Dear Editor,
There is an increase in scientific publications related to COVID-19 since the first case of atypical pneumonia was reported in December 2019. Since that, contagions by SARS-CoV-2 spread worldwide, and, as a consequence, the World Health Organization declared COVID-19 as a pandemic. COVID-19 arrived in Latin America and specifically to Colombia via the intercontinental flights between Colombia and Europe and, to a lesser extent, from the US, since those destinations are among the most frequented by the Colombian citizens. Thus, concerns about the migratory flow via air transport were raised by medical and scientific institutions because of the insufficient control applied to national and foreign travelers, to the point of non-compliance with the incipient restrictive measures initially implemented. Furthermore, the Colombian government closed all land, sea, and river borders on March 17, 2020, but international and national flights were maintained until March 22, 2020. Since the detection of the first case on March 6, 2020, 240 cases were reported in the country until the closure of the airports. At this point, 63.8% of the cases were imported. Later, the number of confirmed imported cases would increase by up to 770 (24.8%). Up to April 15, 2020, the Colombian Ministry of Health had reported 3105 positive cases for COVID-19, of which 452 had recovered, but 131 had died [1]. 31.9% of infected people are closely related to infected travelers. Moreover, the rest of the cases (43.3%) still have an undetermined epidemiological nexus [1].
From January to the end of March, 875,021 travelers entered the country, mainly from the US (30.1%) and Spain (9%), the current major infection hot-spots [2]. Given the lack of epidemiological control, until the first measures were adopted on March 17, 2020, an important number of incoming travelers during January, February, and early March might act as disseminators of the SARS-CoV-2 in the country. As expected, a high number of undetected infection spots significantly increased the number of infected people after the closure of the borders. Colombia has twelve international airports, but the main and most connected airport (El Dorado Intl. Bogotá) concentrated 70% of the total migratory flow, and currently, this city presents almost half of the reported cases [1,2].
Colombia's health system is made up of a social security sector and a private sector with global coverage of 96% of 49.07 million people. The public sector, through a subsidized system, attends the half of the population, but the critical situation arises from the number of institutions with the adequate complexity level of attention. In Colombia, only 423 institutions are considered 3rd level hospitals with a total of 7000 CCUs beds (increased about 30% recently). According to the Pan American Health Organization (PAHO), vulnerability and inequity of the Colombian population have been exacerbated by the armed conflict, the scarce institutional coverage, and corruption in addition to nutritional deficiencies, little access to health care, education, and decent housing [3]. Thus, the national health system is placed in a context of extreme vulnerability under the COVID-19 pandemic scenario.
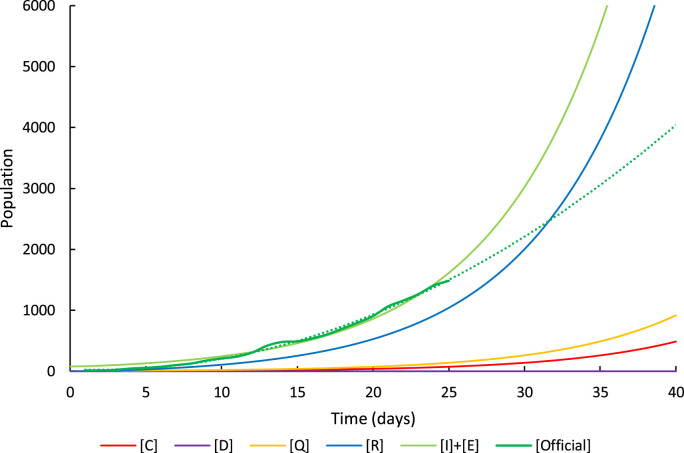
During the first 30 days the number of cases in Colombia followed a typical SEIR (Susceptible - Exposed - Infectious - Recovered) model, agreeing the parameters observed for Wuhan outbreak; i.e., mean latent time (α-1) of 2 days, mean quarantine time (γ-1) of 6.5 days and reproduction number R0 of 2.67 [4,5]. Although increasing, the fatality rate (κ) in Colombia has been 2.4% so far, and the critical rate (c) 4.6% [1]. The calculated mean square error of the SEIR model was 1.2 × 10-6. Our simulations showed that the initial evolution of cases coincided with a non-social distancing scenario (even during quarantine), probably due to the delay in the detection of cases and initial lack of control of infected people (Fig. 1 ). Nevertheless, the reports after April 5, 2020, started to evidence the effect of the quarantine showing a slight but sustained decrease in the daily rate of confirmed cases [1]. The short-term projection of the infection curve has a lower slope compared with the initial trend (Fig. 1), which is presumably the result of quarantine measures. Therefore, under the current situation, the national health system is still not under pressure.
Fig. 1.
Simulation of exposed and infective [I] + [E], recovered [R], quarantined [Q] critical [C] and dead [D] people caused by COVID-19 in Colombia in a non-social distancing scenario. Dashed green line is the current projection of the infection curve. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Nevertheless, concerns remain due to the initial scarce control of the travelers, in addition to the free mobility during the initial stages of the outbreak. Moreover, infection spots are appearing in unexpected places during the quarantine, in addition to a delay in detection of more than 5 days, and the undetermined presence of asymptomatic carriers make critical the maintenance of distancing measures beyond the end of April. Careful return of a minimum of essential workers to the industries and reduction of agglomerations in public transport during May are required to maintain the decreasing trend of the infection curve.
Declaration of competing interest
The authors declare that there is no conflict of interest or financial disclosure about this manuscript.
References
- 1.Instituto Nacional de Salud de Colombia . 2020. COVID 2019 en Colombia. [Google Scholar]
- 2.Migración Colombia . 2020. Flujos migratorios de Colombianos y extranjeros. [Google Scholar]
- 3.Pan American Health Organization . 2017. Health in the Americas. Washington, D.C. [Google Scholar]
- 4.Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Trav Med. 2020:1–4. doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng L., Yang W., Zhang D., Zhuge C., Hong L. Epidemic analysis of COVID-19 in China by dynamical modeling. MedRxiv. 2020;2020 doi: 10.1101/2020.02.16.20023465. 02.16.20023465. [DOI] [Google Scholar]