Abstract
Hospitals are important sources of pollutants resulted from diagnostic, laboratory and research activities as well as medicine excretion by patients, which include active component of drugs and metabolite, chemicals, residues of pharmaceuticals, radioactive markers, iodinated contrast media, etc. The discharge of hospital wastes and wastewater, especially those without appropriate treatment would expose the public in danger of infection. In particular, under the Coronavirus Disease 2019 (COVID-19) pandemic context in China, it is of great significance to reduce the health risks to the public and environment. In this study, technologies of different types of hospital wastes and wastewater disinfection have been summarized. Liquid chlorine, sodium hypochlorite, chlorine dioxide, ozone, and ultraviolet irradiation disinfection are commonly used for hospital wastewater disinfection. While incineration, chemical disinfection, and physical disinfection are commonly used for hospital wastes disinfection. In addition, considering the characteristics of various hospital wastes, the classification and selection of corresponding disinfection technologies are discussed. On this basis, this study provides scientific suggestions for management, technology selection, and operation of hospital wastes and wastewater disinfection in China, which is of great significance for development of national disinfection strategy for hospital wastes and wastewater during COVID-19 pandemic.
Keywords: Disinfection, Hospital, Wastes, Wastewater, Coronavirus disease 2019 (COVID-19)
Graphical abstract
Highlights
-
•
O3, UV, chlorine disinfectants are used for hospital wastewater disinfection.
-
•
Incineration, chemical and physical techniques are used to disinfect hospital wastes.
-
•
Providing suggestions for hospital wastes and wastewater disinfection during COVID-19.
-
•
The chlorine disinfection and incineration are primarily recommended.
1. Introduction
Hospitals are important sources of pollutants resulted from diagnostic, laboratory and research activities as well as medicine excretion by patients, which include active component of drugs and metabolite, chemicals, residues of pharmaceuticals, radioactive markers, iodinated contrast media, etc. (Verlicchi et al., 2010). In addition, it is estimated that 75% of the wastes produced by hospitals are general health care wastes, while the remaining 25% are regarded as hazardous infectious wastes (Prüss et al., 1999; Taghipour et al., 2014). Improper disposal of infectious hospital wastes and wastewater could cause serious risks to public health and environment.
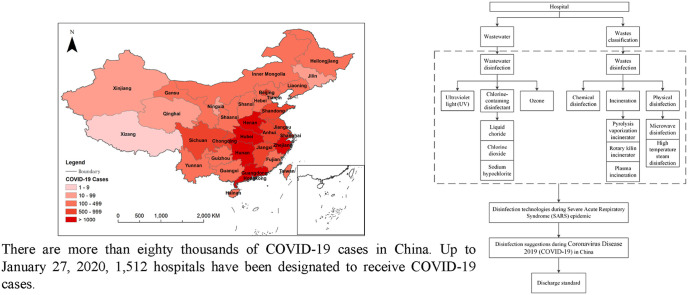
An unexplained case of pneumonia was first reported in Hubei, China (Chan et al., 2020). By January 7th, 2020, Chinese scientists had isolated a Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) from patients in Wuhan (Wang et al., 2020). Following the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-1) outbreak in 2002 and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) outbreak in 2012, SARS-CoV-2 becomes the third coronavirus to emerge in the past two decades, which has put global public health institutions on high alert (Munster et al., 2020). Chan et al. (2020) carried out a study on a family of six patients, they noticed that one family member, who did not travel to Wuhan, became infected after contact with other family members. According to World Health Organization (2020), the transmission routes of SARS-CoV-2 include droplet transmission and contact transmission; airborne transmission may be possible in specific circumstances and settings in which procedures or support treatments that generate aerosols are performed. So far, over eighty thousands of people have been diagnosed as Coronavirus Disease 2019 (COVID-19) all over China (Fig. 1 ). In the globe, the number of confirmed cases have exceeded 2.7 million, and the amount of confirmed cases is still climbing with the accumulated death over 187,000. In the United States, Spain, Italy, Germany, the United Kingdom, France, and Turkey, the number of confirmed cases have all exceeded 100 thousands as of April 25, 2020.
Fig. 1.
The distribution of Coronavirus Disease (2019) (COVID-19) confirmed cases in China on April 2, 2020.
The discharge of hospital wastes and wastewater, especially those without appropriate treatment would expose the public in danger of infection. In particular, under the COVID-19 pandemic context in China, it is of great significance to reduce the health risks to the public and environment. Thus, it is necessary to appropriately disinfect and dispose of the hospital wastes and wastewater before being transported or discharged. Although domestic and foreign scholars have carried out a variety of studies focusing on the wastewater treatment, general waste disposal, hospital management, etc., the systematic studies concerning disinfection of hospital wastes and wastewaters, especially specific disinfection suggestions during COVID-19 pandemic, are rare to date. Therefore, the current review will concentrate on disinfection technologies for treatment of hospital wastes and wastewater, and provide suggestions for hospital wastes and wastewater disinfection during COVID-19 pandemic in China.
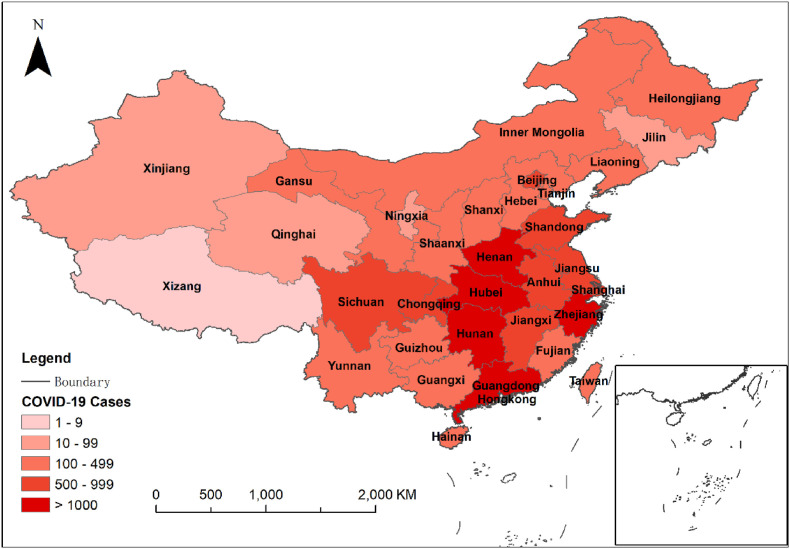
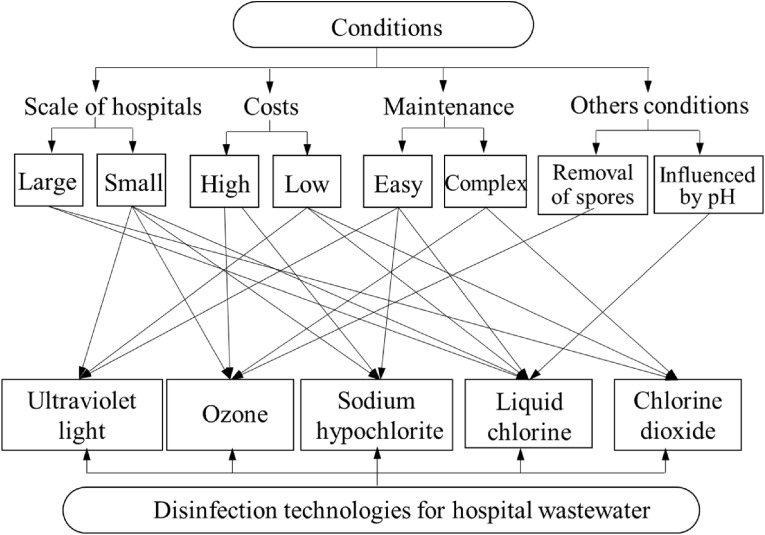
2. Disinfection of hospital wastewater
Ozone, ultraviolet irradiation, liquid chlorine, chlorine dioxide, and sodium hypochlorite disinfections are commonly used technologies for hospital wastewater disinfection (Chen et al., 2014; Lizasoain et al., 2018; Yu et al., 2014). Fig. 2 shows the general wastewater disinfection system in the hospital. Every disinfection technology has unique advantages and disadvantages as summarized in Table 1 . The utilization of a certain type of disinfection technology should be determined by the comprehensive consideration of both economic and feasible factors, such as the amount of wastewater, safety conditions, the supply of disinfectants, the distance between the wastewater treatment system and the ward as well as the residential area, investment and operation costs, operation management level, etc. (Fig. 3 ).
Fig. 2.
Flow chart of hospital wastewater disinfection process.
Table 1.
Comparison of Disinfection technologies for hospital wastewater (Fan et al., 2017; Kühn et al., 2003; Kleinböhl et al., 2018; Messerle et al., 2018; Yu et al., 2013).
| Disinfection technology | Advantages | Disadvantages |
|---|---|---|
| Liquid chlorine | Low energy consumption | High storage risk |
| Ultraviolet light | Low investment and operation costs | Inadequate depth of penetration and occupational health risks |
| Chlorine dioxide | High efficiency and low operation costs | Inconvenient storage and transport |
| Sodium hypochlorite | Low toxicity, simple equipment, stable operation, easy control, and low operation and preparation costs | High energy consumption, strong corrosiveness, and high pollution |
| Ozone | The ability of decoloring and deodorizing and quick decomposition of microorganisms | High operation costs and hazardous by-products |
Fig. 3.
Selection of disinfection technologies for hospital wastewater in different scenarios.
2.1. Chlorination pretreatment
Bleaching powder is commonly used for the chlorination pretreatment (NHC, 2002). For each ward and restroom of an infectious disease hospital or the infectious disease area of a general hospital, 1 kg of bleaching powder containing 25% of available chlorine per 10 beds should be added 3 to 4 times before further disinfection. The optimal addition time is at the end of the peak period of the restroom use. The added bleaching powder should be flushed into the septic tank with flowing water and the residual chlorine would be measured at the outlet of septic tank in case of violation of the water quality standard.
2.2. Chlorine-containing disinfectants
Chlorine is a kind of strong oxidizer, which is one of the most early used disinfection methods in disinfecting hospital wastewater (Yu-Mei et al., 2010). When using chlorine as the disinfectant, a vacuum siphon fixed-ratio chlorine dosing system is generally adopted in hospital wastewater treatment system. The pipes of the chlorination system are installed in open areas, and buried pipes are located in pipe trenches with good support and sufficient slope. When the water collection pipe in the hospital wastewater treatment system is higher than the public wastewater pipe outside the hospital or the water level (usually a height difference of 600 mm is required), a siphon-type fixed-ratio chlorine disinfection system could be used (MEE, 2003). When wastewater needs to be lifted in order to be discharged, a wastewater pump is required to be set up in front of the disinfection mixture contact tank. The disinfectant addition equipment and the lift pump could operate synchronously. The water level of the water collection tank controls the automatic activation of the wastewater pump, and the simultaneous operation of the dosing system. Usually, 30 mg/L-50 mg/L and 15 mg/L-25 mg/L chlorine is added to wastewater after primary treatment and secondary treatment, respectively (NHC, 2002). While the actual amount of chlorine added to the wastewater could be adjusted according to the residual chlorine remaining in the outlet of the wastewater treatment system and the content of reducing substances in the wastewater. In chlorine disinfection, the effective constituent is HClO. The mechanism of chlorine disinfection is:
| (1) |
2.2.1. Liquid chlorine
When using liquid chlorine for wastewater disinfection, a vacuum chlorinator must be used, and the outlet of the chlorine injection pipe should be submerged in the wastewater (Braden, 2003). It is strictly prohibited to directly add chlorine to the wastewater without a chlorinator, or using pipes that are not resistant to chlorine gas corrosion, such as polyvinyl chloride, and metal pipes such as copper, iron, and other pipes which are not resistant to chlorine solutions. Copper pipes and hard PVC pipes should be used to transport chlorine gas and chlorine containing disinfectant solutions, respectively (Zhu et al., 2014). Due to relatively high storage risk, the liquid chlorine disinfection technology is not a proper disinfection technology in regions with high population.
2.2.2. Chlorine dioxide
So far, chlorine dioxide is known as one of the efficient disinfectants with high oxidization capability even under acidic conditions (Wang, 2016). The solubility of chlorine dioxide is five times that of chlorine and the oxidization capacity of chlorine dioxide is 2.63 times that of chlorine gas. It is generally recommended that the amount of chlorine dioxide used to treat hospital wastewater is 1/2.5 that of the available chlorine (NHC, 2002). The dosing system of chlorine dioxide for wastewater disinfection is consistent with the sodium hypochlorite disinfection technology, i.e. a double siphon automatic fixed-ratio dosing chlorine system is adopted for chlorine dioxide disinfection. When using a chlorine dioxide generator, the content of chlorine dioxide must be higher than 50%, and it should ensure safe operation and automatic addition of disinfectants with certain proportion (Wang et al., 2013). Chlorine dioxide could trigger the denaturation of enzyme and protein (Ogata, 2007). It destroys the anabolic pathways of protein and thus kills the microorganism, including bacteria, viruses, fungi, spores, and clostridium botulinum. The chlorine dioxide has the ability of decoloring, deodorization, oxidation, and increasing the oxygen content in wastewater. Due to its chemical structure, the chlorine is inconvenient to be stored or transported, though it still has advantages of lower costs of operation as well as preparation (Fan et al., 2017).
2.2.3. Sodium hypochlorite
Sodium hypochlorite disinfectant could be prepared using standard NaClO generator, which could significantly reduce the costs (Casson and Bess, 2006). A double siphon automatic fixed-ratio dosing chlorine system is usually adopted for sodium hypochlorite disinfection. The content of available chlorine in sodium hypochlorite is approximately 5%–20%. And the mechanism of sodium hypochlorite disinfection is:
| (2) |
Compared with other chlorine-containing disinfectants, the use of sodium hypochlorite is featured with relatively lower toxicity, simpler equipment, more stable operation, easier control, and lower operation and preparation costs, which makes this disinfection method more feasible in smaller scale hospitals (Yu et al., 2013). Though it should be pointed out that sodium hypochlorite disinfection has higher energy consumption, stronger corrosiveness, and higher pollution (Emmanuel et al., 2004). Therefore, when using on-site prepared sodium hypochlorite for disinfection, a safe and reliable sodium hypochlorite generator with high electrical efficiency, low water consumption, low salt and electricity consumption, long operating life, and convenient operation should be employed. When raw salt is used as the raw material, the salt solution should be precipitated and filtered before being added to the sodium hypochlorite generator. Containers, pipes, equipment and accessories that contact the sodium hypochlorite solution should be made of corrosion resistant materials.
2.3. Ozone
Ozone is a disinfectant featured with high bactericidal effect, which has been widely used in water supply engineering and wastewater treatment (Chiang et al., 2003; Kist et al., 2013). The wastewater flows into the first-stage sedimentation tank, and then flows to the second-stage purification tank after purification. After proper treatment, it flows to the regulating storage tank. It is then pumped into the contact tower by the sewage pump, and fully exposed to approximately 15 mg/L-20 mg/L ozone in the tower for 10–15 min before being discharged. Generally, a hospital with 300 beds is suggested to build an ozone treatment system with a wastewater treatment capacity of 18 t/h to 20 t/h (NHC, 2002). Since the ozone disinfection has the capacity of decoloring and deodorizing, the wastewater after treatment becomes bright and transparent without odor. Also, the molecule structure of ozone is unstable, which implies that strong oxidative atomic oxygen produced by the decomposition of ozone molecule would quickly decompose microorganisms, such as bacteria and viruses, in wastewater. Although ozone disinfection could improve the water quality in shorter time with higher efficiency, the operation costs of ozone preparation are high (Arslan et al., 2017). Moreover, the by-products, which are produced through the chemical reaction with bromide and iodide, are hazardous to human health (Kleinböhl et al., 2018). And over-dose of ozone is easy to cause bad smell and secondary pollution. Therefore, ozone disinfection is mainly suitable for smaller scale wastewater treatment system, especially wastewater treatment system with relatively high effluent quality.
2.4. Ultraviolet light (UV)
Ultraviolet light (UV) refers to the electromagnetic wave with length between 200 nm and 400 nm. The UV was first used in disinfection of drinking water in 1910 (White et al., 1986). The UV could be divided into 4 wavebands based on different wavelength, including ultraviolet A (315 nm–400 nm), ultraviolet B (280 nm–315 nm), ultraviolet C (200 nm–280 nm), and vacuum ultraviolet (100 nm–200 nm). Thereinto, vacuum ultraviolet could not be used in disinfection because it is absorbed by the wastewater. The bands with wavelength between 200 nm and 300 nm could damage the structure of both DNA and RNA of the bacteria, viruses, and single-celled microorganisms and thus inhibit the protein synthesis. Therefore, the ultraviolet B and ultraviolet C have the best bactericidal effect. It is generally believed that the band with wavelength of 253.7 nm is optimal for ultraviolet disinfection (Meulemans, 1987). Compared with chlorine disinfection, the investment and operation costs of UV disinfection are significantly lower. However, disinfection with UVC is sometimes unsatisfactory since the depth of penetration is inadequate and there are occupational health risks (Kühn et al., 2003).
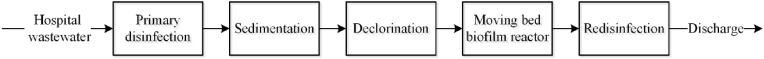
3. Disinfection of hospital wastes
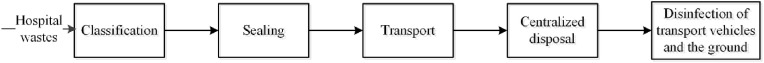
Different with the disinfection of hospital wastewater, the hospital wastes are usually classified before disinfection as shown in Fig. 4 (Blenkharn, 2007). The typical composition of healthcare waste is approximately 85% general non-infectious, 10% infectious/hazardous, and 5% chemical/radioactive (WHO, 2014). This section first summarizes main types of hospital waste disinfection technologies, including incineration, chemical disinfection and physical disinfection, and then illustrates the proper disinfection technologies used in different situations.
Fig. 4.
Flow chart of hospital waste disinfection process.
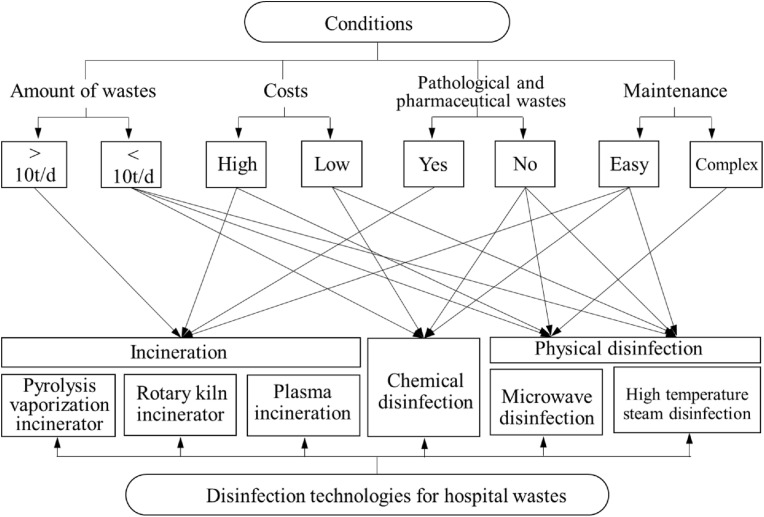
Similar with disinfection technologies for hospital wastewater, the hospital wastes disinfection technologies have their own characteristics. Therefore, factors such as the amount of waste, costs, maintenance and types of waste, etc. should be taken into consideration when selecting appropriate disinfection technologies in a certain hospital as shown in Fig. 5 . For example, the incineration technology could be adopted when the amount of wastes is large and the investment is sufficient when disinfecting pathological or pharmaceutical wastes. If the scale of the hospital is smaller and the investment is limited, chemical disinfection and high temperature steam disinfection which are easily maintained are preferred.
Fig. 5.
Selection of disinfection technologies for hospital wastes in different scenarios.
3.1. Incineration
Incineration is safe, simple and effective, which has been one of the most widely used disposal technology especially in developing countries (Ghodrat et al., 2017). The temperature of the incinerator (outlet temperature) is over 800 °C. This high temperature could not only completely kill microorganisms, but also incinerate and burn most organic matters and transform them into inorganic dusts. After incineration, the volume of solid wastes could be reduced by approximately 85–90% (Lee and Huffman, 1996). Except for explosive and radioactive wastes, other hospital wastes could be incinerated. The waste preparation, waste incineration and flue gas purification in different hospital waste incineration treatment facilities are different. So far, the common incineration technologies include pyrolysis vaporization incinerators, rotary kiln incinerators, plasma incineration technology, etc. (Jiang et al., 2012; Sapuric et al., 2016). Thereinto, pyrolysis vaporization incinerators and rotary kiln incinerators are widely used in China (Chen and Yang, 2016).
3.1.1. Pyrolysis vaporization incinerator
When the pyrolysis vaporization incinerator operates, the air measured below the theoretical chemical reaction is first sent to the fixed furnace level of the primary combustion chamber for combustion. Thus, the organic components of the waste are decomposed into flammable gases in order to avoid dusts due to the turbulence caused by the excess air. As a result, the emission of particulate matters is reduced, the residue is continuously discharged from the end of the hearth, and the flammable gas is sent to the secondary combustion chamber. And sufficient air is supplied to make it completely burn. A high temperature environment above 850 °C is conducive to the complete destruction of toxic and hazardous components, thereby reducing the production of toxic pollutants such as dioxins due to low temperature combustion (Zhu et al., 2008).
3.1.2. Rotary kiln incinerator
This kind of rotation during the operation of the incinerator not only helps the wastes to be automatically transported in the kiln, but also allows the wastes to be well mixed, thereby improving the incineration efficiency. The rotary kiln incinerator technology has advantages on a wide range of applications, good adaptability, handling a variety of different types of wastes, good gas and solid contact, and uniform reaction (Pei and Wu, 2007). The temperature could be as high as 1,200 °C or more, which effectively destroys most hazardous substances. However, for small and medium scales equipment below the disposal capacity scale of 6 t/d to 8 t/d, the investment costs are relatively high and the investment recovery rate is relatively low; in addition, the excess air demand is higher than that of pyrolysis incinerator, and the dust content in the exhaust is slightly higher (Chen and Yang, 2016). The mechanical parts of the incineration system are complicated and the maintenance costs are also high.
3.1.3. Plasma incineration
Plasma incineration technology is a novel wastes disposal technology (Chang-Ming et al., 2016). The essential of this technology is to transfer energy through the plasma, so that the wastes could be quickly decomposed into small molecules and even atoms. Thus, there are no intermediate products of large molecules. Most of the gases produced are flammable and sent to the secondary combustion chamber for complete combustion. It is then discharged into the atmosphere after simple purification. Compared with conventional incineration technologies, the plasma incineration shows a higher energy efficiency, which demonstrates a promising application prospect (Messerle et al., 2018).
3.2. Chemical disinfection
Chemical disinfection technology has a long history and a wide range of applications. Chemical treatment of hospital wastes is usually used in combination with mechanical crushing treatment (Zhang, 2013). Generally, the crushed hospital wastes are mixed with chemical disinfectants (such as sodium hypochlorite, calcium hypochlorite, chlorine dioxide, etc.) and stayed for a sufficient time. During the disinfection process, organic substances are decomposed, and infectious microorganisms are killed or inactivated. Chemical disinfectants are featured with low effective concentration, rapid action, stable performance, and broad sterilization spectrum, they not only kill microorganisms, but also bacteria spores (Wu et al., 2005). Therefore, sodium hypochlorite, calcium hypochlorite, chlorine dioxide, etc. are generally used because they are non-corrosive to items, odorless, tasteless, colorless, inflammable, safe, and easily soluble in water but not easily affected by physical or chemical factors with low toxicity and no residual hazard after disinfection (Chen and Yang, 2016). When the amount of hospital wastes is small, chemical disinfection technology could be considered.
3.3. Physical disinfection
3.3.1. Microwave disinfection
Microwaves are electromagnetic waves with a wavelength of 1 to 1,000 mm and a frequency between hundreds of megahertz and 3,000 MHz. Microwave frequencies used for disinfection are generally (2,450 ± 50) MHz and (915 ± 25) MHz (Neto et al., 1999). The microwave passes through the medium and is absorbed by the medium to generate heat. The heat is generated by the substance molecules vibrating and rubbing for billions of times per second, thereby achieving the effect of high temperature disinfection. The microwave disinfection technology is characterized with energy saving, low action temperature, slow heat loss, rapid action, light damage, and low environmental pollution with no residues or toxic wastes after disinfection (Ohtsu et al., 2011). It has a wide disinfection spectrum of bacteria, which can kill various microorganisms. Regarding the ability to destroy pathogens, there is now convincing evidence that specially constructed microwave systems are able to sufficiently inactivate microorganisms; however, the process has to be strictly controlled by special microwave devices. Conventional microwave units have no means to control the inactivation process and the moisture content. Though a few sophisticated microwave technologies with appropriate measurements are currently only used for the treatment of biohazardous wastes, it needs to be evaluated whether they would also have advantages for processes involving the control of water content such as the drying of biotherapeutic products (Walters et al., 2014).
Microwave disinfection technology, as an effective supplementary technology for incineration, is gradually being promoted in China, which will effectively promote the diversification of hospital wastes disinfection technologies in China. According to Technical specifications for microwave disinfection centralized treatment engineering on medical waste (on trial) published by Ministry of Ecology and Environment (MEE) of China, the disinfection effects of microwave disinfection technology could achieve: (1) the logarithmic value of killing bacteria, fungi, lipophilic or hydrophilic viruses, parasites, and mycobacteria of propagules ≥ 6 and (2) logarithmic value of killing Bacillus subtilis black spores ≥ 4.
3.3.2. High temperature steam disinfection
High temperature steam disinfection refers to the wet heat treatment process that uses high temperature steam (saturated water vapor with temperature higher than 100 °C) to kill microorganisms on the transmission medium (Zhang et al., 2016). The hospital wastes are exposed in an environment with a certain temperature of water vapor for a certain period of time. Due to the latent heat released by the water vapor, pathogenic microorganisms undergo protein denaturation and coagulation, which leads to the death of microorganisms (Bao et al., 2013).
In China, it is required that the logarithmic value of the killing of thermophilic lipobacillus spores should be ≥ 5 (MEE, 2006). Limited by various factors, the sterilization temperature in the sterilization room is generally set to 134 °C, and the fluctuation range is less than 3 °C. At this temperature, the time required to achieve the disinfection effect usually does not exceed 20 min. When the equipment has a high disinfection capacity, the sterilization chamber has a large loading capacity, and the time for steam to penetrate into the hospital wastes packaging is longer. However, the high temperature steam disinfection method has low volume reduction rate, and easily generates toxic volatile organic compounds during the disinfection (Teng et al., 2015); therefore, it is unable to disinfect all kinds of hospital wastes.
3.4. Application of disinfection technologies on different types of hospital wastes in China
Table 2 demonstrates advantages and disadvantages of main disinfection technologies of hospital wastes. It should be pointed out that high temperature incineration is a very effective disinfection technology that can simultaneously achieve the harmlessness, reduction and resource utilization of hospital wastes. Although the high temperature incineration method has a large disposal amount, the investment is high, the heat value of wastes must meet certain requirements, and there is a risk of generating hazardous substances such as dioxins during low temperature combustion (Vermeulen et al., 2012). However, pyrolysis vaporization incinerators and rotary kiln incinerators have already met the requirements of relevant environmental standards with appropriate intervention measures (Zhao et al., 2015). From the perspective of investment and operation costs as well as economic and social benefits, high temperature incineration is still one of the most valuable hospital waste disinfection technology in China. Therefore, when the amount of hospital wastes generated is large, high temperature incineration technology could be considered.
Table 2.
Comparison of Disinfection technologies for hospital wastes (Chang-Ming et al., 2016; Ghasemi and Yusuff, 2016; Ohtsu et al., 2011; Pei and Wu, 2007; Zhao and Xie, 2018).
| Disinfection technology | Advantages | Disadvantages |
|---|---|---|
| Pyrolysis vaporization incinerator | Complete destruction of toxic and hazardous components | High investment costs and strict demand for heat value of wastes |
| Rotary kiln incinerator | High incineration efficiency with wide range of applications and good adaptability | High dust content in the exhaust, high air demand, high investment and maintenance costs, and low investment recovery |
| Plasma incineration | High energy efficiency with no intermediate products | High requirement of technical personnel and high costs |
| Chemical disinfection | Rapid action, stable performance, and broad sterilization spectrum | Residual disinfectants after disinfection |
| Microwave disinfection | Energy saving, low action temperature, slow heat loss, rapid action, light damage, and low environmental pollution with no residues or toxic wastes | Relative narrow disinfection spectrum and complex impact factors of disinfection |
| High temperature steam disinfection | Low investment and operation costs, simple operation management, and low secondary pollution | Weak odor control |
3.4.1. Classification of hospital wastes
Table 3 summaries main types of hospital wastes, including domestic wastes, infectious wastes, pathological wastes, sharp wastes, pharmaceutical wastes, chemical wastes, and radioactive wastes. Most of the hospital wastes are not hazardous, which does not need special treatment or disinfection. However, once these non-hazardous wastes are mixed with other hazardous or infectious pollutants, special disposal and disinfection are required. Therefore, the classification of hospital wastes is a prerequisite for effective disinfection of hospital wastes. In addition, different disinfection and disposal methods should be adopted based on unique characteristics of different hospital wastes.
Table 3.
Classification of hospital wastes (NHC, 2002).
| Classification | Definition |
|---|---|
| Domestic wastes | Domestic wastes are generated from the hospital management and the maintenance of buildings, and it is usually disposed of according to the principle of urban waste disposal. |
| Infectious wastes | Infectious wastes refer to wastes that may contain pathogenic bacteria, viruses, parasites, or fungus in concentrations and quantities sufficient to cause disease in humans, which mainly include: (1) medium of bacterial colonies and pathogenic strain as well as culture preservation solution used in the laboratory; (2) wastes of infectious patients, such as tissues, contaminated materials, and instruments after surgery or autopsy; (3) wastes from infectious wards, such as feces, dressings for surgical or infected wounds, heavily contaminated clothes, etc.; (4) wastes of infectious patients produced in hemodialysis, such as dialysis equipment, test tubes, filters, apron, gloves, etc.; (5) infected animals in the laboratory; (6) any equipment or materials which are contacted by infectious disease patients or animals; (7) used disposable syringes, infusion sets, blood transfusion apparatus, etc. |
| Pathological wastes | Including tissues, organs, parts of the body, fetal death and animal carcasses, blood, body fluids. |
| Sharp wastes | Sharp objects refer to objects that could puncture or cut people, including needles, hypodermic needles, scalpels, infusion sets, surgical saws, broken glasses and nails. |
| Pharmaceutical wastes | The pharmaceutical wastes include expired, eliminated, crushed or contaminated medicines, vaccines, and serum. |
| Chemical wastes | Chemical wastes include solids, liquids, and gases that are toxic, corrosive, flammable, reactive, or genotoxic in the process of diagnosis, testing, cleaning, management, and disinfection. Such as formaldehyde, photography agents, organic compounds, etc. |
| Radioactive wastes | Radioactive wastes contain solids, liquids, and gases contaminated with radionuclides. Such as solid waste (absorbent paper, mop, glassware, syringes, small medicine dishes) with low activity, residues and diagnostic agents in containers of radioactive materials. |
3.4.2. Disinfection of infectious wastes
Wastes in hospitals should be appropriately disposed of because these wastes are proved to be associated with in-hospital transmission of infection or injury (Rutala and Sarubbi, 1983). Liu et al. (2017) investigated 125 hospitals in China, and found that main wastes are infectious wastes and sharp wastes, which account for 87.00% and 11.34% of the total hospital wastes, respectively, with the hospital waste generation rate of approximately 0.48 kg/bed/day. According to Technical Standard For disinfection (NHC, 2002), for wastes of infectious disease patients, the feces, vomit, urine should be disinfected using bleaching powder, restrooms, clothes, towels, etc. should be disinfected using solution containing sufficient available chlorine. In addition, leftovers that could be used as animal feed must be boiled for 30 min before being transported. Inflammable solid wastes with no use value, sharp wastes, and infectious wastes could be incinerated as much as possible under permitted conditions.
3.4.3. Disinfection of disposable medical supplies
Used disposable syringes, infusion sets, transfusion apparatus and other items must be disinfected and destroyed on-site, and collected by the designated unit of the local agency for centralized collection and disposal (Huang et al., 2009). It is strictly prohibited to sell to other non-designated units or discard at will. Disposable medical supplies should be disinfection via direct incineration. If the incineration method is not available, they could be alternatively soaked in a disinfectant containing sufficient effective chlorine before being destroyed.
3.4.4. Disinfection of pharmaceutical wastes
For a small amount of pharmaceutical wastes, landfill and storage could be adopted, and they could also be incinerated with infectious wastes; while for a large number of pharmaceutical wastes, incineration is preferred (NHC, 2002). The pharmaceutical wastes could also be disposed of at sanitary landfills after sealing. Glass ampoules cannot be incinerated, but they could be crushed first and then processed with sharp wastes.
3.4.5. Disinfection of chemical wastes
General chemical wastes, such as sugar, amino acids, and specific salts, could be disposed of with municipal wastes or discharged into the drainage system (Zhao, 2018). If the amount of hazardous chemical wastes is small, such as residual chemical in the package, they could be treated via pyrolysis incinerator, storage or landfill. While if the amount of hazardous chemical wastes is large, flammable wastes could be treated by incineration, others could also be treated using chemical disinfectants.
3.4.6. Disinfection of radioactive wastes
The excrement of patients treated with radiopharmaceuticals should be collected and disposed of. The excrement in the special septic tank should be stored for 10 half-lives and discharged into the drainage system. When collecting feces from patients with 131−I, NaOH or 10% KI solution must be added at the same time and sealed and stored for disposal. However, if patient excrement also contains pathogenic microorganisms, it must be collected separately with special containers, which is not allowed to be discharged into the drainage system until storage, decay and disinfection have been completed (Chen et al., 2015).
4. Suggestions for disinfection of hospital wastes and wastewater during COVID-19 pandemic in China
Recently, RNA of SARS-CoV-2 has been found in feces of patients, which triggered concern to the disinfection of wastes and wastewater of designated hospitals during COVID-19 pandemic in China. Ong et al. (2020) believed that transmission may also occur through fomites in the immediate environment around the infected person. Based on previous studies concerning the pathogen transmission in wastewater system, Gormley et al. (2020) claimed that under some circumstances, the wastewater system has the potential to enable airborne transmission of SARS-CoV-2. These are consistent with the fact in a study that SARS-CoV-2 from a single stool specimen has been cultured (Zhang et al., 2020). It is also reported that wastewater discharged from a COVID-19 designated hospital was SARS-CoV-2 RNA positive, indicating that the virus might contaminate the drainage system (China Citywater, 2020). In addition, the disinfection of hospital wastes is also in high necessity since the waste generation increases exponentially during this period, which may accelerate disease spread and pose a significant risk on both medical staffs and patients without proper collection and disinfection (Yu et al., 2020).
There is only few studies on inactivation of SARS-Cov-2 so far. While, Chan et al. (2020) reported that the genome of the SARS-CoV-2 strains are phylogenetically closest to the bat SARS-related coronaviruses, and the Spike protein has a 78% nucleotide identity with the human SARS-CoV-1. Due to the similarities between SARS-CoV-1 and SARS-CoV-2, the SARS-CoV-2 might also be sensitive to either environment factors or disinfectants. Therefore, disinfection technologies adopted during SARS epidemic could be used as good reference to inactivation of SARS-Cov-2 in hospital wastes and wastewater. SARS-CoV-1 could exist for 2 days, 3 days, and 17 days in the hospital wastewater, stool, and urine at 20 °C, respectively (Wang et al., 2005). All SARS viruses could be inactivated in 30 min at 20 °C with more than 0.5 mg/L residual free chlorine or 2.19 mg/L residual chlorine dioxide left (Chen et al., 2006). Chen et al. (2006) compared disinfection performance of different technologies and reported that chlorine and UV irradiation were the most efficient followed by chlorine dioxide, though efficiency of ozone disinfection was not ideal. This result was in line with findings reported by Wang et al. (2005).
Up to January 27, 2020, there has been 1512 COVID-19 designated hospitals all over China. In Wuhan, local MEE has established an emergency scheme for disposal of wastewater from temporary treatment centers, which are newly built COVID-19 designated hospital for cases with mild symptoms in Wuhan, China. Chlorine disinfection (liquid chlorine, chlorine dioxide, and sodium hypochlorite), which has long been used in hospital wastewater disinfection in China, is adopted in this scheme. The available chlorine is recommended to be approximately 50 mg/L. For disinfection septic tank, the contact duration should be longer than 1.5 h with residual chlorine over 6.5 mg/L and fecal coliform colonies less than 100 per liter. In addition, UV irradiation and heating are also suggested for wastewater disinfection in other COVID-19 designated hospitals because of fewer by-products and ideal disinfection performance. The water quality of wastewater discharged from the hospital should meet requirements below (Table 4 ). Moreover, the infectious wastes should also be collected in time under protective conditions. They are suggested to be disinfected using solid or liquid chlorine containing disinfectants with available chlorine concentration of 20 g/L and disinfection duration of 2 h. Pharmaceutical wastes and chemical wastes are suggested to be incinerated. Radioactive wastes contaminated with SARS-CoV-2 are suggested to be disinfected as infectious wastes after storing for at least 10 half-lives and. Disposable protection products should also be treated as infectious wastes. For example, respirators should be soaked in 75% alcohol for 30 min. Moreover, chlorine disinfectants with 500 mg/L and 1,000 mg/L are suggested for disinfection of other protection products without or with obvious contamination, respectively. The disinfection performance of hospital wastes should meet requirements below.
Table 4.
Indicators of disinfection performance of hospital wastewater and wastes.
| Indicator | Value range | |
|---|---|---|
| Wastewater | Fecal coliform (MPN/L) | ≤900 |
| Enteric pathogens | Not detected | |
| Mycobacterium tuberculosis | Not detected | |
| Disinfection contact time | ≥1.5 h (Chlorination) | |
| ≥0.5 h (Chlorine dioxide method) | ||
| Total residual chlorine (mg/L) | ≥6.5 (Chlorination) | |
| ≥4.0 (Chlorine dioxide method) | ||
| Wastes | Incineration of wastes | Complete |
| pH after alkali disinfection | 12 (for 24 h) | |
| Residual chlorine after Chlorination | >200 mg/L | |
| Pathogens | Not detected |
Hospital wastes and wastewater (as well as the sludge) must be treated and disinfected properly before discharge. Without disinfection, they should not be allowed to be arbitrarily discharged or used as agricultural fertilizer. The use of any infiltration wells/pits to discharge wastewater and sludge, or the discharge into sanitary protection zone of drinking water sources should also be strictly forbidden. In addition, government should take measures to improve the management of hospital wastes and wastewater, especially during the COVID-19 pandemic. The hospital should set up a recycling system and assign special personnel to take charge, and strengthen the management of each department to prevent waste loss. Personnel involved in the disposal of disposable medical supplies must be qualified and strengthened in personal protection. In recent years, many new advances have also been made in hospital wastes and wastewater treatment technologies, such as radiation disinfection technology, reverse polymerization disinfection technology, plasma disinfection technology, and thermal gasification disinfection technology. They have certain promotion value, but due to the high investment costs, these technologies have not been used at a large scale. With the improvement of hospital wastes and wastewater disinfection technologies, the costs of disinfection will continue to decrease, and secondary pollution to the environment will be gradually controlled. During the disinfection, the environmental pollution or effects on human health could be significantly reduced if the operation strictly obeys the requirements. In order to develop more secure, efficient, economical disinfection methods, local environment and actual conditions should be brought into consideration in future studies.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by the National Natural Science Foundation of China [grant number 81903377]. The authors would like to acknowledge all health-care workers involved in the diagnosis and treatment of patients in China; we thank Prof. Xiaoming Shi for guidance in study design; and we thank Ms. Yan Liao and many other staff members at the China CDC for their contributions.
References
- Arslan A., Topkaya E., Özbay B., Özbay I., Veli S. Application of O3/UV/H2O2 oxidation and process optimization for treatment of potato chips manufacturing wastewater. Water Environ. J. 2017;31:64–71. [Google Scholar]
- Bao Z., Jin D., Teng H., Li Y. The general process of medical waste high temperature steam sterilization treatment technology. Adv. Mater. Res. 2013:1160–1163. [Google Scholar]
- Blenkharn J.I. Classification and management of clinical wastes. J. Hosp. Infect. 2007;65:177–178. [Google Scholar]
- Braden M.R. In: Chlorinator for Wastewater Treatment Systems. Patent U.S., editor. U.S; 2003. [Google Scholar]
- Casson L.W., Bess J.W. On-site sodium hypochlorite generation. Proc. Water Environ. Feder. 2006:6335–6352. 2006. [Google Scholar]
- Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J., Xing F., Liu J., Yip C.C.-Y., Poon R.W.-S., Tsoi H.-W., Lo S.K.-F., Chan K.-H., Poon V.K.-M., Chan W.-M., Ip J.D., Cai J.-P., Cheng V.C.-C., Chen H., Hui C.K.-M., Yuen K.-Y. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang-Ming D.U., Wu J., Huang Y. Analysis of critical technology for hydrogen production in plasma pyrolysis and gasification of organic waste. China Environ. Sci. 2016;36:3429–3440. [Google Scholar]
- Chen C., Zhang X., Wang Y., Zhu L., Liu J. Biomedical and Environmental Sciences; 2006. Waste Water Disinfection during SARS Epidemic for Microbiological and Toxicological Control; pp. 173–178. [PubMed] [Google Scholar]
- Chen L., Zhou H., Yu B., Huang Z.W. Comparison study on hospital wastewater disinfection technology. Adv. Mater. Res. 2014;884–885:41–45. [Google Scholar]
- Chen M., Yang H. Currenet status of medical wastes disinfection and disposal technologies. Chin. J. Disinfect. 2016;33:171–174. [Google Scholar]
- Chen X., Qu l., Yin X., Gai R. Analysis of nuclear medical staffs’ knowledge and altitude on radioactive medical wastes management. Chin. J. Radiol. Health. 2015;24:164–166. [Google Scholar]
- Chiang C.-F., Tsai C.-T., Lin S.-T., Huo C.-P., Victor Lo K. Disinfection of hospital wastewater by continuous ozonization. J. Environ. Sci. Health, Part A. 2003;38:2895–2908. doi: 10.1081/ese-120025839. [DOI] [PubMed] [Google Scholar]
- China Citywater . 2020. Measurement to Reveal the Transmission of SARS-CoV-2 from Wards to the Drainage System.http://www.chinacitywater.org/zwdt/swyw/102892.shtml [Google Scholar]
- Emmanuel E., Keck G., Blanchard J.M., Vermande P., Perrodin Y. Toxicological effects of disinfections using sodium hypochlorite on aquatic organisms and its contribution to AOX formation in hospital wastewater. Environ. Int. 2004;30:891–900. doi: 10.1016/j.envint.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Fan D., Tian Y., Han L., Liu Z., Teng Y., Li B. Catalytic electrolysis of sodium chlorite to prepare highly pure chlorine dioxide. J. Funct. Mater. 2017;48 09150-9156. [Google Scholar]
- Ghasemi M.K., Yusuff R.B.M. Advantages and disadvantages of healthcare waste treatment and disposal alternatives: Malaysian scenario. Pol. J. Environ. Stud. 2016;25:17–25. [Google Scholar]
- Ghodrat M., Rashidi M., Samali B. Life cycle assessments of incineration treatment for sharp medical waste. Energy Technol. 2017:131–143. [Google Scholar]
- Gormley M., Aspray T.J., Kelly D.A. COVID-19: mitigating transmission via wastewater plumbing systems. Lancet Glob. Health. 2020 doi: 10.1016/S2214-109X(20)30112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Yu B., Zhang B., Deng M. Study on the status and measures of disposable medical supplies disposal and management. J. Occup. Environ. Med. 2009;26:93–96. [Google Scholar]
- Jiang C., Ren Z.Y., Tian Y.J., Wang K.X. Application of best available technologies on medical wastes disposal/treatment in China (with case study) In: Jinhui L., Hualong H., editors. Seventh International Conference on Waste Management and Technology. Elsevier Science Bv; Amsterdam: 2012. pp. 257–265. [Google Scholar]
- Kühn K.P., Chaberny I.F., Massholder K., Stickler M., Erdinger L. Disinfection of surfaces by photocatalytic oxidation with titanium dioxide and UVA light. Chemosphere. 2003;53:71–77. doi: 10.1016/S0045-6535(03)00362-X. [DOI] [PubMed] [Google Scholar]
- Kist L.T., Rosa E.C., Machado E.L., Camargo M.E., Moro C.C. Glutaraldehyde degradation in hospital wastewater by photoozonation. Environ. Technol. 2013;34:2579–2586. doi: 10.1080/09593330.2013.781200. [DOI] [PubMed] [Google Scholar]
- Kleinböhl A., Willacy K., Friedson A.J., Chen P., Swain M.R. Buildup of abiotic oxygen and ozone in moist atmospheres of temperate terrestrial exoplanets and its impact on the spectral fingerprint in transit observations. Astrophys. J. 2018;862:92. [Google Scholar]
- Lee C.C., Huffman G.L. Medical waste management/incineration. J. Hazard Mater. 1996;48:1–30. [Google Scholar]
- Liu S., Ren N., Li C., Shan S., Miao F., Yang L., Feng L., Meng X., Wen X., Gong R.e., Xiong X., Fu C., Wu A. Status of management of medical waste in 125 medical institutions. Chin. J. Nosocomiol. 2017;27:4265–4269. [Google Scholar]
- Lizasoain A., Tort L.F.L., García M., Gillman L., Alberti A., Leite J.P.G., Miagostovich M.P., Pou S.A., Cagiao A., Razsap A., Huertas J., Berois M., Victoria M., Colina R. Human enteric viruses in a wastewater treatment plant: evaluation of activated sludge combined with UV disinfection process reveals different removal performances for viruses with different features. Lett. Appl. Microbiol. 2018;66:215–221. doi: 10.1111/lam.12839. [DOI] [PubMed] [Google Scholar]
- MEE . 2003. Technical Guideline for Hospital Wastewater Treatment. [Google Scholar]
- MEE . MEE; 2006. Technical Specifications for Steam-Based Centralized Treatment Engineering on Medical Waste (On Trial) [Google Scholar]
- Messerle V.E., Mosse A.L., Ustimenko A.B. Processing of biomedical waste in plasma gasifier. Waste Manag. 2018;79:791–799. doi: 10.1016/j.wasman.2018.08.048. [DOI] [PubMed] [Google Scholar]
- Meulemans C.C.E. The basic principles of UV disinfection of water. Ozone Sci. Eng. 1987;9:299–314. [Google Scholar]
- Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China — key questions for impact assessment. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- Neto A.G., Carvalho J.N.D., Fonseca J.A.C.D., Carvalho A.M.D.C., Castro M.M.D.M.V. IEEE; 1999. Microwave Medical Waste Disinfection: a Procedure to Monitortreatment Quality, 1999 SBMO/IEEE MTT-S International Microwave and Optoelectronics Conference; pp. 63–65. [Google Scholar]
- NHC . 2002. Technical Standard for Disinfection. [Google Scholar]
- Ogata N. Denaturation of protein by chlorine dioxide: oxidative modification of tryptophan and tyrosine residues †. Biochemistry. 2007;46:4898–4911. doi: 10.1021/bi061827u. [DOI] [PubMed] [Google Scholar]
- Ohtsu Y., Onoda K., Kawashita H., Urasaki H. A comparison of microwave irradiation, electric, and hybrid heating for medical plastic-waste treatment. J. Renew. Sustain. Energy. 2011;3:435. [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei Z., Wu W. Application of rotary kiln incinerator in medical waste treatment. Environ. Eng. 2007;25:55–57. [Google Scholar]
- Prüss A., Giroult E., Rushbrook P. World Health Organization; 1999. Safe Management of Waste from Health Care Activities. [Google Scholar]
- Rutala W.A., Sarubbi F.A., Jr. Management of infectious waste from hospitals. Infect. Contr. 1983;4:198–204. doi: 10.1017/s0195941700058227. [DOI] [PubMed] [Google Scholar]
- Sapuric Z., Dimitrovski D., Dimitrovski M., Ivanovski F. Medical waste incineration in skopje. Regulation and standards. J. Environ. Protect. Ecol. 2016;17:805–812. [Google Scholar]
- Taghipour H., Mohammadyarei T., Asghari Jafarabadi M., Asl Hashemi A. On-site or off-site treatment of medical waste: a challenge. J. Environ. Health Sci. Eng. 2014;12:68. doi: 10.1186/2052-336X-12-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng H., Jin D., Bao Z., Li Y. 2015. The Key Problem and Solution of Medical Waste High-Temperature Steam Treatment, Asia-Pacific Energy Equipment Engineering Research Conference. [Google Scholar]
- Verlicchi P., Galletti A., Petrovic M., Barceló D. Hospital effluents as a source of emerging pollutants: an overview of micropollutants and sustainable treatment options. J. Hydrol. 2010;389:416–428. [Google Scholar]
- Vermeulen I., Van Caneghem J., Block C., Dewulf W., Vandecasteele C. Environmental impact of incineration of calorific industrial waste: rotary kiln vs. cement kiln. Waste Manag. 2012;32:1853–1863. doi: 10.1016/j.wasman.2012.05.035. [DOI] [PubMed] [Google Scholar]
- Walters R.H., Bhatnagar B., Tchessalov S., Izutsu K.-I., Tsumoto K., Ohtake S. Next generation drying technologies for pharmaceutical applications. J. Pharmaceut. Sci. 2014;103:2673–2695. doi: 10.1002/jps.23998. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020 doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Cao J., Zhang D., Yang Z. Design and operation of hospital comprehensive wastewater treatment engineering. China Water & Wastewater. 2013;29:74–77. [Google Scholar]
- Wang X.W., Li J.S., Jin M., Zhen B., Kong Q.X., Song N., Xiao W.J., Yin J., Wei W., Wang G.J., Si B.Y., Guo B.Z., Liu C., Ou G.R., Wang M.N., Fang T.Y., Chao F.H., Li J.W. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J. Virol Methods. 2005;126:171–177. doi: 10.1016/j.jviromet.2005.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. Study of wastewater advanced treatment and reclaimed water reuse for a large general hospital. Meteorol. Environ. Res. 2016;7:37–39. [Google Scholar]
- White S.C., Jernigan E.B., Venosa A.D. A study of operational ultraviolet disinfection equipment at secondary treatment plants. J. (Water Pollut. Contr. Feder.) 1986;58:181–192. [Google Scholar]
- World Health Organization (WHO) 2020. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. [Google Scholar]
- World Health Organization (WHO) In: Safe Management of Wastes from Health-Care Activities. second ed. Geneva, editor. WHO; Switzerland: 2014. [Google Scholar]
- Wu A., Huang X., Gong R.e., Li J., Lu Y., Wang M. Effectiveness of immersion disinfectant on medical waste. Chin. J. Nosoconmiol. 2005;15:51–52. [Google Scholar]
- Yu-Mei M.A., Zhao W., Hong-Yan L. Application progress of hospital wastewater treatment methods. Occup. Health. 2010;26:1180–1182. [Google Scholar]
- Yu B., Zhou Y., Huang Z.W. Research on simple disinfection system for medical wastewater of township hospital. Asian J. Chem. 2014;26:3243–3245. [Google Scholar]
- Yu J.L., Li Q., Yan S.C. Design and running for a hospital wastewater treatment project. Adv. Mater. Res. 2013;777:356–359. [Google Scholar]
- Yu H., Sun X., Solvang W., Zhao X. Reverse logistics network design for effective management of medical waste in epidemic outbreaks: insights from the Coronavirus Disease 2019 (COVID-19) Outbreak in Wuhan (China) Int. J. Environ. Res. Publ. Health. 2020;17:1770. doi: 10.3390/ijerph17051770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S. Technology & Eningeering Application; 2013. Study and Application on Chemical Disinfection Technology of Medical Wastes; pp. 42–44. [Google Scholar]
- Zhang Y., Chen C., Zhu S., Shu C., Wang D., Song J., Song Y., Zhen W., Feng Z., Wu G., Xu J., Xu W. Notes from the field: isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the coronavirus disease 2019 (COVID-19) China CDC Weekly. 2020;2:123–124. [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Liu S., Lu J., Yao M. Annual Meeting of Chinese society of Environmental Sciences; Haikou, China: 2016. Development and Application Prospect of High Temperature Steam Technology of Medical Wastes. 2016. [Google Scholar]
- Zhao F. China Environmental Protection Industry; 2018. Application Research on Disposal Technology for Urban Medical Wastes; pp. 59–62. [Google Scholar]
- Zhao N., Xie Z. Current status and application trend of disposal technology of medical wastes in China. Res. Econ. Environ. Protect. 2018:116–117. [Google Scholar]
- Zhao Y., Jiang Y., Zhang J., Liu D., Zhou Z., Zhou J., Lin X., Li S., Chen S. Levels and characteristic analysis of dioxins in fly ash from waste incinerators of Shenzhen. Acta Sci. Circumstantiae. 2015;35:2739–2744. [Google Scholar]
- Zhu H.M., Yan J.H., Jiang X.G., Lai Y.E., Cen K.F. Study on pyrolysis of typical medical waste materials by using TG-FTIR analysis. J. Hazard Mater. 2008;153:670–676. doi: 10.1016/j.jhazmat.2007.09.011. [DOI] [PubMed] [Google Scholar]
- Zhu Z., Wu C., Zhong D., Yuan Y., Shan L., Zhang J. Effects of pipe materials on chlorine-resistant biofilm formation under long-term high chlorine level. Appl. Biochem. Biotechnol. 2014;173:1564–1578. doi: 10.1007/s12010-014-0935-x. [DOI] [PubMed] [Google Scholar]