BED and BMI were more peripheral. This provides additional evidence for the centrality of cognitive features, particularly overvaluation of shape and weight, in BED that warrants greater consideration in the diagnosis and treatment of BED, especially in light of its negative prognostic significance (Grilo et al., 2013a, 2013b).
Supplementary Material
Acknowledgements.
This research was supported by Grant No. R01 DK49587 from the National Institutes of Health (PI: Grilo). Shirley B. Wang is supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-1745303. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Science Foundation.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718002702.
References
- Armour C, Fried EI, Deserno MK, Tsai J and Pietrzak RH (2017) A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. Journal of Anxiety Disorders 45, 49–59. [DOI] [PubMed] [Google Scholar]
- Beard C, Millner AJ, Forgeard MJC, Fried EI, Hsu KJ, Treadway M and Björgvinsson T (2016) Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine 46, 3359–3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Mellenbergh GJ, Van Heerden J (2003) The theoretical status of latent variables. Psychological Review 110, 203–219. [DOI] [PubMed] [Google Scholar]
- Borsboom D and Cramer AOJ (2013) Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Dubois RH, Rodgers RF, Franko DL, Eddy KT and Thomas JJ (2017) A network analysis investigation of the cognitive-behavioral theory of eating disorders. Behaviour Research and Therapy 97, 213–221. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D and Fried E (2018) Estimating psychological networks and their accuracy: a tutorial paper. Behavior Research Methods 50, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z (1993) The eating disorder examination In Binge Eating: Nature, Assessment, and Treatment (ed. Fairburn CG and Wilson GT GT), pp. 317–360. Guilford Press, New York. [Google Scholar]
- Fairburn CG (2008) Cognitive Behavioral Therapy and Eating Disorders. Guilford, NY: Guilford Press. [Google Scholar]
- Fairburn CG, Jones R, Peveler RC, Hope RA and O’Connor M (1993a) Psychotherapy and bulimia nervosa: Longer-term effects of interpersonal psychotherapy, behavior therapy, and cognitive behavior therapy. Archives of General Psychiatry 50, 419–428. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Peveler RC, Jones R, Hope RA and Doll HA (1993b) Predictors of 12-month outcome in bulimia nervosa and the influence of attitudes to shape and weight. Journal of Consulting and Clinical Psychology 61, 696–698. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z and Shafran R (2003) Cognitive behaviour therapy for eating disorders: a ‘transdiagnostic’ theory and treatment. Behaviour Research and Therapy 41, 509–528. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (1997) Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0) New York: New York State Psychiatric Institute. [Google Scholar]
- Forbush KT, Siew CSQ and Vitevitch MS (2016) Application of network analysis to identify interactive systems of eating disorder psychopathology. Psychological Medicine 46, 2667–2677. [DOI] [PubMed] [Google Scholar]
- Forrest LN, Jones PJ, Ortiz SN and Smith AR (2018) Core psychopathology in anorexia nervosa and bulimia nervosa: a network analysis. International Journal of Eating Disorders. [DOI] [PubMed] [Google Scholar]
- Freeman LC (1978) Centrality in social networks conceptual clarification. Social Networks 1, 215–239. [Google Scholar]
- EI Fried, Epskamp S Nesse RM, Tuerlinckx F and Borsboom D (2016) What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. . Journal of Affective Disorders 189, 314–320. [DOI] [PubMed] [Google Scholar]
- EI Fried, van Borkulo CD Cramer AOJ, Boschloo L Schoevers RA and Borsboom D (2017) Mental disorders as networks of problems: a review of recent insights. Social Psychiatry and Psychiatric Epidemiology 52, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Hastie T, Tibshirani R (2018) Glasso: Graphical Lasso: Estimation of Gaussian Graphical Models. R package version 1.10 https://CRAN.R-project.org/package=glasso
- Goldschmidt AB, Hilbert A, Manwaring JL, Wilfley DE, Pike KM, Fairburn CG and Striegel-Moore RH (2010) The significance of overvaluation of shape and weight in binge eating disorder. Behaviour Research and Therapy 48, 187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM (2013) Why no cognitive body image feature such as overvaluation of shape/weight in the binge eating disorder diagnosis? International Journal of Eating Disorders 46, 208–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM (2017) Psychological and behavioral treatments for binge-eating disorder. Journal of Clinical Psychiatry 78, 20–24. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM and Wilson GT (2001a) A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. Journal of Consulting and Clinical Psychology 69, 317–322. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM and Wilson GT (2001b) Different methods for assessing the features of eating disorders in patients with binge eating disorder: a replication. Obesity Research 9, 418–422. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Bianco C and Barry DT (2004) Reliability of the eating disorder examination in patients with binge eating disorder. International Journal of Eating Disorders 35, 80–85. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ and Masheb RM (2008) Overvaluation of shape and weight in binge eating disorder and overweight controls: refinement of a diagnostic construct. Journal of Abnormal Psychology 117, 414–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM and White MA (2010) Significance of overvaluation of shape/weight in binge-eating disorder: comparative study with overweight and bulimia nervosa. Obesity 18, 499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT, Gueorguieva R and White MA (2011) Cognitive–behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: a randomized controlled trial. Journal of Consulting and Clinical Psychology 79, 675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM and Crosby RD (2013a) Predictors and moderators of response to cognitive behavioral therapy and medication for the treatment of binge eating disorder. Journal of Consulting and Clinical Psychology 80, 897–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, White MA, Gueorguieva R, Wilson GT and Masheb RM (2013b) Predictive significance of the overvaluation of shape/weight in obese patients with binge eating disorder: findings from a randomized controlled trial with 12-month follow-up. Psychological Medicine 43, 1335–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Ivezaj V and White MA (2015) Evaluation of the DSM-5 severity indicator for binge eating disorder in a community sample. Behaviour Research and Therapy 66, 72–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren A and McNally RJ (2016) An integrative network approach to social anxiety disorder: the complex dynamic interplay among attentional bias for threat, attentional control, and symptoms. Journal of Anxiety Disorders 42, 95–104. [DOI] [PubMed] [Google Scholar]
- Jones P (2017) networktools: Tools for Identifying Important Nodes in Networks. R package version 1.1.0 https://CRAN.R-project.org/package=networktools
- Jones PJ, Mair P, Riemann BC, Mugno BL and McNally RJ (2018) A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. Journal of Anxiety Disorders 53, 1–8. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Zerwas S, Calebs B, Forbush K, Kordy H, Watson H, Hofmeier S, Levine M, Crosby RD, Peat C, Runfola CD, Zimmer B, Moesner M, Marcus MD, Bulik CM (2017) The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. Journal of Abnormal Psychology 126, 340–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ (2016) Can network analysis transform psychopathology? Behaviour Research and Therapy 86, 95–104. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK and Borsboom D (2015) Mental disorders as causal systems. Clinical Psychological Science 3, 836–849. [Google Scholar]
- McNally RJ, Mair P, Mugno BL and Riemann BC (2017) Co-morbid obsessive-compulsive disorder and depression: a Bayesian network approach. Psychological Medicine 47, 1204–1214. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ and McNally RJ (2015) Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology 125, 747–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T and Grilo CM (2018) Prevalence and correlates of DSM-5 eating disorders in nationally representative sample of United States adults. Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG (1997) Assessing the specific psychopathology of binge eating disorder patients: Interview or self-report? Behaviour Research and Therapy 35, 1151–1159. [PubMed] [Google Scholar]
- Wilson GT, Grilo CM and Vitousek KM (2007) Psychological treatments of eating disorders. American Psychologist 62, 199–216. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS and Bryson SW (2010) Psychological treatments of binge eating disorder. Archives of General Psychiatry 67, 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.