Highlights
-
•
Thailand reported the first imported case of COVID-19 outside of China
-
•
Events requiring an international response from Thailand were compiled
-
•
Thailand's ability to communicate with international stakeholders was evaluated
-
•
Duration of response times were rapid during the early phase of the emergency
-
•
There is a need to nominate official English-speaking spokespeople
Keywords: COVID-19, Thailand, International communication, Mechanisms
Abstract
Objectives
This study aimed to assess the Thailand Department of Disease Control's (DDC) early responses to COVID-19 in respect to communication with the international community and to identify the manner of Thailand's response during public health emergencies.
Methods
Documents and international response communication from 4–31 January 2020 were reviewed and dates of responses were collected for descriptive analysis. A questionnaire was submitted to the DDC officers responsible for international coordination. A meeting to identify responses was held to evaluate the self-assessed capacities of the Department's international communication.
Results
Thailand began the COVID-19 screening protocol on 3 January 2020. International correspondence subsequently occurred continually either through the ASEAN or International Health Regulations (IHR) mechanisms. The total score of communication for international response was 88.9%. For IHR reporting duties, the median duration to respond was 2.49 hours. Official news was sent within a mean of 9.18 hours and the English daily situation reports were always uploaded onto the official website within 24 hours.
Conclusions
This study provided a benchmark for international coordination and communication capacities and also identified areas for improvement during public health emergencies, such as the need to identify English-speaking spokespeople to communicate at an international level.
1. Introduction
On 31 December 2019, the World Health Organization (WHO) China Country Office reported a cluster of pneumonia cases of an unknown cause, which was first identified in Wuhan City, Hubei Province, China (WHO, 2020a). Most cases had links to Wuhan's Huanan Seafood Wholesale Market and presented with symptoms such as fever, dry cough, dyspnea, difficulty breathing in a few cases, and chest radiograph findings of bilateral pulmonary infiltrates (WHO, 2020b). The market was suspected to be the origin of the outbreak and was shut down on 1 January 2020 (Xinhuanet, 2020a). After the Chinese Center for Disease Control and Prevention (CCDC) identified the infectious agent as a new type of coronavirus–which the WHO subsequently referred to as COVID-19 on 11 February 2020 (WHO, 2020c)–China shared the genetic sequence of the novel coronavirus that causes COVID-19 on 12 January 2020 (WHO, 2020d). On 11 January 2020, China reported the first COVID-19 death (Bangkok Post, 2020a). On 13 January 2020, the Ministry of Public Health (MOPH) Thailand reported the first imported case of COVID-19 from Wuhan, which was also the first case outside China (Emergency Operation Center, 2020). China decided to temporarily lock down its public transport and railway stations, including outbound passengers to cut-off the virus spread beyond Wuhan (Xinhuanet, 2020b).
On 30 January 2020, the WHO declared that the outbreak of COVID-19 constituted a Public Health Emergency of International Concern (PHEIC) due to the significant increase in the number of COVID-19 cases, new countries reporting confirmed cases (WHO, 2020e), and to reduce the potential damage it could cause in countries with public health systems that have less capacity. As of 4 February 2020, there were 20,595 confirmed cases globally in 24 countries, including 426 deaths (ASEAN Biodiaspora Virtual Center, 2020). On 5 January, the WHO issued a statement that did not recommend applying any restrictions of travel or trade on China, based on available information and the currently known situation (Pharmaceutical-Technology, 2020).
As COVID-19 emerged and spread, world powers strengthened their resolve to contain the outbreak. In January 2019, the Thailand Department of Disease Control (DDC), the ASEAN Health Cluster and the WHO took measures to coordinate efforts to stop the outbreak and prevent its further spread. International coordination activities can play a major role in the response to disease outbreak and include collecting and sharing information with international and regional organizations, providing documents prepared for public dissemination, and issuing press release documents produced via the coordination mechanisms. Within the larger response, there were two primary units operating to fulfill the departmental assignments: the Office of International Cooperation (OIC) and the Division of Epidemiology (DOE) served as the units for supporting international cooperation in disease prevention and control, coordinating with relevant national and international agencies, and was responsible for serving as the position of liaison officer of international response at the Emergency Operations Center (EOC) of the Department of Disease Control (DDC). In early response efforts for aspects of international coordination, the OIC and the DOE of the DDC conducted a cross-sectional study to assess capacities of communication with the international community, including timely dissemination of information and products of communication, media liaison documents such as drafting talking points, Q&A and press releases, responding to media queries, and media monitoring that encompassed all key stakeholders and concerned parties such as international agencies, embassies and ministries of other countries, and, importantly, the general public.
To ensure effective communication and coordination of the DDC, this study aimed to provide an assessment of the DDC response, highlighting international communication, and to provide recommendations for the continued international response and future public health emergencies.
2. Methods
Documents were reviewed, including: formal and informal communications of official letters and messages addressing COVID-19 between the DDC's sectors (including the international cooperation sector, the international health regulation sector and the incident commander from the EOC) the WHO and ASEAN Secretariat from 4–31 January 2020. Types of responses, dates of notifications (with specific times) and dates of responses (with specific times) were recorded to explore the timeliness of communication. The frequency and duration between assignments (appointed by the EOC to the liaison officers of international response) and release times in minutes and hours to relevant international and regional organizations for assignments–such as duties of the IHR national focal point, press releases in English, daily situation reports in English, and other risk communications–were analyzed.
A structured questionnaire was derived from a session on communication of the WHO checklist for influenza pandemic preparedness planning (WHO, 2005a) and was implemented to DDC officers who were responsible for tasks of international coordination. The questionnaire contained nine questions about the capacities of communication, with a focus on international responses. All questions were focused on the exchange of information with international organizations, an overview of all available information posted for the public, and the designation of spokespersons at an international level. A meeting among the designated officers from the international cooperation sector, the international health regulation sector, and the incident commander from the EOC was held to identify a consensus in the responses to the questionnaire checklist. The initial responses from 4–31 January 2020 were discussed among the officers. A full score of 1 was awarded per question if there was any evidence of the official documents such as a formal letter, an electronic formal letter or minutes from formal meetings. A score of 0.5 was given if there was unofficial documented evidence including an email, video conference or minutes from informal meetings. A score of 0 meant there was a lack of responses or incomplete capacities. Data management and all analyses were performed using Epi Info version 7.2.2.2. Scoring of the capacities of communication was treated as a continuous variable. The duration between assignment and release times, in minutes and hours, for activities of international responses were analyzed. A descriptive analysis was used to describe the data.
3. Results
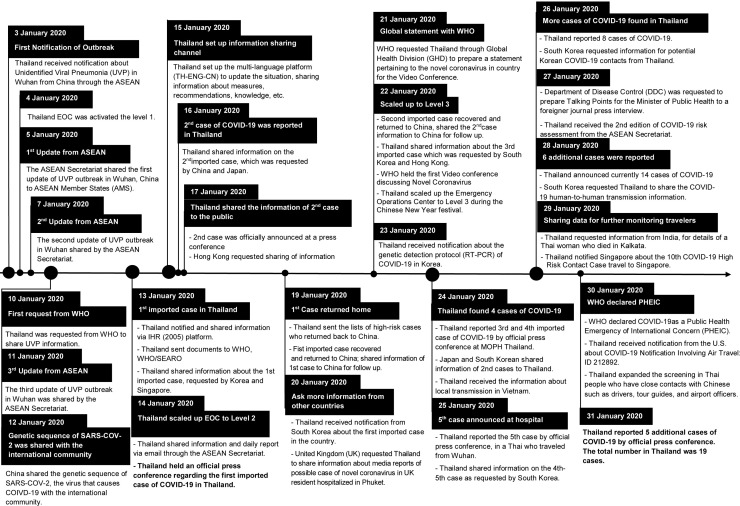
From the initial meeting among the DDC officers, key events were compiled into a timeline (Fig. 1 ) and described as follows. Thailand began screening passengers by checking their temperatures upon arrival from Wuhan starting on 3 January 2020 onwards at the Suvarnabhumi, Don Mueang, Phuket, and Chiang Mai international airports. On 13 January 2020, MOPH Thailand reported the first imported case of laboratory confirmed COVID-19 from Wuhan. The case was a 61-year-old Chinese woman living in Wuhan City (Emergency Operation Center, 2020). On 22 January 2020, MOPH expanded its surveillance procedures by implementing the highest level of precautionary measures and by scaling up the EOC in response to the surge of inbound Chinese tourists expected to arrive during the Chinese New Year Festival celebration (Emergency Operation Center, 2020). On 23 January 2020, the first Thai citizen was confirmed with COVID-19: a 73-year-old woman with travel history to Wuhan (Bangkok Post, 2020b). At the same time, China locked down Wuhan and suspended all public transportation, including city buses, the subway system, ferries, and long-distance passenger transportation (ALJAZEERA, 2020). On 30 January 2020, Thailand increased the screening protocol among workers in the tourist sector–such as tour guides, hotel staff, taxi drivers, and airport staff–who were in frequent contact with foreign tourists, especially Chinese tourists (Reuters, 2020). The MOPH conducted a meeting on the National Committee for Emerging Infectious Disease Preparedness, Prevention and Response on 30 January 2020 (Bangkok Post, 2020d). On 31 January 2020, Thailand reported its first local case of human-to-human transmission of COVID-19 in a Thai taxi driver within the country (Bangkok Post, 2020c). Further formal and informal communications among Thailand MOPH, the WHO, ASEAN Secretariat, and other countries addressing the issue of COVID-19 are shown in Fig. 1.
Fig. 1.
The international response regarding the novel coronavirus 2019 in Thailand.
The total score from the self-assessment of international response communication during the COVID-19 situation was 88.9%. Full scores were found in producing communication channels such as the development of an English website, and distribution of general information and media briefings with knowledge to various target groups including the general public and foreigners in the country. Mechanisms for timely information sharing to international authorities such as the WHO, the ASEAN Secretariat, and effectively sharing website content with other countries through the existing mechanism of the ASEAN Secretariat were assessed with full scores as well. When designating professional specialists to produce timely messages during an epidemic and nominating officially assigned epidemic spokespersons at international levels had not been implemented, they did not receive full scores (Table 1 ).
Table 1.
Capacities of communication as an international response during a situation of COVID-19 cases in Thailand.
| No. | Capacities of communication | Self-assessment scores |
|---|---|---|
| 1 | Develop an official (English) national website | 1 |
| 2 | Link this website to other countries | 1 |
| 3 | Have good relations with professional specialists able to help with the development of accurate and timely messages | 0.5 |
| 4 | During the epidemic period, develop fact sheets or other general information on pandemic preparedness for distribution to various target groups, including professional and community groups | 1 |
| 5 | Nominate epidemic spokespersons at an international level | 0.5 |
| 6 | Ensure that media briefings are held regularly during events | 1 |
| 7 | Ensure that materials are regularly reviewed and updated with new (relevant) knowledge that may become available during an epidemic | 1 |
| 8 | Ensure that mechanisms exist for information sharing between national authorities, WHO and other United Nations agencies. Coordinate with, or use, existing mechanisms for the implementation of the IHR | 1 |
| 9 | Ensure that a mechanism exists for the timely and consistent distribution of information between national bodies and international authorities | 1 |
| Total score (%) | 8 (88.9%) |
According to Article 6 of IHR (2005) (WHO, 2016): Notification (Each State Party shall assess events occurring within its territory by using the decision instrument. Each State Party shall notify WHO, by the most efficient means of communication available, by way of the National IHR Focal Point, and within 24 hours of assessment of public health information, of all events which may constitute a public health emergency of international concern within its territory in accordance with the decision instrument, as well as any health measure implemented in response to those events), the Thai National IHR Focal Point notified the Thailand WHO country office within 30 minutes after receiving laboratory confirmation of the first case of COVID-19 in Thailand. The Thailand IHR National Focal Point sent the epidemiological, clinical and laboratory information of the first imported COVID-19 case to the WHO and China IHR National Focal Point via official letter and email. This immediate response was followed with a recommendation from the Thailand National IHR Committee that assigned the Thailand IHR National Focal Point to include COVID-19 in the standard operating procedures for reporting all dangerous communicable diseases under the Communicable Diseases Act, B.E. 2558 (2015) and public health emergencies of international concern (PHEIC) in Annex II of IHR 2005. The standard operating procedures for dangerous communicable diseases were previously made effective on 19 December 2019.
There were 11 tasks of the Thai National IHR Focal Point to respond to relevant stakeholders regarding Article 44 of IHR (2005) (WHO, 2016): Collaboration and assistance (States Parties shall undertake to collaborate with each other, to the extent possible, in: (a) the detection and assessment of, and response to, events as provided under these regulations; (b) the provision or facilitation of technical cooperation and logistical support, particularly in the development, strengthening and maintenance of the public health capacities required under these regulations). Minimum and maximum response times ranged from 0.37 (22.2 minutes) to 43.40 hours. The median duration was 2.49 hours. The Thai National IHR Focal point maintained communication with the Thailand-WHO Country Office and WHO South-East Asia (SEARO) on the case reporting procedure. Regarding an email message from WHO-SEARO dated 29 January 2020 requesting the Thailand MOPH to report cases through a three-page interim case reporting form for COVID-19, the Thai National IHR Focal point was prompted to submit all case reports online after receiving the password from WHO-SEARO for the SEA COVID-19 case reporting application on 24 February 2020.
Short messages to distribute knowledge to the general public–through flyers, health beware cards provided to travelers upon arrival in Thailand, infographics created in different languages to the target groups, and social media posts in different languages posted onto the official website of the Department of Disease Control–were effectively circulated to the target groups within a short period of time (mean 3.4 hours). A total of 15 press releases and official news correspondence took longer to release, with a mean of 9.18 hours. A total of 17 English daily situation reports were produced and uploaded onto the official website of the Department of Disease Control, with a mean of time of 13.55 hours and always within 24 hours between 4–31 January 2020 (Table 2 ).
Table 2.
Timeliness of communication as an international response during the reporting of COVID-19 cases in Thailand, 2019.
| No. | Categories | Frequency | Duration between assignment times and release time (hrs.) (Minimum - Maximum) | Mean (Median) duration (hrs.) ± Standard Deviations |
|---|---|---|---|---|
| 1 | Duties of International Health Regulation (IHR) focal point | |||
| on article 6 (Notification) | 1 | 0.50 | ||
| on article 44 (Collaboration and assistance) | 11 | 0.37-43.40 | 13.41 ± 18.82 2.49 (Median) | |
| 2 | Press release/News | 15 | 4.56-12.97 | 9.18 ±6.19 |
| 3 | Daily situation report | 17 | 3.93-23.03 | 13.55 ±6.81 |
| 4 | Risk communication (knowledge) | 9 | 2.67 - 4.18 | 3.43 ±1.07 |
4. Discussion
The emergence of COVID-19 has become the most concerning global health issue and has required the immediate attention of medical and public health personnel to respond. Effective and timely communication is one of four essential components that a response team must have mastered to effectively handle a routine or crisis emergency (Everbridge, 2017). This assessment was conducted to ensure that the international response of the DDC was comprehensive and that the DDC had made a concerted effort to achieve effective communication and coordination.
According to Fig. 1, Thailand abided by the ASEAN Health Mechanism, especially the ASEAN Emergency Operation Center Network (ASEAN EOC) under ASEAN Health Cluster 2, which is the health collaboration among ASEAN member states focusing on responding to all hazards and emerging threats, and ensuring a high level of capacity to detect, investigate, contain and manage outbreaks of emerging and re-emerging infectious diseases, neglected tropical diseases, including strengthening laboratory capacities and disaster health management. This network is led by Malaysia and is one of the crucial projects in the endorsed ASEAN Health Cluster 2 Work Program (ASEAN Health Cluster 2 Work Programme for 2016 to 2020), which offers a channel for ASEAN countries to coordinate, share information and knowledge to cope with public health threats occurring in the region. In the early phase of COVID-19, Thailand first received notification of this emerging public health threat through ASEAN EOC Network and this warned Thailand to prepare its readiness and disease control measures to fight against this outbreak. The daily updated situation was shared by ASEAN Member States via email loop and video conferences. Therefore, the efficiency of the ASEAN EOC Network allowed it to serve as a beneficial tool for coping with the emergence of COVID-19.
Exchange of information on the COVID-19 situation and its coordination was organized through the ASEAN Health Mechanism that Thailand has closely cooperated with via the Ministries of Foreign Affairs. Furthermore, all embassies located in Thailand and their missions outside the countries were provided with related information through the ASEAN Health Mechanism platform, including updated situations, documentation of guidelines and best practices. The DDC organized and joined a wide range of face-to-face meetings, including a video conference with the Ministry of Foreign Affairs, international partners and embassies to bridge coordination of the gaps in disease control measures during the pandemic. Questions from the embassies were usually sent to the DDC through contacts at the Ministry of Foreign Affairs via official letters. If the request was urgent, the embassies directly contacted the DDC liaison officers by email.
Across divisions of the DDC, the surveyed officers received full scores (Table 1) on most questions for their ability to produce documented evidence confirming accomplishment of each communication capacity. These results display Thailand's commitment to communication with international partners (managing websites, developing materials, holding press conferences, effectively utilizing existing mechanisms) as well as the efficient systems among the individuals to access and produce official documents. The full scores for ensuring the existence of mechanisms for timely information sharing are a reflection of Thailand's familiarity with the relevant international partners, ability to navigate these mechanisms and ability to adhere to IHR. The results were related to a study by Anema et al. (Anema et al., 2012). From the study, it indicated that 95% of appointed National Focal Points of IHR (2005) Annex 2 were always/usually useful in outlining decision-making criteria for facilitating decisions regarding the ability to send notifications of potential PHEICs. In respect to communication time (Table 2), specifically duration between assignment and release times, it was evident that the DDC values rapid communication and dissemination of information. The short amount of time to report to the WHO country office under Article 6 and the median time under Article 44 are reflections of the importance of having a competent National IHR Focal Point. The Thai National IHR Focal Point explained that the extended time duration of response for some assignments (e.g. the maximum duration for one assignment was 43.40 hours) was due to the fact that some responses involved multiple stakeholders to make a final decision, leading to time-consuming delays. To assess Thailand's capacity to perform duties of the IHR Focal Point, future assessments should be conducted to evaluate the IHR reporting capacities, as determined under Thailand's SOP.
However, there were two areas (Table 1) that did not receive full scores, which were “Nominate epidemic spokesperson at international level” and “Have good relations with professional specialists able to help with the development of accurate and timely messages.” In communication strategies, spokespersons have to be identified to address crisis management and risk communication plans (U.S. Department of Health and Human Services, 2014). During the initial response of the epidemic of COVID-19 in Thailand, the designated spokespersons gave interviews and press releases following the communication plan. When the outbreak was determined to be a PHEIC, the English-speaking spokespersons to communicate at an international level had not been clearly identified. This result identified a gap in international communication that the DDC needs to define an international spokesperson to connect and share information with regional and international organizations. It is essential to stay on top of the information flow and to maintain close coordination with other agencies with spokespersons. All responses require approval from the Incident Commander before release at an international level so all information may slow in a bottleneck. The technical advisory groups should be identified in advance for international responses and be attached to the incident command structure (WHO, 12).
The ability to produce press releases, daily situation reports and risk communication information and release all of them to the public within 24 hours assures that the DDC values its English-speaking partners, residents and tourists. Press releases and news were required to be in an official format and needed approval from the incident commander before release; thus, this took longer, as seen in the mean of 9.18 hours (Table 2). The large standard deviations suggest that some documents took longer to produce and may have been attributed to an available, yet limited, English writing capacity and the time the approval process took.
The overall rapid response and communication capacities exhibited by the DDC in this assessment express the commitment to transparency, sharing information from trusted sources before fake news sources create misinformation, and willingness to collaborate with a variety of international partners for the benefit of global health. This assessment was not without shortcomings. The quality of information was not measured, response times were self-reported and the study was not conducted by a neutral third party. To reduce the potential for bias from overestimating capacities of communication scores during the self-assessment, specific criteria requiring documents as evidence were defined for each score (0, 0.5 and 1). Therefore, scores in this capacity were dependent on official documents rather than human judgment. There was no departmental motivation or personal gain resulting from the overestimation of scores. The only benefits included complying with IHR and timeously informing relevant partners. This study allowed the Department to establish baseline data; therefore, being objective in scoring was beneficial to set realistic benchmark targets for future assessments. Furthermore, the cross-sectional nature was unable to monitor changes over time in how the Department's response has been amended. Although the assessment aimed to show communication efficiency, this is not to be confused with overall efficiency. While additional resources and personnel were shifted towards urgent situations, this study did not measure the assumed loss in efficiency in other areas from which the surge capacity resources were drawn.
With health, social, economic and political implications brought upon the by the emergence of COVID-19, this assessment serves as a baseline to measure the DDC's existing capacities and execution of tasks, with the aims of guaranteeing speed and accuracy in communication with international partners and the public during emergencies and urgent situations.
Conflict of Interest
The authors declare no conflict of interest.
Funding Source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical Approval
The study has not been reviewed or approved by a human research ethics committee because the data are reported in counts and percentages and the participants cannot be identified from the results.
Acknowledgments
The authors would like to thank colleagues (Office of International Cooperation and Division of Epidemiology, Ministry of Public Health) for their help to provide data. Thank you for Thailand MOPH and US CDC Collaboration, and a project of DGHP-iEOC (Capacity and workforce development to strengthen preparedness and emergency response operations across Thailand, Cambodia, Laos PDR, and Malaysia) for support and assistance with the publication. Thank you for Dr. Sombat Thanprasertsuk, and Dr. Darika Kingnate from the Department of Disease Control for support and advice.
References
- ALJAZEERA. No exit: China locks down second city as it steps up virus battle. Available at: https://www.aljazeera.com/news/2020/01/wuhan-sealed-china-steps-battle-deadly-virus-200122234630666.html [accessed 10 Feb 2020].
- Anema Descriptive review and evaluation of the functioning of the International Health Regulations (IHR) Annex 2. Globalization Health. 2012;8:1. doi: 10.1186/1744-8603-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASEAN Biodiaspora Virtual Center (ABVC) in collaboration with Bluedot Inc. Risk Assessment for International Dissemination of 2019-nCoV to the ASEAN Region. https://ddc.moph.go.th/viralpneumonia/file/RiskAssessment/EngVers_240163.pdf [accessed 10 January 2020].
- ASEAN Health Cluster 2 Work Programme for 2016 to 2020. https://asean.org/storage/2017/11/ASEAN-Health-Cluster-2-Work-Programme_FINAL-ENDORSED.pdf [accessed 10 February 2020].
- World Health Organization. Novel Coronavirus (2019-nCoV) SITUATION REPORT No. 1. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf [accessed 10 February 2020].
- WHO. Emergencies preparedness, response. Pneumonia of unknown origin–China. Disease outbreak news: Update 12 January. Available at: https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ [accessed 10 February 2020].
- Xinhuanet. Wuhan seafood market may not be only source of novel coronavirus: expert. Available at: http://www.xinhuanet.com/english/2020-01/29/c_138741063.htm [accessed 10 February 2020].
- World Health Organization. Novel Coronavirus (2019-nCoV) SITUATION REPORT No. 22. 2020. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf [accessed 13 February 2020].
- WHO. Emergencies preparedness, response. Pneumonia of unknown origin–China. Disease outbreak news. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ [accessed 10 February 2020].
- Bangkok Post. China reports first death from mystery virus. Available at: https://www.bangkokpost.com/world/1833374/china-reports-first-death-from-mystery-virus [accessed 10 February 2020].
- BANGKOK(NNT). Health Minister proposes Visa on Arrival suspension for Chinese. Available at: http://thainews.prd.go.th/en/news/detail/TCATG200130183734028 [accessed 10 February 2020].
- Bangkok Post. Human transmission of coronavirus confirmed in Thailand. Available at: https://www.bangkokpost.com/thailand/general/1847884/human-transmission-of-coronavirus-confirmed-in-thailand [accessed 10 February 2020].
- Bangkok Post. First Thai infected with coronavirus. Available at: https://www.bangkokpost.com/learning/easy/1841869/first-thai-infected-with-coronavirus [accessed 10 February 2020].
- Emergency Operation Center, Department of Disease Control. MOPH emphasizes no outbreak of Novel Coronavirus in Thailand, ensuring Thailand's preventive measures for emerging disease, early detection, early treatment. Press Release. https://ddc.moph.go.th/viralpneumonia/eng/file/news/news_no1_130163.pdf [accessed 10 January 2020].
- Everbridge. 4 Key Elements of Effective Crisis Management. 2017. [accessed 10 February 2020].
- Pharmaceutical Technology. Coronavirus: A timeline of how the deadly outbreak is evolving. Available at: https://www.pharmaceutical-technology.com/news/coronavirus-a-timeline-of-how-the-deadly-outbreak-evolved/ [accessed 12 February 2020].
- Reuters. Thailand to screen tour guides for coronavirus. Available at: https://www.reuters.com/article/us-china-health-tourism-thailand/thailand-to-screen-tour-guides-for-coronavirus-idINKBN1ZS0Z8 [accessed 10 February 2020].
- U.S. Department of Health and Human Services. CERC: Crisis Communication Plans 2014.
- World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [accessed 10 February 2020].
- World Health Organization. WHO checklist for influenza pandemic preparedness planning. 2005. [accessed 10 February 2020].
- WHO. International health regulations (2005). 3rd ed. Geneva, Switzerland: World Health Organization; 2016.
- WHO. International health regulations (2005): a guide for public health emergency contingency planning at designated points of entry 2012. Geneva: World Health Organization; 2005.
- Xinhuanet. In unprecedented move, China locks down megacity to curb virus spread. Available at:http://www.xinhuanet.com/english/2020-01/23/c_138729430.htm [accessed 10 February 2020].