Highlights
-
•
Three main CRM research categories covered: e-CRM, implementing CRMS and adopting CRMS.
-
•
Precise CRM research review and summarisation of empirical evidence for healthcare environments.
-
•
Presents positive and negative outcomes of CRM technology in the healthcare sector.
-
•
Results show significant gaps in the knowledge of CRM in the healthcare sector.
-
•
Few studies apply mixed methodologies and theories to investigate the CRM technology in the healthcare sector.
Keywords: Customer relationship management (CRM), Patient relationship management (PRM), Healthcare environment, Healthcare industry, Information and communication technologies (ICT)
Abstract
Customer relationship management (CRM) is an innovative technology that seeks to improve customer satisfaction, loyalty, and profitability by acquiring, developing, and maintaining effective customer relationships and interactions with stakeholders. Numerous researches on CRM have made significant progress in several areas such as telecommunications, banking, and manufacturing, but research specific to the healthcare environment is very limited. This systematic review aims to categorise, summarise, synthesise, and appraise the research on CRM in the healthcare environment, considering the absence of coherent and comprehensive scholarship of disparate data on CRM. Various databases were used to conduct a comprehensive search of studies that examine CRM in the healthcare environment (including hospitals, clinics, medical centres, and nursing homes). Analysis and evaluation of 19 carefully selected studies revealed three main research categories: (i) social CRM ‘eCRM’; (ii) implementing CRMS; and (iii) adopting CRMS; with positive outcomes for CRM both in terms of patients relationship/communication with hospital, satisfaction, medical treatment/outcomes and empowerment and hospitals medical operation, productivity, cost, performance, efficiency and service quality. This is the first systematic review to comprehensively synthesise and summarise empirical evidence from disparate CRM research data (quantitative, qualitative, and mixed) in the healthcare environment. Our results revealed that substantial gaps exist in the knowledge of using CRM in the healthcare environment. Future research should focus on exploring: (i) other potential factors, such as patient characteristics, culture (of both the patient and hospital), knowledge management, trust, security, and privacy for implementing and adopting CRMS and (ii) other CRM categories, such as mobile CRM (mCRM) and data mining CRM.
1. Introduction
Healthcare organisations face substantial pressure to maintain high quality medical care while simultaneously increasing safety and reduce costs [1,2]. Issues such as the growing number of chronic illnesses and the ageing population; higher patient demand and expectations; and the lack of qualified medical professionals, have complicated healthcare organisations’ ability to fulfil their missions [3,4].
Health information technology (HIT, also known as e-health or medical informatics [5]), is viewed as a significant tool to achieve cost savings, efficiency, quality, and safety [6], [7], [8]. The benefits of HIT include: improved medical services and workflows, providing decision-making support and clinical information for medical professionals, expanding the quality, safety, and effectiveness of patient care, preventing medical errors; and reducing expenses, admissions, and paperwork [9], [10], [11], [12], [13], [14], [15], [16]. Many studies suggest that the effectiveness of implementing HIT will determine the success and survival of the healthcare industry. Consumer e-health, patient engagement, and patient-centric care also play significant roles in delivering high quality medical services and meeting patient needs [17]. Many studies have found that the more patients are involved in their own health, the better outcomes in terms of quality, cost, and performance [18], [19], [20]. Healthcare providers now see the patient more clearly as the end consumer of medical services; thus, as in any kind of business, the concept of patient satisfaction and loyalty has become healthcare organisations’ foremost concern [2].
Customer relationship management (CRM) is an innovative technology that seeks to improve customer satisfaction, loyalty, and profitability by acquiring, developing, and maintaining effective customer relationships and interactions [21]. From a healthcare perspective, Benz and Paddison [22] defined CRM as ‘an approach to learn about patients in order to communicate appropriately, and to build good relationships in order to deliver timely information, with the patient's results tracked to make necessary adjustments’. In this study, we embrace a balanced perspective, and define CRM in the healthcare environment as a managerial approach and healthcare information technology (HIT) application that supports the concept of patient-centric care. This allows hospitals to focus more on patients to meet their needs and expectations, improve loyalty, service quality (SQ), and build a long-term relationship.
The use of IT is essential for executing CRM, Yina [23] pointed out that effective CRM requires comprehensive data collection from both inpatients and outpatients through a multi-media platform, as well as integrating CRMS with various clinical networks such as hospital information systems (HIS), electronic health records (EHR), laboratory information systems (LIS), hospital web platforms, call centres, and SMS-based systems [23,24]. This requires healthcare providers to possess IT resources such as hardware, software, and infrastructure, to implement CRMS and store patient records more efficiently. Healthcare providers may be able to achieve patient loyalty if they considered two key factors: (i) the number of patients, and (ii) patient profit. The more ‘loyal patients’ a hospital has, the less investments it must make, the greater the profits it can gain, and vice versa. McDonald [25] stated that life-long value of a patient involves two major aspects: (i) the ‘core relationship’ which consists of a variety of uses of ‘frequency’ and confirming loyalty through ‘commitment’; and (ii) the ‘extended relationship’, which consists of product commercialisation such as ‘communication tools’ and word of-mouth ‘recommendations’. Furthermore, chronic diseases such as asthma, diabetes, hypertension, hyperlipidaemia, and cardiac failure, require continuous follow-up and self-management. Therefore, it is crucial for healthcare providers to know that certain patients require multiple healthcare services, and it is important to maintain high quality medical services and long-term relationships, which will eventually create long-life value [26].
Previous research on CRM has made significant progress in several areas, such as telecommunications [27], [28], [29], banking [30], [31], [32], [33], [34], [35], [36], [37], manufacturing [38], [39], [40], and the service industry [41], [42], [43], [44], [45], but research specific to the medical sector is very limited. Also, while many studies have attempted to review various HIT innovations and applications [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], no systematic review has been conducted on CRM research with a focus on healthcare settings. However, the first systematic literature review to comprehensively investigate the CRM mechanisms from an information system (IS) perspective was performed by Soltani and Navimipour [58]. Twenty-seven studies between 2009 and 2015 were included in the review. The main objective of this work was to explore five common categories of CRM techniques with regards to the IS. These categories were; knowledge management (KM), E-CRM, data mining, social CRM and data quality. While this study focused on CRM mechanisms from IS perspective, our study focuses on CRMS in the healthcare environment. Filling this gap allows a significant contribution to be made, particularly on the issues of consumer e-health, patient engagement, and patient-centric care. For this purpose, we have undertaken a systematic literature review (SLR) of the empirical evidence regarding CRM research in the healthcare environment over the past two decades. Accordingly, we set out to answer the following key research questions:
-
■
RQ1: What are the research categories for CRM technology in the healthcare environment?
-
■
RQ2: What methods of data collection have been used?
-
■
RQ3: What are the positive and negative outcomes of CRM research in the healthcare environment?
This paper is organised as follows, Section 2 illustrates our review methodology which describes the search strategy, keywords used, selection process, critical appraisal, data collection and analysis. Section 3 presents and summarises the key findings of the selected studies. The main findings with response to the research questions, strength and limitations of the review as well as future work suggestions are discussed in Section 4, and Section 5 concludes the paper.
2. Methodology and strategy
2.1. Design
For this study, a systematic review was conducted of disparate (quantitative, qualitative, and mixed) evidence of CRM [59,60], following the criteria of preferred reporting items for systematic reviews and meta-analysis (PRISMA) [61,62]. These include the following steps: (1) eligibility criteria; (2) information sources; (3) search terms; (4) study selection; (5) data collection process and synthesis; and (6) critical appraisal.
2.2. Eligibility criteria
Studies were eligible for inclusion if they were: presenting an empirical and conceptual evidence; directly relevant to CRM in healthcare settings (hospitals, clinics and medical centres); papers that are conducted in developing countries; published from 2000 to present; and published in peer-reviewed journals. The main reason for selecting studies that were conducted in developing countries is because health technologies play an important role in the effectiveness of patient care and treatment, yet access to such technologies remain a big challenge for communities with limited recourses.
We excluded studies if they were: not written in English; traditional reviews, thesis and conference proceedings; papers that focused on other healthcare domains such as insurance and pharmaceuticals; and papers that were not available in full text.
2.3. Information sources
Our methodical procedure used various strategies to obtain as many relevant studies as possible from a diverse evidence base [63,64]. In the first step, we searched the Database of Abstracts of Reviews of Effects (DARE) and the Cochrane Database of Systematic Reviews (CDSR) to verify if there were any existing or ongoing systematic reviews similar to our subject.
Secondly, we conducted an organised, systematic and comprehensive wide-ranging search of six online databases: Web of Science, ScienceDirect, Scopus, SpringerLink, IEEE Xplore, and the Association for Computing Machinery (ACM) Digital Library. We also examined four group publishers of academic journals (Emerald Insight, Wiley Online Library, Taylor & Francis Online, and SAGE Digital Library) and two search engines (PubMed and Google Scholar).
To identify relevant studies, we then performed a library search of six medical informatics and health management journals: (1) the Journal of Medical Internet Research; (2) the Journal of the American Medical Informatics Association (JAMIA); (3) PLOS (Public Library of Science) ONE; (4) BMJ Open; (5) the International Journal of Medical Informatics; (6) BMC Medical Informatics and Decision Making. We also contacted two experts in the field to find additional or unpublished relevant studies. Finally, we checked reference lists of all eligible studies using Google Scholar to discover hidden additional studies. It should be noted that each online database has its own search engine features. Hence, the search string had to be modified and adapted for each online database. To do so, our search was recorded in a separate text that includes the following details: source category, source name, search method and date of search for each online database. This can be seen in Table 1 .
Table 1.
Search space for selected databases.
| Source category | Source name | Search method | Date of search |
|---|---|---|---|
| Online database | Web of Science | Abstract, title and keywords; | 2019–12–10 |
| ScienceDirect | Abstract, title and keywords; | 2019–12–14 | |
| Scopus | Abstract, title and keywords; | 2019–12–10 | |
| SpringerLink | Abstract and keywords; | 2019–12–13 | |
| IEEE Xplore | Abstract and keywords; | 2019–12–17 | |
| ACM | Abstract and keywords; | 2019–12–15 | |
| Search engine | Google scholar | Full text; | 2020–01–08 |
| Pubmed | Full text; | 2020–01–12 | |
| Group publisher | Emerald Insight | Abstract, title and keywords; | 2020–01–14 |
| Wiley | Abstract and keywords; | 2020–01–13 | |
| Taylor & Francis | Abstract, title and keywords; | 2020–01–16 | |
| SAGE | Abstract and keywords; | 2020–01–13 |
2.4. Search terms
The search process is very crucial; therefore, the keywords were optimised. In the first stage, we obtained a set of keywords and terms from the acquired studies and matched them with our research aims and questions. Secondly, we established alternative characteristics and synonyms. The defined keywords were tested in different databases and lastly, we optimised them. Table 2 summarises the final list of keywords used in the search.
Table 2.
List of keywords used in the search process.
| Category | Keywords |
|---|---|
| Customer relationship management | CRM, CRM system, CRM technology. |
| Patient relationship management | PRM, PRM system, PRM technology. |
| Health care environment | Healthcare industry, healthcare sector, hospital, healthcare providers, medical centre, medical service. |
| Developing country | Developing countries. |
Next, Logical operators were connected with different sets of keywords and designed as follows: (CRM OR CRM system OR CRM technology) OR (PRM OR PRM system OR PRM technology) AND (Healthcare industry OR healthcare sector OR hospital OR healthcare providers OR medical centre OR medical service) AND (Developing countries).
2.5. Study selection
The study selection process attempts to analyse, evaluate and identify relevant articles based on the goals of our systematic review. This process was independently performed by three co-authors (H.A., A.P. and G.A.) of this study. Table 3 explains each stage that has been executed in the study selection process. In the first stage (S1), records are identified through different information sources (online database, academic journal and reference list). Once all records are obtained, we applied the first filter in the second stage (S2), to which records are excluded based on duplicates. We used EndNote X9 to remove duplicates and manage all records.
Table 3.
Stages of the study selection process.
| Stage | Description | Participants |
|---|---|---|
| S1 | Selection of studies identified through different information sources. | H.A., A.P. and G.A. |
| S2 | Exclusion of studies based on duplicates. | H.A., A.P. and G.A. |
| S3 | Exclusion of studies based on a “title, abstract and keywords” screening, against the eligibility criteria. | All authors |
| S4 | Consensus meeting. | All authors |
| S5 | Exclusion of studies based on a “full-text” screening. | All authors |
| S6 | Consensus meeting. | All authors |
Once all duplicates are removed, records are screened based on “title, abstract and keywords”, during this third stage (S3), any studies that did not meet the eligibility criteria were excluded. Also, during this stage, we considered studies for a “full-text” screening, and arranged meetings between co-authors whenever there were doubts. Such meetings have allowed co-authors to review and agree on studies that were within the scope and pertinent to this systematic review.
The first meeting (S4), aimed to discuss the findings of the third stage and select the primary studies for the next stage (S5), where a “full-text” screening of all studies was performed. A second meeting, which was the last stage (S6) of the selection process, was carried out to discuss and agree on the final studies that are included in this systematic review.
2.6. Data collection and synthesis
We used EndNote X9 to collect basic publication data such as date, title, authors, publisher, DOI, URL, pages, volume, issues, keywords and abstract. In addition to EndNote, one co-author (G.H.) of this study placed data from eligible studies into a data extraction spreadsheet using Microsoft Excel 2016, then two other co-authors (Y.B. and A.P.) validated it independently. The data items extracted from each eligible study were: year of publication; author; brief description; type of evidence; participants; sample size (n); healthcare organisation type and size; country of origin, and outcomes.
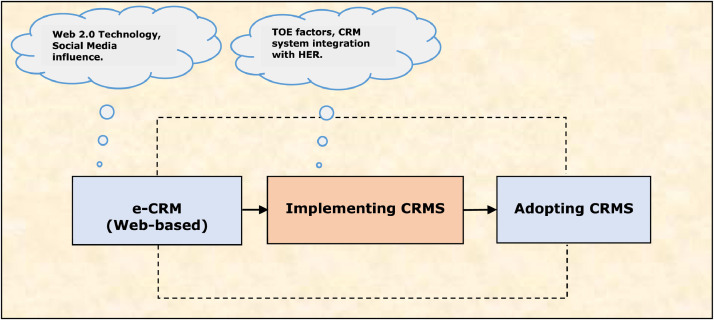
To synthesise the data as accurately and in an unbiased manner as possible, we performed a narrative synthesis review for effectiveness [65] of diverse study characteristics, which allowed us to categorise and identify three main CRM research categories that were relevant to healthcare settings: (i) e-CRM (Web-based CRM); (ii) implementing CRMS; and (iii) adopting CRMS. We also created a qualitative and quantitative evidential narrative summary [60,63] for each CRM research category.
We contacted the original authors of the selected studies by e-mail to resolve any doubts or confirm an absence of information. In addition, any disagreements between co-authors of this study were settled through consensus.
2.7. Critical appraisal
Two co-authors (A.I.A and O.A.) of this study independently appraised the quality of selected studies to avoid misinterpretation and bias. We followed the criteria of quality assessment and assurance tools for undertaking a systematic review of disparate data developed by Hawker et al. [66]. Table 4 elaborates the checklist that is used to appraise each individual study. This checklist is based on nine assessment criteria with four rating scores defined as good, fair, poor and very poor respectively. A description of how these ratings were assigned and evaluated is described and illustrated in Table 4.
Table 4.
Checklist items used for critical appraisal.
| Item | Assessment criteria | *Score | Description |
|---|---|---|---|
| QA1 | Abstract and title: Did they provide clear description of the study? | Good Fair Poor Very Poor |
- Structured abstract with full information and clear title. - Abstract with most of the information. - Inadequate abstract. - No abstract. |
| QA2 | Introduction and aims: Was there a good background and clear statement of aims? | Good Fair Poor Very Poor |
- Concise background/containing up to date literature and highlighting gaps in knowledge. - Clear statement of aim AND objectives including research questions. - Some background and literature review. - Research questions outline. - Some background but no aim/objectives/questions, OR aims/objectives but inadequate background. - No mention of aims/objectives. - No background or literature review. |
| QA3 | Method and data: Is the method appropriate and clearly explained? | Good Fair Poor Very poor |
- Method is appropriate and described clearly. - Clear details of data collection and recording. - Method appropriate, description could be better. - Data described. - Questionable whether method is appropriate. - Method described inadequately. - Little description of data. - No mention of method, AND/OR method in appropriate, AND/OR no details of data. |
| QA4 | Sampling: Was the sampling strategy appropriate to address the aims? | Good Fair Poor Very Poor |
- Details (age/gender/race/context) of who was studied and how they were recruited. - Why this group was targeted. - Response rates shown and explained. - Sample size justified. - Most information given, but some missing. - Sampling mentioned but few descriptive details. - No details of sample. |
| QA5 | Data analysis: Was the description of data analysis sufficiently rigorous? | Good Fair Poor Very poor |
- Clear description of how analysis was done. - Qualitative studies: Description of how themes derived/respondent validation or triangulation. - Quantitative studies: Reasons for tests selected hypothesis driven/numbers add up/statistical significance discussed. - Qualitative: Descriptive discussion of analysis. - Quantitative. - Minimal details about analysis. - No discussion of analysis. |
| QA6 | Ethics and bias: Have ethical issue been addressed, and what necessary ethical approval gained? | Good Fair Poor Very poor |
- Ethics: Where necessary issues of confidentiality, sensitivity, and consent were addressed. - Bias: Researcher was reflexive AND/OR aware of own bias. - The above issues were acknowledged. - Brief mention of issues. - No mention of issues. |
| QA7 | Results: Is there a clear statement of the findings? | Good Fair Poor Very poor |
- Findings explicit, easy to understand, and in logical progression. - Tables, if present, are explained in text. - Results relate directly to aims. - Sufficient data are presented to support the findings. - Findings mentioned but more explanation could be given. - Data presented relate directly to results. - Findings presented randomly, not explained, and do not progress logically from results. - Findings not mentioned or do not relate to aims. |
| QA8 | Transferability or generalisability: Are the findings of this transferable (generalisable) to a wider population? | Good Fair Poor Very poor |
- Context and setting of the study is described sufficiently to allow comparison with other context and settings. - Some context and setting described, more needed to replicate or compare the study with others. - Minimal description of context/setting. - No description of context/setting. |
| QA9 | Implication and usefulness: How important are these findings to policy and practice? | Good Fair Poor Very poor |
- Contributes something new AND/OR different in terms of understanding/insight or perspective. - Suggests ideas for further research. - Suggests implications for policy AND/OR practice. - Two of the above (state what is missing in comments). - Only of the above. - None of the above. |
*Score criteria for QA = Quality assessment
Our primary concern being to obtain sufficient knowledge and evidence of the nature of CRM in the healthcare environment, and we performed sensitivity intervention analysis [67] to determine whether: (i) the inclusion of each study was based on its quality, and (ii) the exclusion of empirical data from conference proceedings would have any effects on our ultimate results. We resolved disagreements on critical appraisal of the selected studies through group discussion and with “chairperson” arbitration assistance given by the first author (Y.B.) of this paper.
3. Results of the systematic review
Firstly, we illustrate the results of our study screening and selection process according to PRISMA guidelines. Secondly, we describe the trends and characteristics of the selected studies and present quantitative data (i.e. publication year and location, methods of data collection, settings, participants and sample sizes). Thirdly, we demonstrate the results of our critical appraisal of each study, and lastly, we summarise the CRM research categories. All findings stated in this section are directly responding to our set of three research questions (RQs).
3.1. Study selection
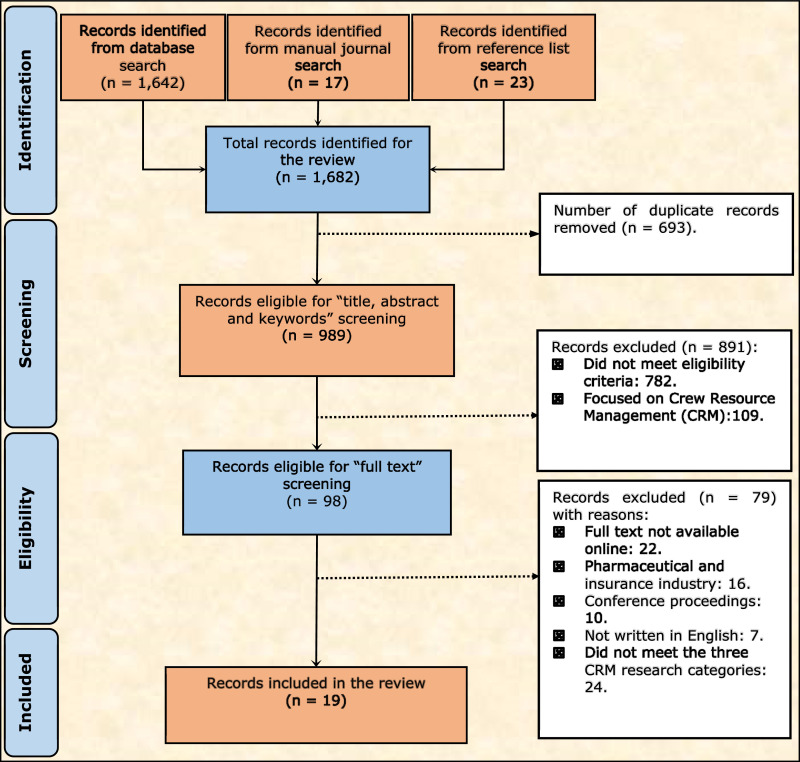
In our initial search, we found 1642 studies (see Fig. 1 ). We identified a total of 1682 studies for the review, including those found through manual searches of medical informatics and management journals (N = 17), and reference lists (N = 23). Studies removed after duplicates (N = 693). Applying the eligibility criteria, we excluded 891 studies by screening the title, the abstract and the keywords. Finally, we excluded 79 based on the full text screening. Hence, the final sample consisted of 19 studies.
Fig. 1.
PRISMA flow chart for the screening and selection process of the selected studies.
3.2. Study trends
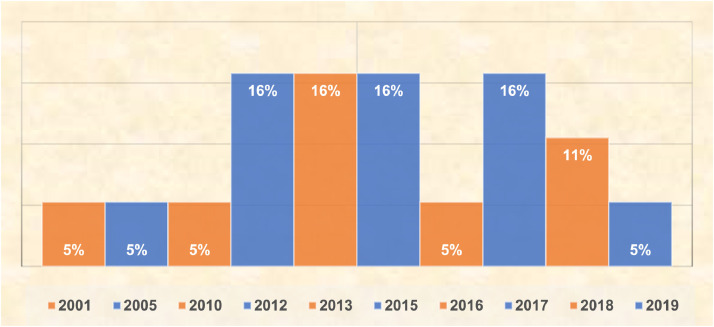
Fig. 2 presents the per year distribution of the selected studies. The number of studies has remarkably increased in recent years, which indicates that CRM in the healthcare environment is progressively attracting the attention of scholars and researchers. Most of the studies selected were conducted between 2012 and 2017 (N = 13, 568%).
Fig. 2.
Distribution of studies per year.
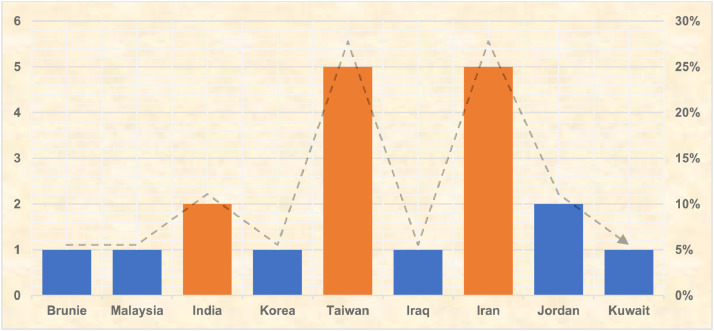
As shown in Fig. 3 , most of the studies were conducted in Taiwan and Iran (N = 10, 53%), which indicates the advanced production of ICT and medical informatics in those regions and therefore associated research efforts into their impact. Of these, 21% (N = 4) were carried out in India and Jordan. The rest took place in Iraq, Brunei, Korea, Malaysia and Kuwait.
Fig. 3.
Distribution of studies per country.
3.3. Study characteristics
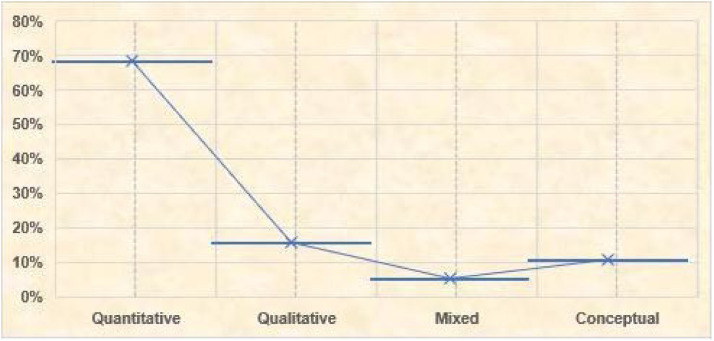
Among the selected studies, 68% (N = 13) had quantitative designs. The remaining studies used qualitative (N = 3, 16%) and mixed-method approaches (N = 1, 5%), while two studies (11%) were based on conceptual modelling of CRM (see Fig. 4 ).
Fig. 4.
Distribution of methods used in the selected studies.
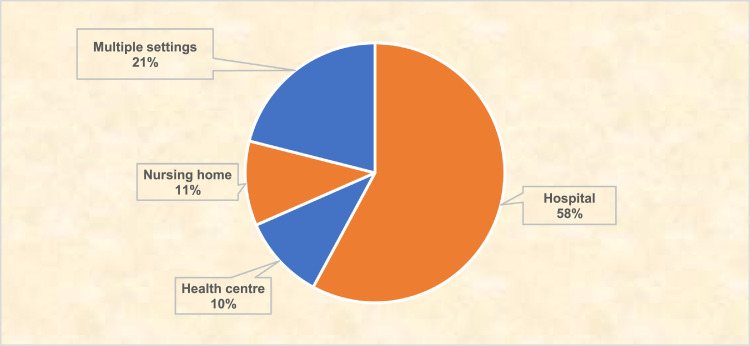
The healthcare settings were mainly various kinds of hospitals (N = 11, 58%) such as private, public, regional, community and university hospitals (Fig. 5 ). The rest of the studies were conducted in nursing homes (N = 2, 11%) and health centres (N = 2, 11%). Four studies (21%) were conducted in multiple settings such clinics, homecare centres, and health promotion centres.
Fig. 5.
Settings of the selected studies.
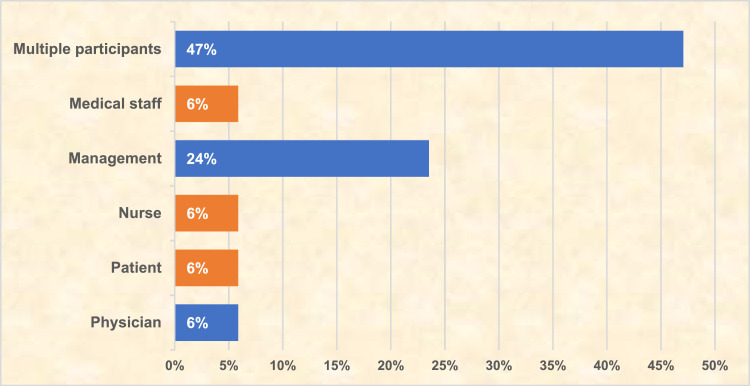
Among the targeted groups, 47% of the studies (N =8), have simultaneously recruited multiple stakeholders such as patients, patient families, medical staffs, CRM experts, nurses, nursing professionals, nurse supervisors, HIS professionals, chief executive officers (CEOs), or chief information technology officers (CITOs). As shown in Fig. 6 , the remaining respondents were management (24%), physicians (6%), patients (6%), nurses (6%), and auxiliary medical staff (6%).
Fig. 6.
Participants of the selected studies.
Majority of the studies have utilised a sample size between 200 and 399 (N = 5, 31%). Only one study has used a sample size of more than 400. Fig. 7 illustrates the variation of the sample sizes used in the selected studies.
Fig. 7.
Sample size of the selected studies.
3.4. Critical appraisal of selected studies
Our critical appraisal of the selected studies (see Table 5 ) found major weaknesses in four areas: (i) research methods and data, (ii) sampling, (iii) ethics and bias and (iv) implications and usefulness. In terms of research methods and data collection and analysis, studies gave little descriptions of the methods and approaches to gather and record data in a consistent manner (rated as fair and poor in 53% and 26% of the studies, respectively).
Table 5.
Critical appraisal of the selected studies.
| Item | Assessment criteria | Score | ||||
|---|---|---|---|---|---|---|
| Good | Fair | Poor | Very poor | NR | ||
| QA1 | Abstract and title | 4 (21) | 13 (68) | 1 (5) | 1 (5) | 0 (0) |
| QA2 | Introduction and aims | 4 (21) | 8 (42) | 7 (37) | 0 (0) | 0 (0) |
| QA3 | Method and data | 4 (21) | 10 (53) | 5 (26) | 0 (0) | 0 (0) |
| QA4 | Sampling | 5 (26) | 9 (47) | 4 (21) | 0 (0) | 1 (5) |
| QA5 | Data analysis | 5 (26) | 11 (58) | 3 (16) | 0 (0) | 0 (0) |
| QA6 | Ethics and bias | 1 (5) | 1 (5) | 3 (16) | 0 (0) | 14 (74) |
| QA7 | Findings | 4 (21) | 12 (63) | 3 (16) | 0 (0) | 0 (0) |
| QA8 | Transferability/generalizability | 2 (11) | 10 (53) | 7 (37) | 0 (0) | 0 (0) |
| QA9 | Implications and usefulness | 3 (16) | 7 (37) | 4 (21) | 0 (0) | 5 (26) |
*Note: Numbers in brackets denotes N (%); and NR denotes not reported.
Regarding the sampling, some researches lacked details on the sampling techniques and strategies, the justification of the sample size and target groups, as well as the response rates (assessed as fair, poor, and not reported in 47%, 21%, and 5% of the studies, respectively). Furthermore, the ethics and risk of bias was not clearly reported in 74% of the studies. We rated the implications and usefulness of the selected studies as poor and not reported in 47% of total studies. The results of this review remained reliable and consistent, even after we performed the sensitivity analysis to determine whether we included each study based on its quality, and whether excluding empirical data from conference proceedings had any effects on our results.
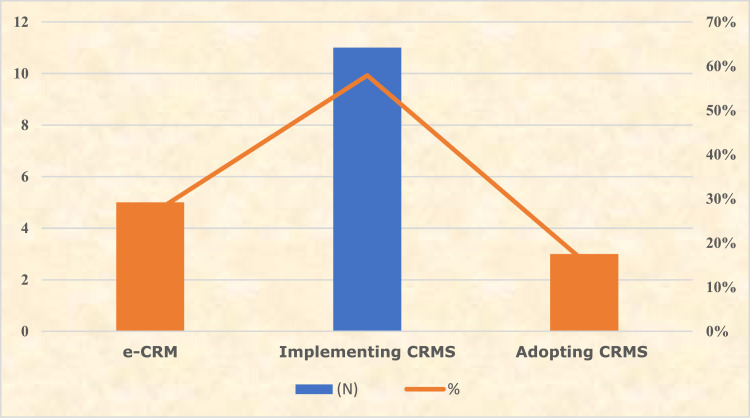
3.5. Category of CRM research in healthcare
Our analysis of the selected studies revealed three main categories of CRM research in the healthcare sector: (i) e-CRM (Web-based CRM); (2) implementing CRMS; and (3) adopting CRMS. While precisely 58% of the selected studies (N = 11) focused on implementing CRMS, other research categories were less frequently investigated: social CRM (N = 5, 26%), and adopting CRM (N = 3, 16%). Fig. 8 shows the representation of CRM research categories.
Fig. 8.
Category of CRM research in healthcare.
3.5.1. e-CRM (web-based/social CRM)
Social CRM or e-CRM is a new concept that has emerged into the CRM systems due to the incessant advancement of IT and web services, as well as other advances in ICT and data science techniques. The authors of [68] defined e-CRM as a modern approach and a system that integrates both Web 2.0 and the influence of online groups with conventional CRM systems to build strong communication and relationships between the customers and the firms. In the healthcare environment, many studies have explored the phenomena of e-CRM. As early as 2001, Kohli et al. [69] explored the Web-based CRM system in a hospital through a physician profiling system (PPS). Results gathered after implementing PPS showed that total charges were significantly reduced, which led to better care and patient's satisfaction.
The authors of [70] proposed a social CRM model to support patient empowerment through a Web 2.0, namely CRM 2.0. They surveyed 366 patients, patients’ family members and medical staff from various hospitals and homecare centres to determine patients’ expectations of e-health services, and to verify the empowerment features proposed in the model. This study found that there was high demand for empowering patients through the Web. The findings also revealed that more than 80% of targeted groups preferred to view health promotions, make appointments and payments online. While more than 75% preferred to go online to view their own medical records and discuss their health conditions on a social network. Also, 73% of participations desired an online consultation.
The authors of [71] developed a framework for implementing e-CRM, and surveyed 150 managing directors and branch managers from 50 clinics and hospitals (both public and private) to investigate the key factors of executing e-CRM based on their importance and priorities. This study concluded that patient's involvement is the most important factor in implementing e-CRM.
An e-CRM adoption framework was proposed by Jalal et al. [72] to determine the crucial factors that influence the adoption of e-CRM in hospitals. TOE, diffusion of technology and institutional theories were utilised in the construction of the framework. This work found that technological factors such as complexity and relative advantage; organizational factors such as size and management support; and environmental factors such as regulatory and external pressure are very crucial for e-CRM adoption.
Similar to this work, the authors of [73] proposed an e-CRM implementation framework utilising Technology-Organization-Environment (TOE), diffusion of technology and Information System (IS) success theories and found that technological (compatibility, interactivity and privacy); organizational factors (management support, social media policy and leadership knowledge) and environmental factors (social trust and bandwagon pressure) are very critical for e-CRM implementation.
3.5.2. Implementing CRMS
As early as 2005, Cheng et al. [74] established a framework to support executing CRM in nursing homes. The authors of [75,76] influenced this framework, which involves three aspects of CRM: case management (CM), data management (DM), and care service management (CSM). The results yielded nine sub-dimensions: (1) an interactive mechanism; (2) an assessment of demand models; (3) customer data collection; (4) data analysis, (5) knowledge management (KM), (6) care service design; (7) care service delivery; (8) support from related units and (9) monitoring and feedback. The final framework showed that implementing CRM in nursing homes required: (A) leadership ‘support from high level managers’; followed by (B) a culture involving the ‘participation of all members’ in order to employ aspects of a (C) CRM system (CM, DM, and CSM) within the nine sub-dimensions. The study also found that most nursing homes have yet to implement CRM, and computerisation requires more effort.
The authors of [77] argued that the CRM framework proposed by Cheng et al. [74] was inappropriate because their results were obtained from a value characteristic questionnaire. However, the two sub-dimensions of CM, ‘interactive mechanism’ and ‘assessment of demand models’, did not clearly map all the attributes defined in the survey. Accordingly, similar to the work of [74], Gulliver et al. [77] adapted a value characteristic framework to support establishing CRM in nursing homes. This study found the most three significant dimensions to be: the ‘behaviour of service personnel’, the ‘design of care processes’, and ‘support from related units’. Based on the findings, the authors claimed that approaches to executing CRM in nursing homes would be inappropriate if only one solution was considered to fulfil all the attributes. Accounting for each attribute would ensure consistency, relevancy, and provide an effective, focused plan. While allowing each individual characteristic to be linked to a specific CRM solution type would support the practical implementation of CRM, we believe the adapted framework could also assist hospitals, especially in terms of answering the following questions: (1) what are the most valuable elements of putting CRM into practice? and (2) How can we link each feature to a CRM solution type?
The authors of [78] adopted the soft system dynamics methodology (SSDM) and used a case study on a physical examination centre to evaluate the steps of applying a CRM model. SSDM integrates the qualities of both soft system methodology (SSM) and system dynamics (SD) that involves four phases with ten systematic steps. The results showed that the four stages and ten systematic steps allowed the authors to positively measure and evaluate the CRM model. Improved efficiency, as well as provided a better service for health organisation were outcomes of this process.
The authors of [79] explored the key factors of realising CRM systems, and proposed a model based on three attributes: (1) the organisation itself (resources, management, and employee factors); (2) applying CRM (the CRM system factor) and (3) the customer (the patient factor). The authors recommended and proposed the ‘DeLone and McLean information systems (IS) success model’ to assess CRM implementation.
The authors of [80] proposed and adopted the ‘DeLone and McLean IS success model’ for executing CRM based on three traits: (1) the system (system quality, information quality, and SQ); (2) the user (perceived usefulness and user satisfaction) and (3) performance (organisational and personal performance). They administered a survey to 243 CRM system users from 13 health promotion centres to validate the aforementioned IS model. The outcomes showed that (1) the CRM model was feasible; (2) of system attributes, only ‘information quality’ and ‘SQ’ had a significant influence and relationship with ‘perceived usefulness’ and ‘user satisfaction’ and (3) ‘perceived usefulness’ and ‘user satisfaction’ had a significant impact on ‘personal performance’ as well as an indirect effect on ‘organisational performance’.
The authors of [81] surveyed 615 staff members in 108 privately run and 30 hospital-based nursing homes to assess CRM implementation. The author adapted the CRM scale developed by Sin et al. [82], which involves four dimensions: (1) a key customer focus; (2) CRM organisation; (3) technology-based CRM and (4) KM, along with 23 sub-dimensions. However, in this study, only 18 sub-dimensions were adapted to evaluate CRM implementation. Furthermore, the study found that the two types of nursing homes had different ways of building relationships with residents. Hospital-based nursing homes leaned toward understanding patients’ needs and delivering prompt medical service through the concept of ‘knowledge learning’. Private nursing homes focused on ‘CRM organisation’ and ‘technology-based CRM’ to foster personal connections with residents.
Another CRM implementation model was introduced by Zamani and Tarokh [83], this model consists of seven components; Customer satisfaction, loyalty, trust, expectations, perceptions, perceived quality and Architecture. A total of 303 patients were surveyed and found that All seven components were significant and have relationship with each other. Also, the authors of [84] designed a CRM implementation model based on HR factors such as employee satisfaction, organizational culture, communication management, empowerment, organizational commitment, organizational structure and change management. This work surveyed 215 managers of a university hospital. Findings revealed that HRM plays a crucial role in the implementation of CRMS. However, the employee satisfaction factor had the highest influence on the implementation of CRMS.
The authors of [85] surveyed 100 patients and CRM users to analyse the factors that influence the implementation of CRM based on software aspects. Results showed that operational efficiency, centralization of data, management of existing customer and hospital image have a significant influence on the implementation of CRMS.
The authors of [86] evaluated the effects of CRMS implementation on customer trust, loyalty, satisfaction and organisational productivity. They administered a survey to 268 CRM nurses from various hospitals. Results showed that customer satisfaction and diversification have the highest effects on CRMS implementation, while organisational productivity had the lowest impact.
The authors of [87] investigated various impacts and benefits of implementing CRMS in hospitals. More than 550 of doctors, administrators and IT staffs were surveyed and found that waiting time reduction, better doctor allocation, and patient satisfaction were the major implication of CRM implementation in health care.
3.5.3. Adopting CRMS
To investigate the critical factors that influence the adoption of CRM systems (CRMS), Hung et al. [21] performed a 95-questionnaire study of Information Systems (IS) executives at three levels of health organisations: medical centres, community hospitals and regional hospitals. The results showed that 39 hospitals adopted CRMS, while 56 did not. ‘Relative advantages’, the ‘size of the organisation’, the ‘IS capabilities of the staff’, ‘KM capabilities’, and the ‘innovation of senior executives’ have significantly influenced the adoption of CRM systems the 39 hospitals. The authors found ‘complexity’ to be insignificant. The authors recommended several implications for CRM vendors, hospitals, government, and researchers to increase possibility of adopting CRM.
To examine the influence and relationship of ‘external influences’, ‘technology’, and ‘organisations’ factors on CRM system adoption, Alkhazali and Hassan [88] conducted a 103-questionnaire of the top management in 18 different hospitals (15 private ones and 3 public ones). This study found that most of the hospitals only used Web-based CRM. Furthermore, the results showed that ‘organisations’ and ‘technology’ significantly influenced the adoption of CRM. The authors found the external factors to be insignificant. Also [89] examined the relationship between CRMS adoption, perception and organisation performance. A 103-survey of the top management in various hospitals was also conducted and found (i) a significant relationship between organisation performance and CRMS adoption, and (ii) a significant relationship between CRMS adoption and CRMS perception.
In light of the above, the majority of studies regarding the three main categories of CRM (e-CRM, implementing and adopting CRMS) were able to produce positive outcomes for patients, medical professionals and healthcare organizations.
To offer a better illustration and respond to our three research questions (RQs), Table 6, Table 7, Table 8 , provide a summary details of each CRM category. These include year, author, brief description, participants, settings and the methods of data collection which directly respond to RQ2. To answer RQ3, we assigned plus (+) and minus (−) symbols to the findings column which indicate the positive and negative outcomes of each study.
Table 6.
Summary of e-CRM studies in healthcare
| Year | Author | Brief Description | Types of Evidence | Participants | Size (n) | Settings | Findings |
|---|---|---|---|---|---|---|---|
| 2001 | [69] | Explored e-CRM through PPS, and performed cost-benefit analysis on the quality and performance of PPS. | Case study. | Physicians. | – | Hospital. | (+)Physician-hospital relationship, medical operations, and patient satisfaction were improved significantly. (+)Better clinical outcomes found in nutrition, neurology; and orthopaedics. |
| 2012 | [70] | Proposed e-CRM model to determine patients’ expectations of e-health services. | Survey. | * Patient. * Patients’ family. * Medical staff. |
336 | * Hospital. * Homecare centre. |
(+)80% preferred to make appointments, payments, and view health promotions online. (+)75% preferred to view/control EMR and discuss health conditions on social networks. |
| 2015 |
[71] | Developed a framework and identified the key factors for e-CRM implementation. |
Survey. | * Managers. * Managing directors. * IT managers. |
150 | * Hospital. * Clinic. |
(+)Resistance to identifying e-CRM, support and involvement from top management, business goals, IT infrastructure, employee training, and patient focus were found to be the key factors. |
| 2018 | [72] | Proposed a framework for e- CRM adoption. | Conceptual framework | – | – | Hospital | (+)Proposed framework was based on TOE, diffusion of technology and institutional theories. (+)Technological factors such as complexity and relative advantage; organizational factors (size and management support); and environmental factors (regulatory and external pressure) are found be crucial for e-CRM adoption. |
| 2019 | [73] | Proposed a framework for e-CRM implementation. | Conceptual framework | – | – | Hospital | (+)Proposed framework was based on TOE, diffusion of technology and IS success theories. (+)Technological factors such as compatibility, interactivity and privacy; organizational factors (management support, social media policy and leadership knowledge) and environmental factors (social trust and bandwagon pressure) are found be crucial for e-CRM implementation. |
* Sample size (n), Positive result (+).
Table 7.
Summary of studies related to implementing CRMS in healthcare.
| Year | Author | Brief description | Types of evidence | Participants | Size (n) | Settings | Results |
|---|---|---|---|---|---|---|---|
| 2005 | [74] | Established a framework to support CRM implementation from 3 aspects of CM, DM, and CSM. | *Interview (Experts) *Survey (structured) |
*CRM expert. *Nurse. *Manager. *Nurse supervisor. |
* 7 *93 |
Nursing home |
(+)Implementing CRM requires leadership and the right culture to employ its features (CM, DM, and CSM). (−)Most nursing homes have yet to implement CRMS. (−)Computerisation requires more effort. |
| 2012 | [78] | Adopted SSDM to evaluate the steps of implementing CRM, which involved 4 phases and 10 systematic steps. | Case study | – | – | Health examination organisation | (+)All developed procedures positively measured/evaluated CRM models, improved efficiency, and provided better services for health organisations. |
| 2012 | [79] | Explored the key factors of implementing CRMS and developed a CRM model based on (i) features of the organisation, (ii) features of the application, and (iii) customer characteristics. | Interview (Experts) | *HIS Professional *CITO. *CEO. |
35 | Hospital | (+)Highest priority and most important factors were the hospital's resources, followed by management. (−)Patient involvement had no significant impact on implementing CRM. (−)Lack of measurement models for executing CRM. |
| 2013 | [80] | Applied the IS success model to assess CRM from 3 aspects (i) system characteristics, (ii) users, and (iii) performance. | Survey | CRMS user. | 243 | Health promotion centre | (+)Of system characteristics, only IQ and SQ had a significant influence on and relationship with perceived usefulness and user satisfaction. (+)Perceived usefulness and user satisfaction had a significant effect on personal performance, as well as an indirect influence on organisational performance. |
| 2013 | [77] | Adapted a value characteristic framework to support CRM implementation based on aspects of CM, DM, and CSM, and linked each characteristic to a specific CRM solution type. | Survey (In-depth) | *Manager. *Nurse Supervisor. |
93 | Nursing home. | (+)The most important dimensions were (i) the behaviour of service personnel; (ii) the design of care processes; and (iii) support from related units. (+)The most executed CRM features were (i) collecting customer data; (ii) the behaviour of service personnel; and (iii) the design of care processes. (−)The most underachieved factors were (i) data analysis; (ii) care service strategy, and (iii) KM. |
| 2013 | [81] | Evaluated CRM implementation and adapted a CRM scale based on 4 dimensions of CRM (i) key customer focus, (ii) CRM organisation, (iii) technology-based CRM, and (iv) KM. |
Survey (Post-mail) | Staff members | *141 *474 |
* Hospital-based nursing home * Privately-run nursing home |
(+)Hospital-based nursing homes leaned toward understanding patient needs and delivering prompt medical services through knowledge learning. (+)Private nursing homes focused on CRM organisation and technology-based CRM for building relationships. |
| 2016 | [83] | Introduced a CRM implementation model that consists of 7 components; Customer satisfaction, loyalty, trust, expectations, perceptions, perceived quality and Architecture. | Survey | Patients. | 303 | Hospital | (+)All 7 components were found significant and have relationship with each other. |
| 2017 | [84] | Designed a CRM implementation model based on HR factors such as employee satisfaction, organizational culture, communication management, empowerment, organizational commitment, organizational structure and change management. | Survey | Managers. | 215 | University hospital. | (+)HRM plays a crucial role in the implementation of CRM. (+)All of the investigated factors have influenced the implementation of CRM (+)Employee satisfaction had the highest influence (−)Organizational mission had the lowest influence. |
| 2017 | [85] | Analysed the factors that influence the implementation of CRM based on software aspects. | Survey | *Patient. *CRM user. |
100 | Hospital | (+)Operational efficiency, centralization of data, management of existing customer and hospital image were found to have a significant influence on the implementation of CRM. |
| 2017 | [86] | Evaluated the effects of CRM implementation on customer trust, loyalty, satisfaction and organisational productivity. | Survey | Nurse. | 268 | Hospital | (+)Customer satisfaction and diversification have the highest effects on CRM implementation. (−)Organisational productivity had the lowest impact |
| 2018 | [87] | Investigated various impacts and benefits of implementing CRM. | Survey | *Doctor *Administrator *IT staff |
578 | Hospital | (+)Waiting time reduction, better doctor allocation, and patient satisfaction were the major implication of CRM implementation in hospitals. |
* Sample size (n), Positive result (+), Negative result (−).
Table 8.
Summary of studies related to adopting CRMS in healthcare.
| Year | Author | Brief description | Types of evidence | Participants | Size (n) | Settings | Results |
|---|---|---|---|---|---|---|---|
| 2010 | [21] | Examined key factors for adopting CRMS and proposed an integrated model that incorporated two components (i) characteristics of CRMS and (ii) characteristics of organisation. | Survey (Online) | IS executive. | 95 | *Regional hospital. *Community hospital. *Medical centre. |
(+)39 hospitals adopted CRMS. (−)56 did not adopt CRMS. (+)5 factors (relative advantages; hospital size; innovation of senior executives; IS capabilities of staff; and KM capabilities) have significantly influenced the adoption of CRMS. |
| 2015 | [88] | Developed a model to examine the influence of external, technology, and organisations factors on CRM adoption. | Survey | Top management. | 103 | Hospital. | (−)Only Web-based CRMS was adopted. (+)Organisation and technology factors have a significant influence and relationship on the adoption of CRMS. (−)External factors were found to be insignificant. |
| 2015 | [89] | Examined the relationship between CRMS adoption, perception and organisation performance. | Survey | Top management. | 103 | Hospital. | (+)Significant relationship between organisation performance and CRMS adoption were found. (+)Significant relationship between CRMS adoption and CRMS perception were also found. |
Sample size (n), Positive result (+), Negative result (−).
4. Discussion
4.1. Findings related to RQ1, RQ2 and RQ3
Our analysis of the current literature indicates that there are significant gaps in knowledge regarding CRM in the healthcare environment. We found three main CRM research categories: (1) e-CRM (N = 5, 26%); (2) implementing CRM (N = 11, 58%); and (3) adopting CRM (N = 3, 16%). We proposed an introductory framework that organises all three aspects.
Fig. 9 presents a framework for categorising CRM research in the healthcare environment, beginning with social web-based CRM (e-CRM). This means that all CRM applications, functions and features are used through the internet environment. This also suggests that hospitals should manage all forms of communication and relationships with their patients through Web 2.0 and social media technologies. Consistent with this, Kohli et al. [69] explored a Web-based CRM application called a PPS, finding positive results in several areas, such as the physician-hospital relationship, medical operations, patient satisfaction, and clinical outcomes (especially in nutrition and neurology). However, the results of this study were based on physician case studies, and empirical data from a cost/benefit analysis of PPS performance during and after its implementation. It would have been more efficient if patients were involved in the case study, to know whether executing PPS had a direct influence and/or relationship with patients. Adding to this, Anshari et al. [70] proposed a CRM 2.0 model to determine patient expectations of e-health services. This study also showed a positive outcome regarding empowerment of patients through the web, given that more than 70% of participants (patients) wished to view their electronic medical records online, as well as make appointments and payments, and obtain consultations and referrals. Only one study proposed a framework for establishing social CRM (i.e. eCRM), and identified key factors based on importance and priorities [71]. Hence, more research is needed to better understand this element in healthcare organisations.
Fig. 9.
CRM research categories framework in the healthcare environment.
Our analysis and evaluation revealed that (i) physician interaction, cleanliness, and nursing were the most significant factors that influenced patients’ choice of hospital, patient satisfaction, and service quality (SQ). (ii) Paediatrics, cardiology, and neurology were the most significant medical preferences and key competitive advantages obtained by hospitals. (iii) Management (i.e. support and involvement), resources (I.e. IT infrastructure), and employee training factors were the most substantial aspects that influenced the implementation of CRM systems, as well as e-CRM. (iv) Hospital size, the medical staff's IS capacity, and knowledge management (KM) capabilities were the most significant factors that impacted the adoption of CRM systems. (v) Collecting patient's data was the most executed CRM feature in the healthcare environment, while data analysis was the most underachieved.
4.2. Strengths and limitations of this study
This appears to be the first systematic review to comprehensively synthesise and summarise the empirical evidence available for CRM research in the healthcare environment. Our search strategy was broad, examining several databases, search engines, platforms and academic journals, striving to find published and unpublished studies based on various CRM concepts, locations and settings. For each selected study, we provided a critical appraisal of its methodology and data, sampling, data analysis, ethics and bias, findings and implications and usefulness. In addition, we highlighted each study's methodological strengths and weaknesses. We have also identified studies with positive and negative outcomes, which will help hospitals and policymakers to better understand the benefits of implementing CRMS.
Despite its strengths, our study also faces some limitations. First, we believe that the matter of the potential exclusion of studies that were not in English and from conference proceedings has been addressed at academic gatherings and in other languages, such as Chinese and French. Second, our critical appraisal showed the quality of selected studies varies from ‘fair’ to ‘poor’. However, our sensitivity analysis did not show that excluding conference proceedings and including ‘poor’ quality studies affected our results. Last, our review may have a publication bias because studies with positive outcomes are more frequently published than negative ones; however, the studies that we found that had positive outcomes had several weaknesses in terms of methodology, sampling, and data analysis.
4.3. Recommendations for future research
We suggest the population-intervention-comparison-outcome (PICO) framework (see Table 9 ) to help scholars form research questions when planning future investigations involving CRM in the healthcare environment. According to [90,91] the PICO framework is widely used in medical/healthcare informatics and health research to help state the terms of reference, define the scope and manage research questions, search strategies, and eligibility criteria.
Table 9.
PICO frame for CRM research in the healthcare environment
| Criteria | Description |
|---|---|
| Population | Patient; medical professionals (physician and nurse); medical staffs; and management. |
| Intervention | e-CRM; implementation; and adoption. |
| Comparison (if any) | Electronic medical records (EMR); and electronic patient records (EPR). |
| Outcome | Patient satisfaction; patient loyalty; relationship and communication; medical staff satisfaction; service quality; health outcomes; chronic illness. |
Our analysis showed that issues such as the privacy and security of patients, and their roles in CRMS development, were not yet investigated by the selected studies. Today, more and more of patient personal and health information (PHI) is being stored in CRMS, many of these data are created by doctors, clinics and hospitals and they offer plenty of advantages such as reducing medical mistakes, sharing information easier and offering better care. Whether PHI is maintained in a paper record or an electronic health record, patients have the right to keep it private, and that privacy is protected by laws called health insurance portability and accountability act (HIPPA) [92] and general data protection regulation (GDPR) [93]. These laws require that certain healthcare providers keep PHI private and secure encrypted form and proper journalised history from its inception. Firewalls, strong encryption, secure login, access control and authentication mechanisms are some of the security measures that healthcare providers may or should use to protect the privacy of patients when implementing CRMS. As patient's privacy continues to evolve, certain policies and guidelines need to be followed to properly control access, disclose and protect PHI under all circumstances to avoid misuse and litigations. Hence, we suggest that future research further focuses on patient public and private information, privacy and security perceptions and how these might influence the implementation and adoption of CRMS in open environments.
Our results also revealed that only organisational and technological factors have been examined using a quantitative method (such as survey), with no formidable theoretical base used (except for 4 studies, which applied the IS success model and TOE theory). We encourage researchers to use different methods more readily to explore other potential factors such as culture and trust to determine how they might influence decision-making, and also to apply a greater variety of theories.
With the increasing number of wearable devices, smart phones and mobile applications (apps), ICT services, the mobile health (mHealth) domain is rapidly developing and gaining momentum at rapid speed as can be observed during the global 2020 coronavirus (CONVID-19) spread. Yet, none of the included studies have addressed mobile CRM (m-CRM) in health care in a consistent and systematic manner. Many studies on mobile health have showed promising results in heart pace monitoring, body weight, blood pressure, and heart disease monitoring [94]. We believe patient with chronic illness could greatly benefit from m-CRM in multiple ways, allowing for immediate medical responses and new symptom and diagnoses detection methods and procedures. Therefore, we recommend more research that addresses m-CRM in healthcare functionality and the issue of privacy and security of both patients as well as all healthcare workers. This might also require a set of de facto and/or international standards to be developed not only in m-CRM and e-CRM domains but everything spanning this phenomenon.
5. Conclusions
In this study, we aimed to review, categorise, summarise, synthesise, and appraise CRM research in the healthcare environment. This SLR was performed by following the criteria of preferred reporting items for systematic reviews and meta-analysis (PRISMA) [61,62]. Our initial search identified 1,642 records, and 40 further studies from manual journals and reference lists search. Our search and selection process went through different phases to degrade the findings. In total, 19 studies were carefully identified and analysed. Each study was evaluated by following the criteria of quality assessment tools for undertaking a systematic review of disparate data developed by Hawker et al. [66]. The findings were qualitatively and quantitatively organised based on three main research categories; e-CRM (Web-based CRM), implementing CRMS, and adopting CRMS. The selected studies were published between 2000 and 2020. Our results indicate that research and development on CRM within the healthcare environment is still in its early stages in uncharted waters, and more research would be helpful. This SLR provides several insights and recommendations for researchers, healthcare institutions, service providers, policymakers, ICT developers and suppliers.
Authors statement
The authors, individually or jointly, have no institutional, financial and personal relationships with other persons, organizations and sponsoring or funding agencies, other than acknowledging such agencies in the manuscript for their generosity funding the research work upon which the manuscript is based. In addition, we hereby declare that the manuscript has not been submitted to any other journal, conference proceedings or books for publication. It is solely the work of the authors.
Declaration of Competing Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Acknowledgments
This work was funded by the Researchers Supporting Project (RSP-2019/102), King Saud University, Riyadh, Saudi Arabia.
Biographies

Yahia Baashar received the B.S. degree in network computing and the master's degree in management information systems from Coventry University, INTI International University, Malaysia. He is currently pursuing the Ph.D. degree in industrial science with The Energy University (UNITEN), Malaysia. He has published in journals and conferences. His research interests include technology acceptance, medical informatics, e-health, artificial intelligence, and machine learning.

Hitham Alhussian received the B.Sc. and M.Sc. degrees in computer science from the School of Mathematical Sciences, Khartoum University, Sudan, and the Ph.D. degree from Universiti Teknologi Petronas, Malaysia, where he is currently a Senior Lecturer with the Computer and Information Sciences Department and Core research member of Centre in Research and Data Science (CERDAS). His main research interests are in real-time parallel distributed systems, cloud computing, big data mining, machine learning and secure computer-based management systems.

Ahmed Patel received his M.Sc. and Ph.D. degrees in Computer Science from Trinity College Dublin (TCD), University of Dublin in 1978 and 1984 respectively, specializing in the design, implementation and performance analysis of packet switched networks. He is Research Professor at Universidade Estadual do Ceará, Fortaleza, Brazil with key research interest in Advanced Computer Networking, Internet of Things, Cloud Computing, Big Data, Predictive Analysis, Use of Advanced Computing Techniques, Impact of e-social Networking, Closing the digital divide ICT gap and ICT Project Management. He has published well-over 272 technical and scientific papers and co-authored three books, two on computer network security and the third on group communications. He co-edited one book on distributed search systems for the Internet and also co-edited and co-authored another book entitled: “Securing Information and Communication Systems: Principles, Technologies and Applications”. He is a member of the Editorial Advisory Board of International Journals and has participated in Irish, Malaysian, Brazilian and European funded research projects.

Gamal Alkaws received the B.S. degree in software engineering and the master's degree in management information systems from Coventry University, INTI, Malaysia, and the Ph.D. degree in information communication technology from The Energy University (UNITEN), Malaysia, in 2019. He is currently a Postdoctoral Researcher with The Energy University (UNITEN). He has published in journals and conferences. His research interests include emerging technology acceptance, user behaviour, adoption of information systems in organizations, the IoT, artificial intelligence, and machine learning.

Ahmed Ibrahim Alzahrani received the master's and Ph.D. degrees in computer science from Western Illinois University, USA, and De Montfort University, U.K., respectively. He is currently an Associate Professor with the Department of Computer Science, Community College, King Saud University. He acts as the Head of the Informatics Research Group, and a member of the Scientific Council-King Saud University. His main research interests span over IT diffusion and innovation, information technology management, human behaviour modelling in technology usage, online social networks, and humancomputer interaction using cognitive research.

Osama Alfarraj received the master's and Ph.D. degrees from Griffith University, in 2008 and 2013, respectively, all in information and communication technology. He is currently an Associate Professor of computer science with King Saudi University, Riyadh, Saudi Arabia. His current research interests include e-Systems (e-Gov, e-Health, and e-commerce), cloud computing, and big data. He served as a consultant for two years and a member of the Saudi National Team for Measuring E-Government, Saudi Arabia.

Gasim Hayder is Charted Engineer (C.Eng.) and a senior lecturer in Civil Engineering Department, College of Engineering, Universiti Tenaga Nasional (UNITEN). He also served as Head of Postgraduate and Laboratory Services Unit in the Institute of Energy and Infrastructure (IEI), Head of Water and Environmental Engineering Unit in the Department of Civil Engineering, and senior researcher for Sustainable Engineering Group UNITEN. He has working experience in engineering practices, teaching and management including as Construction Engineer, Senior Engineer, Technical Manager (multinational company), Graduate Assistant, Research Assistant, Treatment Process Specialist Consultant and Senior Lecturer. He has several publications, patents and awards in both national and international levels. His research interests are Environmental Engineering, Wastewater treatment, Biological processes, Solid Waste Management.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.csi.2020.103442.
Appendix. Supplementary materials
Reference
- 1.Mettler T. Anticipating mismatches of HIT investments: Developing a viability-fit model for e-health services. Int. J. Med. Inf. 2016;85(1):104–115. doi: 10.1016/j.ijmedinf.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 2.M. Skeels and D. S. Tan, "Identifying opportunities for inpatient-centric technology," in Proceedings of the 1st ACM International Health Informatics Symposium, 2010: ACM, pp. 580-589.
- 3.Ahtonen A. Healthy and active ageing: turning the ‘silver'economy into gold’. Policy Brief. 2012;12 [Google Scholar]
- 4.Ahtonen A. European Policy Centre; Brussels: 2013. Economic Governance: Helping European Healthcare Systems to Deliver Better Health and Wealth? [Google Scholar]
- 5.Chavannes N.H., Du Puy R.S., Bai C. Suggestions for health information technology trials for respiratory disorders in low-and middle-income country settings: what can we learn from trials in high-income country settings? NPJ Prim. Care Respir. Med. 2015;25:15045. doi: 10.1038/npjpcrm.2015.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldschmidt P.G. HIT and MIS: implications of health information technology and medical information systems. Commun. ACM. 2005;48(10):68–74. [Google Scholar]
- 7.Chaudhry B., et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann. Intern. Med. 2006;144(10):742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 8.LeRouge C., Hevner A.R., Collins R.W. It's more than just use: An exploration of telemedicine use quality. Decis. Supp. Syst. 2007;43(4):1287–1304. [Google Scholar]
- 9.Hillestad R., et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Affairs. 2005;24(5):1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 10.Carayon P., Smith P., Hundt A.S., Kuruchittham V., Li Q. Implementation of an electronic health records system in a small clinic: the viewpoint of clinic staff. Behav. Inf. Technol. 2009;28(1):5–20. [Google Scholar]
- 11.Holden R.J. Physicians’ beliefs about using EMR and CPOE: in pursuit of a contextualized understanding of health IT use behavior. Int. J. Med. Inf. 2010;79(2):71–80. doi: 10.1016/j.ijmedinf.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lau F., Kuziemsky C., Price M., Gardner J. A review on systematic reviews of health information system studies. J. Am. Med. Inf. Assoc. 2010;17(6):637–645. doi: 10.1136/jamia.2010.004838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dahlan A., Rahman A., Abdulatif Z.K., Mahmoud I., Aydin M. Collaborative healthcare system between clinics and hospitals in Malaysia. Int. J. Comput. Intell. Inf. Secur. 2011;2(2):92–100. [Google Scholar]
- 14.Lake T.K., Higgins T.C., Ginsburg P.B. Mathematica Policy Research; 2011. Fostering Health Information Technology in Small Physician Practices: Lessons From Independent Practice Associations. [Google Scholar]
- 15.Esmaeilzadeh P., Sambasivan M. Healthcare professionals’ adoption of clinical IT in hospital: a view of relationship between healthcare professionals and hospital. Management. 2012;2(5):161–170. [Google Scholar]
- 16.Tsai M.-F., Hung S.-Y., Yu W.-J., Chen C., Yen D.C. Understanding physicians’ adoption of electronic medical records: Healthcare technology self-efficacy, service level and risk perspectives. Comput. Stand. Interfaces. 2019;66 [Google Scholar]
- 17.L. P. Jarrell, “Customer Relationship Management in Healthcare,” 2009, https://www.scribd.com/document/325017343/CRM-MArketting-pdf.
- 18.Jimison H.B., Sher P.P. Consumer health informatics: health information technology for consumers. J. Am. Soc. Inf. Sci. 1995;46(10):783. [Google Scholar]
- 19.Hibbard J.H. Engaging health care consumers to improve the quality of care. Med. Care. 2003;41(1):I-61-I-70. doi: 10.1097/00005650-200301001-00007. [DOI] [PubMed] [Google Scholar]
- 20.Clancy C. How patient-centered healthcare can improve quality. Patient Saf. Qual. Healthc. 2008;5(2):6–7. [Google Scholar]
- 21.Hung S.-Y., Hung W.-H., Tsai C.-A., Jiang S.-C. Critical factors of hospital adoption on CRM system: Organizational and information system perspectives. Decis. Supp. Syst. 2010;48(4):592–603. [Google Scholar]
- 22.Benz G., Paddison N. Developing patient-based marketing strategies. Healthc. Execut. 2004;19(5):40. 42. [PubMed] [Google Scholar]
- 23.Yina W. Proceedings of the 2010 Second International Conference on Multimedia and Information Technology (MMIT) Vol. 1. 2010. Application of customer relationship management in health care; pp. 52–55. IEEE. [Google Scholar]
- 24.T. R. Vardasca and H. M. Martins, "Patient Relationship Management in public healthcare settings," in Proceedings of the 2011 IEEE International Conference on Communications (ICC), pp. 1-4.
- 25.M. A. McDonald, “Service quality and customer lifetime value in professional sport franchises,” 1996. Doctoral Dissertations Available from Proquest. AAI9709627. https://scholarworks.umass.edu/dissertations/AAI9709627.
- 26.Tiu Wright L., Ouschan R., Sweeney J., Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur. J. Mark. 2006;40(9/10):1068–1086. [Google Scholar]
- 27.Haridasan V., Venkatesh S. CRM implementation in Indian telecom industry–evaluating the effectiveness of mobile service providers using data envelopment analysis. Int. J. Bus. Res. Manag. 2011;2(3):110–127. [Google Scholar]
- 28.Beldi A., Cheffi W., Dey P.K. Managing customer relationship management projects: the case of a large French telecommunications company. Int. J. Project Manag. 2010;28(4):339–351. [Google Scholar]
- 29.Blery E.K., Michalakopoulos M.G. An e-CRM application in the telecommunications sector: A case study from Greece. EuroMed. J. Bus. 2006;1(2):5–14. [Google Scholar]
- 30.Vella J., Caruana A. Encouraging CRM systems usage: a study among bank managers. Manag. Res. Rev. 2012;35(2):121–133. [Google Scholar]
- 31.Roy S.K., Padmavathy C., Balaji M., Sivakumar V. Measuring effectiveness of customer relationship management in Indian retail banks. Int. J. Bank Mark. 2012;30(4):246–266. [Google Scholar]
- 32.Malhotra N., Ho C.-T.B. Proceedings of the 8th International Conference on Supply Chain Management and Information Systems (SCMIS) 2010. Factors and barriers affecting the implementation of CRM-Taiwan banking industry; pp. 1–7. IEEE. [Google Scholar]
- 33.Xiaohui W., Yong Z. Proceedings of the 2009 International Forum on Information Technology and Applications. 2009. The implementation of CRM in city commercial banks; pp. 479–482. IEEE. [Google Scholar]
- 34.Geib M., Kolbe L.M., Brenner W. CRM collaboration in financial services networks: a multi-case analysis. J. Enterp. Inf. Manag. 2006;19(6):591–607. [Google Scholar]
- 35.Blery E., Michalakopoulos M. Customer relationship management: a case study of a Greek bank. J. Financ. Serv. Mark. 2006;11(2):116–124. [Google Scholar]
- 36.Zineldin M. Quality and customer relationship management (CRM) as competitive strategy in the Swedish banking industry. TQM Mag. 2005;17(4):329–344. [Google Scholar]
- 37.Karakostas B., Kardaras D., Papathanassiou E. The state of CRM adoption by the financial services in the UK: an empirical investigation. Inf. Manag. 2005;42(6):853–863. [Google Scholar]
- 38.Stein A., Smith M. CRM systems and organizational learning: An exploration of the relationship between CRM effectiveness and the customer information orientation of the firm in industrial markets. Ind. Mark. Manag. 2009;38(2):198–206. [Google Scholar]
- 39.Chung Y., Tien S., Tsai C., Tang L. An empirical study of customer relationship management implementation in taiwan's machine industry. J. Bus. Publ. Affairs. 2007;1(1):1–12. [Google Scholar]
- 40.Schellong A. Proceedings of the 2005 National Conference on Digital Government Research. Digital Government Society of North America; 2005. CRM in the public sector: towards a conceptual research framework; pp. 326–332. [Google Scholar]
- 41.Sundar P.K., Murthy H.N., Yadapadithaya P. CRM success factors in software services firm: a case study analysis. Inf. Knowl. Manag. 2012;2(8):33–39. Citeseer. [Google Scholar]
- 42.Saeednia H., Dastjerdi A., Jafari Sohi A. Prioritization of effective factors on CRM implementation in Parsian international hotels company in Tehran. Int. J. Manag. Bus. Res. 2012;2(1):13–22. [Google Scholar]
- 43.Li L., Mao J.-Y. The effect of CRM use on internal sales management control: An alternative mechanism to realize CRM benefits. Inf. Manag. 2012;49(6):269–277. [Google Scholar]
- 44.Pai J.-C., Tu F.-M. The acceptance and use of customer relationship management (CRM) systems: an empirical study of distribution service industry in Taiwan. Exp. Syst. Appl. 2011;38(1):579–584. [Google Scholar]
- 45.Piskar F., Faganel A. A successful CRM implementation project in a service company: case study. Organizacija. 2009;42(5):199–208. [Google Scholar]
- 46.Liu L., Stroulia E., Nikolaidis I., Miguel-Cruz A., Rincon A.R. Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med. Inf. 2016;91:44–59. doi: 10.1016/j.ijmedinf.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 47.Khosravi P., Ghapanchi A.H. Investigating the effectiveness of technologies applied to assist seniors: A systematic literature review. Int. J. Med. Inf. 2016;85(1):17–26. doi: 10.1016/j.ijmedinf.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 48.Gagnon M.-P., Ngangue P., Payne-Gagnon J., Desmartis M. m-Health adoption by healthcare professionals: a systematic review. J. Am. Med. Inf. Assoc. 2016;23(1):212–220. doi: 10.1093/jamia/ocv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eden K.B., et al. Barriers and facilitators to exchanging health information: a systematic review. Int. J. Med. Inf. 2016;88:44–51. doi: 10.1016/j.ijmedinf.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baysari M.T., Lehnbom E.C., Li L., Hargreaves A., Day R.O., Westbrook J.I. The effectiveness of information technology to improve antimicrobial prescribing in hospitals: A systematic review and meta-analysis. Int. J. Med. Inf. 2016;92:15–34. doi: 10.1016/j.ijmedinf.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 51.West V.L., Borland D., Hammond W.E. Innovative information visualization of electronic health record data: a systematic review. J. Am. Med. Inf. Assoc. 2015;22(2):330–339. doi: 10.1136/amiajnl-2014-002955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salahuddin L., Ismail Z. Classification of antecedents towards safety use of health information technology: A systematic review. Int. J. Med. Inf. 2015;84(11):877–891. doi: 10.1016/j.ijmedinf.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 53.Nguyen C., McElroy L.M., Abecassis M.M., Holl J.L., Ladner D.P. The use of technology for urgent clinician to clinician communications: A systematic review of the literature. Int. J. Med. Inf. 2015;84(2):101–110. doi: 10.1016/j.ijmedinf.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fritz F., Tilahun B., Dugas M. Success criteria for electronic medical record implementations in low-resource settings: a systematic review. J. Am. Med. Inf. Assoc. 2015;22(2):479–488. doi: 10.1093/jamia/ocu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brenner S.K., et al. Effects of health information technology on patient outcomes: a systematic review. J. Am. Med. Inf. Assoc. JAMIA. 2015;23(5):1016–1036. doi: 10.1093/jamia/ocv138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ingebrigtsen T., et al. The impact of clinical leadership on health information technology adoption: systematic review. Int. J. Med. Inf. 2014;83(6):393–405. doi: 10.1016/j.ijmedinf.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 57.Hyppönen H., et al. Impacts of structuring the electronic health record: A systematic review protocol and results of previous reviews. Int. J. Med. Inf. 2014;83(3):159–169. doi: 10.1016/j.ijmedinf.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 58.Soltani Z., Navimipour N.J. Customer relationship management mechanisms: A systematic review of the state of the art literature and recommendations for future research. Comput. Hum. Behav. 2016;61:667–688. [Google Scholar]
- 59.Pope C., Mays N., Popay J. McGraw-Hill Education; UK: 2007. Synthesising Qualitative and Quantitative Health Evidence: A Guide to Methods: A Guide to Methods. [Google Scholar]
- 60.Mays N., Pope C., Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J. Health Serv. Res. Policy. 2005;10(suppl 1):6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 61.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 62.Liberati A., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med. 2009;151(4):W-65-W-94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 63.Dixon-Woods M., Agarwal S., Jones D., Young B., Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J. Health Serv. Res. Policy. 2005;10(1):45–53B. doi: 10.1177/135581960501000110. [DOI] [PubMed] [Google Scholar]
- 64.Pawson R., Greenhalgh T., Harvey G., Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J. Health Serv. Res. Policy. 2005;10(suppl 1):21–34. doi: 10.1258/1355819054308530. [DOI] [PubMed] [Google Scholar]
- 65.Rodgers M., et al. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews effectiveness of interventions to promote smoke alarm ownership and function. Evaluation. 2009;15(1):49–73. [Google Scholar]
- 66.Hawker S., Payne S., Kerr C., Hardey M., Powell J. Appraising the evidence: reviewing disparate data systematically. Qual. Health Res. 2002;12(9):1284–1299. doi: 10.1177/1049732302238251. [DOI] [PubMed] [Google Scholar]
- 67.Higgins J.P., Green S. Wiley Online Library; 2008. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- 68.Askool S., Nakata K. A conceptual model for acceptance of social CRM systems based on a scoping study. AI Soc. 2011;26(3):205–220. [Google Scholar]
- 69.Kohli R., Piontek F., Ellington T., VanOsdol T., Shepard M., Brazel G. Managing customer relationships through E-business decision support applications: a case of hospital–physician collaboration. Decis. Supp. Syst. 2001;32(2):171–187. [Google Scholar]
- 70.M. Anshari, M. N. Almunawar, P. K. Low, and Z. Wint, "Customer Empowerment in Healthcare Organisations Through CRM 2.0: Survey Results From Brunei Tracking a Future Path in e-Health Research," arXiv preprint arXiv:1207.6164, 2012.
- 71.Hosseinianzadeh M. A Framework for e-CRM Implementation in health service industry of a developing country. Int. J. Eng. Innov. Technol. (IJEIT) 2015;4(8) [Google Scholar]
- 72.Jalal A.N., Bahari M., Tarofder A.K. Vol. 1. 2018. Investigating the Crucial Factors Affecting the Social CRM Implementation and Its Benefits in Iraqi Healthcare Industry; p. 50. (1st Malaysia Doctoral Consortium for Information Systems, Association for Information Systems - Malaysia Chapter). [Google Scholar]
- 73.Jalal A.N., Bahari M., Tarofder A.K., Musa W.M.N.M.W. Factors influencing customer social relationship management implementation and its benefits in healthcare industry. Polish J. Manag. Stud. 2019;19 [Google Scholar]
- 74.Cheng B.-W., Chang C.-L., Liu I.-S. Establishing customer relationship management framework in nursing homes. Total Qual. Manag. Bus. Excell. 2005;16(5):607–629. [Google Scholar]
- 75.Rigby D.K., Reichheld F.F., Schefter P. Avoid the four perils of CRM. Harvard Bus. Rev. 2002;80(2):101–109. [PubMed] [Google Scholar]
- 76.Campbell A.J. Creating customer knowledge competence: managing customer relationship management programs strategically. Ind. Mark. Manag. 2003;32(5):375–383. [Google Scholar]
- 77.Gulliver S.R., Joshi U.B., Michell V. Adapted customer relationship management implementation framework: facilitating value creation in nursing homes. Total Qual. Manag. Bus. Excell. 2013;24(9-10):991–1003. [Google Scholar]
- 78.Lyu Jr -.J., Chao H.-L., Chen C.-W., Huang L.-Y. Developing a customer relationship management model for better health examination service. Nang Yan Bus. J. 2012;1(1):38–46. [Google Scholar]
- 79.Monem H., Hussin A., Sharifian R. Comprehensive prioritized perspectives of CRM system for implementation in the developing countries’ hospitals. Int. J. Comput. Appl. 2012;50(20):5–12. [Google Scholar]
- 80.Choi W., Rho M.J., Park J., Kim K.-J., Kwon Y.D., Choi I.Y. Information system success model for customer relationship management system in health promotion centers. Healthc. Inf. Res. 2013;19(2):110–120. doi: 10.4258/hir.2013.19.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang M.-L. An evaluation of customer relationship management in hospital-based and privately run nursing homes in Taiwan. Total Qual. Manag. Bus. Excell. 2013;24(9-10):1004–1021. [Google Scholar]
- 82.Sin L.Y., Alan C., Yim F.H. CRM: conceptualization and scale development. Eur. J. Mark. 2005;39(11/12):1264–1290. [Google Scholar]
- 83.Zamani E., Tarokh M.J. Analysis of customer relationship management in hospitals and present an efficient model for CRM implementation in hospitals. Bull. Soc. R. Sci. Liège. 2016;85:1448–1456. [Google Scholar]
- 84.Taghavi S., Riahi L., Nasiripour A.A., Jahangiri K. Modeling customer relationship management pattern using human factors approach in the hospitals of Tehran university of medical sciences. Health Scope. 2017;6(2) [Google Scholar]
- 85.Gandhi P., Tandon N. Study to analyze the variables that affect the CRM implementation in the hospitals. Adv. Comput. Sci. Technol. 2017;10(5):933–944. [Google Scholar]
- 86.Yaghoubi M., Asgari H., Javadi M. The impact of the customer relationship management on organizational productivity, customer trust and satisfaction by using the structural equation model: A study in the Iranian hospitals. J. Educ. Health Promot. 2017;6 doi: 10.4103/jehp.jehp_32_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.R. JIMS and K. JIMS, "Impact of CRM on Hospitals: A Study Conducted to Gain View of the Practitioners Working in Various Private and Govt. Hospitals in Delhi. Priyanka Gandhi Dr. Neelam Tandon Assistant Professor Professor," 2018.
- 88.Alkhazali A.R., Hassan S. Factors affecting customer relationship management perception: a study of Jordnian hospital sector. J. Manag. Sustain. 2015;5(3):p126. [Google Scholar]
- 89.Alkhazali A.R., Hassan S. The effect of customer relationship management system adoption and perception on organization performance: Study of Jordanian hospital sectors. J. Manag. Sustain. 2015;5:141. [Google Scholar]
- 90.Bettany-Saltikov J. McGraw-Hill Education; UK: 2012. How to do a Systematic Literature Review in Nursing: A Step-by-Step Guide. [Google Scholar]
- 91.Turner T., Misso M., Harris C., Green S. Development of evidence-based clinical practice guidelines (CPGs): comparing approaches. Implem. Sci. 2008;3(45):1–8. doi: 10.1186/1748-5908-3-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nosowsky R., Giordano T.J. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule: Implications for Clinical Research. Ann. Rev. Med. 2006;57(1):575–590. doi: 10.1146/annurev.med.57.121304.131257. [DOI] [PubMed] [Google Scholar]
- 93.Larrucea X., Moffie M., Asaf S., Santamaria I. Towards a GDPR compliant way to secure European cross border Healthcare Industry 4.0. Comput. Stand. Interfaces. 2020;69 [Google Scholar]
- 94.Haddad S.M., Souza R.T., Cecatti J.G. Mobile technology in health (mHealth) and antenatal care-Searching for apps and available solutions: A systematic review. Int. J. Med. Inf. 2019 doi: 10.1016/j.ijmedinf.2019.04.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.