Abstract
Palliation of metastatic disease compromises a significant portion of radiation treatments in the United States. These patients present a unique challenge in resource-limited settings, as expeditious treatment is often required to prevent serious morbidity. In order to reduce the risk of infection with severe acute respiratory syndrome coronavirus-2 and maximize the benefit to patients, we present evidence-based recommendations for radiation in patients with oncologic emergencies. Radiation oncologists with expertise in the treatment of metastatic disease at a high-volume comprehensive cancer center reviewed the available evidence and recommended best practices for the treatment of common oncologic emergencies, with attention to balancing the risk of infection with severe acute respiratory syndrome coronavirus-2 and the potential morbidity of delaying treatment. Many prospective trials and national guidelines support the use of abbreviated courses of radiotherapy for patients with oncologic emergencies. As such, in the setting of the current coronavirus disease 2019 pandemic, the use of hypofractionated radiation therapy for patients requiring palliation for oncologic emergencies achieves desirable functional outcomes without compromising care.
Introduction
Radiation therapy (RT) is critical for the treatment of oncologic emergencies, including neurologic injury from cord compression or brain metastases, airway compromise, and bleeding.1, 2, 3, 4. Palliative RT for patients with limited functional status is crucial for providing effective care and limiting morbidity from disease progression. The current coronavirus disease 2019 (COVID-19) pandemic has heightened our awareness of resource constraints, prompting institutions to create guidelines to delay treatments whenever possible and prioritize cases that are clinically urgent.5, 6, 7, 8
Recent data from China and Italy have demonstrated that cancer patients have a higher risk of contracting the virus and a higher case-fatality rate.9, 10, 11, 12 It is therefore imperative to be judicious in the use of RT and to consider shorter courses of palliative RT for oncologic emergencies. Existing recommendations, such as those from the Choosing Wisely campaign, support the use of short-course RT as a component of value-based care.13 However, its use in the United States has been limited, and therefore cancer centers are less equipped to optimally manage patients considered for palliative radiation.8,14,15 Here, we aim to provide a more detailed departmental approach to triaging and shortening RT for oncologic emergencies at a major comprehensive cancer center in New York City, an epicenter of COVID-19 in the United States.
Methods and Materials
Radiation oncologists with expertise in the management of metastatic disease and inpatient oncologic emergencies at a high-volume comprehensive cancer center in the epicenter of the current COVID-19 outbreak convened to discuss best practices for this time. We reviewed high-impact evidence, prior systematic reviews, and national guidelines to compile recommended practices for the treatment of common oncologic emergencies. Although this was not a comprehensive systematic review of the literature, we discussed our individual institutional best practices in the unique circumstances of this global pandemic. Specific attention was given to balancing the risk of infection with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and the potential morbidity of delaying treatment.
Suggested considerations
Clinical evaluation
In response to departmental guidance to limit clinical exposure and maximize single-use personal protective equipment, the majority of patient assessments, including history of present illness, performance status, current symptoms, and imaging are being evaluated virtually via telemedicine. Prior studies have shown the feasibility and efficacy of assessing symptoms and performance status through electronic and telemedicine platforms.16, 17, 18 When in-person physical examination is crucial to treatment decision-making, including neurologic evaluation and pain assessments, patient encounters are limited to a single radiation oncologist or an advanced practice provider.
We recommend discussion of the patient’s overall prognosis and goals of care with the patient, the primary medical oncologist, and supportive care specialists before determining a radiation plan that uses the provider’s preferred validated prognostic models.19, 20, 21 For patients with an estimated life expectancy of days to weeks, best supportive care with medical therapies alone is encouraged.
For subsequent on-treatment visits and follow-ups, our institution has implemented telemedicine visits as default to reduce the risk of exposure. For patients needing urgent supportive care while receiving RT, a nursing visit or physician visit can be arranged with the designated rotating radiation oncology health care providers of the day. When face-to-face evaluation is clinically indicated, we recommend that all patients, caregivers, and providers adhere to institutional policies and Centers for Disease Control recommendations on social distancing, handwashing, assessment of personal risk factors, and use of appropriate personal protective equipment to mitigate risk of exposure of patients and staff.22
Patient triage
In the setting of the COVID-19 pandemic, our department developed and implemented a 3-tiered system to identify clinically urgent cases in which delaying treatment would result in compromised outcomes or serious morbidity. For patients with metastatic cancer requiring palliative RT, patients with oncologic emergencies are assigned with the tier 1 designation (Table 1). This includes patients with cord compression, symptomatic brain metastases requiring whole brain RT, life-threatening tumor bleeding, and malignant airway obstruction (Table 2). Tier 2 includes patients with symptomatic disease, exclusionary of oncologic emergencies for which RT is the standard of care, and patients with asymptomatic disease for which RT is recommended to prevent impending functional deficits. Tier 3 includes patients with symptomatic or asymptomatic disease for which RT is one of the effective treatment options.
Table 1.
Assignment of radiation tiers based on treatment indication
| Tier 1 (highest priority) | Patients with oncologic emergencies (neurologic compromise, tumor bleeding, airway compromise, etc) requiring palliative RT |
| Tier 2 | Patients with symptomatic disease exclusionary of oncologic emergencies for which RT is the standard of care Patients with asymptomatic disease for which RT is recommended to prevent impending functional deficit |
| Tier 3 (lowest priority) | Patients with symptomatic or asymptomatic disease for which RT is one of the effective treatment options |
Abbreviation: RT = Radiation therapy.
Table 2.
Hypofractionated palliative regimens
| Indication | Treatment | References |
|---|---|---|
| Brain metastases requiring whole brain RT | 4 Gy × 5 daily fractions steroids alone | Rades et al24: 20 Gy/5 fx well tolerated QUARTZ26: Steroids alone for patients with poor performance status |
| Cord compression | 8 Gy × 1 daily fraction | Maranzano et al, SCORAD III, ICORG 05-0330, 31, 32, 33: Similar effect on OS and post-RT motor functions. Retreatment is safe. |
| Tumor bleeding | 3.7 Gy × 4 twice daily fractions 4 Gy × 5 daily fractions |
RTOG 8502, RTOG 790534,35,43: “Quad Shot” is safe and effective. Avoid bid fractionation for COVID + patients. |
| SVC syndrome airway obstruction | 8.5 Gy × 2 weekly fractions 4 Gy × 5 daily fractions |
Sundstrom et al36,37: Equivalent symptom relief and no difference in survival compared with standard fractionation Exercise caution with COVID + patients |
| Bone metastases | 8 Gy × 1 daily fraction | RTOG 971413,38, 39, 40: 8 Gy × 1 similar efficacy in pain relief with less acute toxicity. Retreatment is safe. |
Abbreviations: COVID = coronavirus disease; ICORG = Cancer Trials Ireland (formerly All Ireland Cooperative Oncology Research Group); OS = overall survival; RT = radiation therapy; QUARTZ = Quality of Life after Treatment for Brain Metastases; RTOG = Radiation Therapy Oncology Group; SCORAD = Single-fraction Radiotherapy Compared to Multifraction Radiotherapy; SVC = superior vena cava.
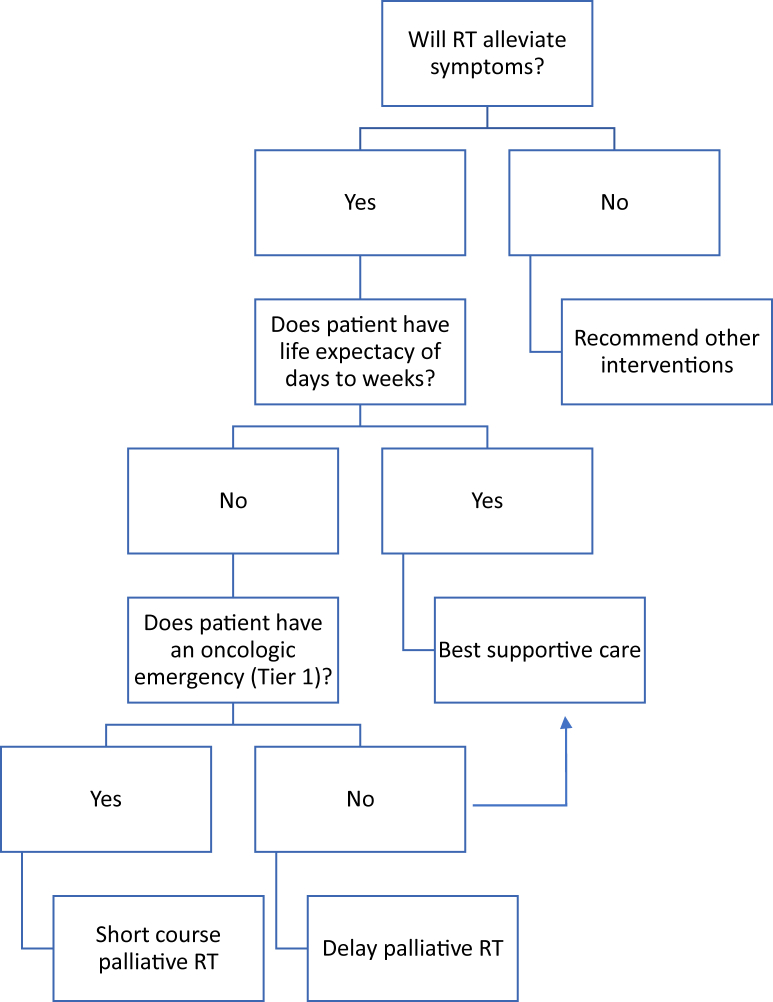
Need for urgent RT is guided by a simple triage flowsheet that includes active symptoms that can be addressed with RT, prognosis, goals of care, and tier 1 designation (Fig 1). The following management recommendations pertain to patients with oncologic emergencies, which are departmentally categorized with tier 1 designation.
Figure 1.
Triaging a patient with an oncologic emergency.
Management of oncologic emergencies
Brain metastases
The management of brain metastases has been an evolving clinical paradigm for which patient prognosis, histology, age, competing risks, and neurologic symptoms must be considered. For patients with favorable prognosis and for whom stereotactic radiosurgery is appropriate, we continue to provide stereotactic radiosurgery for patients and treat all or the dominant lesion(s) that are most likely to cause morbidity to delay or potentially avoid whole brain radiation. However, for patients with urgent indications, such as progressive neurologic symptoms from multiple brain metastases or leptomeningeal disease, whole brain radiation is often indicated. For these patients, particularly those who are hospitalized, 10-fraction treatment increases the risks for patients and staff exposure to SARS-COV-2. Thus, although several dose options are available, we favor 20 Gy in 5 fractions, which has been safely used in multiple studies.23,24 Standard fractionation (30 Gy in 10 fractions) with memantine could be considered for patients in whom longer term survival is expected in order to limit neurocognitive complications.25 For patients with limited prognosis, the Quality of Life after Treatment for Brain Metastases study demonstrated similar rates of overall survival and quality of life with steroids and best supportive care alone compared with whole-brain RT,26 and therefore observation is likely preferred to limit unnecessary exposure to SARS-COV-2.
Spinal cord compression
The management of patients with spinal cord compression requires multidisciplinary discussion especially with neurosurgery, and evaluation of several factors including degree of spinal cord compression and presence or absence of spinal instability. We used the Neurologic, Oncologic, Mechanical, and Systemic paradigm to facilitate selection of optimal treatment.27 If radiation is indicated, over 30 studies have shown equivalent functional outcomes of single-fraction radiation treatment instead of multifraction radiation treatment,4,28 with recent meta-analysis of 3 randomized clinical trials demonstrating preserved motor response with no clinical difference between single-fraction radiation treatment (8 Gy × 1 fraction) and multifraction treatment at a 2-month timepoint.29, 30, 31, 32, 33 However, there is conflicting evidence regarding the role of single-fraction RT for spinal cord compression, particularly given that the Single-fraction Radiotherapy Compared to Multifraction Radiotherapy III study did not meet its prespecified noninferiority endpoints, although the absolute difference of ambulatory status at 8 weeks was small (69.3% in the single-fraction group vs 72.7% in the multifraction group).33 Nevertheless, 8 Gy × 1 provides acceptable rates of palliation and allows for safe retreatment with either conventionally fractionated or stereotactic body radiation therapy approaches if warranted. In the setting of the COVID-19 pandemic, the risk for nosocomial infection from patient daily exposure and prolonged hospitalizations and the potential exposure to staff and other patients must be balanced against the potential benefit of multifractionated treatment.
Tumor bleeding
Uncontrolled tumor bleeding is a life-threatening condition that can be effectively relieved with palliative radiation. Radiation Therapy Oncology Group 8502 used 10 Gy × 1 to palliate advanced pelvic malignancies, but due to frequent late gastrointestinal toxicities (grade 3-4 late toxicities in 49% of patients), it was closed prematurely and replaced with 3.7 Gy × 4 fractions twice daily, repeated at 3-week intervals for a total of 3 courses.34 This “Quad Shot” regimen has also been effective in head and neck malignancies.35 Owing to potential increased risk of nosocomial SARS-COV2 exposure, our center has recommended limiting treatment of patients with COVID-confirmed or suspicious cases to a single treatment machine at the end of the day to facilitate disinfection and risk reduction procedures. As such, it may be logistically preferable to avoid twice-daily treatments and instead favor 4 Gy × 5 as an alternative.
Superior vena cava syndrome/airway obstruction
Superior vena cava syndrome can present with clinically severe airway and neurologic or hemodynamic compromise. Radiation can be effective in relieving hemoptysis but has limited utility for relieving dyspnea and cough. Sundstrøm et al36,37 reported excellent outcomes with 8.5 Gy × 2 fractions given a week apart for patients with central airway emergencies, although our institutional practice favors 4 Gy × 5 daily fractions. Although 8.5 Gy × 2 1 week apart may offer logistical advantages, particularly for inpatients who may be discharged after the first fraction, we felt that this must be balanced with concerns for spinal cord toxicity, especially in patients with prior radiation treatments and those who may need future treatments.
For patients with airway obstruction from a lung or mediastinal tumor, there are no data at this time on the effect of RT exposure to lung in patients with SARS-COV-2 infection. Given the danger of acute respiratory distress syndrome, the possible need for mechanical ventilation, and the potential for structural and obstructive lung disease, a multidisciplinary discussion is recommended for patients requiring RT palliation for malignant airway obstruction.
Painful bone metastases
Although not an oncologic emergency, patients with painful bone metastases frequently require radiation oncology consultation for symptom management. Per National Comprehensive Cancer Network guidelines for supportive care, many medical strategies can also be considered for the management of bone metastases.38 If patients have an impending fracture, we recommend a multidisciplinary discussion with orthopedic surgery or interventional radiology to decide on mechanical stabilization and a potential role for RT. The risk of prolonged hospitalization from pathologic fracture may expose the patient to potential hospital-acquired infections including SARS-COV-2, and thus planned surgical intervention should be considered for patients with impending fracture. Otherwise, radiation should be considered if it is anticipated that localized pain from a metastasis would result in potential admission for pain crisis. If radiation is indicated, several studies and the Choosing Wisely campaign support 8 Gy × 1 fraction treatment for uncomplicated bone metastases.13,39,40 Additionally, for patients with less urgent symptoms who are able to wait for complex treatment planning, single-fraction stereotactic body RT may also be an appropriate way to provide faster and more durable palliation still in a single treatment session, based on randomized evidence.41
Conclusions
Palliative RT plays a critical role in the prevention of serious morbidity for patients with metastatic cancer in the setting of oncologic emergencies, even in the midst of the current COVID-19 pandemic. For patients with metastatic cancer, prognosis must first be clearly estimated and communicated with the patient, followed by a goals-of-care conversation. Data from China suggest that 40% of patients with active cancer diagnoses required either intubation or died, although the authors report that they are only presenting a small sample size and acknowledge the presence of other comorbidities such as age and smoking history.9 Patients who have prognostic awareness are less likely to choose and therefore receive aggressive oncologic treatments in the last month of life.42 As such, these patients may opt for medical supportive care. For patients suitable and requiring palliative RT, an abbreviated course of treatment is of particular importance to reduce the risk of viral exposure to all patients and staff, without compromising functional outcomes. Furthermore, as staffing and clinical treatment capacity remain at risk for fluctuation, abbreviated RT courses better allow for treatment completion without delay. Fortunately, there is high-level evidence supporting these courses for oncologic emergencies to maximize patient benefit and resource allocation. As such, hypofractionated regimens for palliative radiation are preferred to reduce risk and maximize benefit for both individuals and the population during the COVID-19 pandemic.
Acknowledgments
We thank our departmental leadership, especially Dr Simon Powell, Dr Oren Cahlon, and Dr Sean McBride in their guidance and design of the department-wide tier system for patient triage.
Footnotes
Sources of support: National Institutes of Health/National Cancer Institute (P30-CA008748).
Disclosures: none.
References
- 1.Rades D., Stalpers L., Veninga T. Evaluation of five radiation schedules and prognostic factors for metastatic spinal cord compression. J Clin Oncol. 2005;23:3366–3375. doi: 10.1200/JCO.2005.04.754. [DOI] [PubMed] [Google Scholar]
- 2.Rades D., Panzner A., Rudat V., Karstens J.H., Schild S.E. Dose escalation of radiotherapy for metastatic spinal cord compression (MSCC) in patients with relatively favorable survival prognosis. Strahlenther Onkol. 2011;187:729–735. doi: 10.1007/s00066-011-2266-y. [DOI] [PubMed] [Google Scholar]
- 3.Rades D., Šegedin B., Conde-Moreno A.J. Radiotherapy with 4 Gy× 5 versus 3 Gy× 10 for metastatic epidural spinal cord compression: Final results of the SCORE-2 trial (ARO 2009/01) J Clin Oncol. 2016;34:597–602. doi: 10.1200/JCO.2015.64.0862. [DOI] [PubMed] [Google Scholar]
- 4.Lutz S., Chow E., Hoskin P.J. Wiley; West Sussex, UK: 2013. Radiation Oncology in Palliative Cancer Care. [Google Scholar]
- 5.Yale School of Medicine Department of Therapeutic Radiology Faculty COVID19 Yale Radiation Oncology Flowchart - Version 6.0. https://production-mednet-web-assets.s3.amazonaws.com/files/publications/Yale+Radiation+Oncology+-+COVID19+Guidelines+-+Version+6.0+3-20-2020.pdf Available at:
- 6.Zaorsky N., Yu J., McBride S. Prostate Cancer Radiotherapy Recommendations in Response to COVID-19. Adv Radiat Oncol. https://www.astro.org/ASTRO/media/ASTRO/Daily%20Practice/PDFs/COVID-Zaorsky-et-al(ADRO).pdf Available at: [DOI] [PMC free article] [PubMed]
- 7.Braunstein L., Gillespie E., Hong L. Breast radiotherapy under COVID-19 pandemic resource constraints — approaches to defer or shorten treatment from a comprehensive cancer center in the United States. Adv Radiat Oncol. https://www.astro.org/ASTRO/media/ASTRO/Daily%20Practice/PDFs/COVID-Braunstein-et-al(ADRO).pdf Available at: [DOI] [PMC free article] [PubMed]
- 8.Achard V, Tsoutsou P, Zilli T. Radiotherapy in the time of the coronavirus pandemic: When less is better [epub ahead of print]. Int J Radiat Oncol Biol Phys.https://doi.org/10.1016/j.ijrobp.2020.03.008
- 9.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jin R., Xia Y., Zhao J. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21:e181. doi: 10.1016/S1470-2045(20)30150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 12.Remuzzi A., Remuzzi G. COVID-19 and Italy: What next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hahn C., Kavanagh B., Bhatnagar A. Choosing wisely: The American Society for Radiation Oncology’s top 5 list. Pract Radiat Oncol. 2014;4:349–355. doi: 10.1016/j.prro.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Spratt D.E., Mancini B.R., Hayman J.A. Contemporary statewide practice pattern assessment of the palliative treatment of bone metastasis. Int J Radiat Oncol Biol Phys. 2018;101:462–467. doi: 10.1016/j.ijrobp.2018.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lutz S., Spence C., Chow E., Janjan N., Connor S. Survey on use of palliative radiotherapy in hospice care. J Clin Oncol. 2004;22 doi: 10.1200/JCO.2004.11.151. [DOI] [PubMed] [Google Scholar]
- 16.Duursma F., Schers H.J., Vissers K.C., Hasselaar J. Study protocol: Optimization of complex palliative care at home via telemedicine. A cluster randomized controlled trial. BMC Palliat Care. 2011;10:13. doi: 10.1186/1472-684X-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eron L. Telemedicine: The future of outpatient therapy? Clin Infect Dis. 2010;51:S224–S230. doi: 10.1086/653524. [DOI] [PubMed] [Google Scholar]
- 18.Basch E., Deal A.M., Kris M.G. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol. 2016;34:557. doi: 10.1200/JCO.2015.63.0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chow E., Fung K., Panzarella T., Bezjak A., Danjoux C., Tannock I. A predictive model for survival in metastatic cancer patients attending an outpatient palliative radiotherapy clinic. Int J Radiat Oncol Biol Phys. 2002;53:1291–1302. doi: 10.1016/s0360-3016(02)02832-8. [DOI] [PubMed] [Google Scholar]
- 20.Krishnan M.S., Epstein-Peterson Z., Chen Y. Predicting life expectancy in patients with metastatic cancer receiving palliative radiotherapy: The TEACHH model. Cancer. 2014;120:134–141. doi: 10.1002/cncr.28408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krishnan M.S., Hertan L.M., Chen Y.H. Refining the TEACHH Model: Towards improved clinical utility in the modern era. Int J Radiat Oncol Biol Phys. 2018;102:e443–e444. [Google Scholar]
- 22.Centers for Disease Control and Prevention How to protect yourself. Coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/index.html Available at:
- 23.Borgelt B., Gelber R., Larson M., Hendrickson F., Griffin T., Roth R. Ultra-rapid high dose irradiation schedules for the palliation of brain metastases: Final results of the first two studies by the radiation therapy oncology group. Int J Radiat Oncol Biol Phys. 1981;7:1633–1638. doi: 10.1016/0360-3016(81)90184-x. [DOI] [PubMed] [Google Scholar]
- 24.Rades D., Dunst J., Schild S.E. A new scoring system to predicting the survival of patients treated with whole-brain radiotherapy for brain metastases. Strahlenther Onkol. 2008;184:251–255. doi: 10.1007/s00066-008-1831-5. [DOI] [PubMed] [Google Scholar]
- 25.Brown P.D., Pugh S., Laack N.N. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: A randomized, double-blind, placebo-controlled trial. Neuro-Oncol. 2013;15:1429–1437. doi: 10.1093/neuonc/not114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mulvenna P., Nankivell M., Barton R. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): Results from a phase 3, non-inferiority, randomised trial. Lancet. 2016;388:2004–2014. doi: 10.1016/S0140-6736(16)30825-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laufer I., Rubin D.G., Lis E. The NOMS framework: Approach to the treatment of spinal metastatic tumors. Oncologist. 2013;18:744. doi: 10.1634/theoncologist.2012-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnstone C.A., Lutz S.T. Springer Publishing Company; New York: 2016. Handbook of Palliative Radiation Therapy. [Google Scholar]
- 29.Yerramilli D., Simone C., 2nd, Dharmarajan K.V. One & done: Treating cord compression with single-fraction radiation therapy. Ann Palliat Med. 2019;8:356–359. doi: 10.21037/apm.2019.07.05. [DOI] [PubMed] [Google Scholar]
- 30.Donovan E.K., Sienna J., Mitera G., Kumar-Tyagi N., Parpia S., Swaminath A. Single versus multifraction radiotherapy for spinal cord compression: A systematic review and meta-analysis. Radiother Oncol. 2019;134:55–66. doi: 10.1016/j.radonc.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 31.Maranzano E., Trippa F., Casale M. 8 Gy single-dose radiotherapy is effective in metastatic spinal cord compression: Results of a phase III randomized multicentre Italian trial. Radiother Oncol. 2009;93:174–179. doi: 10.1016/j.radonc.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Thirion P., O’Sullivan L., Clayton-Lea A. ICORG 05-03: Prospective randomized non-inferiority phase 3 trial comparing two radiation schedules in malignant spinal cord compression not proceeding with surgical decompression. Int J Radiat Oncol Biol Phys. 2014;90:1263–1264. doi: 10.1080/0284186X.2018.1433320. [DOI] [PubMed] [Google Scholar]
- 33.Hoskin P.J., Hopkins K., Misra V. Effect of single-fraction vs multifraction radiotherapy on ambulatory status among patients with spinal canal compression from metastatic cancer: The SCORAD randomized clinical trial. JAMA. 2019;322:2084–2094. doi: 10.1001/jama.2019.17913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spanos W.J., Perez C.A., Marcus S. Effect of rest interval on tumor and normal tissue response—a report of phase III study of accelerated split course palliative radiation for advanced pelvic malignancies (RTOG-8502) Int J Radiat Oncol Biol Phys. 1993;25:399–403. doi: 10.1016/0360-3016(93)90059-5. [DOI] [PubMed] [Google Scholar]
- 35.Lok B.H., Jiang G., Gutiontov S. Palliative head and neck radiotherapy with the RTOG 8502 regimen for incurable primary or metastatic cancers. Oral Oncol. 2015;51:957–962. doi: 10.1016/j.oraloncology.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sundstrøm S., Bremnes R., Aasebø U. Hypofractionated palliative radiotherapy (17 gy per two fractions) in advanced non–small-cell lung carcinoma is comparable to standard fractionation for symptom control and survival: A national phase III trial. J Clin Oncol. 2004;22:801–810. doi: 10.1200/JCO.2004.06.123. [DOI] [PubMed] [Google Scholar]
- 37.Senkus-Konefka E., Dziadziuszko R., Bednaruk-Młyński E. A prospective, randomised study to compare two palliative radiotherapy schedules for non-small-cell lung cancer (NSCLC) Br J Cancer. 2005;92:1038–1045. doi: 10.1038/sj.bjc.6602477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Swarm R.A., Paice J.A., Anghelescu D.L. Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17:977–1007. doi: 10.6004/jnccn.2019.0038. [DOI] [PubMed] [Google Scholar]
- 39.Hartsell W.F., Scott C.B., Bruner D.W. Randomized trial of short-versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst. 2005;97:798–804. doi: 10.1093/jnci/dji139. [DOI] [PubMed] [Google Scholar]
- 40.Ryu S., Pugh S.L., Gerszten P.C. RTOG 0631 phase 2/3 study of image guided stereotactic radiosurgery for localized (1-3) spine metastases: Phase 2 results. Pract Radiat Oncol. 2014;4:76–81. doi: 10.1016/j.prro.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen Q.-N., Chun S.G., Chow E. Single-fraction stereotactic vs conventional multifraction radiotherapy for pain relief in patients with predominantly nonspine bone metastases: A randomized phase 2 trial. JAMA Oncol. 2019;5:872–878. doi: 10.1001/jamaoncol.2019.0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Temel J.S., Greer J.A., Admane S. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol. 2011;29:2319–2326. doi: 10.1200/JCO.2010.32.4459. [DOI] [PubMed] [Google Scholar]
- 43.Spanos W.J., Jr., Wasserman T., Meoz R., Sala J., Kong J., Stetz J. Palliation of advanced pelvic malignant disease with large fraction pelvic radiation and misonidazole: Final report of RTOG phase I/II study. Int J Radiat Oncol Biol Phys. 1987;13:1479–1482. doi: 10.1016/0360-3016(87)90314-2. [DOI] [PubMed] [Google Scholar]