Food Insecurity and Food Allergy
As coronavirus disease 2019 (COVID-19) spreads in communities across America, local, state, and federal agencies are working to reduce the impact of food insecurity. The US Department of Agriculture (USDA) defines food insecurity as inadequate access to affordable and nutritious food. In 2018, 11% of US households were considered food insecure, meaning they had difficulty at some time during the year obtaining enough food for all members of their household, due to lack of resources.1 Pandemics adversely affect food supply chains and as COVID-19 impacts the lives of millions of Americans, the greatest burden will be felt by low-income families.2 Although drastic measures are being taken to reduce the impact of COVID-19, food-insecure families with food allergies (FAs) and other food-related conditions remain vulnerable.
FA is a potentially life-threatening condition, affecting 10.6% of adults3 and 7.6% of children in the United States.4 Patients with FA must eliminate allergens from their diet, resulting in costly grocery bills and an impaired quality of life.5 Although 170 foods have been reported to cause allergic reactions, the 9 most common food allergens are peanut, milk, egg, soy, tree nut, wheat, fish, shell-fish, and sesame. Elimination of a common allergen, especially milk or wheat, can have a major impact on the nutritional needs of a child,6 negatively affecting short- and long-term health outcomes. In addition, individuals with FA can place great strain on the labored health care system, with frequent emergency department visits due to severe FA reactions. Children with FA in the lowest income stratum spend 2.5 times more on emergency department and hospitalization costs, partially due to limited access to allergen-friendly foods.7 Therefore, it is crucial to ensure these families have access to the necessary foods.
Access Challenges in Federal Nutrition Programs
Recently Congress passed the Family's First Coronavirus Response Act, granting funding and flexibilities for federal nutrition programs.8 Although this provides greater access to the Supplemental Nutrition Assistance Program, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and The Emergency Assistance Program (TEFAP), challenges remain for food-insecure individuals living with FA and related conditions. The Supplemental Nutrition Assistance Program, the nation's largest and most effective nutrition program, provides food-insecure families a monthly stipend to purchase groceries. However, its policies do not fully consider the unique food needs, increased cost burdens, and consequences of food allergen exposure experienced by families with FA.
Currently, the Summer Feeding Program and Senior Farmers' Market Nutrition Program do not provide increased reimbursements to accommodate medical meal modifications for patients with FA or other food-related conditions.9 Therefore, school districts and community organizations that use these programs to provide emergency access to meals will not have funding to provide these resources. In addition, WIC makes limited accommodations for those with dietary restrictions and as the pandemic causes food shortages, the situation for families relying on their services will worsen.
The Emergence Food System
The Emergency Food Assistance Program, which assists families during the pandemic, often does not offer FA- friendly foods. As COVID-19 rampages across the country, food pantries must implement pandemic protocols. This entails limiting clients' choices, opting for predetermined boxed distribution instead, making it harder for families with FA to obtain medically necessary foods.
According to Feeding America's Map the Meal Gap (2018),10 97% of US counties include families facing hunger who are likely ineligible for federal nutrition assistance, and must rely on the charitable feeding system. During the pandemic, such programs face several challenges, including reduced volunteer support due to social distancing guidelines. This leads to the shutting down of food pantries, limiting access to food assistance.
Further compounding access issues at food pantries is the lack of allergen-free options, which provide essential nutrients, particularly for children. One recent study suggests children with FA living in food-insecure households and relying on nutrition assistance programs are at increased risk of exposure to food allergens and have more frequent life-threatening reactions.11 Family's First Coronavirus Response Act increased funding for the federal government to purchase surplus commodities for distribution in TEFAP. Although this increases access, the program still lacks procurement policies to ensure a minimum percentage of commodities are free of the top allergens.
To our knowledge, of the 60,000 food pantries and soup kitchens in the United States only 4 exclusively stock allergen-free foods consistently. Currently, only 2 are operational during the pandemic: the Food Equality Initiative (FEI)12 and the Rachel Way Food Pantry.13
Innovative Solutions to Fill the Gap
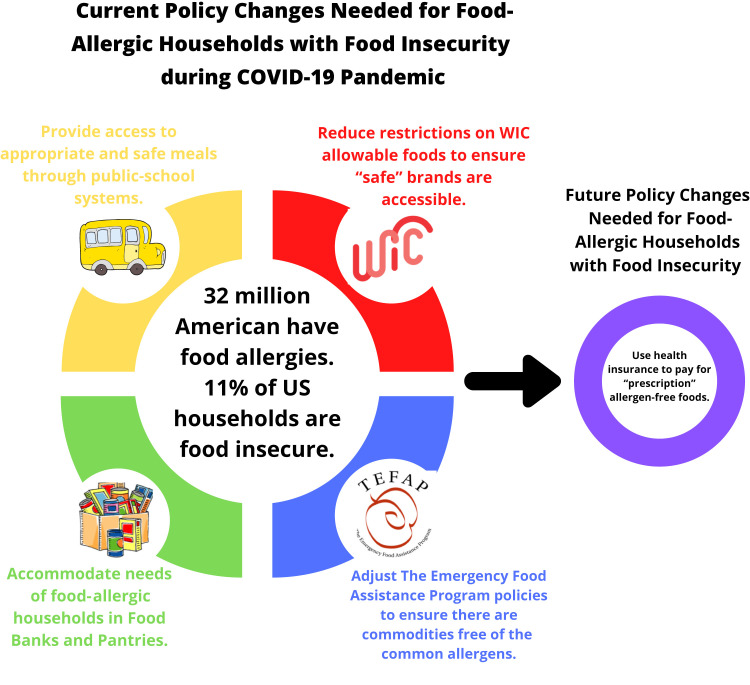
The challenges posed by the pandemic provide opportunities for health systems to address food insecurity among families with FA using several models (Figure 1 ) that create an equitable environment for families at all socioeconomic levels. One promising option is using health insurance to pay for “prescription” allergen-free foods. Another would be to expand the current models used by allergen-free food pantries to a national level.
Figure 1.
Policy changes needed for food-allergic households with food insecurity.
As mentioned above, the FEI is a patient advocacy organization that operates a network of allergen- and gluten-free food pantries. Although there are no residency requirements, the organization currently serves 26 counties surrounding Kansas City, Missouri. Their Allergy Friendly and Gluten Free Nutrition Assistance Program provides supplemental nutrition and education, to help clients adhere to prescribed diets. Foods provided include nondairy milk, seed butter, egg replacers (such as flaxseed), alternative grains, fresh produce, and much more. Clients must meet these qualifying criteria: (1) diagnosed FAs or celiac disease and (2) proof of income at or below 250% of US Poverty Income Guidelines. During the pandemic, FEI clients receive food through no-contact deliveries and shipments through the US Postal Service. The Rachel Way Pantry takes a different approach by creating an online pantry for clients in Plymouth, Pennsylvania. Their clients order allergen-safe foods they require online and then are sent a grocery gift card to purchase those items.
Our recommendation for the country at this time includes systemic policy changes for local, state, and federal agencies that coordinate nutrition programs.
-
1.
Lunches provided by public-school systems—Honor existing meal modifications by providing access to appropriate and safe meals during meals-to-go distribution. Information on how to access special dietary meals should be communicated to the public. This may require increased reimbursements from the Summer Feeding Program.
-
2.
WIC—Reduce brand and size restrictions on WIC-allowable foods to ensure “safe” brands are accessible through the program for each state. Food and Nutrition Services can adjust the 100% whole wheat standard to 100% whole grain to increase access to whole grain foods.
-
3.
Food Banks and Food Pantries—Allow clients to indicate FAs and other related conditions on enrollment and pick-up forms. If possible, food banks and pantries should allocate a minimum percentage of their procurement dollars to source foods free of the top 9 common allergens.
-
4.
TEFAP—Adjust procurement policies to ensure a minimum percentage of commodities purchased are free of the top 9 common allergens and labeled in accordance with the Food Allergen Labeling and Consumer Protection Act.
Conclusions
The COVID-19 pandemic has several adverse economic and health implications; therefore, cross-sector collaborations are needed to solve complex problems and improve health outcomes. Measures must be immediately taken by local, state, and federal agencies to reduce the burden on vulnerable populations experiencing food insecurity. In addition, allergy specialists can screen patients for the social determinants of health to determine whether they are at risk for food insecurity, because the cost of allergen-free groceries may be underestimated. There is an increasing need for health systems to fund interventions that reduce health disparities and provide critical resources to at-risk populations.
Footnotes
This article was supported by the Center for Food Allergy and Asthma Research (R.S.G).
Conflicts of interest: R. S. Gupta reports receiving grants from the National Institutes of Health (grant nos. R21 ID # AI135705, R01 ID# AI130348, and U01 ID # AI138907), Rho Inc, Stanford Sean N. Parker Center for Allergy Research, UnitedHealth Group, Thermo Fisher Scientific, Genentech, and the National Confectioners Association; and serves as a medical consultant/advisor for Before Brands, Kaléo, Inc, Genentech, Institute for Clinical and Economic Review, Food Allergy Research & Education, Aimmune Therapeutics, and DBV Technologies. L.A. Bilaver reports receiving grants from the National Institutes of Health, Rho, Inc, Thermo Fisher Scientific, Genentech, National Confectioners Association, Before Brands, and Food Allergy Research and Education The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Coleman-Jensen A., Rabbitt M.P., Gregory C.A., Singh A. U.S. Department of Agriculture, Economic Research Service; Washington, DC: 2019. Household food security in the United States in 2018. Economic Research Report Number 270. [Google Scholar]
- 2.Huff A.G., Beyeler W.E., Kelley N.S., McNitt J.A. How resilient is the United States’ food system to pandemics? J Environ Stud Sci. 2015;5:337–347. doi: 10.1007/s13412-015-0275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta R.S., Warren C.M., Smith B.M., Jiang J., Blumenstock J.A., Davis M.M. Prevalence and severity of food allergies among US adults. JAMA Network Open. 2019;2:e185630. doi: 10.1001/jamanetworkopen.2018.5630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R.S., Warren C.M., Smith B.M., Blumenstock J.A., Jiang J., Davis M.M. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics. 2019;143:e20183835. doi: 10.1542/peds.2018-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warren C.M., Otto A.K., Walkner M.M., Gupta R.S. Quality of life among food allergic patients and their caregivers. Curr Allergy Asthma Rep. 2016;16:38. doi: 10.1007/s11882-016-0614-9. [DOI] [PubMed] [Google Scholar]
- 6.Mehta H., Groetch M., Wang J. Growth and nutritional concerns in children with food allergy. Curr Opin Allergy Clin Immunol. 2013;13:275–279. doi: 10.1097/ACI.0b013e328360949d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bilaver L.A., Kester K.M., Smith B.M., Gupta R.S. Socioeconomic disparities in the economic impact of childhood food allergy. Pediatrics. 2016;137:e20153678. doi: 10.1542/peds.2015-3678. [DOI] [PubMed] [Google Scholar]
- 8.H.R. 6201 — 116th Congress: Families First Coronavirus Response Act. 2020. www.GovTrack.us Available from:
- 9.U.S. Department of Agriculture FNS Nutrition Programs Food and Nutrition Service. https://www.fns.usda.gov/programs Available from:
- 10.Gundersen C., Dewey A., Crumbaugh A., Kato M., Engelhard E. Feeding America; Chicago, IL: 2018. Map the Meal Gap 2018: A Report on County and Congressional District Food Insecurity and County Food Cost in the United States in 2016. Available from: https://www.feedingamerica.org/sites/default/files/research/map-the-meal-gap/2016/2016-map-the-meal-gap-all-modules.pdf. Accessed April 28, 2020. [Google Scholar]
- 11.Tackett A.P., Farrow M.L., McQuaid E.L. Food security, utilization of food assistance programs, and caregiver perceptions of food-induced anaphylaxis risk in children with food allergies. Pediatric Allergy Immunol Pulmonol. 2018;31:91–96. [Google Scholar]
- 12.Food Equality Initiative https://foodequalityinitiative.org/ Home. Available from: Accessed April 23, 2020.
- 13.Rachel Way Food Pantry http://www.therachelway.org/ The Rachel Way - Home. Available from: Accessed April 23, 2020.