Dear editor,
Tian et al. and Yang et al. have reported characteristics of Coronavirus Disease 2019 (COVID-19) from the perspectives of clinic, epidemiology and imaging manifestations.1 , 2 Here we would like to share our experience of airborne precautions for bedside fiberoptic bronchoscopy examination. The pandemic COVID-19 has become a global threat with 170,000 confirmed cases globally as of Mar 16, 2020. In China, there were 80,000 comfirmed cases, in which 3226 were critically ill patients.3 The mortality rate for the critically ill patients were reported as over 50% by World Health Organization.4 One key reason might be the difficulty with expectoration of secretions. Autopsy showed that the alveolar cavity of patients with COVID-19 was full of serous and fibrin exudate.5 The typical pathologic change was clear membrane formation. Methods to decrease retention of secretions in critically ill patients include percussion, a prone position and endotracheal suctioning. However, since endotracheal suction catheters only reach the main bronchus but not the smaller airways, fiberoptic bronchoscopy has been suggested for diagnosis and treatment when necessary.6 This procedure has been shown to improve respiratory function which can lead to recovery. In addition, a higher rate of confirmed diagnosis of COVID-19 was noticed compared using throat swab.7
Beside the existing value of fiberoptic bronchoscopy in diagnosis and treatment, the potential risk to the health care givers during this procedure should be considered. Aerosol contamination of the environment is increased because the patient's upper respiratory tract is exposed for an extended period. Airborne and contact precautions are critical for the health care team. In addition to strict environmental precautions, decontamination of equipment is another consideration. Tongji Hospital is the largest hospital in central China, and it is a designated center for care of critically ill patients with COVID-19. After the outbreak of the epidemic, two general wards were converted to temporary intensive care units (ICUs) with 72 beds for critical cases of COVID-19 in February 2020.
Preparation prior to fiberoptic bronchoscopy
Patients assessment and care
Not all patients with COVID-19 should undergo a fiberoptic bronchoscopy examination. The client's basic condition, blood gas results, nucleic acid testing and extent of pulmonary secretions should be taken into consideration. The primary focus should be on limiting environmental contamination by aerosol spread of the virus. Four criteria were added which became indicators for use of bronchoscopy in the care of a patient with COVID-19: ① receiving mechanical ventilation, ② severe atelectasis found on chest x-ray revealing a large area of reduced transparency in both lung tissues, ③ suctioning does not clear secretions and PO2≤40 mmHg, ④ throat swab is negative for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nuclei acid but patient was highly suspected for COVID-19. Any patient meeting the first criteria and any one of the other three was deemed appropriate for fiberoptic bronchoscopy.
To avoid choking, patients were pain relieved and sedated by fentanyl, midazolam and/or diprivan to reach a Richmond Agitation-Sedation Scale (RASS) rating of ≤ −4. As closed endotracheal suctioning is commonly used in invasive mechanically ventilated patients with COVID-19, the suction tube should also be removed as it may obstruct the bronchoscope. Since ventilation is suspended when removing the suction catheter, two staff members should work together to contain any aerosol dispersion.
Staff preparation
It is important to make staff aware of the potential challenges to avoid aerosol exposure. Training for personnel included wearing a protective suit, isolation gown, goggles, shoe covers, surgical mask with face shield, gloves and positive pressure hood. Isolation packs included the required items. The appropriate technique for donning and removal of these items was also covered. Posters on the use of this equipment were also placed in appropriate areas. Staff checked each other before entering or returning from a contaminated area. Personnel involved in a fiberoptic bronchoscopy included one physician, one nurse and one nursing assistant.
Environment and supplies
This procedure should be done ideally in a negative airflow room. Since the temporarily established ICUs for COVID-19 did not meet this criteria, modifications were made as following. Each room was equipped with two air exchange fans with an air velocity of 160L/s.8 Additionally, an air sterilizer and ultraviolet radiation units were also used. Patient beds in this large open unit were at least 1 meter apart. Other supplies needed for the bronchoscopy were available in a pack, including sterile gloves, sterile scissors, dressings, disposable towels, gauze, syringes, specimen collection containers, disposable bowl, vials of normal saline and lidocaine, fiberoptic bronchoscope, spray bottle of chlorine-based antiseptic solution and alcohol-based hand sanitizer.
Fiberoptic bronchoscopy precaution strategies
Precaution strategies for fiberoptic bronchoscope were showed in Table 1 and Fig 1 .
Table 1.
Fiberoptic bronchoscopy precaution strategies.
| Procedures | Notes |
|---|---|
| 1. Enter unit, close door and verify patient's information. | |
| 2. Adjust ventilator oxygen concentration to 100%. | Monitor patient's vital signs |
| 3. Physician prepares bronchoscope; nurse prepares patient and needed supplies; nursing assistant connects power and suction device. | Patient should be deeply sedated (RASS ≤ −4) to avoid chocking; make sure balloon pressure is appropriate. |
| 4. Assistant suspends ventilation prior to bronchoscope insertion into the airway. | Minimize aerosol dispersion |
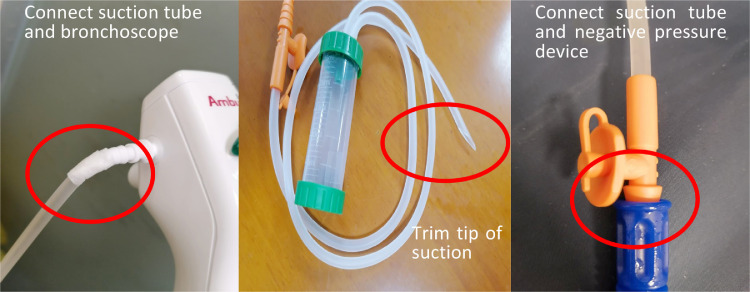
| 5. Nurse assists physician to collect secretion specimens using closed collection method (see Fig. 1). | Minimize scope withdrawal from the airway to reduce aerosol exposure |
| 6. Similarly, assistant suspends ventilation prior to bronchoscope withdrawal from the airway. | Minimize aerosol dispersion |
Fig. 1.
Method to connect bronchoscope and specimen container.
Decontamination of bronchoscope and environment following procedure
Disinfection of fiberoptic bronchoscope
In view of the current method used for cleaning equipment and the COVID-19 epidemic, a new procedure was developed for disinfection of the fiberoptic bronchoscope.9 Changes and rationales were described in Table 2 .
Table 2.
Disinfection procedure, revisions and rationales.
| Procedures | Traditional methods | Revised methods | Rationales |
|---|---|---|---|
| Preprocess | Preprocess at bedside | Packed in disposable biocontainment bag and preprocess occurs in designated room | Reduce the spread of pathologic organisms |
| Manual cleaning | Bronchoscope immersed in enzyme solution for 5–10 min | Bronchoscope immersed in enzyme solution for 15–20 min | Promote enhanced breakdown of microorganism protein |
| Brush inserted to clean bronchoscope | Large syringe filled with enzyme solution is used to repeatedly flush the bronchoscope and tubing | Avoid spills during cleaning | |
| Drying | Inflated with air for 30 s to dry | ||
| Machine cleaning | Machine specially used for fiberoptic bronchoscope cleaning and disinfection | ||
| Flushing | Sterile purified water used to flush bronchoscope | ||
| Drying | 75% alcohol used to flush bronchoscope followed by inflation with air for 30 s | Bronchoscope flushed with 75% alcohol then immersed in alcohol for 10 minutes followed by inflation with air for 30 s | To prolong disinfection time |
| Storage | Placed in cabinet | Exposure to ultraviolet lamp for one hour prior to storage in cabinet | Ultraviolet rays inactivate the virus |
3.2. Environmental cleaning
The use of ultraviolet light, chlorine-based disinfectant and 75% alcohol have been confirmed to be effective in neutralizing the virus.6 A 2000 mg/L sodium hypochlorite disinfectant solution was used to wipe the bedside table and patients’ stretchers; a 1000 mg/L sodium hypochlorite solution was used to clean floors. Following the procedure, involved personnel were sprayed with a 1000 mg/L sodium hypochlorite solution before removing their outermost isolation gown. The reusable positive pressure hoods were wiped using a 2000 mg/L sodium hypochlorite solution, and then placed in biocontainment bags and send to the disinfection center. Since chlorine-based disinfectants are corrosive, the ventilator was disinfected using a 75% alcohol solution.
To date, 22 fiberoptic bronchoscopy exams have been done on 16 patients. Microbiological testing of the bronchoscope was deemed appropriate after disinfection. A total of 18 specimens were collected with 16 were positive for SARS-CoV-2. Throat swabs and sputum specimens were done simultaneously. Nine of these throat swabs were positive while 12 of these sputum specimens were positive, respectively. All staff had no confirmed infection.
Conclusions
The mortality rate for critically ill patients with COVID-19 is high. Retention of secretions represents an important challenge to health caregivers, but fiberoptic bronchoscopy examination might be valuable in optimize the prognosis of COVID-19 patients. It has already showed existing value in diagnosis and treatment. However, the potential risk to the health care givers during this procedure should be considered. This study explain detailed preparation, precaution strategies and decontamination of bronchoscope and environment and respective rationales. Our results proved its effectiveness in diagnosis and safety in staff protection both. This might provide helpful information to facilitate the using of fiberoptic bronchoscopy in the setting of pandemic COVID-19 outbreak worldwide.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
This work is supported by the National Natural Science Foundation of China under Grant No. 71874063.
References
- 1.Yang W, Cao Q, Qin L. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):A multi-center study in Wenzhou city, Zhejiang, China[J] J Infect. 2020;80(4):388–393. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tian S, Hu N, Lou J. Characteristics of COVID-19 infection in Beijing[J] J Infect. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. 2020. Coronavirus disease 2019 (COVID-19) Situation Report-56. Retrieved 2020-4-16 from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200316-sitrep-56-covid-19.pdf?sfvrsn=9fda7db2_6
- 4.World Health Organization. 2020. Coronavirus disease 2019 (COVID-19) Situation Report-41. Retrieved 2020-4-16 from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200301-sitrep-41-covid-19.pdf?sfvrsn=6768306d_2.
- 5.Liu Q, Wang RS, Wang YY. Gross examination report of a COVID-19 death autopsy. J Forensic Med. 2020;36(1):19–21. doi: 10.12116/j.issn.1004-5619.2020.01.005. (in Chinese) [DOI] [PubMed] [Google Scholar]
- 6.National Health Commission of People's Republic of China. 2020. The 7th scheme for diagnosis and treatment of new coronavirus pneumonia. Retrieved 2020-3-16 fromhttp://www.nhc.gov.cn/yzygjs7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf.
- 7.World Health Organization. 2020. Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases. Retrieved 2020-3-11 fromhttps://www.who.int/publicationsdetail/laboratory-testing-for-2019-novel-coronavirus-insuspected-human-cases-20200117.
- 8.World Health Organization. 2020. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Retrieved 2020-3-16 fromhttps://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125.
- 9.Ministry of Health of People's Republic of China Standard for endoscope disinfection. Chinese Nurs Manag. 2004;4(3):11–13. (in Chinese) [Google Scholar]