The emergence of the coronavirus disease (COVID-19) pandemic has resulted in a global public health emergency [1]. It rapidly spread globally infecting many individuals in many countries. In early March 2020, the World Health Organization designated the disease COVID-19 as a pandemic. Common symptoms include fever, severe headache, loss of smell and taste, dry cough with shortness of breath, general malaise, muscle ache, diarrhea, and abdominal pain [2]. Whereas most cases are mild, some become severe progressing to pneumonia with multiorgan failure and death [3].
Evidence shows that the virus spreads mainly during close contact and via respiratory droplets [4]. It may also be contracted by touching contaminated surfaces on which the virus can live for up to 72 hours [5]. The average time from exposure to onset of symptoms varies between 2 and 14 days, with an average of 5 days [6]. The standard method of diagnosis is by reverse transcription polymerase chain reaction (PCR) from a nasopharyngeal swab 7, 8, 9, although rapid IgM-IgG combined antibody tests are being developed [10].
The recommended measures to prevent infection include frequent hand washing, social distancing (maintaining a physical distance of at least 6 ft from others), and covering the mouth and nose when coughing or sneezing to avoid dispersing droplets of body fluids [11]. Aiming to enforce social distancing and to preserve hospital resources, joint statements have been produced by many professional societies, encouraging the suspension of nonessential medical visits. However, emergencies and procedures in which delay could potentially worsen the patient's outcome must be performed.
There is emerging evidence regarding potential viral dissemination during gynecologic minimally invasive procedures owing to the presence of the virus in blood and stool and the aerosolization of the virus, especially when using smoke-generating devices [12]. This risk is greater during aerosol-generating procedures (AGPs) such as laparoscopy or robotic surgery, especially during bowel surgery interventions, and is minimal during hysteroscopy. Because hysteroscopy is not an AGP, the actual risk is unknown, but the theoretic risk is low.
Hysteroscopy is considered the gold standard procedure for the diagnosis and management of intrauterine pathologies [13]. It is frequently performed in an office setting without the use of anesthesia [13,14]. It is usually well tolerated with only a few patients reporting discomfort [14]. It allows for the diagnosis and the immediate treatment, using the “see and treat” approach, of patients with intrauterine pathologies avoiding the risk of anesthesia, in particular, the need for intubation, which is a procedure with a high risk of droplet contamination in individuals with COVID-19 [15].
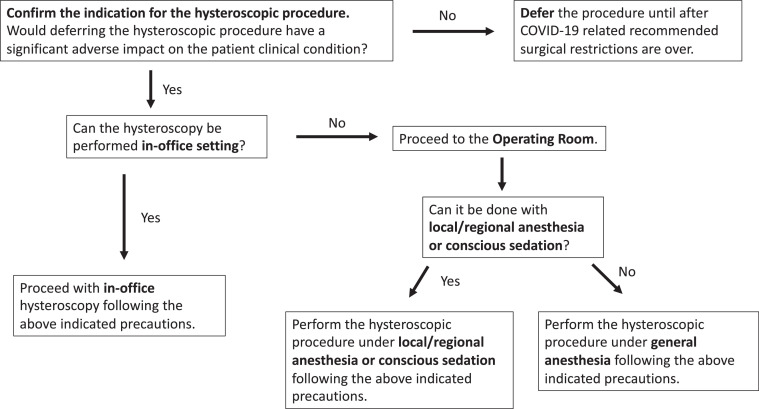
There are several considerations that should guide the clinician who participates in hysteroscopic procedures at this time. Aiming to protect the patients and the healthcare providers by minimizing the risk of viral exposure, the following review will provide recommendations for clinicians performing hysteroscopic procedures during the COVID-19 pandemic. (Fig. 1 ).
Fig. 1.
Algorithm for the triage of a patient requiring hysteroscopic procedures during the COVID-19 pandemic. COVID-19 = coronavirus disease.
Recommendations for Hysteroscopic Procedures during the COVID-19 Pandemic
General Recommendations
-
(1)
Hysteroscopic procedures should be limited to those patients in whom delaying the procedure could result in adverse clinical outcomes [16].
-
(2)
Adequate screening for potential COVID-19 infection, independent of symptoms, and not limited to those patients with clinical symptoms. When possible, a phone interview to triage patients on the basis of their symptoms and infection exposure status should take place before the patient arrives to the hysteroscopic center. Any woman with suspected or confirmed COVID-19 infection should be asked not to come to the hysteroscopic center. Patients with suspected or confirmed COVID-19 infection who require immediate evaluation should be directed to COVID-19 designated emergency areas. Once the patient arrives, a thorough history taking regarding potential viral exposure and physical examination must be performed. Consider preoperative universal COVID-19 testing. Only patients with a negative COVID-19 test (if performed) and a negative history of symptoms (including body temperature <37.3°C) or exposure to COVID-19 should be allowed to enter the unit.
-
(3)
A maximum of 1 adult companion, under the age of 60 years, per patient should be allowed access to the unit when absolutely necessary. It is understood that visitor policy may vary at the discretion of each institution's guidelines. Children and individuals over the age of 60 years should not be granted access to the unit. Companions will be subjected to the same screening criteria as the patients.
-
(4)
If more than 1 patient is scheduled to be at the facility at the same time, ensure that the facility provides adequate space to ensure the appropriate social distancing recommendation between patients. Avoid the presence of multiple individuals in the waiting room at any given time. Ensure that the seating in the waiting room is spaced at least 2 meters apart. Hand sanitizers and face masks should be available for patients and companions. We recommend the use of face masks by all individuals present in the hysteroscopic unit (patients, companions, and staff members). The masks should always be worn, not only during the hysteroscopic procedure.
-
(5)
It is imperative that all healthcare members in close contact with the patient during the procedure wear personal protective equipment (PPE), which includes an apron and gown, a surgical mask, eye protection, and gloves. Extreme caution should be implemented to avoid contamination. Healthcare providers should always wear PPE that is deemed appropriate by their regulatory institutions following their local and national guidelines during clinical patient interaction.
-
(6)
The use of electrosurgery in hysteroscopy is performed in a liquid environment. Bubbles that are generated with the use of thermal energy devices (monopolar, bipolar, or laser) are cooled down rapidly and partly absorbed by the surrounding liquid [17]. Cell fragments generated are contained within the uterine cavity [18]. Any gases that are volatile at ≤37°C and cell fragments are actively suctioned through the outflow channel, in a closed circuit, without an aerosol-generating effect, minimizing any risk of viral dissemination. In addition, it is recommended to avoid multiple insertions and removals of the hysteroscope from inside the uterine cavity.
-
(7)
The participation of learners and physicians in training should be organized by video transmission and not by physical presence in the office or operating room.
-
(8)
In patients with confirmed positive COVID-19 infection and in need of urgent hysteroscopic surgery, the operation should be performed under strict protective conditions ideally in an operating room with negative pressure and independent ventilation.
Hysteroscopy Performed in an Office Setting
Preprocedural Recommendations
-
(1)
Patients should be advised to come to the office alone. If the examination requires a companion, a maximum of 1 companion at the appointment can be accepted. When coming to the unit alone, it is recommended that patients ensure secure transportation that can pick them up after the visit is over to avoid driving immediately after the procedure.
-
(2)
Limit the number of the healthcare team members present in the procedure room.
-
(3)
Favor the use of instruments that do not produce surgical smoke such as scissors, graspers, and tissue retrieval systems.
Intraprocedure Recommendations
-
(1)
Choose a device that will allow an effective and fast procedure.
-
(2)
Use the recommended PPE.
-
(3)
Limit the movement of staff members in and out of the procedure room.
Postprocedure Recommendations
-
(1)
When more than 1 case is scheduled to be performed in the same procedure room, allow enough time in between cases to perform a thorough operating room decontamination.
-
(2)
Allow a patient to recover from the procedure in the same procedure room or in a specific stand-alone patient recovery room, which is subject to the same disinfection rules between 2 patients.
-
(3)
Expedite patient discharge.
-
(4)
Follow-up after the procedure should be by phone or telemedicine.
-
(5)
Standard endoscope disinfection is effective and should not be modified.
Hysteroscopy Performed in the Operating Room
Preprocedural Recommendations
-
(1)
Adequate patient screening for potential COVID 19 infection, independent of symptoms and not limited to those with clinical symptoms.
-
(2)
Limit the number of healthcare team members in the operating procedure room.
-
(3)
Surgeons and staff who are not needed for intubation should remain outside the operating room but be immediately available in case emergency assistance is required, until intubation is completed and should leave the operating room before extubation to minimize unnecessary staff exposure.
Intraprocedure Recommendations
-
(1)
Limit the number of personnel in the operating room to a minimum.
-
(2)
Staff should not go in and out of the room during the procedure.
-
(3)
When possible, use conscious sedation or regional anesthesia to avoid the risk of viral dissemination at the time of intubation/extubation.
-
(4)
Choose a device that will allow an effective and fast procedure.
-
(5)
Favor nonsmoke generating devices such as hysteroscopic scissors, graspers, and tissue retrieval systems.
-
(6)
Active suction should be connected to the outflow, especially when using smoke-generating instruments to facilitate the extraction of surgical smoke.
Postprocedure Recommendations
-
(1)
When more than 1 case is scheduled to be performed in the same room, allow enough time in between cases to perform a thorough operating room decontamination.
-
(2)
Expedite postprocedure recovery and patient's discharge.
-
(3)
After completion of the procedure, remove scrubs and change into clean clothing if available.
-
(4)
Standard endoscope disinfection is effective and should not be modified.
Conclusion
The COVID 19 pandemic has caused a global health emergency. Enforcing social distancing and preserving hospital resources requires suspension of nonessential medical visits. Procedures in which delay could potentially worsen a patient's outcome must be performed. Adequate triage of patients with potential cancer conditions is critical to ensure patient safety during pandemic infections. The theoretic risk of viral dissemination in the operating theater is higher during AGP than hysteroscopy in which the theoretic risk is extremely low or negligible. Always favor the use of mechanical energy over thermal-generating devices. In addition, when needed, use conscious sedation or regional anesthesia to avoid the risk of viral dissemination at the time of intubation/extubation. Healthcare providers must comply with a step-by-step reimplementation of standard operating procedures, expediting the evaluation and the management of all the deferred cases as soon as the benign pathology consultations can be safely restarted. Patients with negative status for COVID-19 confirmed by PCR, requiring hysteroscopic procedures, should be treated using universal precautions.
Disclaimer
These recommendations are based on expert opinion and are meant to serve the general practitioner treating an average patient. They should not be considered rigid guidelines and are not intended to replace clinical judgment. These guidelines are made on the basis of current available information and are likely to change as we gain more knowledge of the disease. Local and national guidelines should take priority over these recommendations. Women tested negative for infection with COVID-19 confirmed by PCR should be managed with standard universal precautions.
Footnotes
The authors declare that they have no conflict of interest.
References
- 1.Al-Shamsi HO, Alhazzani W, Alhuraiji A. A practical approach to the management of cancer patients during the novel coronavirus Disease 2019 (COVID-19) pandemic: an International Collaborative Group. Oncologist. 2020;25:e936–e945. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang X, Yu Y, Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24 doi: 10.1001/jama.2020.2648. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Wang W, Xu Y, Gao R. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 Mar 11 doi: 10.1001/jama.2020.3786. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Doremalen N, Bushmaker T, Morris DH. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu F, Yan L, Wang N. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020 Mar 28 doi: 10.1093/cid/ciaa345. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan JF, Yuan S, Kok KH. A familial cluster of pneumonia associated with the 2019 Novel Coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28 doi: 10.1056/NEJMoa2002032. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Q, Guan X, Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Z, Yi Y, Luo X. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J Med Virol. 2020 Feb 27 doi: 10.1002/jmv.25727. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prem K, Liu Y, Russell TW. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang W, Du RH, Li B. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199–208. doi: 10.1016/j.jmig.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Cicinelli E. Hysteroscopy without anesthesia: review of recent literature. J Minim Invasive Gynecol. 2010;17:703–708. doi: 10.1016/j.jmig.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Association of Gynecologic Laparoscopists. COVID-19: joint society statement on elective surgery. Available at:http://www.aagl.org/news/covid-19-joint-statement-on-elective-surgeries/. Accessed April 5, 2020.
- 17.Farrugia M. University of London; London: 2009. Electrosurgery on the uterus: an investigation of the local and systemic effects [dissertation] [Google Scholar]
- 18.Farrugia M, Hussain SY, Perrett D. Particulate matter generated during monopolar and bipolar hysteroscopic human uterine tissue vaporization. J Minim Invasive Gynecol. 2009;16:458–464. doi: 10.1016/j.jmig.2009.04.006. [DOI] [PubMed] [Google Scholar]