Dear Editor,
Though no specific urologic manifestations of COVID-19 are recognized, it is important that urologists be aware of potential asymptomatic infection in patients presenting with urologic pathology.
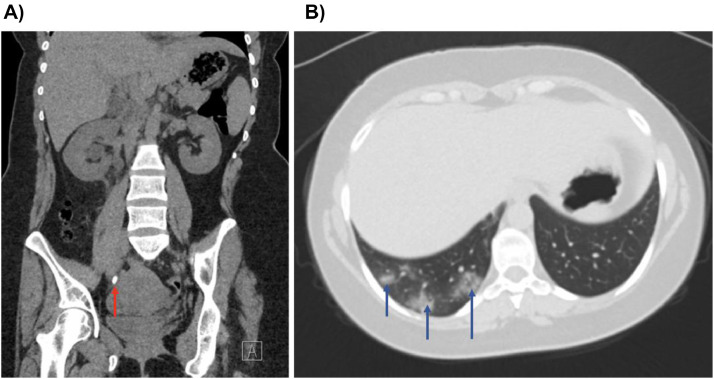
A 31-year old lady with a history of cystinuria presented to a UK hospital with isolated right loin pain. No respiratory symptoms, fever, or signs of sepsis were noted. She was assessed as a nonsuspected COVID-19 case and a noncontrast CT kidney, ureter, bladder (KUB) was arranged. The CT identified a distal 10 × 6 mm right ureteric stone causing hydronephrosis (Fig. 1 A). At the base of her right lung, numerous foci of ground-glass appearances were noted, suggestive of COVID-19 (Fig. 1B). She was isolated on a COVID-19 ward and a ureteric stent was inserted under spinal anesthesia the following day with full personal protective equipment (PPE). Ureteroscopy and stone fragmentation was not undertaken to reduce operative time, whilst spinal anesthesia avoided the need for ventilation with its attendant risks of respiratory compromise and aerosol generation. She was discharged the same evening with a plan for definitive stone surgery in several weeks' time. A subsequent nasopharyngeal swab test was positive for COVID-19 and she was instructed to self-isolate.
Figure 1.
CT images of (A) right distal ureteric stone (red arrow); (B) ground-glass appearance in right lung base (blue arrows). (Color version is available online.)
Although, common symptoms of COVID-19 include fever and dry cough, positive cases can be asymptomatic. Analysis of 112 positive cases from the “Diamond Princess” cruise ship revealed that 73% were asymptomatic, of whom 54% had lung opacities on CT.1 PPE protocols vary widely, with some centers restricting PPE to those approaching suspected or confirmed cases only. Since COVID-19 may not give rise to respiratory symptoms or fever, a strong argument can be made that all those attending the emergency department or acute assessment units with other presenting complaints be assessed as “possible” cases until proven otherwise.
A proportion of asymptomatic COVID-19 patients are identified through investigation for other presenting complaints. A noncontrast CT KUB to investigate suspected ureteric colic will usually include the lung bases. In most situations, scan images are available prior to a radiologist report and clinical decision making is based upon self-reporting by urologists. It is therefore imperative that urologists pay close attention to ground-glass changes in the lung bases when interpreting a CT KUB to identify signs of COVID-19.
Non-steroidal anti-inflammatory steroids (NSAID) increase renal angiotensin-converting enzyme 2 receptors which are bound by severe acute respiratory syndrome-CoV-2, and are hypothesized to increase the risk of developing severe COVID-19.2 , 3 However, there is no convincing evidence that NSAIDs can worsen or increase the risk of COVID-19, and the WHO do not recommend against the use of NSAIDs of ureteric colic.4
Recent evidence suggests a high rate of postoperative mortality in COVID-19 patients undergoing surgery. In a study of 34 patients, postoperative intensive care admission was 44.1% and mortality rate was 20.5%. This was related to postoperative acute respiratory distress syndrome in 60.0%.5 This emphasizes the need for timely recognition of asymptomatic COVID-19 patients presenting with other pathology, so that as in presented case, surgical and aesthetic approaches can be modified to mitigate risk to patients and the healthcare team.
Conflict of interest
None.
References
- 1.Inui S, Fujikawa A, Jitsu M. Chest CT findings in cases from the Cruise Ship “Diamond Princess” with coronavirus disease 2019 (COVID-19) Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020:1–8. doi: 10.1007/s11684-020-0754-0. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pradere B, Ploussard G, Catto JW, Roupret M, Misrai V. The use of nonsteroidal anti-inflammatory drugs in urological practice in the COVID19 era: is “Safe Better than Sorry”? Eur Urol. 2020 doi: 10.1016/j.eururo.2020.03.033. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100331. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]