Highlights
-
•
Chest CT imaging has become an important tool in the diagnosis of COVID-19.
-
•
The involved radiologic technologists become high-risk medical care personnel.
-
•
We share systematic strategies for radiologic technologists against COVID-19.
-
•
It can provide guidance to other radiology departments to reduce infection risk.
Keywords: COVID-19, Chest CT, Radiologic technologist, Personal protection
Abstract
The outbreak of Coronavirus Disease 2019 (COVID-19) is a huge threat to global public health security. In the absence of specific antiviral medicines to prevent or treat COVID-19, it is essential to detect the infected patients at an early stage and immediately isolate them from the healthy population. In view of the advantages of sensitivity and high spatial resolution, CT imaging has played an important role in screening and diagnosing of COVID-19 in China. The radiologic technologists performing CT scans for the infected patients become high-risk medical care personnel. It is critical for the radiology department to ensure the personal safety of radiologic technologists and avoid cross-infection. In this review article, we describe the systematic strategies to combat COVID-19 from the radiology department in Tongji hospital in Wuhan, P.R. China, including personnel arrangements, environmental modification, protection levels and configurations, radiological imaging (CT and radiography), and disinfection methods. It can provide guidance to other radiology departments faced with COVID-19 to reduce infection risk for radiologic technologists.
1. Introduction
In December 2019, an unknown pneumonia appeared in Wuhan, P.R. China, which mainly caused lung inflammation induced by a new coronavirus [1]. With the spread of the epidemic, cases have occurred in many countries and regions of the world, where the virus infected more than 600,000 people to date. WHO named the virus severe acute respiratory syndrome coronavirus 2 (SARS-COV-2), and the pneumonia 2019 coronavirus disease (COVID-19) [2].
In the absence of specific therapeutic drugs for COVID-19, it is essential to detect the infected patients at an early stage of the disease and immediately isolate them from the healthy population. According to the latest guidelines [3], the diagnosis of COVID-19 must be confirmed by gene sequencing or reverse-transcription polymerase chain reaction (RT-PCR) based on respiratory or blood specimens. This is part of the key indicators for hospitalization. However, the RT-PCR test for throat swab samples has limitations such as sample collection and transportation, as well as suboptimal performance. It has been reported that the total positive rate of RT-PCR for throat swab samples is about 30%–60% at initial presentation, and it is prone to be false negative [4].
Chest CT imaging has many advantages such as high sensitivity, fast scanning speed, and high spatial resolution for disease diagnosis. It can help detect subtle changes in lung tissue that are not easily detected by conventional chest radiography. In addition, it has been reported that chest CT outperformed lab testing in the diagnosis of COVID-19, and recent work also supports the notion that CT imaging is a more sensitive test for the virus than the confirmatory RT-PCR test [5,6]. Thus, chest CT is used as the primary screening tool for screening and diagnosing of COVID-19 in China.
Radiologic technologists responsible for CT scanning are at a high risk of direct or indirect exposure to pathogens [7,8]. Even more, as in the early stage of infection of the SARS-COV-2 virus, an exposed individual is asymptomatic. Radiologic technologists are thus at risk of occupational exposure to the SARS-COV-2 virus, due to cross-infection. This endangers the personal safety of radiologic technologist. Therefore, it is of particular importance to describe how to avoid the cross-infection in the radiology department. This review summarizes the systematic strategies to protect radiologic technologists against COVID-19 from the radiology department in Tongji Hospital in Wuhan, P.R. China. This includes personnel arrangements, environmental modification, protection levels and configurations, radiological imaging, and disinfection methods. It can provide guidance to other radiology departments faced with COVID-19 to reduce infection risk for radiologic technologists.
2. Personnel arrangements
In Tongji hospital, there are more than 200 personnel in the radiology department, including four groups for diagnosis, technology, nursing, and registration. After the outbreak of COVID-19, our department quickly set up a group headed by the director to combat COVID-19. At the same time, the director designated professionals to be infection managers, who are familiar with updated guidelines on diagnosis, treatment and control specifications. The infection managers are mainly responsible for training all the personnel in the department. Before working, all the personnel were trained with regards to infection knowledge, including on-site training and guidance, using demonstration pictures, recorded videos, etc. The aim was to ensure that the entire radiology team had accurate knowledge of infection, ultimately ensuring that the personnel had the least risk of infection.
All the personnel in the department, especially the radiologic technologists, conducted personal health monitoring and reporting. The main contents included occupational exposure or fever, cough, chest tightness, diarrhea and other potentially suspicious symptoms. Once personnel found any occupational exposure or symptoms, he/she reported to the Infectious Diseases Department immediately. If necessary, they performed blood testing, CT testing, and RT-PCR, and the radiology department prohibited the sick personnel from continuing to work.
Eighteen radiologic technologists with years of CT scanning and digital chest radiography (DR) experience were selected to form three teams, six technologists in a group. They were responsible for chest CT scanning and mobile DR. After many attempts, the final schedule is shown in Table 1 . According to the schedule, each member works for five or six hours a day and then has a rest for about 24 h. Each day there are four technologists performing CT scanning and two technologists performing mobile DR. Each radiologic technologist performs about 40–50 CTs during one shift. Generally, daily there are about ten critically ill patients in whom chest radiography is performed. Taking chest radiographs for ten patients takes about 5 h, by 2 radiologic technologists.
Table 1.
The schedule for radiologic technologists.
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | |
|---|---|---|---|---|---|---|---|
| A1 | 6−12 | 12−18 | 18−24 | 24−6 | M DR | M DR | 6−12 |
| A2 | 12−18 | 18−24 | 24−6 | M DR | M DR | 6−12 | 12−18 |
| A3 | 18−24 | 24−6 | M DR | M DR | 6−12 | 12−18 | 18−24 |
| A4 | 24−6 | M DR | M DR | 6−12 | 12−18 | 18−24 | 24−6 |
| A5 | M DR | M DR | 6−12 | 12−18 | 18−24 | 24−6 | M DR |
| A6 | M DR | 6−12 | 12−18 | 18−24 | 24−6 | M DR | M DR |
A1 to A6 in the table stands for the personnel on duty. “MDR” represents mobile digital chest radiography. “6−12” means that the medical personnel worked from six o’clock to twelve o’clock. If on CT scanning, personnel should scan the patients for six hours. If on MDR, working hours depend on the number of mobile digital chest radiography. Taking DR photos for ten patients takes about 5 h.
Each group works for 7 days according to the period. If there is no physical abnormality after the 14-day medical isolation observation, these personnel members continue working. The kind of schedule not only avoids long exposure to the virus, but also ensures adequate rest for the radiologic technologists.
3. Environmental modification
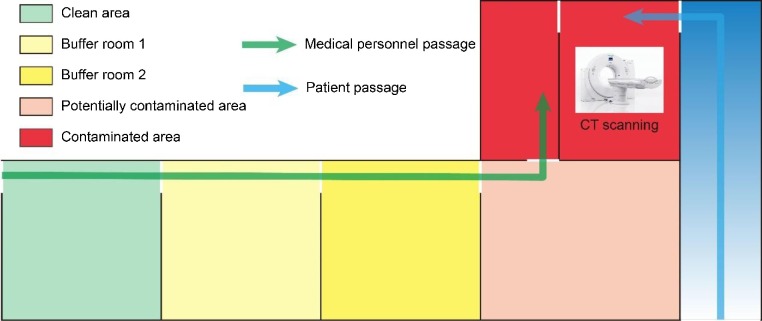
In order to avoid cross-infection, our hospital especially set up a CT scanner for infected patients. According to the concept of "three areas and two passages" [9], we modified the area in the radiology department and set up three areas, that is a contaminated area, potentially contaminated area, and clean area. Also, we added two buffer rooms between the potentially contaminated area and the clean area to further ensure the radiologic technologist’s safety. In addition, we also distinguished between patient passage and medical personnel passage to avoid cross-infection of patients and medical personnel, as shown in Fig. 1 .
Fig. 1.
The flow chart of “three areas and two passages”. Three areas are set up, including the contaminated area, potentially contaminated area, and clean area. And two buffer rooms are added between potentially contaminated area and clean area. Two passages mean the medical personnel passage and the patient passage.
The radiologic technologists can put on personal protective equipment in the clean area, and then go through two buffer rooms and the potentially contaminated area, and finally scan the infected patients in the CT control room, which is considered a contaminated area. This is the medical personnel passage. There are clear signs to help patients quickly find the patient passage. The patients enter the CT scanner room according to the patient passage.
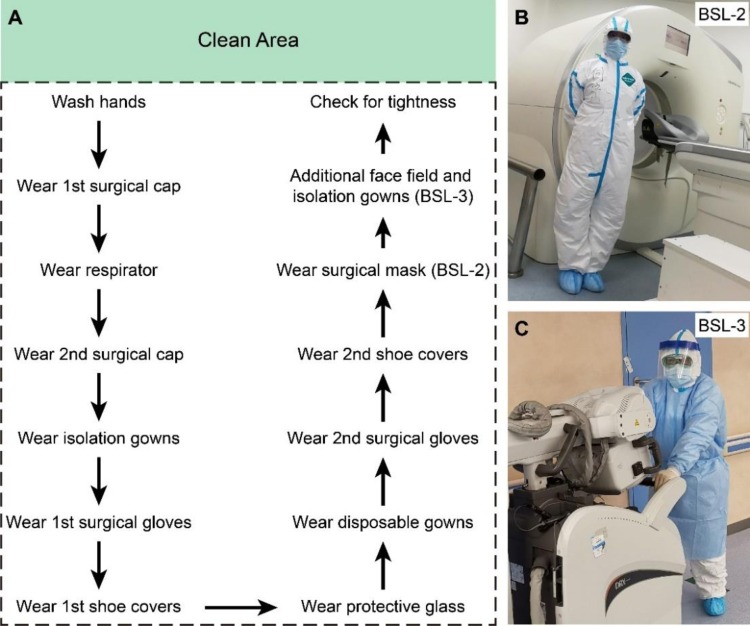
4. Specification of personal protective equipment
The imaging methods for COVID-19 patients mainly comprise CT and digital chest radiography (DR). Thus, the work of the radiologic technologist includes the operation of CT and mobile DR. According to the characteristics of the two duties, we made decisions about the appropriate personal protective equipment. The operators responsible for CT scans perform secondary protection (biosafety level 2, BSL-2) and the operators responsible for mobile DR perform tertiary protection (biosafety level 3, BSL-3) [9,10], as shown in Table 2 .
Table 2.
Lists of personal protective equipment for different biosafety level.
| Biosafety level | List of personal protective equipment |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cap | Surgical mask | Respirator | Protective glass | Isolation gowns | Gloves | Shoe covers | Disposable gowns | Face shield | |
| BSL-2 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| BSL-3 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
The operators responsible for CT scans perform BSL-2 (secondary protection). The operators responsible for mobile DR scans perform BSL-3 (tertiary protection).
The operators performing BSL-2 should wear cap, surgical mask, respirator, protective glass, isolation gowns, gloves, shoe covers, and disposable gowns, at the same time the operators must strictly enforce hand hygiene. The operators performing BSL-3 add face shield and isolation gowns on the basis of BSL-2. The operators should wear cap, surgical mask, respirator, protective glass, isolation gowns, gloves, shoe covers, disposable gowns, and face shield. And the operators must strictly enforce hand hygiene.
The lists of personal protective equipment are shown in Table 2. Next, we introduce the instructions on how to put on and take off the personal protective equipment. The medical personnel walks through the clean access to the clean area and then performs hand hygiene, and puts on personal protective equipment in sequence in the clean area, as shown in Fig. 2 A.
Fig. 2.
Flow chart of how to put on personal protective equipment. The medical personnel put on the personal protective equipment in the clean area in strict order. (A) The sequence for putting on personal protective equipment. The operators performing BSL-3 (tertiary protection) add face shield and isolation gowns on the basis of BSL-2 (secondary protection). (B) The photo of the protection of technicians for BSL-2. (C) The photo of the protection of technicians for BSL-3.
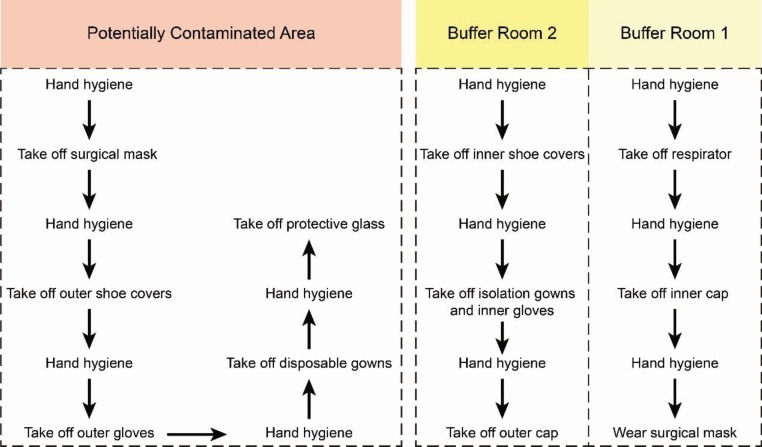
The personal protective equipment must be put on in in strict order. The radiologic technologist first puts on the 1st surgical cap, then the respirator, then the 2nd surgical cap, then isolation gowns, then the 1st surgical gloves, the 1st shoe covers, the protective glass, the disposable gowns, the 2nd surgical gloves, then 2nd shoe covers, then the surgical mask, and at last they must check for tightness of the outfit. This sequence takes about 30 min. Subsequently, the medical personnel pass through the two buffer rooms, the potentially contaminated area, and then enters the contaminated area to work. This is the detailed information of putting on personal protective equipment. Next, we introduce the procedure of how to remove the personal protective equipment. According to the flowchart of taking off protective equipment, the radiologic technologist takes off different protective equipment in different areas after finishing making CT scans, as shown in Fig. 3 .
Fig. 3.
Flow chart of removing personal protective equipment. The radiologic technologist takes off different protective equipment in different areas. The personal protective equipment is taken off in strict order.
After leaving the contaminated area and entering the potentially contaminated area, medical personnel should first disinfect their hands and then remove the surgical mask, outer shoe covers, outer gloves, disposable gowns, and protective glasses in proper order. Hand hygiene must be performed before each step and the personal protective equipment should be placed in a dedicated yellow medical trash can. After this, the medical personnel enter the second buffer room, and in this buffer room they should take off inner shoe covers, isolation gown, inner gloves, and outer cap. Again, the radiologic technologist must perform hand hygiene before each step. And then they enter the first buffer room, take off respirator, the inner cap and finally put on a surgical mask. Hand hygiene should be strictly followed before each step. It is worth noting that the radiologic technologist cannot touch the front of the respirator when removing it. Finally, they perform personal cleaning in the clean area, using 75 % alcohol to disinfect the external auditory canal, using iodine to disinfect the nasal cavity, using normal saline to disinfect the mouth, and then take a thorough bath for less than 30 min after back to apartment.
The above is the sequence of putting on and removing protective material when the radiologic technologist makes CT scanning. When he/she makes mobile DR, the steps are basically similar. The difference is that the operators should add face shield and isolation gowns on the basis of BSL-2 in the clean area. And after taking DR photos the operators remove face shield and outer isolation gowns in the contaminated area and remove different protective equipment in different areas. The remaining steps are consistent with the above description.
5. CT scanning and chest radiography
The value of the DR examination in COVID-19 is very limited, especially for the early inflammatory changes in the lungs (especially pulmonary interstitial changes), which results in many missed diagnoses or false negatives. Chest CT can show early changes in the lungs in COVID-19, and the interstitial and lung parenchyma abnormalities are depicted in detail. It can help detect subtle lesions, and assess the severity of the disease. Above all, chest CT is the main imaging method for screening and diagnosis of COVID-19. However, for critically ill patients (especially in case of tracheal intubation mechanical ventilation), the medical doctor can choose mobile DR to assess the severity of lung lesions.
For CT scanning, the radiologic technologists register and check the identifying information of patients, and inform the patient to remove the metal ornaments above neck and chest through the intercom system in the CT control room. The patients who can move freely, get on and off the examination table by themselves. The technologists can operate the examination bed through the control button in the operating room, and conduct breathing and breath holding training for the patient through the intercom system. If necessary, the technologists need to enter the CT scanner room and help the patient on the table. After doing this and entering the operation room, they must perform hand hygiene. A thin-layer high-resolution scan protocol is used the scan the chest. After scanning, the technologists quickly browse the image to ensure that the image quality meets the diagnostic requirements and guide the patients to leave through the patient passage.
In case of chest radiography at the patient’s bedside, the mobile DR machine is always placed in the ICU, which is especially used for critically ill patients. The technologists should first register and print out the information of the patients, take the lists to the clean area in isolation ward, and put on the protective equipment according to the ward management requirements. It is necessary for the radiologic technologists to wear BSL-3 protective equipment before entering the ward. Subsequently, the mobile DR is pushed to a fixed position to connect to the network. After the patient information is stored in mobile DR, the technologist makes an X-ray of the patient’s chest. It is worth noting that the flat detector of the mobile DR is wrapped with disposable sheets to avoid cross-infection. During shooting, the technologists may minimize close contact with patients. After taking the X-ray, the disposable sheets are placed in a special trash bin place and the flat detector is disinfected with 75 % ethanol solution after every X-ray. The technologists don’t change (part of their) protective gear when moving from one patient to the next. But they must perform hand hygiene. After the images are sent to PACS, technologists can leave isolation ward.
6. Disinfection methods
Air disinfection, surface wiping disinfection and floor disinfection of different areas are performed daily [11]. For air disinfection, all the central air conditioners are turned off to avoid mutual pollution of the air. Additionally, there is an air purifier prepared in the CT control room, which is turned on all the time. The contaminated area, potentially contaminated area, buffer rooms and clean area are all equipped with UV lamps; the air is disinfected by the UV lamps for about 60 min at least 2–3 times daily. For surface wiping disinfection, we use 1000 mg/L chlorine disinfectant to wipe and disinfect the surface. For the wipe of non-corrosive surfaces (such as the CT scanner including gantry and scanner table), we use 75 % ethanol to wipe and disinfect the surface. The frequency is at least twice a day. After the disinfection with the chlorine-containing disinfectant is completed, we use soft cloth dipped with clean water to clean the residual chlorine disinfectant on the surface of the device, and then dry it naturally. After disinfection with ethanol, it can be dried naturally. For floor disinfection, the ground is preferably wiped with 1000 mg/L of chlorine-containing disinfectant, at least twice a day, and disinfected at any time in case of pollutants.
Disposal of medical waste should follow the requirements of the “Medical Waste Management and Regulations”. It is important to point out that the person designated by Infections Diseases Department in the contaminated area is responsible for the hygiene in the contaminated area and potentially contaminated area, and the hygiene in buffer rooms and clean area is done by the person designated by the Infections Diseases Department in clean area. The waste of patients with COVID-19 should be regarded as infectious medical waste; the waste should be double-layered, clearly labeled, and sealed for transfer. The radiologic technologists must follow corresponding regulations. It is strictly prohibited to casually discard masks, gloves, caps and other protective supplies.
Declaration of Competing Interest
No conflict of interest exits in the manuscript.
References
- 1.Zhu N. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diagnosis and Treatment Protocol of Novel Coronavirus (trial version 7th). National Health Commission of the People’s Republic of China website. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. Published March 3, 2020.
- 4.Yang Y. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv. 2020 doi: 10.1101/2020.02.11.20021493. 2020.02.11.20021493. [DOI] [Google Scholar]
- 5.Ai T. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;0 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang P. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology. 2020;0 doi: 10.1148/radiol.2020200330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nyirenda D., Williams R. Infection control recommendations for radiology departments in Malawi. Health SA. 2019;24:1035. doi: 10.4102/hsag.v24i0.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freeman C. 1 edn. The Society of Radiographers; 2006. Health Care Associated Infections (HCAIs): Practical Guidance and Advice. [Google Scholar]
- 9.Professional standards in Health care of the People’s Republic of China (WS/T 311-2009) -Technique standard for isolation in hospitals (In Chinese). National Health Commission of the People’s Republic of China. http://hbba.sacinfo.org.cn/stdDetail/19f4de29810c72257041c6c1fe3fd4fe. Published on April 1, 2009.
- 10.Professional standards in Health care of the People’s Republic of China (WS/T 511-2016)- Regulation for prevention and control of healthcare associated infection of airborne transmission disease in healthcare facilities (In Chinese). National Health Commission of the People’s Republic of China. http://hbba.sacinfo.org.cn/stdDetail/5cd69d070721d9fb01adb8261a7a5f15. Published on December 27, 2016.
- 11.Professional standards in Health care of the People’s Republic of China (WS/T 512-2016)- Regulation for cleaning and disinfection management of environmental surface in healthcare (In Chinese). National Health Commission of the People’s Republic of China. http://hbba.sacinfo.org.cn/stdDetail/de25dd4311fcc16857fe9babb3fd013d. Published on December 27, 2016.