Abstract
Lung ultrasound examination has been demonstrated to be an accurate imaging method to detect pulmonary and pleural conditions. During pregnancy, there is a need for rapid assessment of the maternal lung in patients with suspected coronavirus disease 2019. We report our experience on lung ultrasound examination in the diagnosis of coronavirus disease 2019 pneumonia in a pregnant woman. Typical ultrasound features of this pulmonary pathology, including diffuse hyperechoic vertical artifacts with thickened pleural line and “white lung” with patchy distribution, were observed. We suggest point-of-care lung ultrasound examination as a diagnostic imaging tool in pregnant women with suspected coronavirus disease 2019.
Key words: biomarkers, coronavirus, COVID-19, diagnosis, lung ultrasound, pleural effusion, pregnancy, respiratory failure, viral infection
Click Video under article title in Contents at ajog.org
Coronavirus disease 2019 (COVID-19) is a global public health emergency.1 Since the first diagnosis in Wuhan, China, the infection has spread rapidly to the rest of the country1 and to more than 25 countries around the world, as reported in the World Health Organization European Region.2 The typical symptoms are fever, cough, changes in sense of smell, headache, and diarrhea, and it can cause severe acute respiratory syndrome in some patients.1
Chest computed tomography (CT) is the imaging method of choice in the diagnosis of COVID-19. The hallmarks of COVID-19 on CT scan are bilateral, subpleural, ground-glass opacities with air bronchograms, ill-defined margins, and a slight predominance in the lower lobes and consolidative pulmonary opacities.3, 4, 5 Abnormal lung CT findings can be present even in asymptomatic patients, and lesions can rapidly evolve into a diffuse ground-glass opacity predominance or consolidation pattern within 1–3 weeks after onset of symptoms, peaking at around 2 weeks after onset.5 Chest x-ray (CXR) examination can reveal the disease only in advanced stages.5 , 6
In pregnant women, the diagnosis of COVID-19 pneumonia is particularly challenging. Although chest CT is not contraindicated in pregnancy and remains the gold-standard technique for pulmonary pathologies,7 lung ultrasound (LUS) examination has been found to be an accurate imaging method to detect peripheral pulmonary and pleural conditions including pneumonia, with high accuracy (sensitivity >90% and specificity >95%),8, 9, 10, 11, 12, 13 even in pregnancy.14
Typical ultrasound findings of COVID-19 pneumonia are (1) a patchy distribution of interstitial artifactual signs (single and/or confluent vertical artifacts, small white lung regions), (2) an extended distribution of aforementioned interstitial artifactual signs to multiple areas of the lung surface, and (3) small subpleural consolidation with associated areas of white lung, following an agreed, tested, and standardized image acquisition protocol. The acquisition protocol includes 14 scanning areas (3 posterior, 2 lateral, and 2 anterior) along the paravertebral, midaxillary, and hemiclavear lines (NCT04322487).15 , 16
In our hospital, we studied the use of LUS to research findings of sonographic interstitial syndrome in a pregnant woman at 23 weeks’ gestation admitted for fever and cough on March 10, 2020, using a Wireless Ultrasound Probe Convex Color Doppler—C05C with a frequency of 3.5 MHz (ATL S.r.l., Milan, IT).
At admission, the pregnant woman was eupneic with spontaneous breathing in ambient air. Her peripheral oxygen saturation was 98%. On auscultation, vesicular sounds were reduced bibasally.
Ultrasonographic assessment was performed with the first operator scanning the patient with the probe and the second operator outside the room evaluating images and videos—in real time—exploiting wireless technique to reduce operators’ exposure to contamination (Video 1).
The obstetrical ultrasound examination revealed a normally grown fetus with normal amniotic fluid and Doppler parameters.
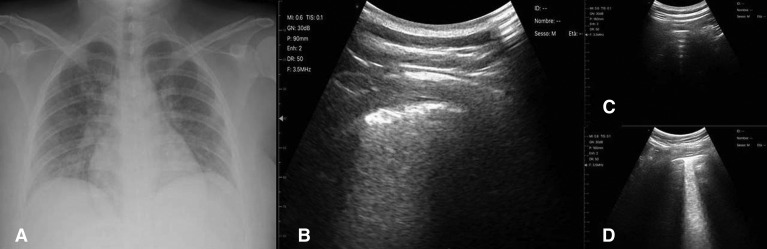
At LUS examination, the patient showed (1) diffuse hyperechoic vertical artifacts with thickened pleural line and (2) “white lung,” with patchy distribution, on 3 of 14 predetermined scan sites (Figure , B and D) (Video 1). CXR, performed on the same day, was not suggestive of viral pneumonia (Figure, A). Throat swabs for the novel coronavirus (2019-nCoV) by real-time polymerase chain reaction confirmed the diagnosis of COVID-19 pneumonia.
Figure.
Chest X-ray and chest ultrasound of a pregnant woman affected by COVID-19 pneumonia
A, Chest x-ray (posterior-anterior projection) of a pregnant woman at 23 week’s gestation, affected by COVID 19 pneumonia showing no pathologic signs suggestive of pneumonia but only a specific bronchial thickening. B, Transversal ultrasonographic scan performed along the paravertebral line on basal posterior zone of the right hemithorax showing a pattern of “white lung.” C, Transversal ultrasonographic scan performed along the paravertebral line on upper posterior zone of the right hemithorax showing a normal ultrasonographic pattern. D, Transversal ultrasonographic scan performed along the hemiclavear line on upper ventral zone of the right hemithorax showing a pattern of “white lung.” Ultrasonographic scans were performed with Wireless Ultrasound Probe Convex Color Doppler—C05C with a frequency of 3.5 MHz (ATL S.r.l., Milan, IT).
Inchingolo. Diagnosis of pneumonia in a pregnant woman with COVID-19 using LUS. Am J Obstet Gynecol 2020.
Discussion
Point-of-care LUS examination could play a key role in the assessment of pregnant women with suspected 2019-nCoV infection. In particular, in this case, LUS findings were crucial to indicate antiviral treatment in the presence of substantially normal CXR.
It is worth underlining that we decided to perform CXR examination because of its different contribution in terms of imaging findings compared with LUS. In particular, CXR allows a panoramic view, giving information also regarding thoracic—not only pulmonary—zones not detectable at ultrasound examination. In contrast, LUS examination has a better sensitivity13 for pneumonia referring to focal alterations of peripheral airspace geometry of the lung. Moreover, CT scan was not performed because we did not need further information to plan management and start treatment.
From the current clinical evidence,17, 18, 19 LUS patterns of subjects with COVID-19 pneumonia include a patchy distribution of interstitial artifactual signs (single and/or confluent vertical artifacts, small white lung regions). Subsequently, these patterns extend to multiple areas of the lung surface. The further evolution is represented by the appearance, still patchy, of small subpleural consolidation with associated areas of white lung. The evolution in consolidations, especially in a gravitational position, with or without air bronchograms, and their increasing extension along the lung surface indicate the evolution toward the phase of respiratory insufficiency.
Studies aimed at clarifying the diagnostic and prognostic role of LUS in COVID-19 are urgently needed, especially in pregnancy. The well-known advantages of LUS in terms of portability, bedside evaluation, safety, and possibility of repeating the examination during follow-up cannot be overlooked and should be exploited and implemented. Moreover, the possibility of performing LUS examination at bedside minimizes the need of transferring the patient, which poses a potential risk of further infection spreading to the healthcare personnel.
Footnotes
The authors report no conflict of interest.
All authors contributed equally.
Supplementary Material
References
- 1.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Regional Office for Europe Countries. http://www.euro.who.int/en/countries Available at: Accessed June 12, 2020.
- 3.Bernheim A., Mei X., Huang M., et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 doi: 10.1148/radiol.2020200463. [Epub head of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu X., Yu C., Qu J., et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi H., Han X., Jiang N., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol. 2020;214:1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 7.Committee opinion no. 723 summary: guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol. 2017;130:933–934. doi: 10.1097/AOG.0000000000002350. [DOI] [PubMed] [Google Scholar]
- 8.Demi L., Demi M., Smargiassi A., Inchingolo R., Faita F., Soldati G. Ultrasonography in lung pathologies: new perspectives. Multidiscip Respir Med. 2014;9:27. doi: 10.1186/2049-6958-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smargiassi A., Inchingolo R., Soldati G., et al. The role of chest ultrasonography in the management of respiratory diseases: document II. Multidiscip Respir Med. 2013;8:55. doi: 10.1186/2049-6958-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zanforlin A., Giannuzzi R., Nardini S., et al. The role of chest ultrasonography in the management of respiratory diseases: document I. Multidiscip Respir Med. 2013;8:54. doi: 10.1186/2049-6958-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soldati G., Demi M., Smargiassi A., Inchingolo R., Demi L. The role of ultrasound lung artifacts in the diagnosis of respiratory diseases. Expert Rev Respir Med. 2019;13:163–172. doi: 10.1080/17476348.2019.1565997. [DOI] [PubMed] [Google Scholar]
- 12.Ye X., Xiao H., Chen B., Zhang S. Accuracy of lung ultrasonography versus chest radiography for the diagnosis of adult community-acquired pneumonia: review of the literature and meta-analysis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0130066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reissig A., Copetti R., Mathis G., et al. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest. 2012;142:965–972. doi: 10.1378/chest.12-0364. [DOI] [PubMed] [Google Scholar]
- 14.Inchingolo R., Smargiassi A., Mormile F., et al. Look at the lung: can chest ultrasonography be useful in pregnancy? Multidiscip Respir Med. 2014;9:32. doi: 10.1186/2049-6958-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moro F., Buonsenso D., Moruzzi M.C., et al. How to perform lung ultrasound in pregnant women with suspected COVID-19 infection. Ultrasound Obstet Gynecol. 2020 doi: 10.1002/uog.22028. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Soldati G., Smargiassi A., Inchingolo R., et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID-19: a simple, quantitative, reproducible method. J Ultrasound Med. 2020 doi: 10.1002/jum.15285. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peng Q.Y., Wang X.T., Zhang L.N., Chinese Critical Care Ultrasound Study Group (CCUSG) Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05996-6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poggiali E., Dacrema A., Bastoni D., et al. Can lung US help critical care clinicians in the early diagnosis of novel coronavirus (COVID-19) pneumonia? Radiology. 2020 doi: 10.1148/radiol.2020200847. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang Y, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19) (February 26, 2020). Available at: 10.2139/ssrn.3544750. Accessed February 28, 2020. [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.