Abstract
The emergence of coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 (SC2) virus, in late December 2019 has placed an overwhelming strain on healthcare institutions nationwide. The modern healthcare system has never managed a pandemic of this magnitude, the ramifications of which will undoubtedly lead to lasting changes in policy and protocol development for viral testing guidelines, personal protective equipment (PPE), surgical scheduling, and residency education and training. The State of Washington had the first reported case and death related to COVID-19 in the United States. Oral and maxillofacial surgeons have a unique risk of exposure to SC2 and developing COVID-19 because of our proximity of working in and around the oropharynx and nasopharynx. The present report has summarized the evolution of COVID-19 guidelines in 4 key areas: 1) preoperative SC2 testing; 2) PPE stewardship; 3) surgical scheduling guidelines; and 4) resident education and training for oral and maxillofacial surgery at the University of Washington, Seattle, Washington.
The emergence of coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 (SC2) virus, in late December 2019 has overwhelmed healthcare institutions nationwide.1 The modern healthcare system has never managed a pandemic of this magnitude, the ramifications of which will lead to lasting changes in policy and protocol development for viral testing guidelines, personal protective equipment (PPE), surgical scheduling, and residency education and training.
On January 19, 2020, the first reported COVID-19 case in the United States was seen in an urgent care clinic in Snohomish County, Washington, and confirmed 2 days later on January 21, 2020.2 Almost 6 weeks later on February 29, 2020, Seattle and King County public health officials confirmed the first COVID-19–related death in the United States.3 Finally, as the virus spread worldwide, with 31 deaths from 374 confirmed cases in Washington state, the World Health Organization officially declared the coronavirus outbreak a pandemic on March 11, 2020.4
By March 12, 2020, the Centers for Disease Control and Prevention (CDC) had released recommendations postponing all nonurgent elective procedures and permitting only urgent or emergent cases to proceed. In addition, for dental healthcare workers, aerosol-generating procedures (AGPs) were only permitted in urgent or emergent settings with proper PPE, as emerging data demonstrated the high risk of viral transmission via respiratory droplets.5 , 6 In addition, Washington Governor Jay Inslee ordered the closure of educational facilities on March 13, 2020, instituted a stay at home order on March 23, 2020, and directed the closure of all nonessential services on March 25, 2020.7
The University of Washington (UW) oral and maxillofacial surgery (OMS) department carries the unique distinction of providing tertiary care for Washington, Wyoming, Alaska, Montana, and Idaho. In addition, the OMS department services 4 different hospitals in the Seattle area and the UW School of Dentistry (SOD). The UW SOD is the only dental school in the State of Washington. The states of Wyoming, Alaska, Montana, and Idaho have no dental schools. This has presented a unique challenge for the OMS service: to provide care for the patients in the direst need and ensure the safety of residents, staff, nurses, and clinical faculty.
With CDC guidelines cautioning against AGPs and the lack of precedent in operating during a pandemic, it became incumbent on the UW OMS department to develop a set of guidelines consistent with the UW School of Medicine (UW Medicine) to ensure the delivery of appropriate patient care, protect vital resources (eg, access to PPE and intensive care facilities), and protect providers and staff from unnecessary risk.
In the present report, we have summarized the evolution of COVID-19 guidelines for UW OMS patient care in 4 key areas: 1) preoperative SC2 testing; 2) PPE stewardship; 3) surgical scheduling guidelines; and 4) resident education and training.
Preoperative SC2 Testing
Initially, testing for SC2 relied on the real-time polymerase chain reaction (RT-PCR) test using a nasopharyngeal swab. The results were available within an average of 15 hours (range, 10 to 19 hours) at our institution.8 The UW virology laboratory has the capacity to run 4000 cases daily of a “non-rapid” SC2 test called “SARS-CoV-2 (COVID-19) qualitative PCR.” The results are expected the same day for specimens received in the morning and the next day otherwise.8 In principle, the RT-PCR test has 100% sensitivity (true positive rate). However, because of sampling error or biology of the disease (eg, virus present in the lower, but not upper, respiratory tract), in the clinical setting, the test will result in some false-negative outcomes. A 2020 study compared chest computed tomography (CT) and RT-PCR for 51 patients in China. The Chest CT scan showed a sensitivity of 98% and the RT-PCR test showed a sensitivity of 71% from the first throat swab or sputum. Using the second RT-PCR, 23% of those initial negative results were positive, with the third test, 4% were positive, and with the fourth test, 2% were positive.9 , 10 The current clinical sensitivity and specificity for SC2 testing using RT-PCR at the UW has been reported to be high; however, the actual values are unknown, because no reference standard is available for COVID-19 status.
By March 21, 2020, the Food and Drug Administration approved the first rapid SC2 RT-PCR.11 The rapid test available at our institution is currently performed every 2 hours on the even hour, with results available within 80 minutes.12 Thus, if a specimen were submitted immediately after the 2-hour run, the result would be delayed accordingly. The capacity of this test is limited to 40 tests daily because of machine capabilities and supply of reagents and, thus, is reserved for inpatients developing new or worsening symptoms, select cases in the emergency department, and in preprocedural areas.12 COVID-19 symptoms include new-onset fever greater than 100°F, cough, shortness of breath, myalgias, rhinorrhea, sore throat, anosmia, and aguesia.13 Given the limited number of daily samples that can be tested, providers must directly speak with the COVID-19 infection control physician on call to justify the necessity for the test and receive formal approval.
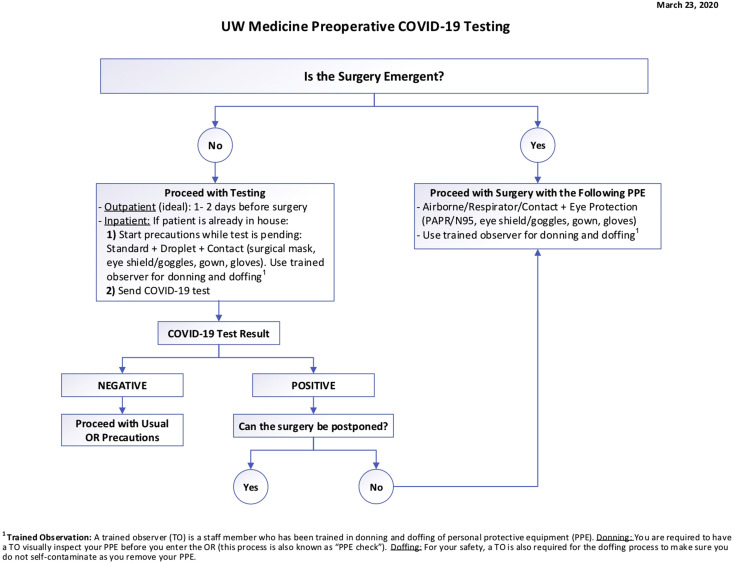
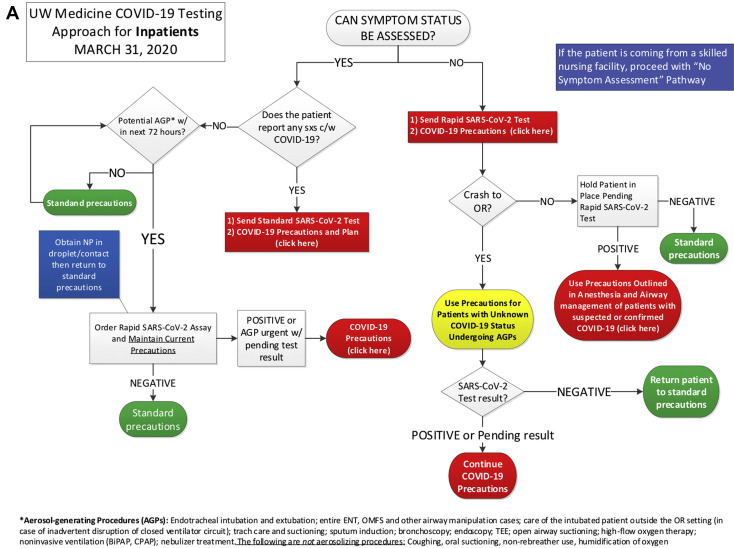
On March 23, 2020, the UW Medicine released an initial COVID-19 testing algorithm for preoperative surgical patients (Fig 1 ). The algorithm distinguished whether the surgery was emergent and then, according to the SC2 test results, recommended the appropriate PPE. The second and current iteration of the COVID-19 testing algorithm was released on March 31, 2020 (Fig 2 ). Given the rapidly evolving recommendation of managing operative treatment in the COVID-19 era, as of April 20, 2019, this algorithm had not changed.
Figure 1.
Initial University of Washington School of Medicine preoperative coronavirus disease 2019 (COVID-19) testing algorithm. OR, operating room; PAPR, powered air purifying respirator; PPE, personal protective equipment.
Figure 2.
University of Washington School of Medicine (UW Medicine) coronavirus disease 2019 (COVID-19) testing approach for A, inpatients and B, asymptomatic patients assessed in clinics. AGP, aerosol-generating procedure; BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; c/w, consistent with; ENT, ear, nose, and throat; F/U, follow-up; HMC, Harborview Medical Center; OMFS, oral and maxillofacial surgery; OPMC, outpatient medical center; OR, operating room; NP, nasopharynx; Pre-op, preoperative; RN, registered nurse; sxs, symptoms; TEE, transesophageal echocardiography; trach, tracheal; UWMC, University of Washington Medical Center.
The current process for the choice of operative venue (standard vs negative pressure operating rooms) and PPE (standard vs aerosolized transmissible disease [ATD] precautions) is based on 3 parameters: operative urgency, symptom status, and SC2 testing result (Fig 2). All operative procedures are limited to urgent or emergent cases. To qualify for urgent operative treatment, the patient must be asymptomatic and have had a negative SC2 test result within 72 hours before the procedure. If the same patient required reoperation more than 72 hours after SC2 testing, the patient would require repeat testing. Given an asymptomatic patient with a negative SC2 test result, standard precautions (ie, mask, face shield or goggles, gown, surgical cap, and gloves) would be used. For example, we performed surgery using the standard precautions for an asymptomatic and SC2-negative patient with a mandible fracture.
If the case were urgent, but the patient was symptomatic or had tested positive for SC2, the operation was deferred. If the case could not be delayed for 14 days, the emergent case limb of the algorithm was followed. If the case were emergent and the symptoms and SC2 test status could be ascertained, the emergent case limb of the algorithm was followed. If the symptom and test status could not be determined, ATD precautions were implemented (eg, airborne, respiratory, and contact precautions, negative pressure room, powered air purifying respirators [PAPRs] or N95 respirators, eye shield or goggles, gown, gloves surgical cap, and a trained observer for donning and doffing).
Of special note was the definition of “urgent.” The concept of “urgency” is widely variable and dependent on the specialty and provider. However, with institutional prioritization of PPE preservation, urgent cases were defined as those for which the patient's health outcome would be adversely affected within a specific timeline. At UW, this timeline was initially 2 weeks and was then changed to 4 weeks. As of April 13, 2020, consistent with Governor Inslee's proclamation, UW Medicine changed the cutoff to 90 days.14 These changes reflected the COVID-19 projections within Washington and the need to conserve PPE and the availability of PPE.15
For special circumstances or questions, a COVID-19 resource clinician can be reached for testing questions. In our experience, we had 1 patient with Le Fort II fractures and a displaced nasal fracture. Because of the risk of performing a nasopharyngeal swab, an anterior nasal swab was recommended, with the possibility that the more anterior sample would provide a false-negative result. In another case, a patient with a panfacial fracture and tracheostomy, a lower respiratory tract aspirate was acquired for testing.
Furthermore, preoperative testing of urgent or emergent operating room cases provided additional information. Of the first 240 asymptomatic patients tested, 2 tested positive (0.8%; (the upper limit of the 95% confidence interval was 3%). Of the symptomatic patients tested at the UW virology laboratory, the range of SC2-positive tests ranged from 3 to 15%. At present, among symptomatic patients, the frequency of SC2-positive tests has hovered around 10%.16 , 17 Finally, on April 13, 2020, UW Medicine initiated SC2 testing for all patients admitted to all 4 of its hospitals.
PPE Stewardship
From mid-January to early March, no official recommendations on PPE were in place to help providers reduce the risk of exposure to SC2. However, in March, various guidelines from the CDC were implemented. It was initially thought that if an AGP was performed on an asymptomatic patient with a negative SC2 test result, at a minimum, a N95 disposable respirator mask would be required.5 , 18 In addition, confusion was still present regarding the PPE required when a non-AGP was performed on an asymptomatic patient and whether that situation would only require standard PPE precautions. The need to conserve PPE complicated matters.
The current UW Medicine and OMS department protocol is to use standard PPE precautions (ie, no N95) when treating an asymptomatic, SC2-negative patient who has been tested within the previous 72 hours. The standard PPE precautions include a mask, face shield or goggles, gown, surgical cap, and gloves. The use of standard PPE applies to AGPs and non-AGPs. As of submission, no OMS provider at UW has had a known work-related exposure to SC2. If the patient is SC2 positive and treatment cannot be deferred, care is rendered in the operating rooms because our OMS outpatient clinics are not suitable environments to treat patients with ATDs. No OMS outpatient clinic within the 4 hospitals nor the UW SOD served by the OMS department has a negative pressure room.
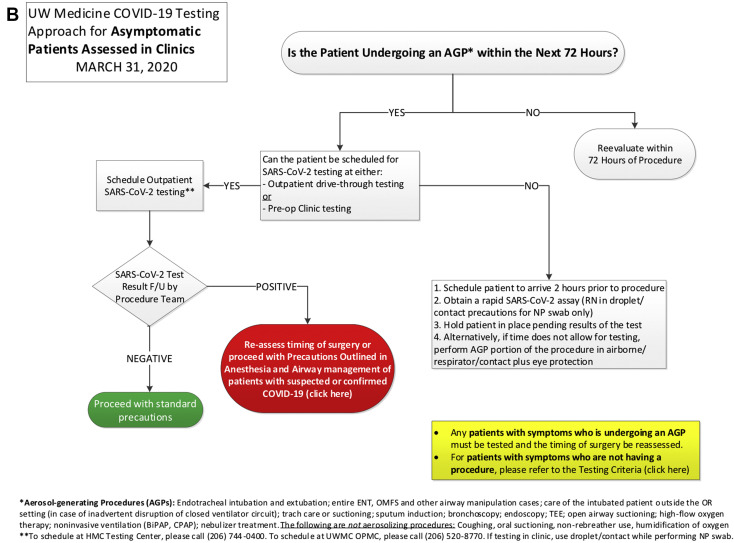
On March 23, 2020, UW Medicine began to implement operative COVID-19 PPE training seminars. These included both in-person PAPR training and an online video of donning and doffing a PAPR after use. In addition, a trained observer is required to monitor and aid in proper doffing to prevent contamination (Fig 3 ).
Figure 3.
University of Washington (UW) personal protective equipment (PPE) algorithm. BiPAP, bilevel positive airway pressure; COVID-19, coronavirus disease 2019; CPAP, continuous positive airway pressure; HMC, Harborview Medical Center; PAPR, powered air purifying respirator; UWMC, University of Washington Medical Center.
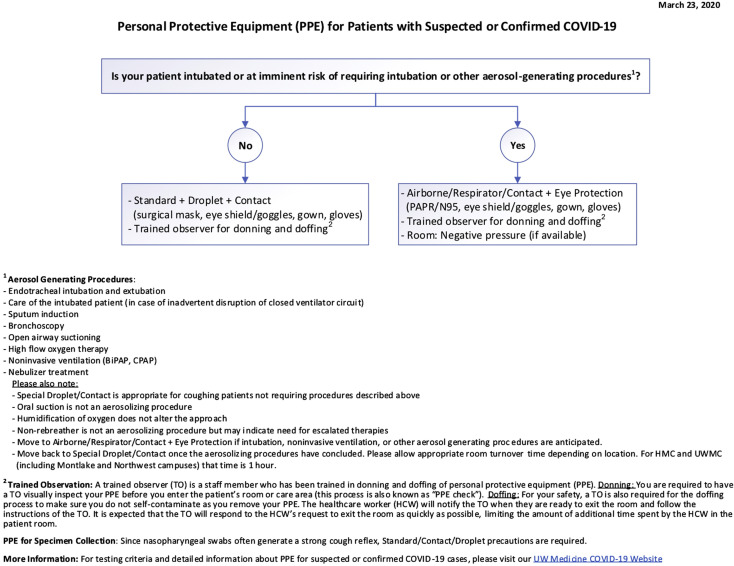
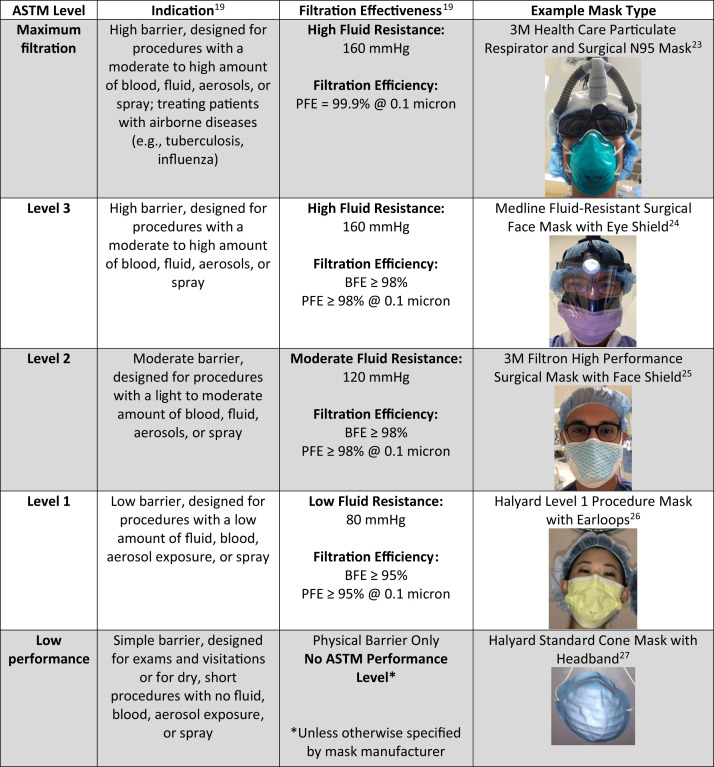
Manufacturers have released different styles of single-use face masks, surgical masks, and N95 disposable respirator masks with different levels of bacterial filtration effectiveness, particle filtration effectiveness, and fluid resistance in accordance with performance specifications from the American Society for Testing and Materials.19 In selecting the appropriate mask, one must consider what level of protection is required (Fig 4 ). A respiratory droplet averages 6 μm, and the size of a single SC2 virion is reported to be 0.1 μm.20 In the case of SC2, mask levels 1 to 3 provide acceptable protection. For OMS, it is especially important to choose a mask that also provides adequate fluid resistance.
Figure 4.
Comparison of mask levels, indications, and filtration effectiveness. ASTM, American Society for Testing and Materials; BFE, bacterial filtration efficiency; PFE, particle filtration efficiency.
At our institutions, the current prevalence of a patient being asymptomatic and having a positive SC2 test is 0.03 (upper limit of the 95% confidence interval). Assuming a level 1 mask provides 95% or more effectiveness in limiting exposure to respiratory droplets, the risk of SC2 exposure from an asymptomatic patient while wearing a Level I surgical mask is estimated to be 15 (0.03 × 0.05) per 10,000 exposures. The risk of SC2 from a symptomatic patient is estimated to be 50 per 10,000 (0.10 × 0.05) exposures. Thus, compared with the risk from an asymptomatic patient, the risk of exposure to SC2 from a symptomatic patient is increased 3.3-fold.
Computations of exposure risk are based on the local estimates of disease prevalence and assumptions regarding mask leakage. Estimates of SC2 exposure should be determined by the local prevalence of SC2 and assumptions regarding mask leakage. As such, it is likely that readers will compute a different estimate of the risk of SC2 exposure and should adjust their behavior and PPE usage accordingly. Ultimately, 3 factors should be evaluated to assess the level of PPE required and ensure provider, patient, and staff safety: 1) procedure acuity (urgent or emergent); 2) symptom status (asymptomatic vs symptomatic); and 3) SC2 test results (positive vs negative).
Surgical Scheduling Guidelines
The initial surgical scheduling guidelines were sparse. After the CDC released its interim guidance on March 6, 2020 to postpone all nonurgent elective procedures, the UW SOD and UW Medicine began developing protocols regarding AGPs. Effective March 12, 2020, all of UW Medicine and the SOD limited care to urgent and emergent cases in the clinic and operating room. Washington state Governor Jay Inslee's current proclamation has suspended elective surgeries and procedures until May 18, 2020, although this is subject to change.14
The guidelines defining urgent or emergent procedures varied and progressed rapidly during the month of March across the United States. The American College of Surgeons (ACS) released guidance for triage of nonemergent surgical procedures on March 17, 2020, delineating elective surgeries into 3 tiers (low, intermediate, high),and further subdividing each tier into 2 categories (healthy or unhealthy).21 Examples of operative procedures were given; however, these were specific to general surgery.
The American Association of Oral and Maxillofacial Surgery (AAOMS) followed a bulletin from the American Dental Association (ADA) released on March 19, 2020.22 On March 26, 2020, the Arbeitsgemeinschaft für Osteosynthesefragen Craniomaxillofacial (AO CMF) released recommendations for maxillofacial procedures for facial trauma, oncologic care, and dental procedures.18 On April 13, 2020, the UW Medicine moved forward with scheduling patients for procedures if delaying the procedure or operation for more than 90 days would adversely affect the patient's health outcome.14
The UW OMS department developed OMS-specific guidelines and provided these to all faculty and residents on March 23, 2020. Subsequently, incorporating the advice from local and national organizations, a surgical acuity scale was developed (Table 1 ).23, 24, 25, 26, 27 The data provided in Table 1 are adapted from the ACS surgery acuity scale. We synthesized the recommendations from the AAOMS, ADA, AO CMF, and the Commission of Dental Accreditation guidelines for OMS training programs. The procedures are subdivided into the domains of anesthesia, trauma, pathology, orthognathic surgery, and reconstructive or cosmetic surgery.28 The decision to delay an operating room or clinic procedure was at the discretion of the attending OMS surgeon and based on a professional determination that delay would not have a significant effect on the patient's health outcomes within the next 90 days.14
Table 1.
UW OMS Surgery Acuity Scale
| Tier | Definition | Location | Examples (per CODA OMS Residency Training Categories) | Action | COVID-19 Testing |
|---|---|---|---|---|---|
| 1a | Low acuity surgery/healthy patient (ASA 1-2); outpatient surgery; not life-threatening illness | OMS OP; HOPD; ASC | Dentoalveolar surgery, asymptomatic; routine outpatient anesthesia; implant therapy; facial trauma (eg, arch bar removal); orthognathic surgery; cosmetic surgery; benign pathology; reconstruction; TMJ | Postpone surgery | NA |
| 1b | Low acuity surgery/unhealthy patient (ASA 3-5) | OMS OP; HOPD; ASC | Dentoalveolar surgery, asymptomatic; routine outpatient anesthesia; implant therapy; facial trauma (eg, arch bar removal); orthognathic surgery; cosmetic surgery; benign pathology; reconstruction; TMJ | Postpone surgery or proceed with appropriate PPE∗ if medical history necessitates procedure | Negative within 72 hours |
| 2a | Intermediate acuity/healthy patient (ASA 1-2); not life-threatening but potential for future morbidity and mortality within 90 days; requires hospital admission | OMS OP; HOPD; ASC | Odontogenic infection; dental extraction, symptomatic; facial trauma (eg, minimally displaced fracture, simple mandible fracture, closed condyle fracture, zygoma, and/or zygomatic arch); benign pathology; reconstruction | Postpone surgery (medical management) or proceed with appropriate PPE∗ and consider the following: trauma: closed reduction, self-drilling screws, limit drilling; delay complex reconstruction where possible (eg, free flaps) | Negative within 72 hours or consider rapid test |
| 2b | Intermediate acuity/unhealthy patient (ASA 3-5) | Hospital | Odontogenic infection; dental extraction, symptomatic; facial trauma (eg, minimally displaced fracture, simple mandible fracture, closed condyle fracture, zygoma, and/or zygomatic arch); benign pathology; reconstruction | Postpone surgery (medical management) or proceed with appropriate PPE∗ and consider the following: trauma: closed reduction, self-drilling screws, limit drilling; delay complex reconstruction where possible (eg, free flaps) | Negative within 72 hours or consider rapid test |
| 3a | High acuity surgery/healthy patient (ASA 1-2); life-threatening and/or high potential for future morbidity and mortality within 90 days; requires hospital admission | Hospital | Odontogenic infection; facial trauma (eg, comminuted open fractures, panfacial injury, ocular emergency, soft tissue injury); head and neck cancer | Proceed with appropriate PPE∗; if nonoperative therapy is equivalent to surgery (eg, radiotherapy), nonoperative therapy is recommended | Negative within 72 hours or consider rapid test |
| 3b | High acuity/unhealthy patient (ASA 3-5) | Hospital | Odontogenic infection; facial trauma (eg, comminuted open fracture, panfacial injury, ocular emergency, soft tissue injury); head and neck cancer | Proceed with appropriate PPE∗; if nonoperative therapy is equivalent to surgery (eg, radiotherapy), nonoperative therapy is recommended | Negative within 72 hours or consider rapid test |
Data adapted from American College of Surgeons.21
Abbreviations: AGP, aerosol-generating procedure; ASA, American Society of Anesthesiologists; ASC, ambulatory surgery center; CODA, Commission on Dental Accreditation; COVID-19, coronavirus disease 2019; HOPD, hospital outpatient department; OMS, oral and maxillofacial surgery; OP, office-based clinic/practice; PAPR, powered air purifying respirator; PPE, personal protective equipment; SC2, SARS-CoV-2; TMJ, temporomandibular joint; UW, University of Washington.
Appropriate PPE—for COVID-19 (SC2) test negative: standard precautions (ie, mask, face shield or goggles; gown, surgical cap, gloves); for COVID-19 (SC2) test positive or unknown: 1) for AGP—airborne respirator/contact precautions (PAPR, N95, eye shield or goggles, gown, surgical cap, gloves), trained observer for donning and doffing, negative pressure room, if available; 2) for non-AGP—standard plus droplet and contact precautions (surgical mask, eye shield or goggles, gown, surgical cap, gloves), trained observer for donning and doffing.
Resident Education and Training
By mid-March, the OMS department had transitioned to limited clinical services to minimize provider exposure and comply with the physical and social distancing recommendations. All residents and faculty underwent “fit” testing for N95s if not previously performed within the previous year. This “fit” test was used to confirm that the N95 (a disposable respirator mask) fit the user. At Harborview Medical Center (HMC), the chief resident coordinates and schedules for 1 to 2 junior residents to come to HMC and provide support for managing in- and outpatients, perform urgent clinical procedures, and, if needed, assist in operating room procedures. Performing rounds for inpatients was limited to the chief resident and attending to limit unnecessary personnel exposure and conserve PPE. No physical prerounds are performed. All prerounds consist of medical record reviews. The residents not on site are available on standby to be called to the hospital as needed. Visitors are restricted for clinical visits. Ideally, it would only be the patient. If a visitor needed to accompany the patient, the number was limited to 1 person. If possible, the accompanying visitor was asked to wait in the car.
We implemented telehealth consultations to ascertain the urgency of a patient's condition and develop a tentative treatment plan. The goal of telehealth consultations was to eliminate the physical exposure associated with an in-person clinical visit and limit the number of times a patient had to be physically present in the clinic. Additionally, a telehealth consultation allows for a single physical visit to render treatment. Follow-up appointments are executed using telehealth where possible. All postoperative patients are routinely telephoned 1 week after surgery in accordance with our regular clinical work flow.
Additionally, patients in our clinic are reassessed for new-onset COVID-19 symptoms at 1 week postoperatively because the incubation period for SC2 is up to 14 days. In accordance with the UW Medicine guidelines, in the event, a patient has new-onset symptoms, they are retested. If positive for SC2, the staff members and clinicians who might have been exposed to a SC2-positive patient are notified and asked to perform twice-daily temperature checks and assess for other COVID-19 symptoms. If any new-onset symptom develops, that staff member or clinician is tested. If the test results are negative for SC2, they are asked to self-isolate until symptom free for 72 hours. Once they have returned to work, they are required to wear a mask for 14 days after symptom onset.29
In the unusual circumstance of performing an AGP on an asymptomatic patient with unknown SC2 status in the outpatient clinic, the recommended practice has been for the surgeon and assistants to wear, in addition to the standard precautions (ie, face shield or goggles, gown, surgical cap, and gloves), an N95 mask with a conventional surgical mask over the N95. The purpose of double masking was to conserve and permit the reuse of the limited N95 masks. The surgical mask prevented the N95 from becoming soiled, permitting its reuse. The covering surgical mask was discarded.
In addition, the hospitals issued residents and staff reusable protective eyewear that could be cleaned after use. At HMC, each resident received a plastic box labeled with their name to store reusable googles and an unused appropriately sized N95 disposable respirator mask. The used N95 was subsequently placed into a breathable paper bag labeled with the user's name. If an N95 mask was not available, PPARs were available for use in the clinic and operating room locations. Once universal SC2 testing for all procedures became available, the PPE requirements were determined by the SC2 test results and symptoms status (see the “Preoperative SC2 Testing” section). The treatment of SC2-positive patients was deferred. If the treatment could not be deferred, it was performed in the operating room, not the outpatient clinic setting.
To allow for the OMS department's continued didactic and administrative functions, weekly meetings were transitioned to web-based video conferencing. Remote communication facilitated important departmental discussions and resident didactics. Resident operative exposure was decreased as a consequence of limiting operations to those deemed to urgent or emergent. The residents took advantage of this time to emphasize their didactic education through journal clubs, directed book readings, lectures, and research.
Discussion
It is an unfortunate truth that from the initial COVID-19 case on January 19, 2020 until March 13, 2020, the SC2 virus was spreading across Washington. Because of the lack of testing, dental, OMS, and other healthcare providers were performing AGPs with standard PPE. Among the medical community, oral and maxillofacial surgeons are at a high risk of contracting respiratory infections owing to our proximity of working in and around the oropharynx and nasopharynx.30 The final number of preventable SC2 exposures will remain unknown. This 8-week period of unpreparedness has demonstrated the fundamental need for pandemic protocols to be developed proactively and rapidly implemented when needed.
For many academic institutions, ensuring the safety of providers is a priority. News reports detailed 1 OMS resident at Brooklyn Hospital Center in New York requiring intensive care unit admission after testing positive and, with great sadness, the death of another resident at Ascension Macomb Hospital in Detroit.31 , 32 The development of our department's protocol for virus testing, PPE stewardship, surgical scheduling, and resident didactics has ensured that the essential functions of the resident training program can continue in a safe, productive manner.
The lessons learned from this pandemic will shape our profession for years to come. The protocols and guidelines released during the month of March, although vital, demonstrate a medical community playing catchup in managing a once in a lifetime crisis. We must remain vigilant and ensure that the protocols developed during this pandemic continue to evolve to allow us to act proactively when, not if, the next pandemic strikes. It is our hope that the protocols developed at the UW Medicine will provide guidance for when that time comes.
As of April 19, 2020, Washington state had 12,085 confirmed cases and 652 deaths and had tested 141,011 individuals, with a positive rate of 8.6%.33
Acknowledgments
Thank you to all the healthcare and essential workers in the United States and around the world who have continued to work selflessly, in some cases without proper PPE, to ensure the well-being and survival of their patients. Thanks also to UW Medicine and Laboratory Medicine for their tireless efforts in formulating the testing algorithms.
Footnotes
The present study was supported in part by the Department of Oral and Maxillofacial Surgery's Laboratory for Applied Clinical Research and the Education and Research Fund.
Conflict of Interest Disclosures: Dr Dillon is the recipient of an Oral and Maxillofacial Surgery Foundation and an Osteo Science Foundation grant, outside the scope of the present study. Dr Dodson is a consultant to American Association of Oral and Maxillofacial Surgeons and provides service as Associate Editor of the Journal of Oral and Maxillofacial Surgery. None of the remaining authors have any relevant financial relationship(s) with a commercial interest.
References
- 1.Peng X., Xu X., Li Y. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:1. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Washington State Report First COVID-19 Death. CDC Online Newsroom, 2020. https://www.cdc.gov/media/releases/2020/s0229-COVID-19-first-death.html Available at: Accessed April 14, 2020.
- 4.McNerthney C. Coronavirus in Washington state: A timeline of the outbreak through March 2020. KIRO7. https://www.kiro7.com/news/local/coronavirus-washington-state-timeline-outbreak/IM65JK66N5BYTIAPZ3FUZSKMUE/ Available at: Published April 3, 2020. Accessed April 11, 2020.
- 5.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) Information for Healthcare Professionals. March 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html Available at: Accessed March 27, 2020.
- 6.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Washington State Washington State Coronavirus Response. https://coronavirus.wa.gov/ Available at: Accessed April 14, 2020.
- 8.Department of Laboratory Medicine, University of Washington School of Medicine: Frequently Asked Questions About COVID-19 Testing. https://testguide.labmed.uw.edu/public/guideline/covid_faq Available at: Accessed April 14, 2020.
- 9.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases [e-pub ahead of print] https://doi.org/10.1148/radiol.2020200642 Radiology. accessed April 14, 2020. [DOI] [PMC free article] [PubMed]
- 10.Fang Y. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR [e-pub ahead of print] https://doi.org/10.1148/radiol.2020200432 Radiology. accessed April 17, 2020. [DOI] [PMC free article] [PubMed]
- 11.US Food and Drug Administration: Coronavirus (COVID-19) Update: FDA Issues First Emergency Use Authorization for Point of Care Diagnostic. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-first-emergency-use-authorization-point-care-diagnostic Available at: Accessed April 19, 2020.
- 12.Department of Laboratory Medicine University of Washington School of Medicine: SARS-CoV-2 (COVID-19) Qualitative Rapid PCR (special approval only) https://testguide.labmed.uw.edu/public/view/NCVRPD Available at: Accessed April 19, 2020.
- 13.Centers for Disease Control and Prevention Symptoms of Coronavirus. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html Available at: Accessed April 21, 2020.
- 14.Washington Governor Jay Inslee Inslee orders halt to elective surgeries and dental services to reserve critical equipment for COVID-19 health care workers. https://www.governor.wa.gov/news-media/inslee-orders-halt-elective-surgeries-and-dental-services-reserve-critical-equipment Available at: Accessed April 18, 2020.
- 15.Institution for Health Metrics and Evaluation COVID-19 Projections: Washington. http://covid19.healthdata.org/united-states-of-america/washington Available at: Accessed April 20, 2020.
- 16.Kim D., Quinn J., Pinsky B. Rates of co-infection between SARS-CoV-2 and other respiratory pathogens [e-pub ahead of print] https://doi.org/10.1001/jama.2020.6266 JAMA. accessed April 17, 2020. [DOI] [PMC free article] [PubMed]
- 17.Department of Laboratory Medicine. University of Washington School of Medicine UW Virology COVID-19 Dashboard 2020. https://depts.washington.edu/labmed/covid19/ Available at: Accessed April 17, 2020.
- 18.Arbeitsgemeinschaft für Osteosynthesefragen Craniomaxillofacial: AO CMF International Task Force Recommendations on Best Practices for Maxillofacial Procedures during COVID-19 Pandemic. https://www.aofoundation.org/what-we-do/covid-19-resources-for-surgeons#COVIDnews_o=News%20Date%20Facet,Descending Available at: Accessed March 28, 2020. [DOI] [PMC free article] [PubMed]
- 19.ASTM International ASTM F2100 - 19 Standard Specification for Performance of Materials Used in Medical Face Masks. https://www.astm.org/Standards/F2100.htm Available at: Accessed April 19, 2020.
- 20.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American College of Surgeons: COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. Available at: https://www.facs.org/covid-19/clinical-guidance/triage. Accessed March 27, 2020
- 22.American Dental Association What Constitutes a Dental Emergency? https://success.ada.org/∼/media/CPS/Files/Open%20Files/ADA_COVID19_Dental_Emergency_DDS.pdf Available at: Accessed April 19, 2020.
- 23.3M: 3M™ Health Care Particulate Respirator and Surgical Mask 1860, N95 120 EA/Case. https://www.3m.com/3M/en_US/company-us/all-3m-products/∼/3M-Health-Care-Particulate-Respirator-and-Surgical-Mask-1860-N95-120-EA-Case/?N=5002385+3294795990&rt=rud Available at: Accessed April 19, 2020.
- 24.Medline Industries Inc: Fluid-Resistant Surgical Face Masks with Eye Shield. https://www.medline.com/product/Fluid-Resistant-Surgical-Face-Masks-with-Eye-Shield/Masks/Z05-PF07364;ecomsessionid=YDjKKb7xybgJIeMskd0SO_m0y-A1013x0OcpRZnG.OC5-b2b?question=&index=P3&indexCount=3#mrkDocumentation Available at: Accessed April 19, 2020.
- 25.3M: 3M™ Surgical Mask 1838FSG Tie-On with Face Shield, High Performance, 50/CTN 4 CTN/CS. https://www.3m.com/3M/en_US/company-us/all-3m-products/∼/3M-Surgical-and-Specialty-Masks/?N=5002385+3294543258&preselect=6240&rt=rud Available at: Accessed April 19, 2020.
- 26.Halyard Health HALYARD ∗ Level 1 Procedure Mask with Longer Earloops. https://products.halyardhealth.com/infection-prevention/facial-respiratory-protection/masks-respirators/halyard-level-1-procedure-mask-with-longer-earloops.html#frp_type_957 Available at: Accessed April 19, 2020.
- 27.Halyard Health Standard Cone Mask with Headband, Blue. https://products.halyardhealth.com/infection-prevention/facial-respiratory-protection/masks-respirators/standard-cone-mask-with-headband-blue.html#frp_type_957 Available at: Accessed April 19, 2020.
- 28.Commission on Dental Accreditation: Accreditation Standards for Advanced Dental Education Programs in Oral and Maxillofacial Surgery, 2018. https://www.ada.org/∼/media/CODA/Files/2018_omp.pdf?la=en Available at: Accessed April 19, 2020.
- 29.University of Washington School of Medicine: FAQ for Employees with Symptoms of an Acute Respiratory Infection and Employees without Symptoms Who have been Diagnosed with COVID-19. Available at: https://www.washington.edu/coronavirus/#faculty. Accessed April 21, 2020
- 30.Gamio L. The Workers Who Face the Greatest Coronavirus Risk. New York Times. https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html?action=click&module=Top+Stories&pgtype=Homepage Available at: Published March 15, 2020. Accessed April 11, 2020.
- 31.Fink S. “We’re in Disaster Mode”: Courage Inside a Brooklyn Hospital Confronting Coronavirus. New York Times. https://www.nytimes.com/2020/03/26/nyregion/coronavirus-brooklyn-hospital.html Available at: Accessed April 16, 2020.
- 32.Dixon J. Ascension doctor becomes 7th Michigan health care worker to die of coronavirus. Bridge Magazine, Detroit Free Press. https://www.bridgemi.com/michigan-health-watch/ascension-doctor-becomes-7th-michigan-health-care-worker-die-coronavirus Available at: Accessed April 16, 2020.
- 33.Washington State Department of Health Novel Coronavirus Outbreak 2020 (COVID-19) https://www.doh.wa.gov/Emergencies/Coronavirus Available at: Accessed April 18, 2020.