Highlights
-
•
The CDC recommends not touching the eyes to prevent 2019-nCoV
-
•
Non-hermetically sealed eye protection does not protect the eyes against airborne particulates
-
•
Hermetically sealed goggles protect the eyes, but tend to fog up, which is a barrier to use
-
•
A filtered eye mask (FEM) is a design to both protect the eyes from particulates and prevent fog
-
•
An FEM may help to mitigate the spread of 2019-nCoV and should be researched further
Keywords: Coronavirus, COVID-19, Eye protection, Filtered eye mask (FEM)
Abstract
Objective
Non-hermetically sealed eye protection does not fully protect the eyes from airborne particles. Hermetically sealed eye protection fully protects the eyes from particles, but tends to fog up, rendering it unusable. This study aimed to build and test a filtered eye mask (FEM) to protect the eyes from airborne particles, while being usable without excessive fog build up.
Methods
The steps performed to build the FEM were described. A hermetically-sealed standard eye mask (SEM) and an FEM were examined at 1-minute, 5-minute and 60-minute periods for performance metrics relating to fog.
Results
The SEM showed minimal fog at 1 minute, lots of fog at 5 minutes and was dripping with condensation at 60 minutes. The FEM was clear at 1 minute, 5 minutes and showed minimal fog at 60 minutes.
Conclusion
An FEM may play an important role in preventing novel coronavirus (COVID-19) exposure by protecting the eyes from airborne particles and preventing fog, rendering it usable. Further research is strongly recommended.
1. Introduction
The 2019 novel coronavirus (COVID-19) originated in Wuhan City, Hubei Province, China with clinical manifestations similar to those of the severe acute respiratory syndrome (SARS) outbreak in 2003 (Huang et al., 2020, Li et al., 2020, Phan et al., 2020). In a matter of months, the COVID-19 outbreak has rapidly evolved into a global pandemic. At the time of writing this, COVID-19 has infected over 2,000,000 people and has claimed the lives of over 125,000, with the numbers growing daily (Worldometer, 2020).
Since there is no currently available vaccine to prevent a COVID-19 infection, the best method to prevent the infection is by avoiding exposure. The Centers for Disease Control and Prevention (CDC) has published online information relating to prevention (CDC, 2020). To prevent acquiring the infection through the eyes, the CDC recommends that all people avoid touching their eyes. Many hospitals also recommend wearing eye protection to minimize risk of transmission. There are well-documented limitations of the currently existing eye protection as either (1) non-hermetically sealed (i.e. not air-tight), wherein viruses may contact the user's eyes; or (2) hermetically sealed (i.e. air-tight), wherein the mask fogs up, limiting the user's ability to perform tasks.
The purposes of this paper were to: (1) review the strengths and limitations of eye protection currently available on the market; and (2) introduce a novel filtered eye mask (FEM), which holds promise in overcoming limitations of conventional eye protection. A technical discussion of how the FEM was built and the results of initial testing are provided along with a discussion on various design considerations. Finally, the scope of this paper focused on isolated eye protection devices. Full head gas masks or body suits, which protect the eyes along with other body parts, are not discussed in this paper. While such protection strategies may be effective, they are expensive, burdensome and hinder verbal communication, and are unlikely to be appropriate for long-term use for the everyday citizen.
2. Current eye protection options
There are currently two main categories of isolated eye protection devices available for purchase in the market: (1) non-hermetically sealed eye protection (i.e. not air-tight) and (2) hermetically sealed eye protection (i.e. air-tight seal).
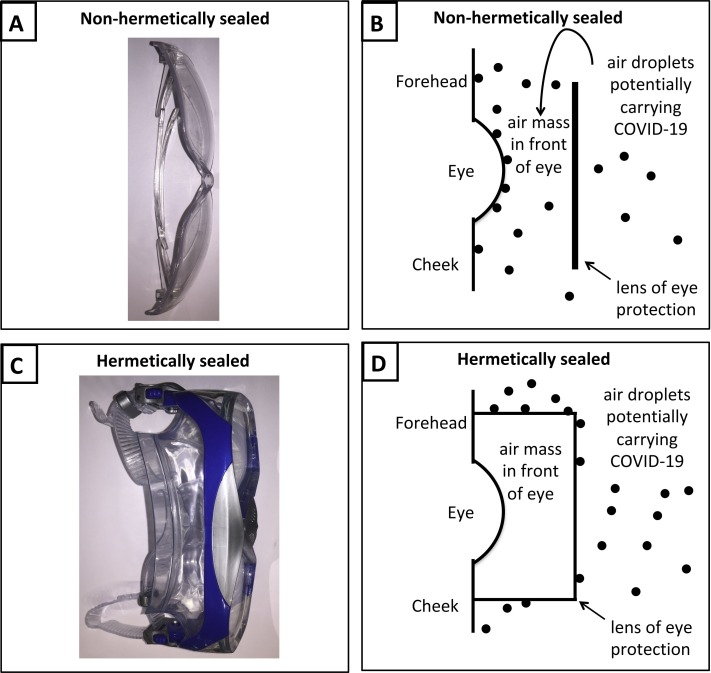
With respect to non-hermetically sealed eye protection (Fig. 1A), some droplets will be stopped and some protection achieved. For example, in the event of a sneeze directed towards the lenses of the eye protection device, many particles will be stopped. However, it is still possible that airborne particles carrying the virus can pass around the lenses and come in contact with the eyes. This is because the droplets from the external environment can pass over, under or around the lenses, enter the air mass in front of the eye and contact the surface of the eye (Fig. 1B).
Fig. 1.
Pictures of non-hermetically sealed and hermetically sealed eye protection devices. Figure 1A shows a photo of a non-hermetically sealed eye protection device. Figure 1B illustrates droplets potentially carrying COVID-19 passing over the top of the lens into the air mass in front of the eye and contacting the surface of the eye. Figure 1C shows a photo of a hermetically sealed eye protection device. Figure 1D illustrates droplets potentially carrying COVID-19 contacting the outer surface of the lens; however, the air mass in front of the eye remains virus-free.
With respect to hermetically sealed eye protection (Fig. 1C), the droplets do not enter the air mass in front of the eye (Fig. 1D). However, a key limitation is the limited usability due to the fact that they fog up, which is well documented in the literature and is a main cause of poor compliance (Chughtai et al., 2020, Dain et al., 1999). This is because the lacrimal glands keep forming tears, which evaporate into the contained space. Condensation subsequently forms on the inner surface of the hermetically sealed eye protection and limits usability.
3. Technical development
Overview: The technical development is a filtered eye mask (FEM) comprising an eye protection device with a filter to maintain a virus-free air mass in front of the eye, which overcomes the limitation of condensation build up in hermetically sealed eyewear (which is well documented to cause poor usability and poor compliance).
Participant: Testing was performed on a single user by author D.D.
Methods: Two devices were used for testing. The first device was a hermetically-sealed standard eye mask (SEM) straight out of the box, which could be hermetically sealed to the face. The second device was an FEM, constructed using the steps below.
Materials: The materials included: a swimming mask; an medium-sized N95 respiratory mask (i.e. for the nose and face); a drill with a dime-sized drill bit; a roll of double-sided tape; and a role of packing tape.
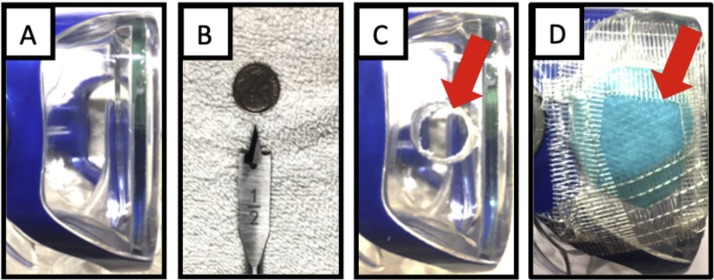
Construction: The FEM was created with the following five steps: 1. The site of drilling was determined, as shown in Fig. 2A. The side of the swimming mask was selected so that it did not block the field of view. 2. A dime-sized hole was drilled into the side of the swimming mask, as shown in Fig. 2B. 3. A quarter-sized air filter was cut out of the N95 mask. 4. A layer of double-sided tape was placed such that one sticky surface of the tape contacted the outside of the swimming mask near the hole and the other sticky surface of the tape contacted the inner portion of the cut-out N95 filter. Care was taken not to cover the opening in the swimming mask with tape. 5. The sides of the cut-out N95 filter were reinforced with packing tape.
Fig. 2.
Pictures obtained from the materials and methods. Figure 2A illustrates the side of the mask. Figure 2B illustrates the drill used, showing that the drill bit was approximately the size of a dime. Figure 2C illustrates the hole, as indicated by the red arrow, in the side of the mask created by the drill. Figure 2D illustrates the cut-out N95 mask, as indicated by the red arrow, reinforced with packing tape.
Analysis: Three time points were assessed: after 1 minute, 5 minutes and 60 minutes of wear. At each time point, two data points were assessed. The first data point was whether or not the mask fogged up and the subjective degree of fog. The second data point whether or not the user could read the words in a book.
4. Results
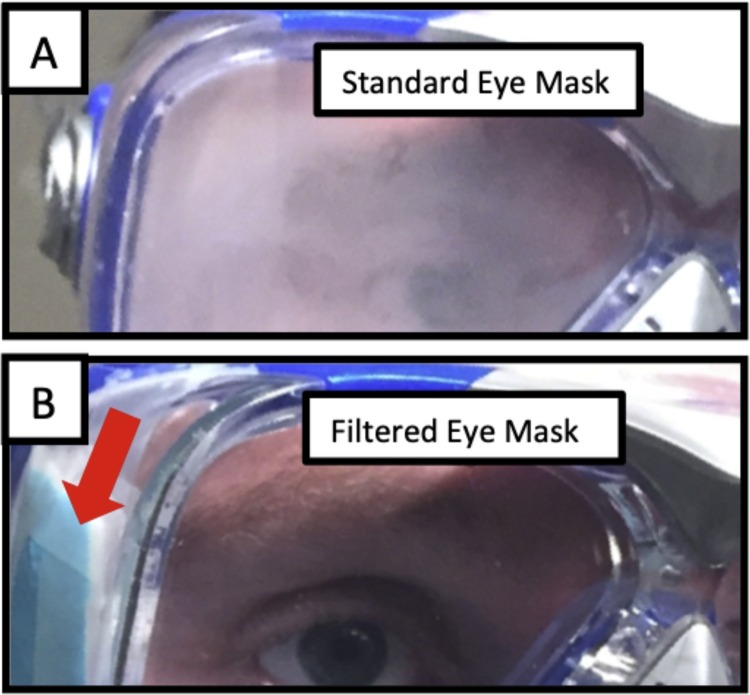
There was a clear difference in the amount of fog seen in the SEM and FEM, as shown in Fig. 3 and Table 1 below.
Fig. 3.
Photograph of standard eye mask and filtered eye mask at 5 minutes. Figure 3A illustrates the SEM after 5 minutes of wear. Note the fog build up in the mask. Figure 3B illustrates the FEM after 5 minutes of wear. Note that there was no build up of fog.
Table 1.
Comparison between the standard eye mask and filtered eye mask over three time points.
| 1-minute time point | 5-minute time point | 60-minute time point | |
|---|---|---|---|
| Standard eye mask (SEM) | Slightly foggy; difficult to read a book | Very foggy; unable to read a book | Dripping with condensation; unable to read a book |
| Filtered eye mask (FEM) | Clear; easy to read a book | Clear; easy to read a book | Minimal fog; easy to read a book |
5. Discussion
Eye protection is critical for preventing person-to-person spread of COVID-19. The ideal eye protection method would meet three important criteria.
First, and foremost, it must be effective at preventing the virus from causing infection through the eye. The exact risk of the infection through airborne particles is still unknown; however, the goal of eye protection must be to prevent the virus from contacting the surface of the eye. Eye protection will also help remind the person not to touch their eye out of habit. It should be noted that the experiment in this article did not test for viral concentration or droplet concentration in the air mass in front of the eyes. The hypothesis that the FEM would result in as good protection against transmission as the hermetically sealed SEM was therefore untested. Thus, it is quite crucial to test the efficacy of the filter-attaching system in terms of airborne particle transmission through the edges of the filter/mask attachment side before commercializing such a product, otherwise wearing such a mask would not protect a person from being infected through the eyes.
Second, the eye protection must be designed in such a way that a user wears it with high compliance. For example, a user would need to be able to perform the tasks of daily living (e.g. delivering medications, drawing blood, going to the grocery store, reading small print, etc.) while wearing the eye protection. If the eye protection fogs up, the user's compliance has been shown to drop (Chughtai et al., 2020, Dain et al., 1999), which will render the user at higher risk of infection.
Third, an important yet overlooked aspect of an outbreak is the adverse mental health effects, including high levels of stress (Douglas et al., 2009). Personal protective equipment (PPE) is critically important to healthcare workers’ physical and mental health (Gold, 2020). In fact, nurses across the country have protested due to a lack of PPE (McNamara, 2020). Having appropriate equipment, including quality eye protection (i.e. effective and of good compliance) will help a user to perform the activities of daily living and mitigate stress.
How could an FEM work in with the overall prevention strategy? The FEM is meant to be worn along with a high-efficiency respiratory mask (e.g. N95). The FEM will prevent exposure of COVID-19 through the eyes. The high-efficiency respiratory mask will prevent exposure of COVID-19 through the respiratory system. Together, the FEM plus the high-efficiency respiratory mask yield more comprehensive protection.
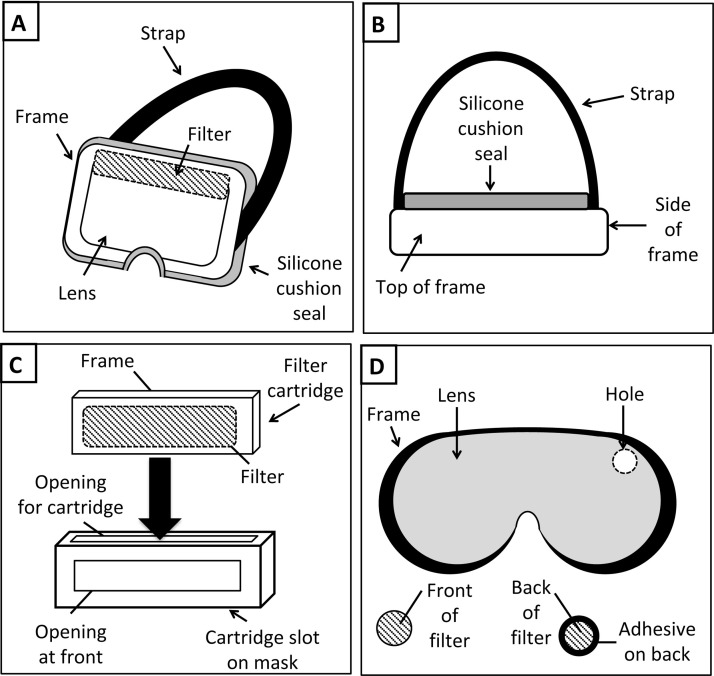
With respect to the FEM design, the materials and construction methods in this paper were meant to be illustrative to clearly convey the concept of an FEM to readers. A wide range of designs could achieve the function, as described in this paper, such as is shown in Fig. 4 . Several design considerations to maximize effectiveness and compliance and minimize costs are discussed in Table 2 below.
Fig. 4.
Illustration of various design considerations for a filtered eye mask (FEM). Figure 4A illustrates a front-oblique view of an FEM design with a large, high-efficiency filter on the top portion of the lens of the mask. The top position of the filter could potentially help to more efficiently eliminate water vapor. An air-filled silicone tube is utilized to create an air-tight silicone cushion seal with the user's face. Figure 4B illustrates a top-down view of the design in Figure 4A. Note that the frame creates a separation between the face and the lens, which is designed to fit over prescription glasses. Figure 4C illustrates a front view of a filter cartridge with a frame and filter. The filter cartridge is placed (large arrow) into the cartridge slot on an FEM. Note that there is an opening at the top where the filter cartridge is slid in and an opening at the front for ventilation, wherein the air mass in front of the eyes remains clean and virus-free. An air-tight design of the cartridge is important to prevent any non-filtered air from entering into the FEM. Figure 4D illustrates an alternative design, wherein the FEM has a hole on the front of the lens. This hole can be covered with a small replaceable filter with an adhesive portion to secure it to the lens. Additional filters could be implemented, so as to improve virus-free air flow through the mask. Note that the FEM is meant to be worn in conjunction with a separate respiratory mask during times at which a user is exposed, such as working in the intensive care unit on active COVID-19 patients. After high-risk exposure is finished, the filter can be discarded and the goggles washed. The goggles can be reused with a fresh filter placed prior to a subsequent exposure.
Table 2.
Design considerations for a filtered eye mask (FEM).
| Design options | Considerations for optimization |
|---|---|
| Mask material | Capable of being washed to eliminate build up of potentially dangerous particles on the outside of the mask (e.g. with soap and water). |
| Filter types | Optimal protection against virus particles contacting the eyes is via a high-efficiency air filter (e.g. N95 and N100). A higher protection efficiency filter (e.g. N100) may be used for higher-risk activities (e.g. prolonged direct contact with an active COVID-19 patient). |
| Technique of filter replacement | A removable and replaceable filter would be cost-effective (e.g. filters could come in small packages, opened and be secured in place via clamps, buckles or straps). |
| Frequency of filter replacement | Optimal protection will be achieved when a new filter is placed on the eye protection each time it is used, although reuse of filters can be performed under specialized protocols if supplies are short (e.g. quarantine used filters for a specified period of time). |
| Securing filter to the mask | Reliable seal during use is essential to keep the air mass in front of eyes virus-free (e.g. cartridge fixation may prove more effective than tape, which has the potential to fall off and ruin the seal). |
| Size of filter | Optimum size may depend on multiple factors, including moisture content of user (e.g. amounts of natural tears, perspiration, etc.) and environment (e.g. temperature). |
| Positioning of filter on mask | Optimal positioning would be in a location (e.g. side of mask) capable of adequate ventilation (e.g. not covered by head cover) and providing an adequate field of view (e.g. not blocking user's view). |
| Mask seal to face | A comfortable seal is important for good user compliance (e.g. an air-filled, silicone balloon for contact with the face). |
| Variations in securing mask to head | An air-tight seal with the face is needed to prevent air from leaking in along the skin surface of the face (e.g. a strap coursing over the back lower and back upper portions of the user's head). |
Finally, the use of proper PPE, including eye protection, is very important, especially for health workers who are in close contact with patients with active COVID-19 infections during a pandemic or even an outbreak. Additionally, such eye protection would also be quite useful for research personnel around the world who must wear eye protection with a face shield or full head respirators, such as Powered Air Purifying Respirators (PAPRs).
6. Conclusion
First, and foremost, heeding the recommendations of the CDC is of paramount importance in mitigating the COVID-19 outbreak. See https://www.cdc.gov/coronavirus/index.html. With respect to minimizing transmission through the eyes, the CDC recommends avoiding touching the eyes with unwashed hands. It is important to consider that even basic, non-hermetically sealed eye wear can prevent some of the droplets. This article discussed a novel FEM, which holds promise in reducing the spread of COVID-19. It is important that rigorous testing be performed to maximize effectiveness and compliance (Wong, 2013). Further research, especially on the efficiency of the FEM to protect against transmission of infection, is needed and must be done rapidly.
Conflicts of interest: Author Dr. David Douglas is a medical doctor and his father, Dr. Robert Douglas, is an engineer. They co-authored a non-provisional patent pending (#16/773,960) including a variety of designs disclosed in patent pending, and would be more than happy to collaborate with any and all parties in efforts to try and mitigate the spread of COVID-19.
Funding source: None.
Ethical approval: Not required.
References
- CDC . 2020. 2019 Novel Coronavirus, Wuhan, China. Available from: https://www.cdc.gov/coronavirus/2019-ncov/about/prevention-treatment.html [accessed 28 January 2020] [Google Scholar]
- Chughtai A.A., Seale H., Rawlinson W.D., Kunasekaran M., Macintyre C.R. Selection and Use of Respiratory Protection by Healthcare Workers to Protect from Infectious Diseases in Hospital Settings. Ann Work Exposures Health. 2020 doi: 10.1093/annweh/wxaa020. [DOI] [PubMed] [Google Scholar]
- Dain S.J., Hoskin A.K., Winder C., Dingsdag D.P. Assessment of fogging resistance of anti-fog personal eye protection. Ophthal Physiolog Optics. 1999;19(4):357–361. doi: 10.1046/j.1475-1313.1999.00418.x. [DOI] [PubMed] [Google Scholar]
- Douglas P.K., Douglas D.B., Harrigan D.C., Douglas K.M. Preparing for pandemic influenza and its aftermath: mental health issues considered. Int J Emerg Mental Health. 2009;11(3):137–144. [PubMed] [Google Scholar]
- Gold J. 2020. The Covid-19 crisis too few are talking about: health care workers’ mental health. Available from: https://www.statnews.com/2020/04/03/the-covid-19-crisis-too-few-are-talking-about-health-care-workers-mental-health/ [accessed 15 April 2020]. [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. New Eng J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara A. 2020. Nurses across the country protest lack of protective equipment. Available from: https://www.cbsnews.com/news/health-care-workers-protest-lack-of-protective-equipment-2020-03-28/ [accessed 15 April 2020]. [Google Scholar]
- Phan L.T., Nguyen T.V., Luong Q.C., Nguyen T.V., Nguyen H.T., Le H.Q. Importation and Human-to-Human Transmission of a Novel Coronavirus in Vietnam. New Eng J Med. 2020 doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong K.K. 2013. Methods in research and development of biomedical devices: World Sci. [Google Scholar]
- Worldometer . 2020. COVID-19 CORONAVIRUS. Available from: https://www.worldometers.info/coronavirus/coronavirus-cases/ [accessed 15 April 2020]. [Google Scholar]