Abstract
The COVID-19 pandemic is spreading globally. COVID-19 has an effect on the systemic state, cardiopulmonary function and primary disease of patients undergoing surgery. COVID-19's high contagiousness makes anesthesia and intraoperative management more difficult. This expert consensus aims to comprehensively introduce the application of perioperative ultrasound in COVID-19 patients, including pulmonary ultrasound and anesthesia management, ultrasound and airway management, ultrasound-guided regional anesthesia and echocardiography for COVID-19 patients.
PERIOPERATIVE ULTRASOUND has been widely used in the field of anesthesiology due to its simplicity, rapidity, practicality, low cost, absence of radiation, and reproducibility. Point-of-care ultrasound has become an indispensable tool for anesthesiologists to evaluate cardiopulmonary status, guide procedures, and manage emergencies.1 , 2 Coronavirus disease 2019 (COVID-19) has become a public health emergency of international concerns,3 and perioperative ultrasound has played important roles in the evaluation and management of COVID-19 patients in China. The Chinese Society of Anesthesiologists aims to provide expert consensus from the authors’ clinical experiences in China on comprehensive applications of point-of-care ultrasound in the care of COVID-19 patients for anesthesiologists worldwide.
All providers should practice meticulous precautions against COVID-19 infections during performance of perioperative ultrasound. The ultrasound equipment, including an ultrasound transducer, should be protected from contamination using plastic covers and disinfected routinely and systemically.
Lung Ultrasound for COVID-19 Patients
In recent years, lung ultrasound has gradually gained popularity in anesthesia practices.4 COVID-19 patients suffer from severe lung injuries, and the pathologic changes includ bronchiolitis and alveolitis, which are accompanied by epithelial cell proliferation, atrophy, and exfoliation.5 In addition, extensive pulmonary interstitial fibrosis, hemorrhagic pulmonary embolism, and massive inflammatory cell infiltration also are observed.5 The average diameter of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is about 120 nm, so it is speculated that the virus particles can be inhaled into the airway and lungs, even into the alveoli. This may explain why the lesions of SARS-CoV-2 viral pneumonia are mainly in the subpleural areas. Because COVID-19 generally begins in the terminal alveoli, which are close to the pleura, pathologies can be observed clearly by lung ultrasound.6 In addition, strict infection control requirements for COVID-19 patients make transport to radiology suites complex and carry high risks of severe hypoxemia. Lung ultrasound has become an important diagnostic tool to rapidly assess the severity of SARS-CoV-2 pneumonia/acute respiratory distress syndrome at presentation, to track the progression of disease, to monitor lung recruitment maneuvers, to evaluate responses to prone position, to guide and manage extracorporeal membrane oxygenation therapy, and to make decisions related to weaning the patient from ventilatory support.7
Lung Ultrasound Examination Procedure
In general, the convex array probe is the probe of choice, and the high-frequency linear array probe is appropriate to monitor pleural or subpleural lesions. Patients are usually examined in the supine position, with the probe perpendicular to the ribs. The anterior axillary line and the posterior axillary line divide the lung of each side into the following 3 areas: the anterior, the lateral, and the posterior area. Each area is further divided into 2 regions—the upper region and the lower region—by the nipple line. All 12 lung areas should be examined comprehensively. It should be noted that there may be a blind spot in the posterior areas due to the shadowing from the scapula.
Characteristics of Lung Ultrasound in COVID-19 Patients
The characteristics of lung ultrasound in COVID-19 patients might vary significantly from patient to patient or from day to day due to different stages of the disease, the severity of the lung lesions, secondary lung lesions caused by dysfunction of other organs, iatrogenic lung lesions, and pre-existing cardiopulmonary diseases. The predominant pattern is of varying degrees of interstitial syndrome and alveolar consolidation, the degree of which are correlated with the severity of the lung injury. COVID-19 lung lesions usually involve the subpleural area, thus abnormalities can be identified easily on lung ultrasound.6 In rare cases, the lung lesions only affect deep lung tissues and cannot be diagnosed by lung ultrasound, and chest computed tomography should be reserved for these patients when ultrasonography cannot answer the clinical question.
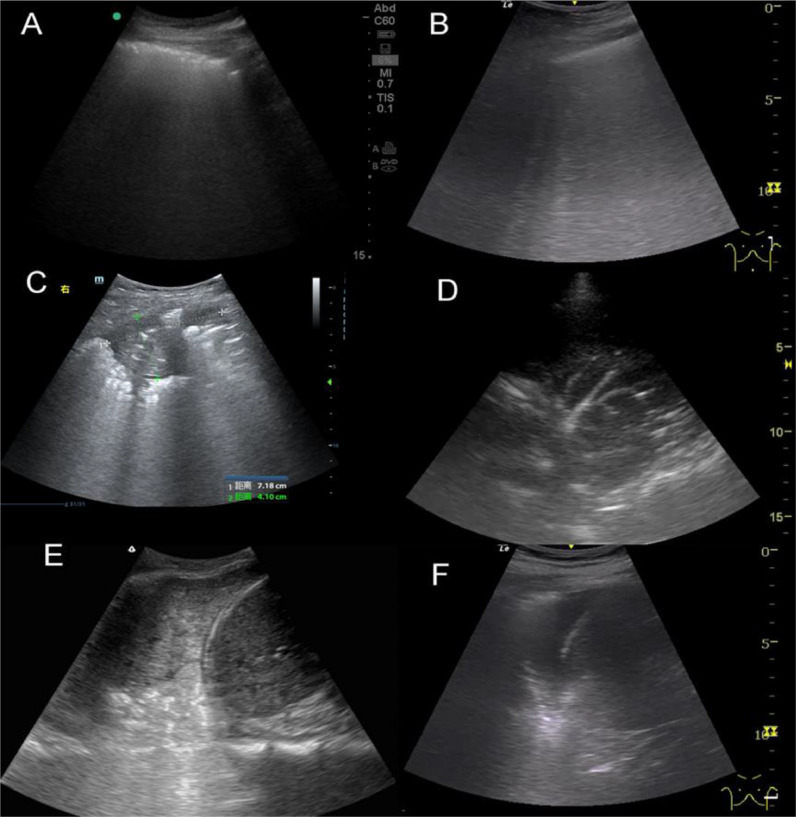
The ultrasonic manifestations of the lung lesions in COVID-19 patients are as follows6 , 7: (1) thickening of the pleural line with pleural line irregularity; (2) B lines in a variety of patterns including focal, multifocal, and confluent; (3) consolidations in a variety of patterns including multifocal small, nontranslobar, and translobar with occasional mobile air bronchograms; (4) appearance of A lines during recovery phase; and (5) pleural effusions that are uncommon (Fig 1 ). The observed patterns occurs across a continuum from mild alveolar interstitial pattern, to severe bilateral interstitial pattern, to lung consolidation.6 , 7 Lesions are mostly located in the posterior fields of both lungs. Multiple discontinuous or continuous fused B lines (waterfall sign) under the pleural line are visible, or diffused B lines (white lung sign) and the A lines disappeared. Compared with the B lines caused by cardiogenic pulmonary edema, the B lines here were more likely to be fused and fixed.8 The B lines had blurred edges and no bifurcation signs. The origination point of the subpleural lesion was more obtuse (convex array probe) compared with that of B lines of pulmonary edema. High- frequency ultrasound could further show that the pleural line was unsmooth, rough, and interrupted mainly due to the decreased gas content and sound wave reflection in the subpleural alveoli and interstitial lesions.
Fig 1.
Typical lung sonographic findings in Coronavirus Disease 2019 patients. (A) Thickened pleural line with pleural irregularity. (B) B lines. (C) Consolidations. (D) Air bronchograms. (E) Tissue-like changes. (F) Pleural effusion.
Multiple small patchy consolidations were observed in the subpleural lesion, and strip consolidation. The echogenicity in the lesions was homogenous or inhomogeneous, and air bronchogram sign was visible (mostly early and progressive stages because secondary pulmonary lobules were involved by interstitial inflammation, the interstitial tissues were thickened and swollen, some bronchioles and alveoli were not involved by high gas content). When symptoms improved, the ultrasound showed irregular nodule subpleural echo shadow, with fused B lines in fixed position, localized pleural thickening, and local pleural effusion around the subpleural lesion.6 In patients with pneumothorax, the pleural sliding sign will disappear, and the lung point sign will be present.9
Color Doppler Flow Imaging shows low blood flow signals in subpleural consolidation, possibly due to the pathologic nature and progression of lesions in COVID-19. This is in contrast to pulmonary consolidation caused by common inflammation, which generally shows abundant blood flow signals.6
Application of Lung Ultrasound in Anesthesia Management of COVID-19 Patients
Preoperative
Lung ultrasound can be used to diagnose the etiology of hypoxemia, manage the ventilator settings, and evaluate fluid status in COVID-19 patients. Along with other modalities, ultrasound can evaluate the lung conditions before the surgery to decide if a patient is optimized. Pleural effusion, pneumothorax, and other pathologies could be managed promptly by a chest tube if indicated. If lung consolidation exists, lung recruitment maneuvers could be attempted to improve oxygenation under ultrasound guidance. If airway obstruction is suspected, endotracheal tube suctioning or fiberoptic bronchoscopy could be performed.
Intraoperative and Postoperative
Lung ultrasound can help to select the best surgical position. For example, COVID-19 patients with poor oxygenation might benefit from prone position if possible, and lung ultrasound can help to monitor the lung status with position changes.10 In addition, lung ultrasound is useful to identify patients at high risk for hypoxemia and atelectasis during and after surgery.11, 12, 13 For these patients, restrictive fluid management, low tidal volume (below 6 mL/kg ideal body weight), and low plateau pressure (<30 cmH2O) protective mechanical ventilation should be adopted.
Ultrasound and Airway Management of COVID-19 Patients
The symptoms of COVID-19 include dyspnea and hypoxemia with bilateral diffuse alveolar injury.5 Airway management is an important part of rescuing these critically ill patients. Timely invasive mechanical ventilation with endotracheal intubation will directly affect the prognosis of COVID-19 patients. Airway ultrasound is helpful to predict difficult airway at bedside, verify correct positioning of the endotracheal tube, assist ultrasound-guided tracheotomy, and evaluate readiness before extubation.
Ultrasound Airway Evaluation
It is critical to evaluate the airway before any intubation. However, for critically ill COVID-19 patients, traditional methods such as Mallampati classification, mouth opening, interincisor gap, thyromental distance, and mandibular protrusion are difficult to perform due to infection control gear on the patient. The thickness of neck soft tissue on the anterior aspect of the trachea, neck circumference, hypomental distance ratio, the width of tongue, and lateral pharyngeal wall can be easily measured by bedside ultrasound to predict difficult airways.14 Multiple layers of personal protective equipment make lung auscultation impossible in COVID-19 patients, and anesthesiologists must rely on end- tidal carbon dioxide and airway ultrasound to verify the presence of endotracheal tube artifacts in the trachea, not the esophagus.15
Ultrasound-guided Tracheotomy
Tracheotomy plays an important role in the care of critically ill COVID-19 patients because many patients require prolonged mechanical ventilation before their lungs eventually recover. Although tracheotomy is considered minimally invasive, the blind technique could reduce the success rate and increase tracheal and adjacent tissue injuries. Ultrasound-guided tracheotomy could improve the success rate of locating the trachea and significantly shorten the procedure, which is particularly beneficial in critically ill COVID-19 patients with severe hypoxemia.16
Ultrasound-assisted Weaning from Mechanical Ventilation and Extubation
When respiratory failure occurs in COVID-19 patients, mechanical ventilation is inevitable. However, prolonged endotracheal intubation leads to tracheal mucosal damage, edema, and granuloma formation. Premature extubation is also detrimental and increases reintubation rate and mortality. During mechanical ventilation weaning, ultrasound should be used to evaluate the status of lung, diaphragm, and chest walls to guide the progress of spontaneous breathing.17 Lung ultrasound also can be used to predict extubation risks, and there is a high possibility of having complications after extubation if the lung ultrasound score is greater than 17.18 , 19 Such COVID-19 patients should remain intubated after surgery and transported to the intensive care unit directly.
Ultrasound-guided Regional Anesthesia
When providing anesthesia to COVID-19 patients, anesthesiologists must wear multiple layers of heavy personal protective equipment that pose many unforeseen challenges. Airway manipulation poses the greatest infectious risks to anesthesiologists and all the healthcare providers in the operating rooms through aerosol generation.20 Ultrasound-guided peripheral nerve block, epidural, or spinal anesthesia could avoid airway manipulations, reduce transmission risks, and improve respiratory functions in COVID-19 patients.21 Regional anesthesia should be preferred whenever possible.21 The ultrasound equipment, including an ultrasound transducer, should be protected from contamination using plastic covers. Spinal anesthesia is not contraindicated in COVID-19 patients and early epidural analgesia is recommended to reduce the need for general anesthesia for emergent cesarean delivery.22
The hand sensation for landmarks will be severely compromised by wearing multiple layers of protective equipment and gloves. If possible, real-time ultrasound-guided spinal or epidural anesthesia should be performed due to their high success rates.23 Attempts should be made to choose the block that is least likely to interfere with respiratory function. In other words, axillary or infraclavicular brachial plexus block should be chosen over supraclavicular brachial plexus block, and superior trunk block or other alternatives are preferred over interscalene block.21 Ultrasound guidance makes these peripheral nerve blocks safer, easier, and quicker. In addition, these blocks should be performed with ultrasound guidance to reduce the risk of local anesthetic systemic toxicity. It may be advisable to choose a block that does not require patient repositioning over those that require repositioning if appropriate. Ultrasound-guided transverse abdominous plane block and ilioinguinal block may provide excellent postoperative analgesia in respiratory-compromised COVID-19 patients.21 , 24
Perioperative Echocardiography in COVID-19 Patients
There is an association between pre-existing cardiovascular disease and severe COVID-19, and patients with cardiovascular comorbidities suffer a higher mortality rate.25 Myocardial injury, myocarditis, acute coronary syndromes, cardiac arrhythmia, cardiomyopathy, and cardiac arrest are common sequelae and certainly could happen perioperatively in COVID-19 patients.25, 26, 27 Bedside echocardiography is an invaluable tool to monitor the cardiovascular functions of COVID-19 patients perioperatively.
Recommended Views for Transthoracic Echocardiography
Transesophageal echocardiography is an aerosol-generating procedure and should be avoided, if possible, to reduce infections. Transthoracic echocardiography should be used instead. Parasternal long-axis, parasternal short-axis, apical 4-chamber, 2-chamber, and 5-chamber views, subxiphoid views, and inferior vena cava measurements with and without color Doppler should be obtained and stored.
Evaluate Hemodynamic Status With Echocardiography in COVID-19 Patients
The main factors affecting hemodynamics include cardiac preload, pump function, and cardiac afterload. Preload parameters include left ventricular end-diastolic volume, left atrial pressure estimation, inferior vena cava diameter, and respiratory variation. Left ventricular systolic function includes ejection fraction by M mode, modified Simpson method, left ventricular outflow tract time-velocity time integral, and three-dimensional calculations. Left ventricular diastolic function is assessed with the E and A waves of mitral valve diastolic blood flow, the tissue Doppler E' and E'/E ratio. Right ventricular systolic function can be measured with right ventricular fractional area change, tricuspid plane annular systolic exertion, right ventricular wall strain and strain rate, and three-dimensional method.
COVID-19 Specific Echocardiography
Hemodynamic disorders in COVID-19 patients could be from septic shock, hypoxemia, deterioration of pre-existing cardiovascular diseases, or innate myocardial damage from SARS-CoV-2.5 Patients with COVID-19 may not have completed an echocardiogram before surgery. If the patient has a history of cardiovascular disease or the patient is currently hemodynamically unstable, a focused bedside echocardiogram should be performed in the operating room to assess the structure and function of the heart, guide the volume replacement, and cardiac medications use during surgery.
The incidence of hypotension seems to be high in parturient patients with COVID-19 undergoing cesarean section under neuraxial anesthesia.28 Evaluation of the volume status with echocardiography is crucial to avoid congestive heart failure, respiratory dysfunction, and organ hypoperfusion.
In conclusion, perioperative point-of-care ultrasound is a useful tool in COVID-19 patients to assess the cardiopulmonary function, manage the airway, and guide procedures. Proper application of perioperative ultrasound could improve safety and prognosis of COVID-19 patients.
Conflict of Interest
None
Footnotes
This study was supported by National Key Research and Development Program of China (2018YFC2001800) and National Key Research and Development Program of China (Grant No. 2018YFC 2001900)
References
- 1.Marhofer P., Greher M., Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005;94:7–17. doi: 10.1093/bja/aei002. [DOI] [PubMed] [Google Scholar]
- 2.McCormick T.J., Miller E.C., Chen R. Acquiring and maintaining point-of-care ultrasound (POCUS) competence for anesthesiologists. Can J Anaesth. 2018;65:427–436. doi: 10.1007/s12630-018-1049-7. [DOI] [PubMed] [Google Scholar]
- 3.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. Accessed April 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouhemad B., Mongodi S., Via G. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology. 2015;122:437–447. doi: 10.1097/ALN.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 5.Xu Z., Shi L., Wang Y. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. Accessed April 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang Y, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19);2000. Available at: 10.2139/ssrn.3544750. Accessed February 26, 2020. [DOI]
- 7.Peng Q.Y., Wang X.T., Zhang L.N. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05996-6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volpicelli G., Skurzak S., Boero E. Lung ultrasound predicts well extravascular lung water but is of limited usefulness in the prediction of wedge pressure. Anesthesiology. 2014;121:320–327. doi: 10.1097/ALN.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 9.Lichtenstein D., Meziere G., Biderman P. The “lung point”: An ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26:1434–1440. doi: 10.1007/s001340000627. [DOI] [PubMed] [Google Scholar]
- 10.Haddam M., Zieleskiewicz L., Perbet S. Lung ultrasonography for assessment of oxygenation response to prone position ventilation in ARDS. Intensive Care Med. 2016;42:1546–1556. doi: 10.1007/s00134-016-4411-7. [DOI] [PubMed] [Google Scholar]
- 11.See K.C., Ong V., Tan Y.L. Chest radiography versus lung ultrasound for identification of acute respiratory distress syndrome: A retrospective observational study. Crit Care. 2018;22:203. doi: 10.1186/s13054-018-2105-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riviello E.D., Buregeya E., Twagirumugabe T. Diagnosing acute respiratory distress syndrome in resource limited settings: The Kigali modification of the Berlin definition. Curr Opin Crit Care. 2017;23:18–23. doi: 10.1097/MCC.0000000000000372. [DOI] [PubMed] [Google Scholar]
- 13.Song I.K., Kim E.H., Lee J.H. Effects of an alveolar recruitment manoeuvre guided by lung ultrasound on anaesthesia-induced atelectasis in infants: A randomised, controlled trial. Anaesthesia. 2017;72:214–222. doi: 10.1111/anae.13713. [DOI] [PubMed] [Google Scholar]
- 14.Garg R., Gupta A. Ultrasound: A promising tool for contemporary airway management. World J Clin Cases. 2015;3:926–929. doi: 10.12998/wjcc.v3.i11.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y., Wang J., Wei X. Confirmation of endotracheal tube depth using ultrasound in adults. Can J Anaesth. 2015;62:832. doi: 10.1007/s12630-015-0359-2. [DOI] [PubMed] [Google Scholar]
- 16.Sustic A., Kovac D., Zgaljardic Z. Ultrasound-guided percutaneous dilatational tracheostomy: A safe method to avoid cranial misplacement of the tracheostomy tube. Intensive Care Med. 2000;26:1379–1381. doi: 10.1007/s001340000589. [DOI] [PubMed] [Google Scholar]
- 17.Osman A., Sum K.M. Role of upper airway ultrasound in airway management. J Intensive Care. 2016;4:52. doi: 10.1186/s40560-016-0174-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva S., Ait Aissa D., Cocquet P. Combined thoracic ultrasound assessment during a successful weaning trial predicts postextubation distress. Anesthesiology. 2017;127:666–674. doi: 10.1097/ALN.0000000000001773. [DOI] [PubMed] [Google Scholar]
- 19.Soummer A., Perbet S., Brisson H. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress. Crit Care Med. 2012;40:2064–2072. doi: 10.1097/CCM.0b013e31824e68ae. [DOI] [PubMed] [Google Scholar]
- 20.Tran K., Cimon K., Severn M. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uppal V., Sondekoppam R.V., Landau R. Neuraxial anaesthesia and peripheral nerve blocks during the COVID-19 pandemic: a literature review and practice recommendations. Anaesthesia. 2020 doi: 10.1111/anae.15105. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bauer M., Bernstein K., Dinges E. Obstetric anesthesia during the COVID-19 pandemic. Anesth Analg. 2020 doi: 10.1213/ANE.0000000000004856. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Y., Qian W., Ke X.J. Real-time ultrasound-guided spinal anesthesia using a new paramedian transverse approach. Curr Med Sci. 2018;38:910–913. doi: 10.1007/s11596-018-1961-7. [DOI] [PubMed] [Google Scholar]
- 24.Liu Y., Ke X., Wu X. Ultrasound-guided lumbar plexus block in supine position. Anesthesiology. 2018;128:812. doi: 10.1097/ALN.0000000000001939. [DOI] [PubMed] [Google Scholar]
- 25.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. doi: 10.1016/j.jacc.2020.03.031, Accessed March 2020. [DOI] [PMC free article] [PubMed]
- 26.Zeng J.H.L., Liu Y.-X., Wang F. First case of COVID-19 infection with fulminant myocarditis complication: Case report and insights. Preprints. 2020 doi: 10.1007/s15010-020-01424-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li X., Guo Z., Li B. Extracorporeal membrane oxygenation for coronavirus disease 2019 in Shanghai, China. ASAIO J. 2020;66:475–481. doi: 10.1097/MAT.0000000000001172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen R, Zhang Y, Huang L, et al. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: A case series of 17 patients [e-pub ahead of print]. Can J Anaesth. doi: 10.1007/s12630-020-01630-7, Accessed March 2020. [DOI] [PMC free article] [PubMed]