Highlights
-
•
Patients who are infected by SARS-Cov-2 and HIV tend to have a longer disease course and slower generation of specific antibodies
-
•
For suspected cases of COVID-19, nucleic acid detection, gene sequencing and antibody detection can confirm the diagnosis, respectively
-
•
SARS-Cov-2 may damage lymphocytes, especially T-lymphocytes, and the immune system is impaired during the period of disease
Keywords: COVID-19, SARS-Cov-2, HIV, Antibody
Abstract
The ongoing outbreak of COVID-19 that began in Wuhan, China, become an emergency of international concern when thousands of people were infected around the world. This study reports a case simultaneously infected by SARS-Cov-2 and HIV, which showed a longer disease course and slower generation of specific antibodies. This case highlights that a co-infection of SARS-Cov-2 and HIV may severely impair the immune system.
1. Introduction
Since December 2019, an outbreak of coronavirus disease, officially named by the World Health Organization as COVID-19, appeared in Wuhan, Hubei Province, China. Patients present with severe viral pneumonia and respiratory illness. Lymphopenia has been considered as a poor prognostic factor for severe acute respiratory syndrome (SARS) (Leung et al., 2004) as well as COVID-19 (Qin et al., 2020). This study reports the clinical findings from a patient confirmed with COVID-19 who was also co-infected by human immunodeficiency virus (HIV).
2. Case presentation
A patient infected by SARS-Cov-2 had a relatively long course of disease with an unstable state. Eight markers of infectious diseases were checked and the results showed that antibodies to HIV and syphilis were positive. The patient was then transferred to a specialty hospital for further treatment on 08 March 2020. In the specialty hospital, the CD4 cell count was 34/uL, CD8 cell count was 737/uL and CD4/CD8 was 0.05. The detection of Cryptococcus antigen in the serum was negative and the patient was then given anti-HIV treatment.
On 11 February 2020, a 37-year-old man presented to Wuhan Huo Shen Shan Hospital with a history of fever, dry cough and chest pain since 10 January 2020. The chest CT of this patient on 08 February showed multiple infiltrations in both lungs, consistent with viral infection. But the RT-PCR amplification of SARS-Cov-2 virus nucleic acid from a nasopharyngeal swab was negative. He denied any other diseases before this onset. The initial physical examination revealed a body temperature of 38.8 °C, oxygen saturation (SPO2) 85–90% under ambient air, respiratory rate of 40 breaths/minute, blood pressure of 145/93 mmHg, and pulse of 119 bpm. The laboratory results reflected normal lymphocytes, normal procalcitonin (0.04 ng/mL) and elevated C-reactive protein (CRP, 96.5 mg/L), a-hydroxybutyrate dehydrogenase (a-HBDH, 318 IU/L) and glutamyl transpeptidase (GGT, 136 IU/L).
The RT-PCR amplification of SARS-Cov-2 virus nucleic acid from a nasopharyngeal swab was tested four times after admission. They were all negative except for the swab on 20 February, which was ORF1ab gene positive, but N gene negative. The serum tests of IgG and IgM of SARS-Cov-2 on 05 and 07 March were also negative. After transportation to a specialty hospital, SARS-Cov-2 IgM was detected in his serum, which confirmed the SARS-Cov-2 infection.
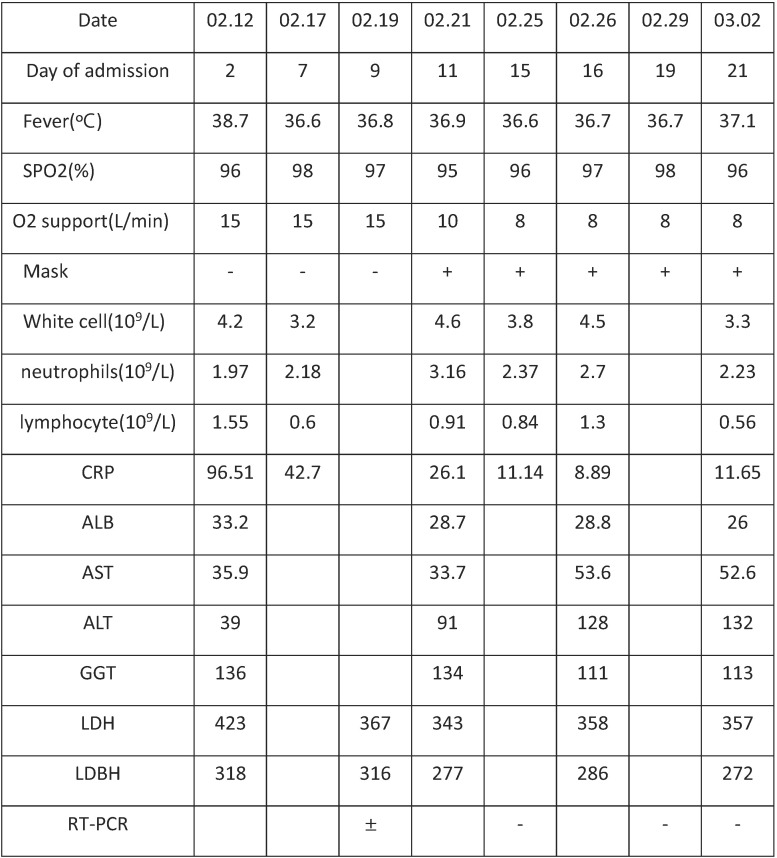
After admission to the current hospital, the patient was treated with high-flow oxygen (15 L/minute) and Arbidol (0.2 g, Tid). His vital signs remained stable for the first 3 days, apart from dyspnea and chest pain (Table 1 ). On 14 February, he developed a high fever of 39.4 °C accompanied with dyspnea and palpitations. Short-term corticosteroid therapy was commenced: methylprednisone 40 mg/day for 5 days. Moxifloxacin was also given for antibacterial therapy. His body temperature returned to normal, but he still had dyspnea, palpitations and chest pain and he still needed high-flow oxygen (10 L/minute) through a mask. On 29 February the second chest CT showed inflammation absorption compared with the previous one. His lymphocytes steadily dropped. On 03 March, the IL-6 in serum was 9.87 pg/mL. Sulbactam/cefoperazone (sulperazone) was added for antibacterial therapy. Human serum albumin, thymosin and ulinastatin were also used. Tocilizumab was given to fight the inflammation storm on 05 March. The IL-6 in serum rose to 141.4 pg/mL on 07 March.
Table 1.
Vital signs and examination from the day of hospitalization, 11 February, to 08 March 2020.
| Date | 02.12 | 02.17 | 02.19 | 02.21 | 02.25 | 02.26 | 02.29 | 03.02 |
|---|---|---|---|---|---|---|---|---|
| Day of admission | 2 | 7 | 9 | 11 | 15 | 16 | 19 | 21 |
| Fever (°C) | 38.7 | 36.6 | 36.8 | 36.9 | 36.6 | 36.7 | 36.7 | 37.1 |
| SPO2 (%) | 96 | 98 | 97 | 95 | 96 | 97 | 98 | 96 |
| O2 support (L/min) | 15 | 15 | 15 | 10 | 8 | 8 | 8 | 8 |
| Mask | - | - | - | + | + | + | + | + |
| White cells (109/L) | 4.2 | 3.2 | 4.6 | 3.8 | 4.5 | 3.3 | ||
| Neutrophils (109/L) | 1.97 | 2.18 | 3.16 | 2.37 | 2.7 | 2.23 | ||
| Lymphocytes (109/L) | 1.55 | 0.6 | 0.91 | 0.84 | 1.3 | 0.56 | ||
| CRP | 96.51 | 42.7 | 26.1 | 11.14 | 8.89 | 11.65 | ||
| ALB | 33.2 | 28.7 | 28.8 | 26 | ||||
| AST | 35.9 | 33.7 | 53.6 | 52.6 | ||||
| ALT | 39 | 91 | 128 | 132 | ||||
| GGT | 136 | 134 | 111 | 113 | ||||
| LDH | 423 | 367 | 343 | 358 | 357 | |||
| LDBH | 318 | 316 | 277 | 286 | 272 | |||
| RT-PCR | ± | - | - | - |
Abbreviations: CRP, C-reactive protein; GGT, glutamyl transpeptidase;.
Figure 1.
Chest CT imaging changes.
The first CT scan (A, C) showed bilateral diffuse ground glass appearance with some patchy consolidations.
Another CT scan (B, D) performed after 9 days of treatment showed some improvement.
3. Discussion
The SARS-Cov-2 virus nucleic acid RT-PCR test from nasopharyngeal swabs has become the standard method for diagnosing SARS-Cov-2 infection. However, these test kits have many limitations because there are so many interference factors during collection, preservation and transportation of the swab specimen, and high false negative rates had been reported. According to the seventh edition of clinical practice guidelines for COVID-19 in China, nucleic acid detection, gene sequencing and antibody detection can confirm the diagnosis, respectively.
In the current case, the patient had a history of fever, lived in Wuhan and had CT findings of viral pneumonia, which was the suspected case. According to the laboratory test results, the patient had lower lymphocytes and elevated CRP levels, which were consistent with viral infection. On this basis, COVID-19 was diagnosed by the positive results of the ORF1ab gene of SARS-Cov-2 from a nasopharyngeal swab and specific antibodies in his serum.
COVID-19 is caused by a novel type of coronavirus SARS-Cov-2. People are generally susceptible to SARS-Cov-2 infection, especially the elderly and those with underlying diseases (Qin et al., 2020). The median time from onset of symptoms to first hospital admission is 7 days, shortness of breath is 8 days, ARDS is 9 days, mechanical ventilation is 10.5 days, and ICU admission is 10.5 days (Huang et al., 2020).
The current case was admitted to the hospital because of fever, which lasted nearly 1 month, and typical changes of viral pneumonia on lung CT imaging. The prominent complaint was dyspnea, especially after moving. After systemic treatment from 11 February to 08 March the hypoxemia had not improved. For SARS-Cov-2 infection, 2 months was too long in duration. The co-infection of HIV gave a reasonable answer for this.
It is widely accepted that IgM provides the first line of defense during viral infection prior to the generation of IgG. It has been reported that after SARS infection, the IgM antibody could be detected in a patient's blood after 3–6 days and IgG could be detected after 8 days (Lee et al., 2010). From the limited data on COVID-19 patients from Wuhan Red Cross Hospital, 94.83% had both IgM-positive and IgG-positive test lines, and 1.72% and 3.45% had only IgM-positive or only IgG-positive lines, respectively. The test times were at day 8 to day 33 after clinical symptoms appeared. The difference in individual immune responses with antibody production may be an important reason for the negative IgM and IgG results (Li et al., 2020).
For this case, 2 months after infection symptoms appeared, SARS-Cov-2 IgM was detected in his serum. The co-infection of HIV may have played an important role. HIV destroys the immune system and specific antibody responses are delayed or even vanish, which consequently resulted in the long course of his disease. Further studies and information collection are needed for this.
The study by Qin showed that the total number of B-cells, T-cells and NK-cells significantly decreased in patients with COVID-19, and was more evident in severe cases than non-severe cases. The author suggested that SARS-Cov-2 might damage lymphocytes, especially T-lymphocytes, and the immune system becomes impaired during the period of disease (Qin et al., 2020).
During the chronic phase of untreated HIV, generalized immune activation and systemic CD4 lymphocyte depletion occurs, and the remaining T-cells may have abnormal responses to antigens. This is accompanied by B-cell dysfunction resulting in abnormal polyclonal activation and a lack of specific antibody responses.
In view of the large number of cytokines induced by SARS-CoV, MERS-CoV and 2019-n CoV infections, corticosteroids are frequently used in the treatment of patients with severe illness, for the possible benefit of reducing inflammatory-induced lung injury. On the other hand, corticosteroids may delay viral clearance (Huang et al., 2020). In this case, corticosteroid therapy was used (methylprednisone 200 mg total) accompanied by Arbidol for antivirus therapy. The body temperature became normal. Tocilizumab was also used once to fight the inflammation storm, which did not show a reduction in IL-6 in his serum.
In conclusion, this paper reports the clinical features of a patient infected by SARS-Cov-2 and HIV. The case appeared to have a long disease course of > 2 months. It was not until later that the IgM in serum could be detected, which may have been due to the immune response being destroyed by the two viruses together.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding Sources
The research received no external funding.
Ethics approval and consent to participate
Not applicable.
References
- Leung G.M., Hedley A.J., Ho L.M. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Ann Intern Med. 2004;141:662–673. doi: 10.7326/0003-4819-141-9-200411020-00006. [DOI] [PubMed] [Google Scholar]
- Qin C., Zhou L., Hu Z. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa248. (accepted article) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.K., Lee B.H., Seok S.H. Production of specific antibodies against SARS-coronavirus nucleocapsid protein without cross reactivity with human coronavirus 229E and OC43. J Vet Sci. 2010;11(2):165–167. doi: 10.4142/jvs.2010.11.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Yi Y., Luo X. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-Cov-2 infection diagnosis. J Med Virol. 2020 doi: 10.1002/jmv.25727. (accepted article) [DOI] [PMC free article] [PubMed] [Google Scholar]