Abstract
Objective
The novel coronavirus disease 2019 (COVID-19) pandemic poses a substantial threat to the health of health care personnel on the front line of caring for patients with COVID-19. The Centers for Medicare and Medicaid Services have announced that all nonessential planned surgeries and procedures should be postponed until further notice and only urgent procedures should proceed. Neurologic surgeries and procedures should not be delayed under the circumstance in which it is essential at saving a life or preserving functioning of the central nervous system.
Methods
With the intent to advise the neurosurgery team on how to adequately prepare and safely perform neurosurgical procedures on confirmed and suspected patients with COVID-19, we discuss considerations and recommendations based on the lessons and experience shared by neurosurgeons in China.
Results
Perioperative and intraoperative strategies, considerations, as well as challenges arisen under the specific circumstance have been discussed. In addition, a case of a ruptured aneurysm in a suspected patient with COVID-19 is reported. It is advised that all health care personnel who immediately participate in neurosurgical surgeries and procedures for confirmed and suspected patients with COVID-19 should take airborne precautions and wear enhanced personal protective equipment.
Conclusions
Following the proposed guidance, urgent neurosurgical surgeries and procedures can be safely performed for the benefit of critical patients with or suspected for COVID-19.
Key words: COVID-19, Neurosurgical procedures, Pandemic, Personal protective equipment, SARS-CoV-2
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; CT, Computed tomography; OR, Operating room; PPE, Personal protective equipment; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2
Introduction
The novel coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in the city of Wuhan, China, in December 2019. Despite strenuous efforts to contain the virus, it quickly turned into a pandemic that has swept through all continents except Antarctica. With an exponentially increasing number of patients being diagnosed, COVID-19 heavily strains our health care system and resources. In response to the escalating pandemic of the COVID-19, the Centers for Medicare and Medicaid Services announced that all nonessential planned surgeries and procedures be postponed until further notice.
As per the Centers for Medicare and Medicaid Services tiered framework, neurosurgery falls under the category of tier 3a (high acuity surgery), and it should not be postponed.1 The Centers for Disease Control and Prevention informed that COVID-19 could spread through close contact or respiratory droplets between persons and from contact with contaminated surfaces or objects.2 However, whether COVID-19 could be airborne is still in dispute. Nonetheless, airborne precautions should be taken while performing neurosurgical procedures on all confirmed or suspected patients with COVID-19.
The first case with a wide nosocomial spread of COVID-19 in Wuhan was an endoscopic endonasal transsphenoidal pituitary tumor resection.3 All 14 people who spent time in the operating room (OR) during the procedure became infected. The standard surgical gowns and masks worn by health care personnel do not protect them from contracting COVID-19. With the intent to advise the neurosurgery team on how to adequately prepare and safely perform life-saving neurosurgical procedures amid the pandemic of COVID-19, we discuss the following considerations and recommendations based on the lessons and experience shared by neurosurgeons in China. Rather than serving as stand-alone guidance, these recommendations should be integrated into the systemic planning and preparation implemented by health care facilities and systems.
General Treatment Strategies for Intensive Care Unit Procedures
Except for emergent and urgent neurosurgical procedures that can save a life, preserve the brain, or restore spinal cord function, other nonurgent elective spine surgeries, peripheral nerve surgeries, pain procedures, and functional procedures should be postponed. When deemed emergent or urgent, airborne precautions must be taken before and during contact with confirmed or suspected COVID-19 cases. Inpatients with suspected COVID-19 should be treated as a confirmed case for neurosurgical bedside procedures. Each patient should be placed separately in a negative-pressure isolation room. Only essential health care personnel should be allowed to treat patients with COVID-19 to minimize medical trainees or students' exposure to the virus. A properly fitted N95 or higher respirator must be used. All health care personnel should undergo respirator fit testing before participating in the patient's care. It is recommended that men with beards shave their face to ensure a tight seal between their face and the mask. A gown spanning and covering the entire body (coverall gown), protective goggles, and shoe covers are recommended. Avoid touching the eyes, nose, or mouth after taking off the face mask or goggles at the completion of the procedure.
General Guidelines During Perioperative Care and Transportation
Collaborate with the anesthesia team and hospitality team to secure a smooth transition between perioperative care and the neurosurgical procedure. A designated patient transport route should be established for patients with COVID-19. The patient should wear an N95 respirator during transit. If the patient is already intubated, a mask should be placed over the mouth to avoid any respiratory secretions or droplets contamination due to cough reflex. The preoperative holding area and the postanesthesia care unit should be bypassed if an isolation room is not available in these areas to limit potential contamination of these units. When obtaining consent, telecommunication is strongly recommended. If the patient is to return to the designated intensive care unit or medical ward directly, extubation and postoperative recovery should be allowed in the OR to further minimize the number of staff members directly exposed to the patient's airway. The patient care team should be prepared with enhanced personal protective equipment (PPE) for possible immediate medical intervention and avoid procedures performed with inadequate protection. Wearing a minimum of 2 sets of gloves is recommended during perioperative care and patient transit.
Intraoperative Strategies and Considerations
All health care personnel in the OR should be prepared both mentally and physically. The operation should be performed in a negative-pressure OR paired with an anteroom implemented with airborne precautions.4 In the case in which a negative-pressure OR is not available, an HEPA (i.e., high-efficiency particulate air) standard filtering system should be implemented. Surgeons in the OR must undergo a careful sequence for putting on proper PPE in addition to sterile surgical gown prior to performing the neurosurgical procedure.5 , 6 First, a visual inspection of PPE is performed to ensure that no gross defects are present. Hand washing is performed with soap and water for a minimum of 20 seconds. Shoe covers and nonsterile inner gloves are obtained. A gown is worn that covers the entirety of arms, legs, head, and trunk (coverall gown). Then, a properly fitting N95 or higher respirator is used. Next, a surgical hood, goggles, and face shield are put on. Sterile gloves, sterile gown, and a second set of sterile gloves are fitted and worn outside of the sterile gown.
Wearing goggles will prevent the use of surgical loupes. Goggles with an anti-fog coating are recommended, as they may block vision when covered in fog. Furthermore, wearing goggles and face shield makes performing surgery under the neurosurgical microscope exceedingly difficult. Three layers of gloves diminish tactile sensation and make it less reliable during neurosurgical procedures. Wearing this extensive amount of PPE for a prolonged period during a neurosurgical operation may make the surgeon fatigued and dehydrated due to excessive sweating. Communication among the health care providers may become difficult, given the muffled voices and hearing that results from multiple layers of PPE. Additional measures, including the use of hand gestures, may be required for communication during the surgery.7 An example of health care personnel wearing proper PPE is provided in Figure 1 .
Figure 1.
(A) Making sure N95 mask is well-fitting. (B) HEPA (i.e., high-efficiency particulate air) filter used in the operating room (OR) if a negative-pressure OR room is not available. (C) Putting on goggles and wearing proper personal protective equipment (PPE). (D) Now in proper PPE in a coronavirus disease 2019 OR environment.
Other personnel, including anesthesiologists, surgical technologists, and circulating nurses in the OR, should also be equipped with proper PPE. Personnel entering and leaving the OR should be rigorously restricted. A buffering area outside the OR should be used for the delivery of surgical supplies operated by a designated team. This team also should be fully protected and be ready to enter the OR should an emergency arise. All equipment used during the procedure should be thoroughly sterilized or properly disposed of to prevent viral spread. Health care providers involved should perform immediate self-cleaning before leaving the procedure area, preferably showering the whole body and changing into a new surgical outfit.
A Suspected COVID-19 Patient with a Ruptured Aneurysm
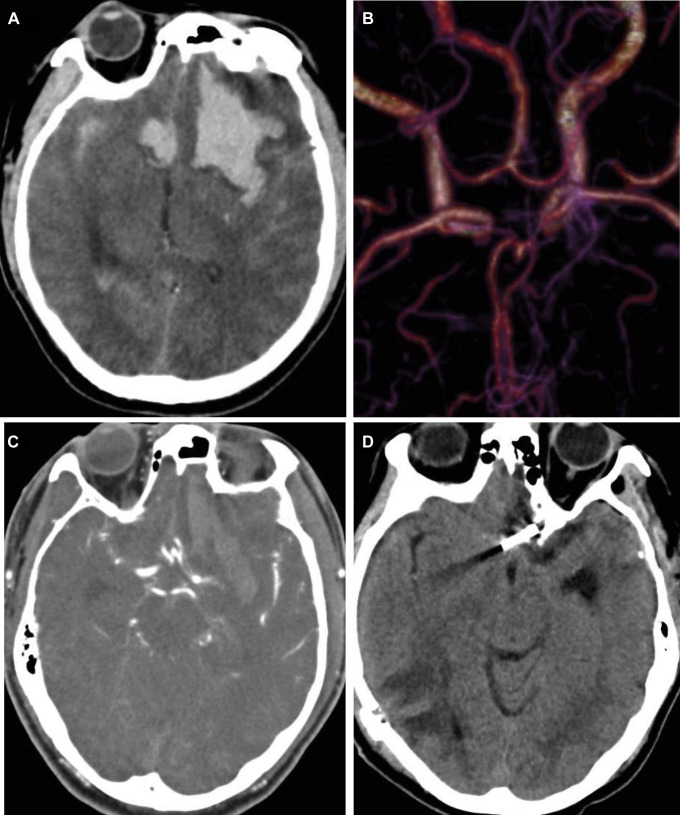
On February 6, 2020, a patient presented to the emergency department with headache followed by a loss of consciousness at a local hospital in Guangzhou. Computed tomography (CT) scan of the head revealed subarachnoid hemorrhage and left frontal lobe hematoma (Figure 2A ). The patient was then transferred to our facility for neurosurgical consultation and treatment. Upon arrival, the patient was unconscious, body temperature 38.9°C (102°F), pulse 61 bpm, respiratory rate 17 bpm, and blood pressure 179/120 mm Hg. Neurologic examination showed bilateral pupil diameter 2.5 mm, sluggish pupillary light reflex, nuchal rigidity, extremities withdrawal to pain, bilateral positive Babinski sign. Glasgow Coma Scale was 5 points, Hunt & Hess was grade 4, Modified Fisher's Scale was grade 4, and World Federation of Neurosurgical Societies grading system score was grade 5. Medical history was unremarkable, with no hypertension or diabetes mellitus. There was no family history of subarachnoid hemorrhage. The patient had a history of traveling to Hubei province, where COVID-19 started and became the epicenter in China. The patient's family stated that the patient returned from Hubei province 12 days ago and started having a fever the day of presentation to the emergency department. Given the travel history and high body temperature, we suspected that the patient contracted the SARS-Cov-2 virus during the trip to Hubei province.
Figure 2.
(A) Computed tomography (CT) of the head showed subarachnoid hemorrhage and left frontal lobe hematoma. (B and C) CT angiography of the patient showed an anterior communicating artery aneurysm ([B] 3-dimensional reconstruction; [C] source image). (D) Two-month follow-up CT of the head showed improvement.
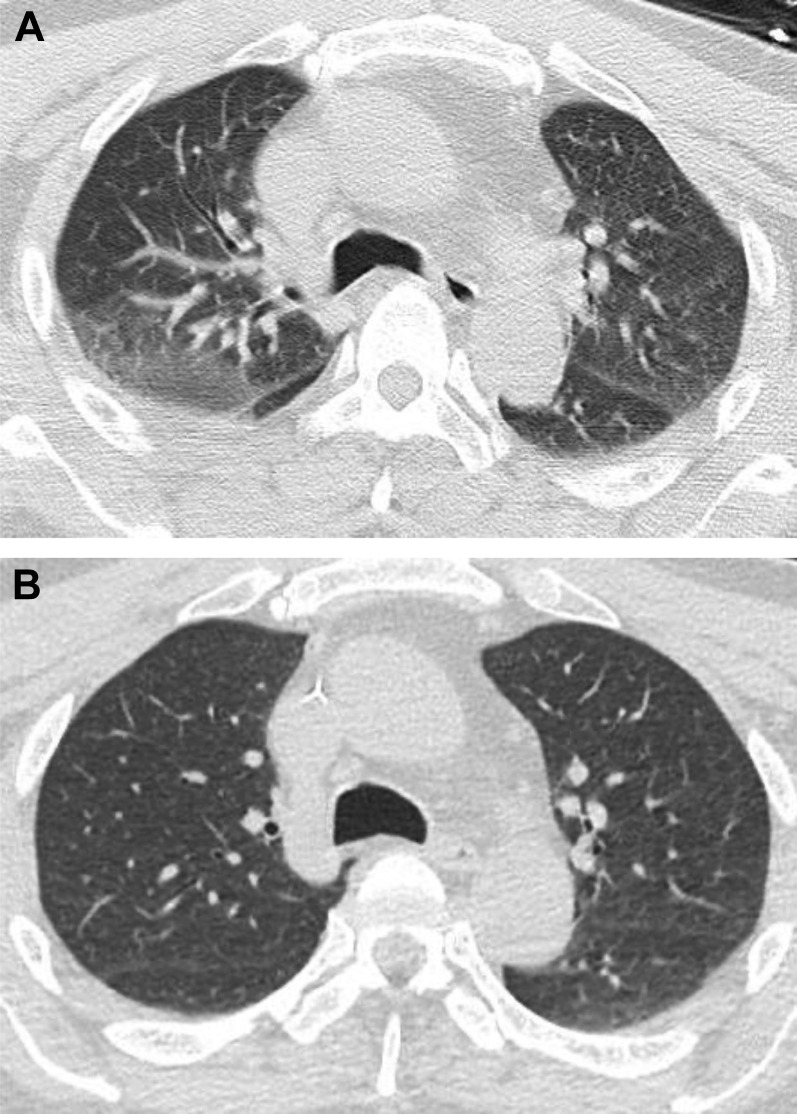
The COVID-19 task force of our hospital was consulted, and a suspected diagnosis of COVID-19 was made. Specimens were collected for testing. A nasopharyngeal swab sample was sent for reverse-transcription polymerase chain reaction testing for SARS-CoV-2 virus. CT angiography of the head (Figure 2B and C) and thoracic CT were obtained, with all health care personnel in enhanced PPE. CT angiography of the head revealed an anterior communicating artery aneurysm. Thoracic CT showed bilateral lower lobe inflammatory changes and suspected right upper-lobe exudative change (Figure 3A ). Definitive aneurysm repair procedure was deemed necessary and urgent by the neurosurgery team; the COVID-19 emergency surgery protocol was then activated. A negative-pressure OR was requested, and the anesthesiology team was informed of the situation and the planned surgical treatment. An isolation room was reserved for the patient for immediate postoperative care. The patient was transitioned to the OR through the designated route. All participating health care personnel was wearing enhanced PPE, as mentioned previously (Figure 4 ). The patient underwent a modified pterional craniotomy for hematoma evacuation with anterior communicating artery aneurysm clipping, and placement of intracranial pressure monitor.
Figure 3.
(A) Thoracic computed tomography (CT) scan showed bilateral lower-lobe inflammatory changes and suspected right upper lobe exudative change. (B) At 2-month follow-up, thoracic CT scan showed resolved inflammatory changes and now normal lungs.
Figure 4.
All health care personnel wearing enhanced PPE during the surgery in the OR.
After surgery, the patient was transported to an isolation room for recovery and postoperative care, as well as COVID-19 treatment. The nasopharyngeal testing of COVID-19 returned to be negative. However, due to the high false-negative rate (30%) of the testing and the patient's symptoms and CT findings, a decision was made by the COVID-19 task force to treat the patient as a patient under investigation for 14 days. The patient did well and eventually was discharged home at 14 days postoperatively with intact neurologic function. Two-month postoperative CT of the head (Figure 2D) was obtained, which showed resolved hematoma, stable aneurysm clip, and no hydrocephalus. A thoracic CT also was obtained and showed improvement from previous hospital admission images (Figure 3B).
Conclusions
Although not without challenges, with proper protection following the aforementioned guidance, emergent and urgent neurosurgical surgeries and procedures can be safely performed for the benefit of critical patients during the COVID-19 pandemic.
CRediT authorship contribution statement
Jun Wen: Data curation, Formal analysis, Investigation, Writing - original draft. Xiaoming Qi: Data curation, Formal analysis, Investigation, Writing - original draft. Kristopher A. Lyon: Investigation, Writing - original draft, Methodology. Buqing Liang: Investigation, Writing - original draft, Methodology. Xiangyu Wang: Conceptualization, Methodology, Project administration, Resources, Supervision, Writing - review & editing. Dongxia Feng: Methodology, Project administration, Writing - review & editing, Validation. Jason H. Huang: Conceptualization, Methodology, Project administration, Resources, Supervision, Validation, Writing - review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Jun Wen and Xiaoming Qi contributed equally to this article.
References
- 1.Centers for Medicare & Medicaid Services Adult Elective Surgery and Procedures Recommendations. https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf Available at:
- 2.Centers for Disease Control and Prevention How COVID-19 Spreads. (March 4, 2020) https://www.cdc.gov/coronavirus/2019-ncov/prepare/transmission.html Available at: [PubMed]
- 3.China Newsweek Restore the spreading route of a super-spreader. http://View.inews.qq.com/a/20200125A07TT200?uid=&devid=BDFE70CD-5BF1-4702-91B7- 329F20A6E839&qimei=bdfe70cd-5bf1-4702-91b7-329f20a6e839 Available at:
- 4.Chow T.T., Kwan A., Lin Z., Bai W. Conversion of operating theatre from positive to negative pressure environment. J Hosp Infect. 2006;64:371–378. doi: 10.1016/j.jhin.2006.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Ebola: personal protective equipment (PPE) donning and doffing procedures. https://www.cdc.gov/vhf/ebola/hcp/ppe-training/n95Respirator_Coveralls/donning_01.html Available at:
- 6.Centers for Disease Control and Prevention Sequence for putting on personal protective equipment (PPE) https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf Available at:
- 7.Chen X., Shang Y., Yao S., Liu R., Liu H. Perioperative care provider’s considerations in managing patients with the COVID-19 infections. Transl Perioper Pain Med. 2020;7:216–224. [Google Scholar]