To the Editor
The spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-COVID 19 has rapidly taken on pandemic proportions, with nearly 2.400.000 people infected and 165.000 dead, at the time writing (https://www.ecdc.europa.eu/).
It has become evident that fragile patients are at enhanced risk of hospitalization, general complications and death. In such a harsh scenario, cancer patients are at significant risk and need particular care in order to prevent, reduce and avoid all the possible contagion occasions [1].
Several Authors have suggested an optimization of patients access to radiotherapy (RT), proposing the reinterpretation of treatments priority and intents; the modification of dose fractionations and concurrent chemotherapy regimens; and the introduction of procedures aimed to reduce patients and personnel exposure to biological risks. Various strategies have been adopted to face the risk of infection during RT course fpr the different anatomical sites reducing the numbers of treatments, introducing safety procedures such as scanning body temperature before each fraction, properly using personal protective equipment (PPE) or admitting the most frail patients in hospitals [2], [3], [4], [5], [6], [7], [8], [9], [10].
Especially during the first most pacey weeks, the different RT centers have adopted inhomogeneous strategies with regards to radiotherapy treatment delivery and screening solutions: some centers systematically excluded patients with fever and airways symptoms from treatments; other decided to perform thorough diagnostic investigation with nasopharyngeal swabs for each patient undergoing therapy; other preferred to administer RT only to admitted patients.
In this context, the known imaging techniques used for simulation (CT) or IGRT monitoring, may represent a significant tool to detect early signs of SARS-Cov-2 pneumonia in patients undergoing radiotherapy. More specifically, Cone Beam CT (CBCT) is one of the best known IGRT solutions, being a reliable tool for setup verification, especially in high precision treatments. Its scanning resolution, slice thickness and speed of acquisition have been improved during last years and have already been used as a monitoring tool during treatment on thoracic malignancies in the past, with interesting results [11].
Furthermore, the recent introduction of Magnetic Resonance Imaging as IGRT support, may also allow to identify still unknown early diagnostic patterns for this disease, opening brand new scenarios.
An aware use of radiotherapy imaging in the SARS-CoV-2 epidemic setting could potentially allow early diagnosis of pneumonia, especially when patients are still in the asymptomatic phase, addressing patients to protected SARS-CoV-2 diagnostic or therapeutic paths, in order to prevent worse evolution of clinical conditions due to the still unknown lung disease progress and limiting the risk of contagion among the other patients in common areas (i.e. waiting rooms) and for the Radiation Therapy Technologists attending the treatment [12].
We here report the case of a 60 years old, HIV positive, male patient currently in home care and candidate for palliative RT for thoracic and lumbar bone metastases of hepatocarcinoma.
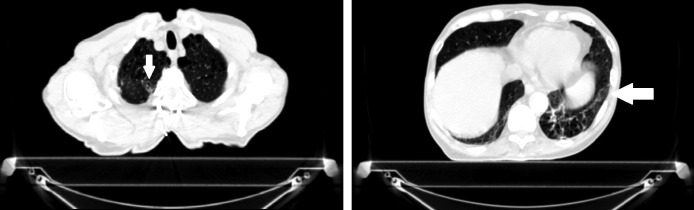
Suspicious findings were observed in the Simulation CT (Fig. 1 ) and first positioning CBCT (Fig. 2 ) and the patient was referred to the infectious diseases path of care for SARS-CoV-2 diagnostic procedures start.
Fig. 1.
Simulation CT with two suspicious areas of opacity: right lung apex (left) and left lung inferior lobe (right).
Fig. 2.
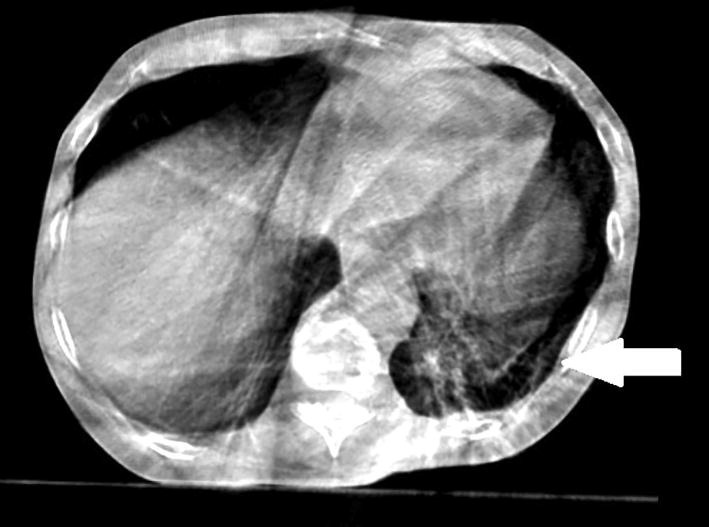
First CBCT: only the suspicious left inferior lobe opacity is encompassed in the field of view.
The patient developed cough and fever two days after image acquisition and pain is currently treated with medical approach, postponing the start of RT when all the diagnostic and quarantine procedures will be completed.
We encourage therefore all the radiation oncology community to be on alert about this potential screening opportunity and train the Simulation and Linac teams accordingly (i.e. RTTs), so that all the figures involved in treatment delivery will pay great attention to IGRT images, referring suspicious cases to the diagnostic department for standard CT acquisition or infectious disease monitoring, contributing in the early diagnosis for our frail patients.
Footnotes
The Editors of the Journal, the Publisher and the European Society for Radiotherapy and Oncology (ESTRO) cannot take responsibility for the statements or opinions expressed by the authors of these articles. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. For more information see the editorial “Radiotherapy & Oncology during the COVID-19 pandemic”, Vol. 146, 2020.
References
- 1.Wei W., Jiang H., Chen W., Zhou Y., Guo S., Zhong G. How should we implement radiotherapy for cancer patients in China during the endemic period of COVID-19? Radiother Oncol. 2020;147:100–102. doi: 10.1016/j.radonc.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thureau S., Faivre J.C., Assaker R., Biver E., Confavreux C.B., Debiais F. Adapting palliative radiation therapy for bone metastases during the Covid-19 pandemic: GEMO position paper. J Bone Oncol. 2020;100291 doi: 10.1016/j.jbo.2020.100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braunstein L.Z., Gillespie E.F., Hong L., Xu A., Bakhoum S.F., Cuaron J. Breast radiotherapy under COVID-19 pandemic resource constraints – approaches to defer or shorten treatment from a Comprehensive Cancer Center in the United States. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones C.M., Hawkins M., Mukherjee S., Radhakrishna G., Crosby T. Considerations for the treatment of oesophageal cancer with radiotherapy during the COVID-19 pandemic. Clin Oncol (R Coll Radiol) 2020 doi: 10.1016/j.clon.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marijnen C.A.M., Peters F.P., Rödel C., Bujko K., Haustermans K., Fokas E. International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. Radiother Oncol. 2020;148:213–215. doi: 10.1016/j.radonc.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guckenberger M., Belka C., Bezjak A., Bradley J., Daly M.E., DeRuysscher D. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: an ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;146:223–229. doi: 10.1016/j.radonc.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomson D.J., Palma D., Guckenberger M., Balermpas P., Beitler J.J., Blanchard P. Practice recommendations for risk-adapted head and neck cancer radiotherapy during the COVID-19 pandemic: an ASTRO-ESTRO consensus statement. Int J Radiat Oncol Biol Phys. 2020 doi: 10.1016/j.ijrobp.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaorsky N.G., Yu J.B., McBride S.M., Dess R.T., Jackson W.C., Mahal B.A. Prostate cancer radiotherapy recommendations in response to COVID-19. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meattini I., Franco P., Belgioia L., Boldrini L., Botticella A., De Santis M.C. Radiation therapy during the coronavirus disease 2019 (covid-19) pandemic in Italy: a view of the nation’s young oncologists. ESMO Open. 2020;5 doi: 10.1136/esmoopen-2020-000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tchelebi L.T., Haustermans K., Scorsetti M., Hosni A., Huguet F., Hawkins M.A. Recommendations on the use of radiation therapy in managing patients with gastrointestinal malignancies in the era of COVID-19. Radiother Oncol. 2020;148:194–200. doi: 10.1016/j.radonc.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Møller D.S., Khalil A.A., Knap M.M., Hoffmann L. Adaptive radiotherapy of lung cancer patients with pleural effusion or atelectasis. Radiother Oncol. 2014;110:517–522. doi: 10.1016/j.radonc.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 12.Suppli M.H., Riisgaard de Blanck S., Elgaard T., Josipovic M., Pøhl M. Early appearance of COVID-19 associated pulmonary infiltrates during daily radiotherapy imaging for lung cancer. J Thorac Oncol. 2020 doi: 10.1016/j.jtho.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]