Abstract
Background:
Both parent-child relationship quality (PCRQ) and sleep are important for health and development, but few studies have examined links between PCRQ and adolescent sleep, and potential interactions by race/ethnicity or sex.
Methods:
We used cross-sectional data from 6,019 participants (mean = 15.9 years; 50% male; 66% non-Hispanic White, 16% non-Hispanic Black, 5% Hispanic all races) from the National Longitudinal Study of Adolescent to Adult Health, a nationally representative sample of U.S. adolescents. Our exposure was current adolescent-rated PCRQ score. Outcomes were adolescents’ reports of chronic insufficient sleep, sleep duration (mins), and frequency of insomnia symptoms (i.e., trouble falling or staying asleep “almost every day”/“every day” versus “never”/“just a few times”/“about once a week”).
Results:
Adjusting for demographic characteristics, each 1-point increase in PCRQ score was associated with lower odds of insomnia symptoms (odds ratio [OR] = 0.92, 95% confidence interval [CI]: 0.90, 0.94), chronic insufficient sleep (OR = 0.93, 95% CI: 0.91, 0.95), and longer sleep duration (B = 2.56, 95% CI: 1.90, 3.22). After adjustment for depressive symptoms, the association with insomnia symptoms was no longer statistically significant. Race/ethnicity moderated the association between PCRQ and chronic insufficient sleep such that the magnitude of the association was greater in Hispanics vs. Whites and Blacks. There were no interactions of PCRQ with sex.
Conclusions:
Among adolescents, better PCRQ was associated with better sleep, and this association varied by race/ethnicity for perceived chronic insufficient sleep. Longitudinal studies with objective and subjective sleep measures are needed to further understand these associations.
Keywords: adolescents, parent-child relationship quality, insomnia, sleep duration
Introduction
Chronic sleep insufficiency in adolescence is the norm in modern-day society.1 Although the recommended sleep duration for adolescents is 8–10 hours per night,2 45% reported < 8 hours on school nights according to the National Sleep Foundation’s Sleep in America Poll.3 A U.S.-based cohort study found that 20–25% of adolescents reported < 6 hours per night.4 Chronic insufficient sleep in adolescence can be attributed to a biological shift toward a later bedtime preference and factors like early school start times and electronic media.5 Insomnia symptoms, defined as complaints of difficulty falling or staying asleep, early morning awakenings, or unrefreshing sleep despite adequate opportunity, are another major concern among adolescents.6 Estimates of insomnia symptom prevalence range from 14–40%,7,8 with a 10.7% lifetime prevalence of insomnia disorder in this group.9 Sleep disturbances such as these are associated with numerous negative outcomes in adolescents, including depression, suicidal ideation, substance use, drowsy driving, obesity,5 and poor academic performance.10 Thus, identifying modifiable factors that may influence adolescent sleep is of critical importance.
Numerous studies have demonstrated the significance of optimal parent-child bonding for health and development.11 Developmental theory suggests that the parent-child relationship may also be a driver of adolescent sleep health. During puberty, systems associated with vigilance and threat perception undergo significant development.13 Sleep initiation and maintenance necessitate downregulation of these systems, which requires feelings of safety and security.13 Evolutionarily, experiencing these feelings during sleep stemmed from being surrounded by a protective social group.14 In adolescents, warmth and connectedness in the parent-child relationship may promote feelings of safety and security.15 Research investigating the association between parent-child relationship quality (PCRQ) and sleep characteristics, however, is scarce.16
Among the few such studies that have been conducted, two in adults found that retrospective reports of better parental bonding during childhood were associated with better sleep in adulthood.17,18 One of these, in Japan, found that bonding with the same-sex parent was most strongly associated with adulthood sleep.17 Among younger children, better parental bonding has been linked with longer sleep duration and less disturbed sleep,19–21 with more mixed findings in adolescents. Some adolescent studies found no parental bonding-sleep association,19,22,23 while others tied better parental bonding to longer sleep duration, greater sleep efficiency, less wake after sleep onset, lower sleep variability, shorter sleep onset latency, earlier bedtimes, and better sleep quality.24–26 These prior studies have several limitations. First, only one was in a nationally representative U.S. sample,19 limiting generalizability of results. Second, despite the finding in adults that the association between PCRQ and sleep varied by sex,17 and another study that found that PCRQ was only associated with sleepiness among racial/ethnic minority adolescents,26 few studies have examined sex or race/ethnicity as potential moderators. Third, although poorer PCRQ is associated with depressive symptoms among adolescents,11 and depressive symptoms are linked to poorer sleep,5 few studies have examined depressive symptoms as an important confounder or perhaps mediator of the PCRQ-sleep association.17,18,24,25
To advance the literature on PCRQ and sleep, we investigated in a nationally representative sample of U.S. adolescents, cross-sectional associations of adolescent perceived PCRQ with sleep outcomes of high relevance to adolescents: perceived chronic sleep insufficiency, sleep duration, and insomnia symptoms. To fill gaps in previous research, we examined whether associations between PCRQ and sleep varied by sex or race/ethnicity, and performed additional analyses adjusting for depressive symptoms.
Methods
Participants and Procedure
We studied participants enrolled in the National Longitudinal Study of Adolescent to Adult Health (Add Health). Add Health is an ongoing, prospective, nationally representative sample of U.S. adolescents (N = 20,745) in grades 7–12 (Wave I), during the 1994–1995 school year. Sampling for Add Heath consisted of selection of a stratified sample of schools, with the probability of selection for each school proportional to the size of the school. Additional details about the Add Health study design and methods have been reported elsewhere.27 For the current cross-sectional study we used the public use Wave I dataset, which contains data from 6,504 participants. Of these, 6,103 (weighted % = 93.6) had complete data on PCRQ, and 6,088 (99.8%) of these had complete data for the sleep outcomes of interest. Sixty-nine (1.2%) were missing data on a covariate of interest (i.e. age, sex, race/ethnicity, or parental receipt of public assistance), leaving an analytic sample of 6,019 participants with complete PCRQ, sleep, and relevant covariate data. Informed consent procedures were established and followed in accordance with the University of North Carolina School of Public Health Institutional Review Board. This secondary analysis is not considered human subjects research, because data were publicly available and de-identified.
Measures
Parent-child relationship quality (PCRQ)
The PCRQ questionnaire is a 5-item measure that assesses adolescent perception of their current relationship with each parent on a 5-point Likert-type scale.28 The first three items asked “Do you agree or disagree with the following statement”: 1. “Most of the time, your mother/father is warm and loving toward you.”; 2. “You are satisfied with the way your mother/father and you communicate with each other.”; and 3. “Overall, you are satisfied with your relationship with your mother/father.” Response options ranged from “1 = strongly agree” to “5 = strongly disagree”. The last two items asked: 4. “How close do you feel to your mother/father?”; and 5. “How much do you feel that your parents care about you?”; response options ranged from “1 = not at all” to “5 = very much”. Items 1–3 were reverse scored; higher scores indicated better PCRQ. To score the questionnaire, we first created a separate summary score for each parent. We calculated Cronbach’s alpha (α) to quantify internal consistency reliability, which was good for mothers (α = 0.83) and fathers (α = 0.79). Because mother-child and father-child relationship quality scores were correlated (r = 0.53, p < 0.001) and 92% of the sample only had data for one parent (mothers only: N = 5,505, fathers only: N = 9, both: N = 505), we created a composite score for both parents by 1) averaging the mother and father scores for each of the first 4 items that ask about each parent and summing these average scores; and 2) adding this sum to item-5 scores. We did so because item 5 asks about both parents together, as opposed to the first 4 items, which query about each parent individually. Internal consistency reliability for the composite score for both parents was good (α = 0.82). For adolescents with data from only one parent, the summary score for that parent was used, consistent with previous Add Health analyses using this measure.28 Scores could range from 5 to 25.
Chronic insufficient sleep, sleep duration, insomnia symptoms
To quantify perceived habitual sleep sufficiency, participants were asked “Do you usually get enough sleep” (yes = 0, no = 1). Sleep duration was assessed by “How many hours of sleep do you usually get?”; responses were made in integers. To facilitate interpretation, we transformed sleep duration from hours to minutes. To assess insomnia symptoms, participants were asked “In the past 12 months, how often have you had trouble falling asleep or staying asleep?”, with response options: never (N = 2,500); just a few times (N = 2,151); “about once a week” (N = 804); “almost every day” (N = 400); or “every day” (N = 164). We constructed a binary variable with answers of “almost every day” and “every day” considered positive for insomnia symptoms.
Depressive symptoms
A modified 19-item version of the Center for Epidemiologic Studies Depression Scale (CES-D) adapted for use with adolescents was used to assess past-week self-reported depressive symptoms.29 Responses were measured on a 4-point Likert-type scale. Positive items were reverse coded, and we excluded the sleep-related item from the total score to avoid overlap with our sleep-related outcomes, yielding an 18-item scale. Internal consistency reliability was good (α = 0.86). Higher scores indicate greater depressive symptoms; scores could range from 0–54.
Additional covariates
We calculated participant age by subtracting their birth year from the year of the interview and categorizing it as: 12–14 years; 15–16 years; 17–18 years; and > 18 years. Participants reported their sex (male or female). Race/ethnicity, based on self-identification, was coded as: Non-Hispanic White; Hispanic all races; Non-Hispanic Black or African American; Non-Hispanic Asian; Non-Hispanic Native American; and Non-Hispanic Other. Given substantial missing data for parental annual income (weighted % = 21.7), we constructed a binary variable for parental receipt of public assistance as a proxy for socioeconomic status,30 with a score of 1 assigned if either residential parent in a two-parent household or the sole parent in a single-parent household received public assistance per adolescent report.
Data Analysis
To generate unbiased estimates and retain national representativeness, we applied sampling weights and a variable to identify clustering within schools using the survey software package in Stata version 15.0 (StataCorp, College Station, TX). We calculated descriptive statistics for the entire sample and used chi-square and two-sample t-tests to compare participant characteristics by insomnia symptoms (yes vs. no) and chronic insufficient sleep (yes vs. no). We fit logistic regression models to examine associations of PCRQ score with each binary sleep outcome of interest (i.e., chronic insufficient sleep (yes vs. no (reference)) and insomnia symptoms (yes vs. no (reference)), and linear regression to examine the association of PCRQ with sleep duration in minutes. For each outcome, we fit 3 models: Model 1 (unadjusted); Model 2 (adjusted for age, sex, race/ethnicity, and receipt of public assistance); and Model 3 (Model 2 covariates + modified CES-D score).
To determine whether the association of PCRQ score with sleep outcomes differed by race/ethnicity or sex, we added interaction terms to Model 3 for each outcome (i.e., PCRQ x race/ethnicity, PCRQ x sex). We performed interaction tests using the Wald test, and if significant, we repeated analyses stratified by racial/ethnic category or sex, visually investigated potential between-groups differences (i.e., non-overlapping 95% CIs), and evaluated whether observed between-group differences were statistically significant using linear combinations of estimator tests. For all analyses, a p-value < 0.05 was considered statistically significant.
We conducted sensitivity analyses removing potential outliers (n = 36) for the sleep duration outcome and repeating analyses. Outliers were identified as sleep duration ± 3 SDs from the mean (i.e., < 216.6 minutes and > 720.6 minutes).31
Results
Overall, 93.7% of participants were ≤ 18 years of age, 49.8% of participants were female, 10.6% reported parental receipt of public assistance, 66.0% were Non-Hispanic White, 4.9% were Hispanic all races, and 15.5% Non-Hispanic Black (Table 1). Modified CES-D scores were skewed toward lower scores, median = 9 (interquartile range (IQR) = (5, 14); Range: 0–47), and the PCRQ scores were skewed toward higher scores, median = 22.5 (IQR = (21, 25); Range: 6–25). A total of 25.4% of adolescents reported chronic insufficient sleep, 9.8% reported insomnia symptoms, and 4.6% reported both (all weighted %s). Sleep duration was approximately normally distributed, with a mean of 471.65, SE = 2.47. There were no significant differences in age, sex, or race/ethnicity between participants with and without insomnia symptoms; however, participants with insomnia symptoms did significantly differ from participants without insomnia symptoms on receipt of public assistance, modified CES-D score (i.e., depressive symptoms), PCRQ score, and sleep duration. In participants with and without chronic insufficient sleep, significant differences in age, sex, modified CES-D score, PCRQ score, and sleep duration emerged. There were no differences by chronic insufficient sleep in race/ethnicity or public assistance.
Table 1.
Participant characteristics by insomnia symptoms and chronic insufficient sleep.
| Total sample | Insomnia symptoms | Chronic insufficient sleep | |||||
|---|---|---|---|---|---|---|---|
| (N = 6,019) | No | Yes | p-value | No | Yes | p-value | |
| (n = 5,455) | (n = 564) | (n = 4,443) | (n = 1,576) | ||||
| Age, mean (se) | 15.91 (0.11) | 15.91 (0.12) | 15.93 (0.13) | .832 | 15.76 (0.12) | 16.36 (0.10) | .000 |
| Age, n (weighted %) | .182 | .000 | |||||
| 12–14 | 1,408 (25.73) | 1,281 (91.30) | 127 (8.70) | 1,176 (84.45) | 232 (15.55) | ||
| 15–16 | 2,102 (34.76) | 1,895 (88.82) | 207 (11.18) | 1,557 (74.87) | 545 (25.13) | ||
| 17–18 | 2,141 (33.20) | 1,942 (90.77) | 199 (9.23) | 1,459 (68.18) | 682 (31.82) | ||
| >18 | 368 (6.32) | 337 (90.490 | 31 (9.51) | 251 (66.67) | 117 (33.33) | ||
| Sex, n (weighted %) | .181 | .001 | |||||
| Male | 2,872 (50.17) | 2,626 (90.80) | 246 (9.20) | 2,195 (76.85) | 677 (23.15) | ||
| Female | 3,147 (49.83) | 2,829 (89.62) | 318 (10.38) | 2,248 (72.32) | 899 (27.68) | ||
| Race/Ethnicity, n (weighted %) | .865 | .083 | |||||
| Non-Hispanic White | 3,479 (65.98) | 3,146 (90.05) | 333 (9.95) | 2,615 (75.52) | 864 (24.48) | ||
| Hispanic all races | 278 (4.85) | 252 (91.67) | 26 (8.33) | 208 (75.30) | 70 (24.70) | ||
| Non-Hispanic Black | 1,431 (15.48) | 1,309 (90.77) | 122 (9.23) | 1,047 (73.21) | 384 (26.79) | ||
| Non-Hispanic Asian | 240 (3.45) | 219 (89.96) | 21 (10.04) | 158 (65.42) | 82 (34.58) | ||
| Non-Hispanic Native American | 196 (3.10) | 173 (88.23) | 23 (11.77) | 139 (73.00) | 57 (27.00) | ||
| Non-Hispanic Other | 395 (7.13) | 356 (90.46) | 39 (9.54) | 276 (73.68) | 119 (26.32) | ||
| Public assistance, n (weighted %) | .003 | .338 | |||||
| No | 5,387 (89.39) | 4,906 (90.65) | 481 (9.35) | 3,964 (74.37) | 1,423 (25.63) | ||
| Yes | 632 (10.61) | 549 (86.55) | 83 (13.45) | 479 (76.46) | 153 (23.54) | ||
| Modified CES-D score, median (iqr) | 9 (5, 14) | 8 (5, 13) | 14 (9, 20) | .000 | 8 (4, 12) | 12 (7,17) | .000 |
| PCRQ score, median (iqr) | 22.50 (21, 25) | 23 (21, 25) | 22 (19, 24) | .000 | 23 (21, 25) | 22 (19, 24) | .000 |
| Sleep duration (hours), mean (se) | 7.86 (0.04) | 474.11 (2.53) | 449.00 (4.77) | .000 | 8.11 (0.04) | 7.12 (0.05) | .000 |
CES-D = Center for Epidemiologic Studies Depression Scale; PCRQ = Parent-child relationship quality questionnaire. Significantly different group comparisons are bolded. Scores on the PCRQ ranged from 6–25, and scores on the CES-D ranged from 0–47. If continuous variables were normally distributed, we present the mean and standard error (se), and if they were skewed, we presented the median and interquartile range (iqr).
PCRQ and insomnia symptoms
In the unadjusted Model 1, each unit increase in PCRQ score was associated with an 8% lower odds of reporting insomnia symptoms (odds ratio [OR] = 0.92, 95% confidence interval [CI]: 0.90, 0.94; Table 2). This association remained after adjusting for demographic characteristics (Model 2; OR = 0.92, 95% CI: 0.90, 0.94), but not after further adjusting for depressive symptoms (Model 3; OR = 0.99, 95% CI: 0.96, 1.02). In Model 2, results translate to a 40% lower odds for those with a PCRQ score of 6 (the minimum PCRQ score in the sample) compared to a score of 0, a 75% lower odds for those with a PCRQ score of 22.5 (the median PCRQ score in the sample) compared to a score of 6, and a 80% lower odds for those with a PCRQ score of 25 (the highest PCRQ score in the sample) compared to a score of 6.
Table 2.
Association of PCRQ with insomnia symptoms in adolescents.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| PCRQ score | 0.92*** | [0.90, 0.94] | 0.92*** | [0.90, 0.94] | 0.99 | [0.96, 1.02] |
| Age | ||||||
| 12–14 | Ref | Ref | ||||
| 15–16 | 1.2 | [0.90, 1.61] | 1.1 | [0.82, 1.48] | ||
| 17–18 | 0.96 | [0.71, 1.29] | 0.85 | [0.63, 1.15] | ||
| >18 | 1.01 | [0.64, 1.61] | 0.8 | [0.51, 1.26] | ||
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 1.06 | [0.87, 1.30] | 0.88 | [0.71, 1.08] | ||
| Race/Ethnicity | ||||||
| Non-Hispanic White | Ref | Ref | ||||
| Hispanic all races | 0.75 | [0.47, 1.19] | 0.67 | [0.42, 1.06] | ||
| Non-Hispanic Black | 0.88 | [0.67, 1.15] | 0.73* | [0.55, 0.97] | ||
| Non-Hispanic Asian | 0.92 | [0.57, 1.47] | 0.76 | [0.45, 1.27] | ||
| Non-Hispanic Native American | 1.13 | [0.72, 1.78] | 0.93 | [0.57, 1.52] | ||
| Non-Hispanic Other | 0.89 | [0.57, 1.38] | 0.71 | [0.45, 1.14] | ||
| Public assistance | ||||||
| No | Ref | Ref | ||||
| Yes | 1.53** | [1.14, 2.05] | 1.17 | [0.84, 1.62] | ||
| Modified CES-D score | 1.10*** | [1.09, 1.12] | ||||
Survey-adjusted logistic regression models. Model 1: unadjusted; Model 2: adjusted for age, sex, race/ethnicity, and public assistance; and Model 3: adjusted for Model 2 covariates and modified CES-D score.
p < .5,
p < .1,
p < .1
PCRQ and chronic insufficient sleep
In Model 1, each unit increase in PCRQ score was associated with a 12% lower odds of reporting chronic insufficient sleep (OR = 0.88, 95% CI: 0.86, 0.89), and this association remained in Model 2 (OR = 0.89, 95% CI: 0.87, 0.91; Table 3). After further adjusting for depressive symptoms in (Model 3), the association decreased but remained significant (OR = 0.93, 95% CI: 0.91, 0.95). This translates to a 37% lower odds for those with a PCRQ score of 6 (the minimum PCRQ score in the sample) compared to a score of 0, a 72% lower odds for those with a PCRQ score of 22.5 (the median PCRQ score in the sample) compared to a score of 6, and a 76% lower odds for those with a PCRQ score of 25 (the highest PCRQ score in the sample) compared to a score of 6.
Table 3.
Association of PCRQ with chronic insufficient sleep in adolescents.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| PCRQ score | 0.88*** | [0.86, 0.89] | 0.89*** | [0.87, 0.91] | 0.93*** | [0.91, 0.95] |
| Age | ||||||
| 12–14 | Ref | Ref | ||||
| 15–16 | 1.62*** | [1.35, 1.96] | 1.56*** | [1.28, 1.89] | ||
| 17–18 | 2.20*** | [1.82, 2.67] | 2.13*** | [1.75, 2.59] | ||
| >18 | 2.39*** | [1.69, 3.39] | 2.14*** | [1.50, 3.04] | ||
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 1.19* | [1.04, 1.36] | 1.08 | [0.94, 1.25] | ||
| Race/Ethnicity | ||||||
| Non-Hispanic White | Ref | Ref | ||||
| Hispanic all races | 0.99 | [0.74, 1.32] | 0.92 | [0.68, 1.26] | ||
| Non-Hispanic Black | 1.14 | [0.97, 1.34] | 1.04 | [0.88, 1.23] | ||
| Non-Hispanic Asian | 1.46* | [1.06, 2.01] | 1.3 | [0.92, 1.85] | ||
| Non-Hispanic Native American | 1.17 | [0.82, 1.66] | 1.05 | [0.74, 1.49] | ||
| Non-Hispanic Other | 1.08 | [0.81, 1.44] | 0.96 | [0.72, 1.27] | ||
| Public assistance | ||||||
| No | Ref | Ref | ||||
| Yes | 0.87 | [0.70, 1.10] | 0.72** | [0.58, 0.90] | ||
| Modified CES-D score | 1.07*** | [1.06, 1.08] | ||||
Survey-adjusted logistic regression models. Model 1: unadjusted; Model 2: adjusted for age, sex, race/ethnicity, and public assistance; and Model 3: adjusted for Model 2 covariates and modified CES-D score.
p < .5,
p < .1,
p < .001
PCRQ and sleep duration
In Model 1, each unit increase in PCRQ score was associated with a 3.73 minute longer reported sleep duration (B = 3.73, 95% CI: 3.00, 4.47; Table 4). This association was attenuated in Model 2 (B = 2.56, 95% CI: 1.90, 3.22) and further attenuated after adjusting for depressive symptoms (B = 1.82, 95% CI: 1.12, 2.52). This translates to a 10.93 minute longer average sleep duration for those with a PCRQ score of 6 (the minimum PCRQ score in the sample) compared to a score of 0, a 30.05 minute longer average sleep duration for those with a PCRQ score of 22.5 (the median PCRQ score in the sample) compared to a score of 6, and a 34.60 minute longer average sleep duration for those with a PCRQ score of 25 (the highest PCRQ score in the sample) compared to a score of 6.
Table 4.
Association of PCRQ with sleep duration (min), in adolescents.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| B | 95% CI | B | 95% CI | B | 95% CI | |
| PCRQ score | 3.73*** | [3.00, 4.47] | 2.56*** | [1.90, 3.22] | 1.82*** | [1.12, 2.52] |
| Age | ||||||
| 12–14 | Ref | Ref | ||||
| 15–16 | −24.31*** | [−30.42, −18.20] | −23.46*** | [−29.59, −17.34] | ||
| 17–18 | −52.77*** | [−59.34, −46.21] | −51.76*** | [−58.40, −45.13] | ||
| >18 | −62.80*** | [−74.66, −50.94] | −60.56*** | [−72.43, −48.69] | ||
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | −6.60* | [−11.76, −1.43] | −5.13 | [−10.34, 0.07] | ||
| Race/Ethnicity | ||||||
| Non-Hispanic White | Ref | Ref | ||||
| Hispanic all races | 1.39 | [−9.47, 12.24] | 2.59 | [−8.60, 13.78] | ||
| Non-Hispanic Black | −13.93*** | [−21.30, −6.56] | −12.36** | [−19.92, −4.80] | ||
| Non-Hispanic Asian | −22.76** | [−37.53, −7.98] | −20.70** | [−35.45, −5.95] | ||
| Non-Hispanic Native American | 1.69 | [−14.17, 17.55] | 3.35 | [−12.39, 19.08] | ||
| Non-Hispanic Other | −1.92 | [−10.99, 7.14] | 0.09 | [−9.16, 9.34] | ||
| Public assistance | ||||||
| No | Ref | Ref | ||||
| Yes | 3.74 | [−4.61, 12.09] | 6.54 | [−2.03, 15.10] | ||
| Modified CES-D score | −1.07*** | [−1.43, −0.72] | ||||
Survey-adjusted linear regression models. Model 1: unadjusted; Model 2: adjusted for age, sex, race/ethnicity, and public assistance; and Model 3: adjusted for Model 2 covariates and modified CES-D score.
p < .5,
p < .1,
p < .1
PCRQ x race/ethnicity and sex interactions
There were no significant interactions of race/ethnicity or sex with PCRQ for insomnia symptoms or sleep duration. When chronic insufficient sleep was the outcome, race/ethnicity interacted with PCRQ in Model 3 (Wald test for overall interaction: F (5, 127) = 3.20, p = 0.009), but sex did not. When examining the individual interaction term regression coefficients, the term comparing Hispanics of all races to non-Hispanic Whites was significant (OR = 0.87, 95% CI: 0.79, 0.96).
In analyses stratified by race/ethnicity, each unit increase in PCRQ score was associated with 22% lower odds (95% CI: 0.71, 0.84) of chronic insufficient sleep among Hispanics in Model 1 (unadjusted), but only with 12% lower odds (95% CI: 0.85, 0.90) of chronic insufficient sleep among non-Hispanic Whites. These associations remained in Model 2 (adjusted for age, sex, and public assistance), and were slightly attenuated but remained significant when adding depressive symptoms in Model 3 (Table 5). After graphing stratified results by race/ethnicity in Model 3 (see Figure 1), the association between PCRQ and chronic insufficient sleep also appeared to differ between non-Hispanic Blacks and Hispanics of all races, such that the magnitude of the association of PCRQ with chronic insufficient sleep was larger among Hispanics of all races. This was confirmed by a linear combinations of estimator test comparing non-Hispanic Blacks to Hispanics of all races (OR = 1.20, 95% CI: 1.08, 1.33). In Model 3, Each unit increase in PCRQ score was associated with a 20% lower odds of chronic insufficient sleep among Hispanics of all races, but PCRQ was not significantly associated with chronic insufficient sleep among non-Hispanic Blacks.
Table 5.
Association of PCRQ with chronic insufficient sleep, stratified by race/ethnicity in adolescents.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Non-Hispanic White | 0.88*** | [0.85, 0.90] | 0.89*** | [0.87, 0.91] | 0.93*** | [0.90, 0.95] |
| Hispanic all races | 0.78*** | [0.71, 0.84] | 0.78*** | [0.72, 0.85] | 0.80*** | [0.73, 0.87] |
| Non-Hispanic Black | 0.91*** | [0.87, 0.95] | 0.93*** | [0.89, 0.97] | 0.97 | [0.92, 1.02] |
| Non-Hispanic Asian | 0.86*** | [0.79, 0.93] | 0.88** | [0.81, 0.95] | 0.89* | [0.81, 0.97] |
| Non-Hispanic Native American | 0.86*** | [0.79, 0.93] | 0.88** | [0.81, 0.95] | 0.89* | [0.81, 0.97] |
| Non-Hispanic Other | 0.86*** | [0.80, 0.92] | 0.89** | [0.82, 0.95] | 0.92 | [0.84, 1.00] |
Figure 1.
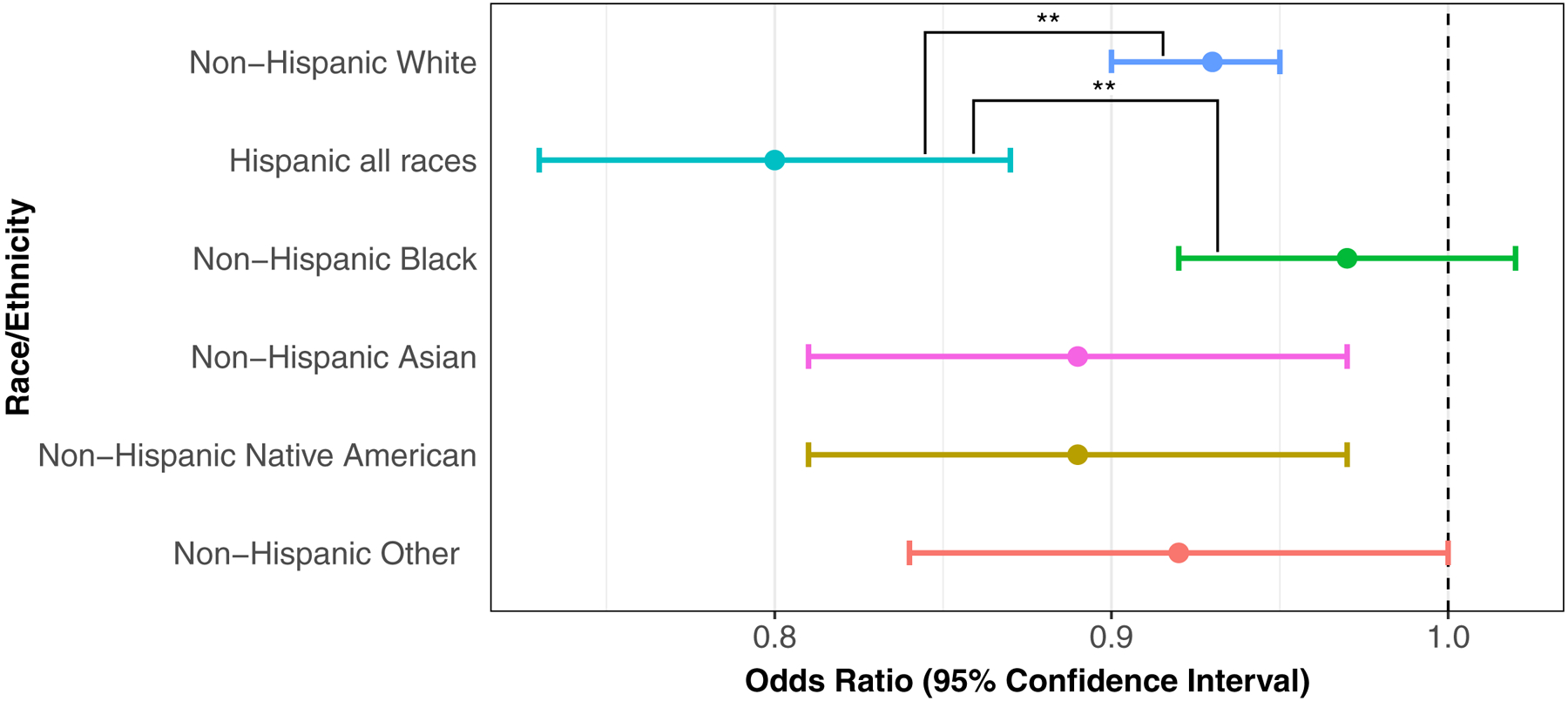
Association between PCRQ and chronic insufficient sleep (odds ratios and 95% confidence intervals), stratified by race/ethnicity in adolescents, and adjusting for demographic characteristics and depressive symptoms. **p < .01
Among all other race/ethnic groups, each unit increase in PCRQ was also associated with lower odds of chronic insufficient sleep in Models 1 and 2. When further adjusting for depressive symptoms in Model 3 however, there was no longer a significant association between PCRQ and chronic insufficient sleep in non-Hispanic “Others”. In the sensitivity analysis removing outliers for the sleep duration variable, associations for all analyses remained.
Discussion
In a nationally representative sample of U.S. adolescents, we found that adolescents’ ratings of better parent-child relationship quality (PCRQ) were cross-sectionally associated with a lower odds of insomnia symptoms and perceived chronic insufficient sleep, and with longer sleep duration. Associations of PCRQ with chronic insufficient sleep and sleep duration remained after adjustment for demographic characteristics and depressive symptoms, but associations with insomnia symptoms were accounted for by depressive symptoms. Our findings suggest that PCRQ may be an important protective factor for sleep health among adolescents. We also found that race/ethnicity modified the association between PCRQ and chronic insufficient sleep such that the magnitude of the association was greater among Hispanics compared to non-Hispanic White and non-Hispanic Blacks. To our knowledge, this is the first nationally representative U.S. study to examine the associations between parent-child relationship quality, insomnia symptoms, perceived chronic insufficient sleep, and sleep duration in adolescents and evaluate sex or race/ethnicity as moderators.
Findings from the current study, if replicated in longitudinal studies, could have implications for a range of potential outcomes in adolescence and beyond. For instance, suboptimal parent-child relationship quality is associated with poor cognitive outcomes, negative health behaviors,11 cardio-metabolic disease,32 greater healthcare utilization,11 mental disorders,11 and suicidal ideation.33 Sleep disturbances are also well-established risk factors for most of these outcomes,5,10,34,35 and may therefore mediate links between PCRQ and poor health. It may also be that PCRQ mediates relationships between sleep and health. Better PCRQ may promote adolescent sleep health by creating a sense of safety, consequently downregulating vigilance and threat perception/response systems that become increasingly active during puberty and interfere with sleep.13 Additionally, PCRQ may be correlated with other factors that promote sleep, such as parent-set bedtimes, which have been linked to better and longer sleep and better daytime functioning in adolescents.36 Evidence of a stronger association in Hispanics compared to non-Hispanic Whites and non-Hispanic Blacks could mean that Hispanic youth are especially vulnerable to effects of PCRQ on sleep, or sleep on PCRQ. Evidence of a weaker association in non-Hispanic Blacks compared to Hispanics of all races suggests that other factors may have a greater effect on sleep (or PCRQ) in this population. Differential associations between PCRQ and sleep by race/ethnicity in adolescents may be explained by differences in parenting perceptions and norms, social networks that can assist with caretaking, external factors like poverty or low socioeconomic status, exposure to discriminatory experiences that influence access to relevant resources, or by unmeasured confounders.37 More research is needed.
Our findings are consistent with studies of adolescents in the U.S.24 and abroad25,26 that have found positive associations of PCRQ with sleep, but conflict with others that found no association.19,22,23 A longitudinal study in Amsterdam found that over two years, better PCRQ was associated with longer time in bed, better sleep quality and less sleepiness.26 The authors also found that higher parental monitoring (i.e., rule setting)—a concept not addressed here—was linked to earlier bedtimes, longer time in bed, less sleepiness, and better sleep quality. Indeed, other studies found that parental monitoring was associated with better adolescent sleep, but PCRQ was not.19,22 As was observed in one of these studies, it may be that parental monitoring is more important to adolescent sleep than PCRQ when considering both in the same model,22 or that PCRQ becomes more important in stressful contexts, as was found in another U.S. adolescent cohort.23
Similar to our finding that the magnitude of the relationship between PCRQ and chronic insufficient sleep was greater in Hispanic adolescents compared to White adolescents, greater PCRQ was associated with lower sleepiness in ethnic minorities in the aforementioned Dutch study.26 Although all of our findings are similar to those from some other countries, our results may not generalize to others. For example, contrary to the community study of adults in Japan,17 we did not find significant differences by sex in the association between PCRQ and sleep. This may be due to cultural differences, or sex differences may emerge later in life.
The present study is one of the few that have accounted for the role of depressive symptoms when examining the PCRQ-sleep link in adolescents. A study of adolescents with a history of substance abuse found that psychological distress mediated the link between parental involvement and objectively measured sleep efficiency.24 Similarly, in the current study, the association between PCRQ and insomnia symptoms became non-significant after adjusting for depressive symptoms. It may be that depressive symptoms mediate the association between PCRQ and insomnia symptoms, or that insomnia symptoms mediate the association between PCRQ and depressive symptoms.
This study has several notable strengths, including a nationally representative U.S. sample, measures of three sleep outcomes relevant to adolescents, adjustment for multiple potential confounders, consideration of the role of depressive symptoms, and exploration of sex and race/ethnicity as moderators. It also, however, has several limitations. First, given the cross-sectional analyses, we cannot infer directionality of the association between PCRQ and our sleep outcomes, and this relationship may be bidirectional. We chose PCRQ as the exposure and sleep as the outcome based on developmental theory, which emphasizes the importance of feeling safe and secure for sleep promotion through downregulation of vigilance and threat response systems, on evolutionary theory, which suggests that these feelings of safety and security stemmed from a protective social group, and on past research in this domain. It is also possible, however, that sleep problems in adolescents also negatively affect PCRQ (e.g. difficulties waking on time due to insufficient nighttime sleep could lead to poorer PCRQ, or poor sleep could lead to greater adolescent irritability and poorer sleep).20 In addition, our findings are based on retrospective self-report sleep items that cannot capture the variability in sleep that might be ascertained through other self-report measures (e.g., repeatedly administered sleep diaries), and they may yield different results from an objective measure like wrist actigraphy. Previous research in adults also suggests the potential for differential measurement error (i.e., reporting bias) of subjective sleep by race/ethnicity, with Whites more likely to overestimate sleep compared to Blacks,38 and Hispanics and Blacks less likely to report sleep complaints compared to Whites.39 Further, the sleep items we used were designed specifically for the Add Health study, and thus have limited available psychometrics data, and there is risk of bias from common method variance (i.e., self-reported exposure and outcomes). Another important point is that 92% of the sample only had PCRQ data on one parent, mostly the mother. Mother and father PCRQ may have differential links with sleep.17 The current sample represents the U.S. population of adolescents over two decades ago in 1994–1995. We cannot be sure that findings would generalize to today’s U.S. adolescents, especially given declines in adolescent sleep duration,40 which may be due in part to screen-based media device use.41 Finally, there is no consensus regarding whether and how to adjust for multiple statistical comparisons.42 In the present study, we chose not to correct for multiple comparisons because this would be too conservative at this early stage of research. Thus, the present results should be considered preliminary and require confirmation in future research. In sum, future studies of PCRQ and adolescent sleep should be prospective to assess directionality of the PCRQ-sleep link, use subjective measures of insomnia symptoms (questionnaires and sleep diaries), and objective measures of sleep parameters (e.g., actigraphy), and further examine whether psychological distress mediates links between PCRQ and sleep.
Conclusion
In U.S. adolescents, better PCRQ is associated with lower odds of perceived chronic insufficient sleep and insomnia symptoms, and longer sleep duration in adolescents when adjusting for demographic characteristics. When further adjusting for depressive symptoms, better PCRQ was still associated with lower odds of perceived chronic insufficient sleep and longer sleep duration, but not insomnia symptoms. The association of PCRQ and perceived chronic insufficient sleep appears to differ by race/ethnicity, with stronger associations in Hispanic adolescents. In considering sleep interventions for adolescents, it may be important to also consider the family context, such as PCRQ, in addition to factors like early school start times.
Acknowledgements
A component of this study was accepted for presentation at the 33rd Annual Meeting of the Associated Professional Sleep Societies in San Antonio, Texas from June 8-12, 2019. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Acknowledgement is due to Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Darlynn M. Rojo-Wissar is supported by the National Institute of Mental Health’s Psychiatric Epidemiology Training Program (5T32MH014592-39; PI: Zandi, Peter). This work was funded, in part, by the Intramural Program at the NIH, National Institute of Environmental Health Sciences (Z1A ES103325-01; Chandra L. Jackson). Adam Spira received an honorarium from Springer Nature Switzerland AG for Guest Editing a Special Issue of Current Sleep Medicine Reports. The other authors have no financial relationships relevant to this article to disclose.
Abbreviations:
- PCRQ
Parent-child relationship quality
- CES-D
Center for Epidemiologic Studies Depression Scale
References
- 1.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12(2):110–118. doi: 10.1016/j.sleep.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 2.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Heal. 2015;1(4):233–243. doi: 10.1016/j.sleh.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 3.National Sleep Foundation. 2006 Teens and sleep Sleep in America Polls. Washington, DC: National Sleep Foundation; http://sleepfoundation.org/sites/default/files/2006_summary_of_findings.pdf. Published 2006. Accessed November 15, 2018. [Google Scholar]
- 4.Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: Prospective data on sleep deprivation, health and functioning. J Adolesc. 2009;32(5):1045–1057. doi: 10.1016/j.adolescence.2009.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Owens J Insufficient Sleep in Adolescents and Young Adults: An Update on Causes and Consequences. Pediatrics. 2014;134(3):e921–e932. doi: 10.1542/peds.2014-1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Psychiatric Association [APA]. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Arlington, VA, US; 2013. [Google Scholar]
- 7.Chung KF, Kan KKK, Yeung WF. Insomnia in adolescents: Prevalence, help-seeking behaviors, and types of interventions. Child Adolesc Ment Health. 2014;19(1):57–63. doi: 10.1111/camh.12009 [DOI] [PubMed] [Google Scholar]
- 8.Roberts RE, Roberts CR, Chan W. Persistence and change in symptoms of insomnia among adolescents. Sleep. 2008;31(2):177–184. doi: 10.1093/sleep/31.2.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson EO. Epidemiology of DSM-IV Insomnia in Adolescence: Lifetime Prevalence, Chronicity, and an Emergent Gender Difference. Pediatrics. 2006;117(2):e247–e256. doi: 10.1542/peds.2004-2629 [DOI] [PubMed] [Google Scholar]
- 10.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. doi: 10.1016/J.SMRV.2009.10.004 [DOI] [PubMed] [Google Scholar]
- 11.Ranson KE, Urichuk LJ. The effect of parent-child attachment relationships on child biopsychosocial outcomes: A review. Early Child Dev Care. 2008;178(2):129–152. doi: 10.1080/03004430600685282 [DOI] [Google Scholar]
- 12.Worthman C, Melby M. Toward a comparative developmental ecology of human sleep. 2002. http://psycnet.apa.org/record/2003-04411-006. Accessed June 14, 2018.
- 13.Dahl RE, Lewin DS. Pathways to adolescent health: Sleep regulation and behavior. J Adolesc Heal. 2002;31(6 SUPPL):175–184. doi: 10.1016/S1054-139X(02)00506-2 [DOI] [PubMed] [Google Scholar]
- 14.McKenna JJ, Thoman EB, Anders TF, Sadeh A, Schechtman V, Glotzbach S. Infant-Parent Co-Sleeping in an Evolutionary Perspective: Implications for Understanding Infant Sleep Development and the Sudden Infant Death Syndrome. Am Sleep Disord Assoc Sleep Res Soc. 1993;16(3):263–282. https://academic.oup.com/sleep/article-abstract/16/3/263/2749380. Accessed June 14, 2018. [DOI] [PubMed] [Google Scholar]
- 15.MacDonald K Warmth as a Developmental Construct: An Evolutionary Analysis. Child Dev. 1992;63(4):753–773. doi: 10.1111/j.1467-8624.1992.tb01659.x [DOI] [Google Scholar]
- 16.Meltzer LJ, Montgomery-Downs HE. Sleep in the Family. Pediatr Clin North Am. 2011;58(3):765–774. doi: 10.1016/j.pcl.2011.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shibata M, Ninomiya T, Anno K, et al. Perceived inadequate care and excessive overprotection during childhood are associated with greater risk of sleep disturbance in adulthood: the Hisayama Study. BMC Psychiatry. 2016;16(1):215. doi: 10.1186/s12888-016-0926-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rojo-Wissar DM, McQuaid JR, Ancoli-Israel S, Gengler DN, Haynes PL. Maternal Bonding Predicts Actigraphy-Measured Sleep Parameters in Depressed and Nondepressed Adults. J Nerv Ment Dis. 2019;In press. doi: 10.1097/NMD.0000000000001071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adam E, Snell E, Pendry P. Sleep Timing and Quantity in Ecological and Family Context: A Nationally Representative Time-Diary Study. J Fam Psychol. 2007;21(1):4–19. doi: 10.1037/0893-3200.21.1.4 [DOI] [PubMed] [Google Scholar]
- 20.Bell BG, Belsky J. Parents, parenting, and children’s sleep problems: Exploring reciprocal effects. Br J Dev Psychol. 2008;26(4):579–593. doi: 10.1348/026151008X285651 [DOI] [Google Scholar]
- 21.Keller P, El-Sheikh M. Children’s emotional security and sleep: Longitudinal relations and directions of effects. J Child Psychol Psychiatry Allied Discip. 2011;52(1):64–71. doi: 10.1111/j.1469-7610.2010.02263.x [DOI] [PubMed] [Google Scholar]
- 22.Maume DJ. Social Ties and Adolescent Sleep Disruption. J Health Soc Behav. 2013;54(4):498–515. doi: 10.1177/0022146513498512 [DOI] [PubMed] [Google Scholar]
- 23.Tsai KM, Dahl RE, Irwin MR, et al. The Roles of Parental Support and Family Stress in Adolescent Sleep. Child Dev. 2018;89(5):1577–1588. doi: 10.1111/cdev.12917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cousins JC, Bootzin RR, Stevens SJ, Ruiz BS, Haynes PL. Parental involvement, psychological distress, and sleep: A preliminary examination in sleep-disturbed adolescents with a history of substance abuse. J Fam Psychol. 2007;21(1):104–113. doi: 10.1037/0893-3200.21.1.104 [DOI] [PubMed] [Google Scholar]
- 25.Brand S, Hatzinger M, Beck J, Holsboer-Trachsler E. Perceived parenting styles, personality traits and sleep patterns in adolescents. J Adolesc. 2009;32(5):1189–1207. doi: 10.1016/j.adolescence.2009.01.010 [DOI] [PubMed] [Google Scholar]
- 26.Meijer AM, Reitz E, Dekoviċ M. Parenting matters: a longitudinal study into parenting and adolescent sleep. J Sleep Res. 2016;25(5):556–564. doi: 10.1111/jsr.12406 [DOI] [PubMed] [Google Scholar]
- 27.Resnick MD. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA J Am Med Assoc. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823 [DOI] [PubMed] [Google Scholar]
- 28.Ehrlich KB, Hoyt LT, Sumner JA, McDade TW, Adam EK. Quality of relationships with parents and friends in adolescence predicts metabolic risk in young adulthood. Health Psychol. 2015;34(9):896–904. doi: 10.1037/hea0000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 30.Austin AE, Shanahan ME. Association of childhood abuse and neglect with prescription opioid misuse: Examination of mediation by adolescent depressive symptoms and pain. Child Youth Serv Rev. 2018;86:84–93. doi: 10.1016/J.CHILDYOUTH.2018.01.023 [DOI] [Google Scholar]
- 31.Peach HD, Gaultney JF. Sleep, impulse control, and sensation-seeking predict delinquent behavior in adolescents, emerging adults, and adults. J Adolesc Heal. 2013;53(2):293–299. doi: 10.1016/j.jadohealth.2013.03.012 [DOI] [PubMed] [Google Scholar]
- 32.Bae D, Wickrama KAS. Stress Processes Linking Parent–Child Disconnection to Disease Risk in Young Adulthood: Amplification by Genotype. J Youth Adolesc. 2017;46(5):1137–1148. doi: 10.1007/s10964-017-0666-8 [DOI] [PubMed] [Google Scholar]
- 33.Kuramoto-Crawford SJ, Ali MM, Wilcox HC. Parent-child connectedness and long-term risk for suicidal ideation in a nationally representative sample of US adolescents. Crisis. 2017;38(5):309–318. doi: 10.1027/0227-5910/a000439 [DOI] [PubMed] [Google Scholar]
- 34.Matthews KA, Pantesco EJM. Sleep characteristics and cardiovascular risk in children and adolescents: an enumerative review. Sleep Med. 2016;18:36–49. doi: 10.1016/J.SLEEP.2015.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller MA, Kruisbrink M, Wallace J, Ji C, Cappuccio FP. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep. 2018;41(4). doi: 10.1093/sleep/zsy018 [DOI] [PubMed] [Google Scholar]
- 36.Short MA, Gradisar M, Wright H, Lack LC, Dohnt H, Carskadon MA. Time for Bed: Parent-Set Bedtimes Associated with Improved Sleep and Daytime Functioning in Adolescents. Sleep. 2011;34(6):797–800. doi: 10.5665/SLEEP.1052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yasui M, Dishion TJ. The Ethnic Context of Child and Adolescent Problem Behavior: Implications for Child and Family Interventions. Clin Child Fam Psychol Rev. 2007;10(2):137–179. doi: 10.1007/s10567-007-0021-9 [DOI] [PubMed] [Google Scholar]
- 38.Jackson CL, Patel SR, Jackson WB, Lutsey PL, Redline S. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(6). doi: 10.1093/sleep/zsy057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11(5):470–478. doi: 10.1016/J.SLEEP.2009.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The Great Sleep Recession: Changes in Sleep Duration Among US Adolescents, 1991–2012. Pediatrics. 2015;135(3):460–468. doi: 10.1542/peds.2014-2707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carter B, Rees P, Hale L, Bhattacharjee D, Paradkar MS. Association Between Portable Screen-Based Media Device Access or Use and Sleep Outcomes. JAMA Pediatr. 2016;170(12):1202. doi: 10.1001/jamapediatrics.2016.2341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Streiner DL, Norman GR. Correction for multiple testing: Is there a resolution? Chest. 2011;140(1):16–18. doi: 10.1378/chest.11-0523 [DOI] [PubMed] [Google Scholar]


