Lei Fang and colleagues1 suggest that clinicians should consider withholding angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) because of a potential increased risk of worse clinical outcomes in patients with coronavirus disease 2019 (COVID-19), and they suggest calcium channel blockers as an alternative. The hypothesis behind this suggestion is that the entry point for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the ACE2 receptor and that ACEIs and ARBs have the potential to upregulate ACE2. However, data for this mechanism are largely from animal studies of heart tissue. Human data have not consistently shown increased ACE2 levels.2, 3
This premature hypothesis has generated confusion across various media channels and in the medical community. Some medical centres have suggested withholding renin–angiotensin system (RAS) inhibitors, despite calls from international societies (eg, the European Society of Cardiology, Hypertension Canada, The Canadian Cardiovascular Society, UK Renal Association, and the International Society of Hypertension) urging against such action. Fang and colleagues based their hypothesis on unadjusted observational data and proposed that patients with hypertension are at increased risk of mortality from COVID-19, attributable to ACE2 as the binding protein for SARS-CoV-2. Although unadjusted observational data suggest that patients with hypertension are at increased risk of mortality, no data are available for the blood pressure regimen of patients with more severe or fatal COVID-19.4 It is equally plausible that patients with hypertension have an overactive RAS, placing them at increased risk for pulmonary complications from COVID-19 in view of the counter-regulatory role of ACE2 on activated RAS. It is also important to distinguish between use of ACEIs and ARBs, because these drugs could have differential effects on RAS components.
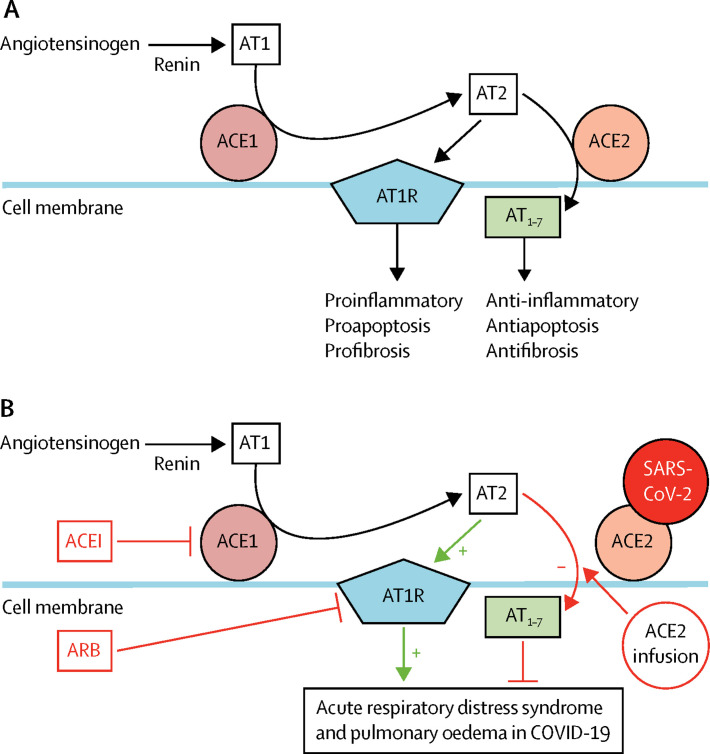
Similar to severe acute respiratory syndrome coronavirus (SARS-CoV), SARS-CoV-2 binds with the ACE2 receptor for intracellular invasion, and the mechanism for acute lung injury during infection has been postulated to be mediated through activation of RAS.5 In several studies, RAS blockade has been proposed as a potential treatment for COVID-19 (figure ).6 Angiotensin 2 (AT2) primarily activates the type 1 angiotensin 2 receptor (AT1R), which potentially mediates pulmonary inflammation, fibrosis, and oedema.7 ACE2 activation results in low amounts of AT2 and increased production of the anti-inflammatory heptapeptide angiotensin(1-7). Impaired ACE2 activity results in excessive amounts of AT2, allowing for unopposed activation of AT1R and subsequent development of acute respiratory distress syndrome (ARDS).5, 8 Fang and colleagues postulate that patients with SARS-CoV-2 treated with ARBs and ACEIs are at a higher risk for severe COVID-19 infection because of a potential upregulation of ACE2. However, preclinical models of SARS-CoV infection do not support this hypothesis. In 2005, Kuba and colleagues8 found that mice treated with losartan after acid aspiration-induced acute lung injury (with addition of SARS-CoV spike protein) had significantly diminished lung injury and pulmonary oedema compared with mice treated with placebo.8 Furthermore, recombinant human ACE2 infusions or losartan both prevented severe lung injury and pulmonary oedema in ACE2-knockout mice.9 Administration of recombinant human ACE2 improved lung injury in patients with SARS-CoV infection and in acid aspiration and sepsis-induced models of ARDS.8, 9 This premise supports the initiation of randomised controlled trials assessing recombinant human ACE2 infusions and losartan in patients with COVID-19. Severe ARDS secondary to impaired ACE2 activity has been identified in other viral pneumonias (eg, H5N1 and H7N9 influenza).10 Treatment of mice after infection with H5N1 influenza with losartan versus placebo was associated with reduced pulmonary oedema, pulmonary neutrophil infiltration, and significantly improved survival.10 Although controversy exists about the role of RAS inhibition in COVID-19, no evidence is available to support routine discontinuation of ACEIs or ARBs. Preclinical evidence suggests that RAS blockade might attenuate progression of COVID-19. We argue that clinical equipoise exists and, before the medical community makes recommendations for patients to withhold potentially life-saving drugs, there is a critical and urgent need for multicentre trials to test this hypothesis in patients with COVID-19.
Figure.
Potential therapeutic options to address AT1 receptor-mediated lung injury in patients with COVID-19
(A) Mechanism in a healthy individual. (B) Mechanism in an individual with COVID-19. AT1=angiotensin 1. AT2=angiotensin 2. ACE1=angiotensin converting enzyme 1. ACE2=angiotensin converting enzyme 2. AT1R=type 1 angiotensin 2 receptor. AT1-7=heptapeptide angiotensin(1-7). ACEI=angiotensin-converting enzyme inhibitor. ARB=angiotensin receptor blocker. COVID-19=coronavirus disease 2019. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
Related links.
Acknowledgments
We declare no competing interests.
References
- 1.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30116-8. published online March 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramchand J, Patel SK, Srivastava PM, Farouque O, Burrell LM. Elevated plasma angiotensin converting enzyme 2 activity is an independent predictor of major adverse cardiac events in patients with obstructive coronary artery disease. PLoS One. 2018;13 doi: 10.1371/journal.pone.0198144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walters TE, Kalman JM, Patel SK, Mearns M, Velkoska E, Burrell LM. Angiotensin converting enzyme 2 activity and human atrial fibrillation: increased plasma angiotensin converting enzyme 2 activity is associated with atrial fibrillation and more advanced left atrial structural remodelling. Europace. 2017;19:1280–1287. doi: 10.1093/europace/euw246. [DOI] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li W, Moore MJ, Vasilieva N. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020 doi: 10.1002/ddr.21656. published online March 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuba K, Imai Y, Rao S, Jiang C, Penninger JM. Lessons from SARS: control of acute lung failure by the SARS receptor ACE2. J Mol Med. 2006;84:814–820. doi: 10.1007/s00109-006-0094-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuba K, Imai Y, Rao S. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imai Y, Kuba K, Rao S. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou Z, Yan Y, Shu Y. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nat Commun. 2014;5 doi: 10.1038/ncomms4594. [DOI] [PMC free article] [PubMed] [Google Scholar]