Graphical abstract
Keywords: COVID-19, Outbreak, Prevention, Protective measures, Epidemiology, Public health
Highlights
-
•
The prevalence of WHO personal protective measures was approximately 60–85%.
-
•
The prevalence of avoiding touching the eyes, nose, and mouth was the lowest.
-
•
Only 34.7% implemented all 5 personal protective measures recommended by the WHO.
-
•
Some ordinary citizens may practice insufficient personal protective measures.
Abstract
Objectives
To clarify the implementation status of personal protective measures by ordinary citizens in Japan during the coronavirus disease 2019 (COVID-19) outbreak.
Methods
This was a cross-sectional study based on internet-based survey. A total of 2400 people (50% male: 20–79 years) were selected between February 25 and 27, 2020, from registrants of an Internet research company, to complete a questionnaire. Participants were asked to indicate how often they implemented the following five personal protective measures recommended by the World Health Organization (hand hygiene, social distancing measures, avoiding touching the eyes, nose and mouth, respiratory etiquette, and self-isolation). In addition, the participants responded to questions regarding the daily frequency of hand hygiene events.
Results
The prevalence of the five personal protective measures ranged from 59.8% to 83.8%, with the lowest being avoiding touching the eyes, nose, and mouth. In total, 34.7% implemented all personal protective measures. The median daily hand hygiene events were 5 per day (25th percentile, 75th percentile: 3,8).
Conclusions
The protective measures implemented by ordinary citizens are insufficient and further public awareness activities are required.
Introduction
The coronavirus disease 2019 (COVID-19) outbreak has become a global problem (WHO, 2020b). As of March 23, 2020, the global number of reported cases of COVID-19 totaled approximately 330,000 cases, with 14,510 deaths (WHO, 2020c). Japan reported the first case of laboratory-confirmed COVID-19 on January 15, 2020, following confirmed cases in China and Thailand (WHO, 2020d). The number of patients is increasing daily.
It is vital that personal protective measures are implemented by the public as a method to mitigate the epidemic of respiratory viruses such as COVID-19, especially before a well-matched vaccine is widely available (Qualls et al., 2017). The World Health Organization (WHO) recommends the following five main personal protective measures against the COVID-19: “wash your hands frequently” = hand hygiene, “maintain social distancing” = social distancing measures, “avoid touching the eyes, nose and mouth,” “practice respiratory hygiene” = respiratory etiquette, and “stay home if you feel unwell” = self-isolation (WHO, 2020a). The WHO also recommended that people should “stay informed and follow advice given by your healthcare provider, your national and local public health authority, or your employer” = obtaining information from a reliable source (WHO, 2020a). During the early phase of COVID-19 outbreak, in which there is no effective vaccine, how well the public implements these protective measures is an important issue.
The purpose of this study was to clarify the status of implementation of these protective measures by ordinary citizens in Japan during the early phase of COVID-19 outbreak.
Methods
Study sample and data collection
This was a cross-sectional study conducted through an internet-based survey. The survey was conducted between February 25 and February 27, 2020. At the time of the survey, there were sporadic cases of unknown transmission routes in multiple regions in Japan, and small clusters of patients in some regions of the country, mainly in urban areas. (JMHLW, 2020b). As of February 25, the number of reported cases of COVID-19 in Japan totaled 157 (WHO, 2020c). Outside Japan, a sudden increase in cases was reported in Italy, Iran, and South Korea (Figure 1 ) (WHO, 2020c). The study participants were recruited from the registrants of a Japanese Internet research service company called MyVoice Communication, Inc., which had approximately 1.12 million registered participants as of January 2020. In this study, we aimed to collect data from 2400 men and women aged 20 to 79 years (sampling by sex and 10-year age groups; 12 groups, n = 200 in each group) who were living in seven prefectures near the Tokyo metropolitan area (i.e., Tokyo, Kanagawa, Saitama, Chiba, Ibaraki, Tochigi, and Gunma). The Tokyo metropolitan area is home to approximately 35% of the total Japanese population (total area: 32,433.4 km2; total population: 43,512,238 people as of January 2019). The company invited registrants to participate in the survey by email on February 25 (n = 8156). The questionnaires were placed in a protected area of a website, and the potential respondents received a specific URL in their invitation email. When 200 participants in each group responded to the questionnaire voluntarily, we stopped accepting responses from that group, and concluded the survey on February 27 when 200 responses were collected from all groups. Reward points valued at 50 yen were provided as an incentive for participation (approximately 0.5 US dollars as of February 2020).
Figure 1.
Total cases of COVID-19 in Japan and in other countries (excluding China) at the time of this survey period.
Created based on World Health Organization coronavirus disease (COVID-2019) situation reports (WHO, 2020c).
Measurement
Assessment of the five personal protective measures as recommended by the WHO
Participants described self-reported implementation of the five personal protective measures (hand hygiene, social distancing measures, avoiding touching the eyes, nose and mouth, respiratory etiquette, and self-isolation) recommended by the WHO (WHO, 2020a). Regarding the four personal protective measures other than self-isolation, participants were asked about the frequency of implementation during the last week and responded using a 4-point-Likert scale (1. “Always,” 2. “Sometimes,” 3. “Rarely,” or 4. “Never”). As for social distancing measures, participants were asked to disclose the frequency as to which they avoided places where many people would be gathered together. Regarding self-isolation, the participants were asked the question, “if you have a fever or a cold, can you take time off from work?” Participants responded using a 4-point Likert scale (1. “Definitely can,” 2. “Probably can,” 3. “Probably can’t,” 4. “Definitely can’t”) or 5. “not working”.
Assessment of obtaining information from a reliable source
In this study, we defined reliable sources as healthcare workers and public institutions (Japanese Ministry of Health, Labour and Welfare, and WHO), and evaluated whether participants were obtaining information from a reliable source. Participants answered as to whether they obtained information on COVID-19 from either of the aforementioned sources. When participants indicated either source as their point of information, it was deemed that they obtained information from a reliable source.
Assessment of the total number of hand hygiene events per day
Regarding hand hygiene, the number of events per day was also evaluated. Participants reported the mean number of hand hygiene events using soap and water per day and the mean number of hand hygiene events using alcohol-based hand sanitizers per day. The sum of the two was defined as the total number of hand hygiene events per day.
Assessment of sociodemographic attributes
Participants reported their sex, age, marital status (not married/married), smoking (smokers/non-smokers), self-rated health (good/poor), past medical history (hypertension, diabetes, and respiratory disease), residential area (Tokyo/others), and seasonal influenza vaccination history (vaccinated/not vaccinated annually).
The research company provided categorized data as follows: living arrangement (with others/alone), educational attainment (university graduate or above), and household income level (<5 million yen or ≥5 million yen).
Statistical analysis
Regarding the five personal protective measures, when a participant responded 1 (“Always”/“Definitely can”) or 2 (“Sometimes”/“Probably can”) on the 4-point-Likert scale, it was determined that the personal protective measures were implemented (in this study, referred to as “loose standards”). We clarified the prevalence of each personal protective measure, implementing all personal protective measures, and obtaining information from a reliable source. The proportion of participants for each total number of implementing personal protective measures was also clarified. With regards to self-isolation, those who selected point 5, “not working” (n = 740), were excluded from the analysis. The prevalence of personal protective measures was calculated through the selection 1 of the 4-point Likert scale (“Always”/“Definitely can”), defined as the implementation of personal protective measures (in this study, referred to as “strict standards”). To clarify the association between each sociodemographic attribute and implementing all personal protective measures recommended by the WHO, a multivariate logistic regression analysis was performed. The dependent variable was implementing all personal protective measures under the loose standards, and the independent variables were sex, age (older adults (≥65 years old)/persons under 65 years old), marital status (not married/married), living arrangement (with others/alone), smoking status (smokers/non-smokers), residential area (Tokyo/others), educational attainment (university graduate or above/below), and household income level (<5 million yen or ≥5 million yen).
The distribution of the total number of hand hygiene events per day in all participants and participants who claimed to practice hand hygiene under the “loose standards” was clarified using histograms and box plots, respectively. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 26 (IBM Japan, Tokyo, Japan).
Results
Participant enrollment and descriptive statistics
A total of 2400 participants (1200 men; age range: 20 to 79 years) were included in the present study (Table 1 ).
Table 1.
Participant characteristics.
|
N = 2400 |
||
|---|---|---|
| n (%)/mean (SD) | ||
| Sex (men) | 1200 | (50%) |
| Age, years | 49.7 | (16.4) |
| Marital status (married) | 1362 | (56.8%) |
| Living arrangement (with others) | 1886 | (78.6%) |
| Smoking (smokers) | 340 | (14.2%) |
| Self-rated health (good) | 2024 | (84.3%) |
| Past medical history (yes) | ||
| Hypertension | 453 | (18.9%) |
| Diabetes | 135 | (5.6%) |
| Respiratory disease | 104 | (4.3%) |
| Residential area (Tokyo) | 922 | (38.4%) |
| Educational attainment (University graduate or above) | 1258 | (52.4%) |
| Household income level (≥5 million yen) | 1232 | (51.3%) |
| History of seasonal influenza vaccination (received annually) | 666 | (27.8%) |
SD; standard deviation.
Table 2 shows the percentage of participants for each frequency of protective measures against COVID-19 recommended by the WHO (Table 2). The prevalence of participants obtaining information from a reliable source was 38.1%.
Table 2.
The percentage of participants for each frequency of protective measures against COVID-19 recommended by the WHO.
| N | 1. Always n (%) |
2. Sometimes n (%) |
3. Rarely n (%) |
4. Never n (%) |
|
|---|---|---|---|---|---|
| Hand hygiene | 2400 | 1405 (58.5) | 605 (25.2) | 244 (10.2) | 146 (6.1) |
| Social distancing measures#1 | 2400 | 710 (29.6) | 907 (37.8) | 480 (20.0) | 303 (12.6) |
| Avoiding touching eyes, nose and mouth | 2400 | 585 (24.4) | 851 (35.5) | 515 (21.5) | 449 (18.7) |
| Respiratory etiquette | 2400 | 1408 (58.7) | 581 (24.2) | 249 (10.4) | 162 (6.8) |
| N | 1. Definitely can n (%) |
2. Probably can n (%) |
3. Probably can’t n (%) |
4. Definitely can’t n (%) |
|
|---|---|---|---|---|---|
| Self-isolation | 1660#2 | 665 (40.1) | 571 (34.4) | 297 (17.9) | 127 (7.7) |
| N | Yes n (%) |
No n (%) |
|
|---|---|---|---|
| Obtaining information from a reliable source | 2400 | 914 (38.1) | 1486 (61.9) |
#1 Participants were asked about the frequency of avoiding places where many people are gathered together.
#2 Regarding self-isolation, in response to the question “If you have a fever or cold, can you take time off from work?”, the participants selected from one of the items of the 4 point-Likert scale or 5. Not working, and persons who selected 5. (n = 740) were excluded from analysis.
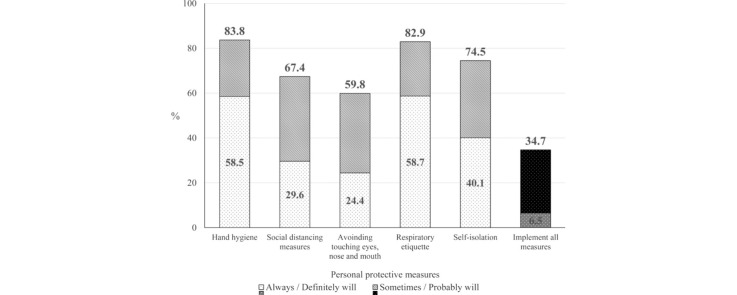
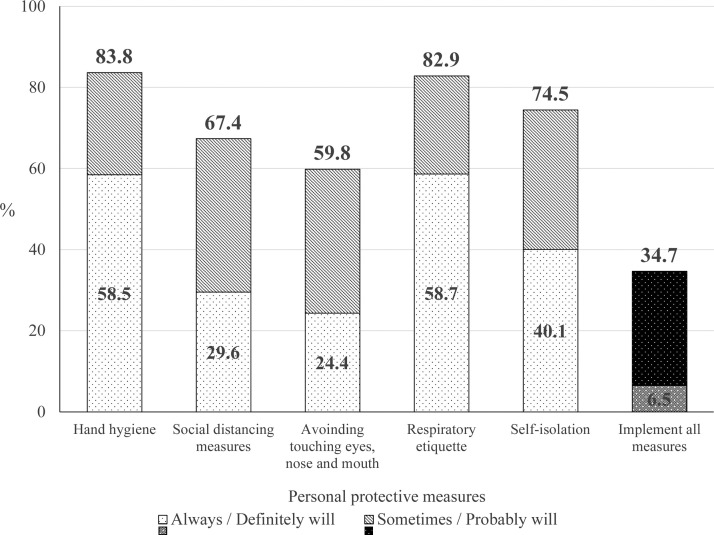
Figure 2 shows the prevalence of personal protective measures against COVID-19 recommended by the WHO, and Figure 3 presents the proportion of participants for each total number of implementing personal protective measures. Based on the loose standards, approximately 80% of participants implemented hand hygiene, respiratory etiquette, and self-isolation. However, 67.4% and 59.8% implemented social distancing measures and avoided touching the eyes, nose, and mouth, respectively. The prevalence of the loose and strict standards of implementation of all personal protective measures was 34.7% and 6.5%, respectively. In stratification by each sociodemographic attribute, the prevalence of implementing all personal protective measures in women, older adults, married, living with other, non-smokers, lower educational attainment, and higher household income level was higher (Supplementary table). According to multivariate logistic regression analysis, women and older adults have a significantly higher odds ratio (OR) than men and persons under 65 years old, respectively (women OR: 1.57. older adults OR: 1.83, Table 3 ).
Figure 2.
The prevalence of personal protective measures against COVID-19 recommended by the WHO.
Figure 3.
The proportion of participants for each total number of implementing personal protective measures.
When the participant replied “Always,” “Sometimes,” or “Definitely can” or “Probably can” (in the case of self-isolation) for each personal preventive measure, it was considered that the personal protective measure was being implemented.
Table 3.
Association between each sociodemographic attribute and implementing all personal measures recommended by the WHO.
| Coefficient | Odds ratio | 95% Confidence Interval | p value | |
|---|---|---|---|---|
| Sex: women | 0.45 | 1.57 | 1.27-1.96 | <0.001 |
| Age: older adults (≥65 years old) | 0.60 | 1.83 | 1.35–2.47 | <0.001 |
| Marital status: married | 0.23 | 1.26 | 0.98–1.63 | 0.074 |
| Living arrangement: with other | 0.23 | 1.25 | 0.90–1.73 | 0.181 |
| Smoking: smoker | −0.09 | 0.91 | 0.68–1.23 | 0.545 |
| Residential area: Tokyo | 0.02 | 1.02 | 0.82–1.27 | 0.847 |
| Educational attainment: university graduate or above | −0.16 | 0.86 | 0.68–1.07 | 0.171 |
| Household income: ≥5 million yen | 0.11 | 1.12 | 0.88–1.42 | 0.374 |
When the participant replied “Always,” “Sometimes,” or “Definitely can” or “Probably can” (in the case of self-isolation) for all personal preventive measure recommended by the WHO, it was considered that the personal implemented all personal protective measures (under the loose standards).
Multivariate logistic regression analysis was performed. The dependent variable was implementing all personal protective measures under the loose standards, and the independent variables were sex, age (older adults (≥65 years old)/persons under 65 years old), marital status (not married/married), living arrangement (with others/alone), smoking status (smokers/non-smokers), residential area (Tokyo/others), educational attainment (university graduate or above/not), and household income level (<5 million yen or ≥5 million yen).
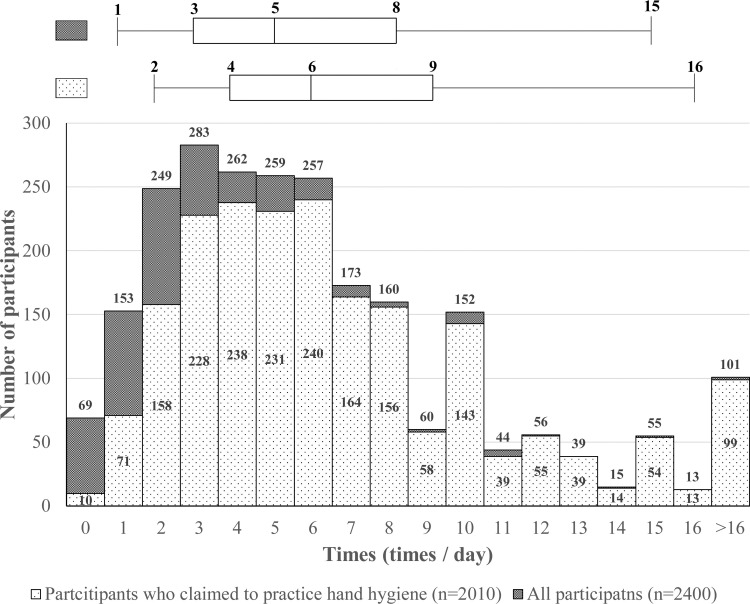
Figure 4 shows a histogram and box plot of the total number of hand hygiene per day. The median number of hand hygiene events per day in all participants and participants who claimed to practice hand hygiene under the loose standards was 5 times/day (25th percentile, 75th percentile: 3 times/day, 8 times/day), and 6 times/day (25th percentile, 75th percentile: 4 times/day, 9 times/day), respectively.
Figure 4.
Histogram and box plot of the total number of hand hygiene events per day.
When the participant replied “Always,” “Sometimes,” for hand hygiene, it was defined that they claimed to practice hand hygiene (under the loose standards)./Box-whisker plot indicates median line, quartile box, and whiskers at 5th and 95th percentile.
Discussion
We set out to determine the implementation status of personal protective measures by ordinary citizens in Japan during the early phase of COVID-19 outbreak. The prevalence of each personal protective measure recommended by WHO was approximately 60–85%. Only 34.7% of participants implemented all measures under the loose standards, and when the strict standards were applied, the prevalence was further reduced to only 6.5%. The prevalence of those in men and persons under 65 years old was lower in women and older adults, respectively. It is difficult to estimate if the prevalence reported in this study is high or low by international comparisons, but this study revealed that there is room for improvement in personal protective measures among ordinary citizens, especially men and persons under 65 years old, in Japan.
Of the five personal protective measures recommended by the WHO, the prevalence of social distancing measures and avoiding touching the eyes, nose, and mouth were particularly low, although the prevalence of personal protective measures in this study was generally higher than those reported in the United Kingdom between March 17 and March 18 (Atchison et al., 2020). The two personal protective measures may still leave much to be desired in Japan.
During the early phase of the COVID-19 outbreak, the interest of people with regards to personal protective measures had been focused on wearing face masks, and it triggered soaring demand, panic buying, hoarding and misuse of face masks (WHO, 2020f). The demand for face masks was up to 100 times higher than normal and prices were up to 20 times higher (WHO, 2020g). In contrast, the WHO states that wearing medical masks may create a false sense of security, leading to the neglect of other essential preventive measures (WHO, 2020e). Personal protective measures should ideally be combined with other approaches, as individual measures may not be so effective when implemented alone (European Centre for Disease Prevention and Control, 2020, Lee et al., 2009). It may be unclear to what extent the preventive effects differ depending on the frequency and type of preventive action and the number of actions taken but increasing the frequency and type of action may be effective in stopping the spread of COVID-19.
This study was a self-reported evaluation, and it is possible that social desirability bias may have led to an overestimation of the implementation status (Paulhus, 1984) and that methods of implementation of personal protective measures may be incorrect. For example, the prevalence of hand hygiene implementation among the participants in this study was 83.8% under the loose standards and 58.5% under the strict standards. However, the median daily hand hygiene events implemented by participants who claimed to practice hand hygiene under loose standards were 6 times/day. The WHO has not recommended a specific number of times a day that hand hygiene should be practiced, but the U.S. Centers for Disease Control and Prevention recommends implementation after going to the bathroom, before eating, and after blowing your nose, coughing, or sneezing (US CDC, 2020). In general, the average person eats meals and uses the toilet multiple times per day, so hand hygiene performed 6 times/day is unlikely to be sufficient. When advocating for public awareness of personal protective measures, it may also be important to communicate specific ways of implementing preventive actions. The Japanese government provides detailed explanations on personal protective measures on its website (JMHLW, 2020a), but the percentage of respondents of people obtaining information from a reliable source was only 38.1%. It is therefore essential that the government conduct further educational campaigns targeting ordinary citizens, especially men and persons under 65 years old.
There are some limitations that should be considered in our study. The most important point is the fact that in this study, participants were recruited from people enrolled in a single internet research company, and the results may have been affected by selection bias. Relatively little is known about the characteristics of people in online communities (Wright, 2017). Furthermore, the age and sex demographics of the participants in this study were different from that of the Japanese population (Statistics Bureau of Japan, 2019). Additionally, this survey was conducted during the early phase of the COVID-19 outbreak. Thus, the prevalence of personal protective measures may change with time. Finally, the results may only be directly applied to Japanese populations. In the case of other populations with different cultural, ethnic, and geographical backgrounds, the prevalence of the personal protective measures may be very different compared with those reported in the present survey. Despite these limitations, to the best of our knowledge, this is the first study to clarify the implementation status of personal protective measures by ordinary citizens during the early phase of COVID-19 outbreak in Japan.
In conclusion, the prevalence of the five personal protective measures recommended by the WHO was approximately 60–85%, and only 34.7% of ordinary citizens in Japan implemented all measures during the early phase of COVID-19 outbreak. Further educational campaigns on the implementation of personal protective measures of WHO and the government are required.
Founding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study was approved by the Ethics Committee of Tokyo Medical University, Tokyo, Japan (No: T2019-0234). Informed consent was obtained from all respondents.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgement
We express our sincere thanks to all the participants who enrolled in this study.
Footnotes
Supplementary material related to this article can be found, in the online version, at https://doi.org/10.1016/j.ijid.2020.04.014.
Appendix A. Supplementary data
The following are supplementary data to this article:
References
- Atchison C., Bowman L., Eaton J.W., Imai N., Redd R., Pristera P. 2020. Public Response to UK Government Recommendations on COVID-19: Population Survey, 17–18 March 2020. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-Population-Survey-20-03-2020.pdf (accessed 22.03.20) [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC) 2020. Guidelines for the use of non-pharmaceutical measures to delay and mitigate the impact of 2019-nCoV. https://www.ecdc.europa.eu/en/publications-data/guidelines-use-non-pharmaceutical-measures-delay-and-mitigate-impact-2019-ncov (accessed 22.03.20) [Google Scholar]
- Japanese Ministry of Health, Labor and Welfare (JMHLW) 2020. About coronavirus disease 2019 (COVID-19) https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/newpage_00032.html (accessed 22.03.20) [Google Scholar]
- Japanese Ministry of Health, Labor and Welfare (JMHLW) 2020. Basic policy on prevention of new coronavirus infection. https://www.mhlw.go.jp/content/10900000/000599698.pdf (accessed 22.03.20) (Only Japanese) [Google Scholar]
- Lee V.J., Lye D.C., Wilder-Smith A. Combination strategies for pandemic influenza response – a systematic review of mathematical modeling studies. BMC Med. 2009;7:76. doi: 10.1186/1741-7015-7-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulhus D.L. Two-component models of socially desirable responding. J Pers Soc Psychol. 1984;46(3):598–609. [Google Scholar]
- Qualls N., Levitt A., Kanade N., Wright-Jegede N., Dopson S., Biggerstaff M. Community mitigation guidelines to prevent pandemic influenza – United States, 2017. MMWR Recomm Rep. 2017;66(1):1–34. doi: 10.15585/mmwr.rr6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Bureau of Japan . 2019. 2015 population census. https://www.e-stat.go.jp/en/stat-search/files?page=1&toukei=00200521&tstat=000001080615 (accessed 22.03.20) [Google Scholar]
- US Centers for Disease Control and Prevention (U.S.CDC) 2020. How to protect yourself. https://www.cdc.gov/coronavirus/2019-ncov/about/prevention-treatment.html (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. Basic protective measures against the new coronavirus. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. Novel Coronavirus (2019-nCoV) SITUATION REPORT – 1 21 JANUARY 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4 (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19) https://apps.who.int/iris/handle/10665/331498 (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. Shortage of personal protective equipment endangering health workers worldwide. https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed 22.03.20) [Google Scholar]
- World Health Organization (WHO) 2020. WHO emergencies press conference on novel coronavirus – 7 February. https://www.who.int/docs/default-source/coronaviruse/transcripts/transcript-coronavirus-press-conference-full-07feb2020-final.pdf?sfvrsn=3beba1c0_2 (accessed 22.03.20) [Google Scholar]
- Wright K.B. Researching internet-based populations: advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. J Comput-Mediat Commun. 2017;10(3) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.