Highlights
-
•
The number of COVID-19 cases surpassed 300,000, WHO identified as a global pandemic.
-
•
COVID-19 has been a serious threat to old population.
-
•
The COVID-19 infection is generally susceptible with a relatively high fatality rate in older patients.
-
•
More attention should pay to the elderly patients with COVID-19 infection.
Keywords: Novel coronavirus (COVID-19), Older patients, Clinical characteristics
Abstract
Objectives
Since the outbreak of 2019 novel coronavirus (COVID-19), which has spread in the world rapidly. Population have a susceptibility to COVID-19, older people were more susceptible to have a variety diseases than younger, including COVID-19 infection with no doubt. This study focused on older patients with COVID-19 infection and analyzed the epidemiological and clinical characteristics of them.
Methods
We collected information on confirmed older patient transferred by Beijing Emergency Medical Service (EMS) to the designated hospitals from Jan 20 to Feb 29, 2020. The information including demographic, epidemiological, clinical, classification of severity and outcomes. All cases were categorized into three groups and compared the difference between aged 50–64 years, 65–79 years and older than 80 years.
Results
56.7 % of elderly confirmed patients were male, fever (78.3 %), cough (56.7 %), dyspnea (30.0 %), and fatigue (23.3 %) were common symptoms of COVID-19 infection. Classification of severity has statistically significant differences between the three groups, compared with middle-aged patients and aged 65–79 years group, older than 80 years group had significant statistical differences in contacted to symptomatic case in 14 days. As of Feb 29, 38.3 % patients had discharged and 53.3 % patients remained in hospital in our study, the fatality of COVID-19 infection in elderly was 8.3 %.
Conclusions
The COVID-19 infection is generally susceptible with a relatively high fatality rate in older patients, we should pay more attention to the elderly patients with COVID-19 infection.
1. Introduction
Along with the outbreak of the epidemic of 2019 novel coronavirus (COVID-19), the number of older patients infected with COVID-19 was increasing in the world and it brought a serious threat to life and health. A study in the New English Journal of Medicine (NEJM) by Guan reported the clinical characteristics of coronavirus diseases 2019 in China that the rate of older patients older than 65 years with COVID-19 infection was 15.1 % (Guan et al., 2020), while the proportion of older than 80 years was 3 % reported in the JAMA by Wu and McGoogan (Wu & McGoogan, 2020). It was proved that population including old people was generally susceptible, and the older patients with high infection rate and fatality (Yang, Yu et al., 2020). Unfortunately, the clinical characteristics of COVID-19 infection in older patients is unknown. According to the World Health Organization (WHO) report, as of March 3, 2020, a total of 90,870 cases with laboratory-confirmed with COVID-19 infection have been detected in the world (WHO, 2020). As a new disease and a new global health issue, COVID-19 infection is understandable that its emergence and spread cause anxiety and fear among the older population. In addition, aging population has been one of the largest problems in many countries, and there were a higher prevalence of multimorbidity and lower resistance in older patients (Feng, Liu, Guan, & Mor, 2012; Low et al., 2019), no doubt, there are many old people who will face the risk of infected with COVID-19 with the globalization and aging population, which imposing a heavy burden on the public and health care systems in the world. Furthermore, the clinical clues that an infection might be present in an older person include fever and some obvious clinical signs, such as fever, cough, and rales, the elder patients may have typical or atypical presentations of infection as that described by the Infectious Diseases Society of America (IDSA) (High et al., 2009), how about the COVID-19 infection? Given that, we collected the data on the 60 older patients infected with laboratory-confirmed COVID-19, described and analyzed the epidemiological and clinical characteristics of the older patients with COVID-19 infection.
2. Methods
2.1. Participants and settings
We did a retrospective review of medical records from 60 older patients with COVID-19 infection who was transferred from the general hospitals to the designated hospitals for special treatment infectious diseases by Beijing Emergency Medical Service (EMS) from Jan 20 to Feb 29, 2020. A confirmed case was defined as a suspected cases with the laboratory test for the 2019-nCoV virus from the respiratory specimens show positive result by means of real-time reverse-transcription-polymerase-chain-reaction (RT-PCR) assay, while a suspected case was defined as a case that fulfilled both the following criteria: clinical have fever, radiographic evidence of pneumonia, low or normal white-cell count or low lymphocyte count; and the epidemic history have a travel to Wuhan or direct contact with patients from Wuhan who have fever or respiratory symptoms within 14 days before illness according to the new coronavirus pneumonial diagnosis and treatment program (3id ed.) which were published by the National Health Commission of China. A mild case was defined as a confirmed case with fever, respiratory symptoms and radiographic evidence of pneumonia. While a severe case was defined as a mild cases with dyspnea or respiratory failure. Only laboratory-confirmed COVID-19 infection was enrolled in this study, laboratory confirmation of COVID-19 was detected in the first admission hospital and verified by the local Center for Disease Control and Prevention (CDC). We collected the data on the demographic, epidemiological, clinical, laboratory tests, diagnosis types, cluster cases and outcomes of COVID-19 infection in elderly patients, and categorized into three groups and compared the difference between middle aged 50–64years, aged 65–79 years and older than 80 years. If the data we need was missing, we directly communicated with EMS providers.
2.2. Ethics
The study was approved by Ethics Committee of Beijing Emergency Medical Center (No.2020-01) and the written informed consent was waived.
2.3. Statistical analysis
All statistical analyses were conducted using the SPSS software version 21.0. The continuous variables were expressed as mean ± SD and were compared with Mann-Whitney U test between two groups. Percentages for categorical variables were analyzed using the Wilcoxon test, although Fisher's exact test was used with limited data. P < 0.05 was the threshold for statistical significance.
3. Results
There were 60 older patients and 81 middle aged patients identified as confirmed COVID-19 infection in this study by Feb 29, 2020. Of them, 44 patients were categorized into aged 65–79 years group, 16 patients were categorized into older than 80 years group. 34 (56.7 %) patients were male, there were no significant differences between male and female in three groups (χ2 = 2.060, p = 0.151). 31 patients had medical history record information, including hypertension (15, 48.4 %), chronic obstructive pulmonary disease (COPD) (9, 29.0 %), coronary heart disease (5, 16.1 %), diabetes (3, 9.7 %), cerebrovascular disease (2, 6.5 %) and other diseases (8, 25.8 %), there were significant differences between in three groups (χ2 = 8.164, p = 0.004) in medical history, especially COPD in older than 80 years group were significantly higher than those in other two groups (χ2 = 12.024, p < 0.001).
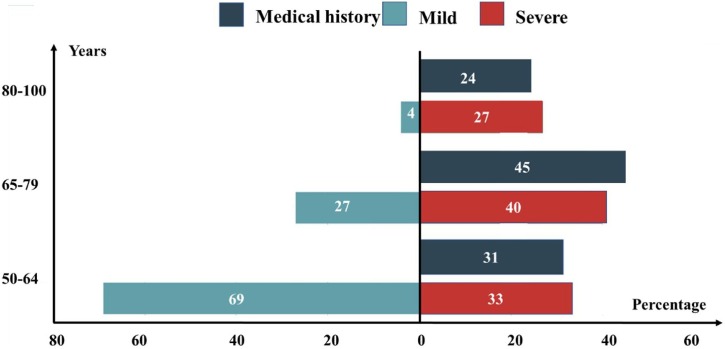
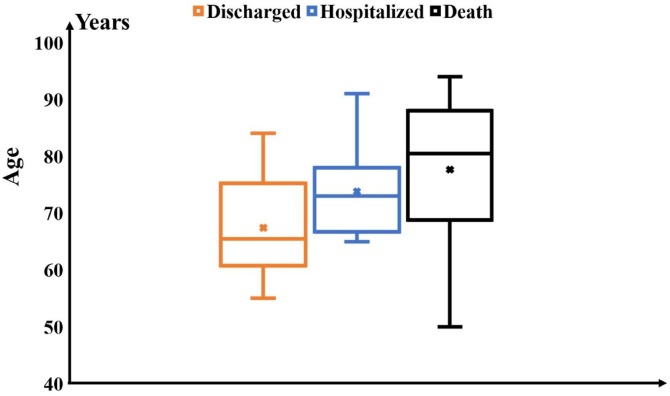
In this study, the most common symptom of diagnosed confirmed COVID-19 infection in older patients were fever (47, 75 %) and other common symptoms were cough (34, 56.7 %), dyspnea (18, 30.0 %) and fatigue (14, 23.3 %) respectively. The body temperature of 13 (21.7 %) patients were less than 37.3 ℃, while 24 (40.0 %) were between 37 ℃ to 38 ℃, and 23 (38.3 %) were over 38 ℃ (Table1 ). There were no significant differences in fever and highest temperature between the older patients and middle aged groups (χ2 = 0.006, p = 0.937), but there were significant differences in dyspnea and respiratory rate between two groups (χ2 = 14.597, p < 0.001).The difference in classification of severity between the two groups was statistically significant (χ2 = 17.31, P < 0.001), 32 (53.3 %) patients were classified as severe cases, including 13 patients older than 80 years, accounted for 81.3% in this group. Both the number of patients with underlying diseases and the severe patients were increased as aging (Fig. 2). Nearly half of the all cases contacted to symptomatic case in 14 days, and older than 80 years group had a higher proportion compared with aged 65–79 years and 50–64 years group (χ2 = 4.804, 0.028). The mean time from contact symptomatic case to illness onset was 7.4 days, from illness onset to visit hospital was 3.6 days, from visit hospital to defined confirmed case was 2.6 days. 36 (60.0 %) and 41 (68.3 %) patients were indigenous cases and clustering cases respectively. By the end of Feb 29, 2020, 32 (53.3 %) older patients are still hospitalized, 23 (38.3 %) were discharged. 5 (8.3 %) patients died. However, the fatality in the aged older than 80 years group was 18.8 %, significantly higher than those in other two groups (χ2 = 7.413, p = 0.025) (Fig. 1 ).
Table 1.
Characteristics of older patients infected with COVID-19.
| Older patients |
Age 50–64 y (n = 81) | P-value | |||
|---|---|---|---|---|---|
| Total (n = 60) | Age 65–79 y (n = 44) | Age ≥ 80 y (n = 16) | |||
| Male, n(%) | 34(56.7) | 26(59.1) | 8(50) | 36(44.4) | 0.151 |
| Medical history, n(%) | 26(n = 31) | 17(n = 22) | 9(n = 9) | 12(n = 25) | 0.004 |
| Hypertension | 15(48.4) | 12(54.5) | 3(33.3) | 7(28.0) | 0.120 |
| Coronary heart disease | 5(16.1) | 4(18.2) | 1(11.1) | 3(12.0) | 0.659 |
| COPD | 9(29.0) | 3(13.6) | 6(66.7) | 0(0.0) | 0.001 |
| Diabetes | 3(9.7) | 3(13.6) | 0(0.0) | 2(8.0) | 0.826 |
| Cerebrovascular disease | 2(6.5) | 1(4.5) | 1(11.1) | 3(12.0) | 0.470 |
| Other | 8(25.8) | 6(27.3) | 2(22.2) | 6(24.0) | 0.877 |
| Signs and symptoms, n(%) | |||||
| Fever | 47(78.3) | 35(79.5) | 12(75) | 63(77.8) | 0.937 |
| Highest temperature,℃ | 0.952 | ||||
| <37.3 | 13(21.7) | 9(20.5) | 4(25.0) | 18(22.2) | |
| 37.3-38.0 | 24(40.0) | 19(43.2) | 5(31.3) | 34(42.0) | |
| >38.0 | 23(38.3) | 16(36.4) | 7(43.8) | 29(35.8) | |
| Cough | 34(56.7) | 27(61.4) | 7(43.8) | 37(45.7) | 0.197 |
| Dyspnea | 18(30.0) | 14(31.8) | 4(25.0) | 5(6.2) | <0.001 |
| Fatigue | 14(23.3) | 10(22.7) | 4(25.0) | 26(32.1) | 0.254 |
| Headache | 4(6.7) | 3(6.8) | 1(6.3) | 7(8.6) | 0.665 |
| Respiratory rate | 22.5 ± 5.1 | 21.6 ± 5.2 | 25.1 ± 4.1 | 19.9 ± 3.5 | <0.001 |
| Oxygen saturation | 92.0 ± 6.4 | 92.9 ± 4.7 | 90.6 ± 8.5 | 93.3 ± 2.7 | 0.474 |
| Classification of severity, n(%) | <0.001 | ||||
| Mild | 28(46.7) | 25(56.8) | 3(18.8) | 65(80.2) | |
| Severe | 32(53.3) | 19(43.2) | 13(81.3) | 16(19.8) | |
| History of contact, n(%) | 47(78.3) | 33(75) | 14(87.5) | 74(91.4) | 0.028 |
| Have been to Wuhan in 14 days | 20(33.3) | 17(38.6) | 3(18.8) | 30(37.0) | 0.327 |
| Contacted to symptomatic case in 14 days | 28(46.7) | 17(38.6) | 11(68.8) | 45(55.6) | 0.296 |
| Days from contact to illness onset | 7.4 ± 4.2 | 7.8 ± 4.1 | 5.7 ± 5.1 | 8.8 ± 5.0 | 0.353 |
| Days from illness onset to visit hospital | 3.6 ± 4.9 | 3.9 ± 4.5 | 2.4 ± 5.9 | 2.8 ± 3.5 | 0.294 |
| Days from visit hospital to defined | 2.6 ± 3.0 | 2.5 ± 2.2 | 2.9 ± 4.6 | 1.9 ± 2.4 | 0.126 |
| Distribution, n (%) | 0.611 | ||||
| Imported cases | 24(40.0) | 20(45.5) | 4(25.0) | 29(35.8) | |
| Indigenous cases | 36(60.0) | 24(54.5) | 12(75.0) | 52(64.2) | |
| Clustering case, n (%) | 41(68.3) | 28(63.6) | 13(81.3) | 60(74.1) | 0.455 |
| Family | 34(56.7) | 24(54.5) | 10(62.5) | 47(58.0) | 0.848 |
| Other | 7(11.7) | 4(9.1) | 3(18.8) | 13(16.0) | 0.486 |
| Outcomes, n(%) | 0.025 | ||||
| Hospitalized | 32(53.3) | 23(52.3) | 9(56.3) | 58(71.6) | |
| Discharged | 23(38.3) | 19(43.2) | 4(25.0) | 22(27.2) | |
| Death | 5(8.3) | 2(4.5) | 3(18.8) | 1(1.2) | |
Fig. 2.
The distribution of mild, severe and medical history after COVID-19 infection by age.
Fig. 1.
Distribution of outcomes of COVID-19 infections by age.
4. Discussion
The COVID-19 strokes and as emergencies continued to developing, the WHO declares global emergency on Jan 31, 2020 (Sohrabi et al., 2020). Older people are more susceptible to a variety of diseases than younger, of course, including COVID-19 infection, which could dramatically increased the healthcare burden under the background of an aging society (Kingston, Robinson, Booth, Knapp, & Jagger, 2018; Rasmussen et al., 2017). The entire population is susceptible to the COVID-19, and the confirmed patients, asymptomatic carrier and people in the incubation period are contagious, it is difficult to control source of infection (Yang & Duan, 2020), and most of the adult patients were old people, who had higher morbidity and case-fatality rate (Sun, Lu, Xu, Sun, & Pan, 2020). However, the clinical characteristics of COVID-19 infection in older patients were not reported currently. In this study, to our knowledge, we firstly described and analyzed the epidemiological and clinical characteristics of the older patients with COVID-19 infection and compared the difference between aged 50–64 years, aged 65–79 years and older than 80 years groups in Beijing.
In our study, the most common symptom were fever (78.3 %) and cough (56.7 %) in the older patients, which was same as the results of many studies (Deng & Peng, 2020; Guan et al., 2020; Wu, Liu et al., 2020; Xu et al., 2020; Yang, Cao et al., 2020). Usually, the infected older patients initially have fever, fatigue, dry cough, and gradually appear dyspnea, some patients may develop acute respiratory distress syndrome (ARDS) and septic shock, even die(Chen et al., 2020). 40 % older patients have a fever, the body temperatures were between 37.3–38.0 ℃, and the body temperature of 38.3 % patients were higher than 38.0 ℃, only two patients were over 39 ℃, while not all old patients had fever, 21.7 % old patients were afebrile in our study, which may be caused by old populations with low immune function. The afebrile and low-grade fever, especially older patients, may increase the difficulty to identify and diagnosis COVID-19 in clinical practice if too much attention was given to fever detection, the results same as that described by IDSA.
A research reported that the first death of COVID-19 infection mostly occurred in old people, and developed quickly (Wang, Tang, & Wei, 2020). Existing research found that the overall fatality rate of infected COVID-19 was estimated 2 %–5 % (Elisabeth, 2020; Ji, Ma, Maikel, & Pan, 2020; Sun, Qie et al., 2020; Wu, Chen, & Chan, 2020; Wu & McGoogan, 2020;), however, the case-fatality rate were 8.0 % and 14.8 % in aged 70–79 years and older than 80 years patients respectively (Wu & McGoogan, 2020). The case-fatality rate was 18.8 % of older than 80 years patients in our study, and higher than it mentioned in previous study, which was mainly for the older patients got the more underlying diseases as a result of the weaker immune functions. When old populations were infected with COVID-19, prompting administration of antibiotics to prevent infection and strengthening of immune support treatment might reduce the case-fatality rate (Chen et al., 2020).
Our study found that number of older patients with underlying diseases were relatively susceptible to COVID-19 and indicated that the infected COVID-19 elderly with relatively high proportion of comorbidities, and the most common comorbidities were hypertension (48.8 %), coronary heart disease (16.1 %), COPD (29.0 %), diabetes (9.7 %) and cerebrovascular disease (6.5 %) respectively, which was in accordance with previous studies (Chen et al., 2020; Yang, Cao et al., 2020). Latest research stated that the older patients and among those with coexisting conditions had a higher morbidity and case-fatality rate (Fauci, Lane, & Redfield, 2020; Peng et al., 2020). COVID-19 confirmed older patients who were older than 65 years with comorbidities were at increased risk of death (Yang, Yu et al., 2020)
In our study, severe patients were significantly more than mild patients in older patients, which was similar with recent study that patients have more severe symptom in elderly population (Chan et al., 2020). Multiple factors lead to a higher proportion of elderly patients with severe situation, such as senior, comorbidities, low immune functions and so on. There is no doubt that old severe patients are more likely to die, therefore, the clinical treatment capacity need to improve to decrease the case-fatality rate of severe patients with COVID-19 infection, and the elderly should be pay special attention. There was a 65-year-old man who was afebrile and well, and noteworthy, he was an asymptomatic case, which is one of the particular features of our study. The proportion of contacted to symptomatic case in 14 days was significantly higher in aged older than 80 years group compared with the aged 65–79 years group in our study, which owing to the aged older than 80 years elderly were mostly accompanied by their families. Familial cluster of infected with COVID-19 have been reported in homes, especially without obvious symptoms. If the asymptomatic and mild cases cannot be found or ignored, they will spread the virus to others quickly. Therefore, to identify and control the infected cases, as well as early quarantine for their close contacts, especially in families are important measures to prevent transmission of the COVID-19 infection in older population.
This study has some limitations. First, only the COVID-19 confirmed older cases transferred by EMS in Beijing were included, the first admission to the designated hospitals cases were not enrolled, nor other provinces or cities which dominated by imported. It would be better to cover as wide population as possible to get more accurate results. Second, the observation time of this study is 39 days, which is still short, many patients need time to further observed. However, this study represents characteristics of early stage of COVID-19 confirmed elderly in Beijing, which has practical significance for the control and research of the older patients.
5. Conclusions
The older confirmed patients with COVID-19 infection has a high proportion of severe cases, and the COVID-19 infection is generally susceptible with a relatively high fatality rate in older population. We should pay more attention to the older patients.
Funding
This study was supported by funding from Beijing Municipal Science and Technology Project (Z191100004419003).
CRediT authorship contribution statement
Shengmei Niu: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Supervision, Writing - original draft. Sijia Tian: Formal analysis, Investigation, Methodology, Resources, Supervision. Jing Lou: Data curation, Investigation. Xuqin Kang: Data curation. Luxi Zhang: Data curation. Huixin Lian: Data curation. Jinjun Zhang: Conceptualization, Funding acquisition, Investigation, Validation, Visualization, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
All authors declare to have no conflict of interest.
Acknowledgments
We thank all the Beijing EMS staff for their efforts in transferring the confirmed patients,we thank all patients involved in this study.
References
- Chan J.F.W., Yuan S., Kok K.H., To K.K.W., Chu H., Yang J.…Yuen K.Y. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y.…Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. Epub 2020 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng S.Q., Peng H.J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. Journal of Clinical Medicine. 2020;9(2) doi: 10.3390/jcm9020575. undefined. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauci A.S., Lane H.C., Redfield R.R. Covid-19 - navigating the uncharted. The New England Journal of Medicine. 2020 doi: 10.1056/NEJMe2002387. undefined (undefined), undefined. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z.L., Liu C., Guan X.P., Mor V. China’s rapidly aging population creates policy challenges in shaping a viable long-term care system. Health Affairs. 2012;31(12):2764–2773. doi: 10.1377/hlthaff.2012.0535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X.…Zhong N.S. Clinical Characteristics of Coronavirus Disease 2019 in China [published online ahead of print, 2020 Feb 28] The New England Journal of Medicine. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- High K.P., Bradley S.F., Gravenstein S., Mehr D.R., Quagliarello V.J., Richards C. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities 2008 update by the Infectious Diseases Society of America. Journal of the American Geriatrics Society. 2009;57(March (3)):375–394. doi: 10.1111/j.1532-5415.2009.02175.x. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji Y.P., Ma Z.R., Maikel P.P., Pan Q.W. Potential association between COVID-19 mortality and health-care resource availability. The Lancet Global Health. 2020 doi: 10.1016/s2214-109x(20)30068-1. Published: February 25, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston A., Robinson L., Booth H., Knapp M., Jagger C. Projections of multi-morbidity in the older population in England to 2035: Estimates from the population ageing and care simulation (PACSim) model. Age and Ageing. 2018;47(3):374–380. doi: 10.1093/ageing/afx201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low L.L., Kwan Y.H., Ko M.S.M., Yeam C.T., Lee V.S.Y., Tan W.B.…Thumboo J.L. Epidemiologic characteristics of multimorbidity and sociodemographic factors associated with multimorbidity in a rapidly aging asian country. JAMA Netw Open. 2019;2(11) doi: 10.1001/jamanetworkopen.2019.15245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elisabeth M. Coronavirus covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641. doi: 10.1136/bmj.m641. undefined. [DOI] [PubMed] [Google Scholar]
- New coronavirus pneumonial diagnosis and treatment program (5th ed.) (in Chinese). (2020).http://www.nhc.gov.cn/xcs/zhengcwj/202002/3b09b894ac9b4204a79db5b8912d4440.shtml (Accessed Feb 20, 2020).
- Peng Y.D., Meng K., Guan H.Q., Leng L., Zhu R.R., Wang B.Y.…Zeng Q.T. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(0):E004. doi: 10.3760/cma.j.cn112148-20200220-00105. [DOI] [PubMed] [Google Scholar]
- Rasmussen S.H., Andersen R.K., Thinggaard M., Jeune B., Skytthe A., Christiansen L.…Christensen K. Cohort profile: The 1895, 1905, 1910 and 1915 Danish birth cohort studies - secular trends in the health and functioning of the very old. International Journal of Epidemiology. 2017;46(6) doi: 10.1093/ije/dyx053. 1746–1746j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Ahmed A.…Agha R. World health organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) International Journal of Surgery. 2020 doi: 10.1016/j.ijsu.2020.02.034. S1743-9191(20)30197-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P., Qie S., Liu Z., Ren J., Li K., Xi J. Clinical characteristics of 50466 hospitalized patients with 2019-nCoV infection. Journal of Medical Virology. 2020 doi: 10.1002/jmv.25735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P.F., Lu X.S., Xu C., Sun W.J., Pan B. Understanding of COVID-19 based on current evidence. J. Med. Virol. 2020 doi: 10.1002/jmv.25722. undefined(undefined), undefined. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Tang J.M., Wei F.Q. Updated understanding of the outbreak of 2019 novel coronavirus (2019‐nCoV) in Wuhan, China. Journal of Medical Virology. 2020;92(4):441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. World experts and funders set priorities for COVID-19 research.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200303-sitrep-43-covid-19.pdf?sfvrsn=2c21c09c_2 (Accessed March 3, 2020) [Google Scholar]
- Wu Y.C., Chen C.S., Chan Y.J. The outbreak of COVID-19: An overview. Journal of the Chinese Medical Association. 2020;83(3):217–220. doi: 10.1097/JCMA.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J., Liu J., Zhao X.G., Liu C.Y., Wang W., Wang D.W.…Li L.J. Clinical characteristics of imported cases of COVID-19 in Jiangsu province: A multicenter descriptive study. Clin Infect Dis. 2020;2020 doi: 10.1093/cid/ciaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z.Y., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. Published online February 24, 2020. [DOI] [PubMed] [Google Scholar]
- Xu X., Yu C.C., Qu J., Zhang L.G., Jiang S.F., Huang D.Y.…Luo L.P. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2 [published online ahead of print, 2020 Feb 28] European Journal of Nuclear Medicine and Molecular Imaging. 2020 doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H.Y., Duan G.C. Analysis on the epidemic factors for the corona virus disease. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(0):E021. doi: 10.3760/cma.j.cn112150-20200227-00196. [DOI] [PubMed] [Google Scholar]
- Yang W.J., Cao Q.Q., Qin L., Wang X.Y., Cheng Z.H., Pan A.…Yan F.H. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):A multi-center study in Wenzhou city, Zhejiang, China [published online ahead of print, 2020 Feb 26] The Journal of Infection. 2020 doi: 10.1016/j.jinf.2020.02.016. S0163-4453(20)30099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X.B., Yu Y., Xu J.Q., Shu H.Q., Xia J.A., Liu H.…Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine. 2020;2020 doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]