Abstract
Background
Multiple modern Indian hospitals operate at very low cost while meeting US-equivalent quality accreditation standards. Though US hospitals face intensifying pressure to lower their cost, including proposals to extend Medicare payment rates to all admissions, the transferability of Indian hospitals’ cost advantages to US peers remains unclear.
Methods
Using time-driven activity-based costing methods, we estimate the average cost of personnel and space for an elective coronary artery bypass graft (CABG) surgery at two American hospitals and one Indian hospital (NH). All three hospitals are Joint Commission accredited and have reputations for use of modern performance management methods. Our case study applies several analytic steps to distinguish transferable from non-transferable sources of NH’s cost savings.
Results
After removing non-transferable sources of efficiency, NH’s residual cost advantage primarily rests on shifting tasks to less-credentialed and/or less-experienced personnel who are supervised by highly-skilled personnel when perceived risk of complications is low. NH’s high annual CABG volume facilitates such supervised work “downshifting.” The study is subject to limitations inherent in case studies, does not account for the younger age of NH’s patients, or capture savings attributable to NH’s negligible frequency of re-admission or post-acute care facility placement.
Conclusions
Most transferable bases for a modern Indian hospital’s cost advantage would require more flexible American states’ hospital and health professional licensing regulations, greater family participation in inpatient care, and stronger support by hospital executives and clinicians for substantially lowering the cost of care via regionalization of complex surgeries and weekend use of costly operating rooms.
Introduction
Policy-makers worldwide seek to lower the cost of providing high-quality healthcare. American presidential candidates are currently debating whether US hospitals could successfully adapt if Medicare payment amounts applied to all patients. Prior research documents structural and operational sources of efficiency in modern Indian hospitals.1., 2., 3., 4., 5., 6., 7. Parsing inter-country cost differences to identify sources of cost advantage transferable to US hospitals requires accounting for the actual costs of a well-specified treatment meeting a common quality standard.8 , 9
Prevailing healthcare cost accounting systems use imprecise methods to measure the costs of treatment.10 Other industries, such as financial services and retailing, use time-driven activity-based costing (TDABC) to measure the costs of their services more accurately. Until recently, TDABC has rarely been applied in healthcare.11., 12., 13., 14., 15., 16., 17., 18., 19., 20. To explore the transferability of modern Indian hospitals’ cost advantages to US hospitals, we apply TDABC to support a case study of three hospitals with reputations for effective use of modern performance management methods.
Methods
We examine first, non-urgent, isolated, multi-vessel coronary artery bypass graft surgeries (CABG) without complications. To reduce the effects of inter-hospital variation in quality, governance, and training burden on cost, we select for an exploratory case study of three private Joint Commission21 , 22 accredited urban hospitals that are not major teaching hospitals: The Heart Hospital Baylor Plano (THHBP) near Dallas, Intermountain Medical Center (IMC) in Salt Lake City, and Narayana Hospital (NH) in Bangalore (Table I , Table OA.2). The Joint Commission adjusts its accreditation content to accommodate some inter-country differences but maintains that its international accreditation standard is equivalent to its US standard, including examination of hospital complication rates. We compare the three hospitals’ 2013 personnel and space costs, which comprise the majority of variable hospital costs in the US and India.
Table I.
Comparative 2013 characteristics of study sites, including Society of Thoracic Surgeons (STS) isolated CABG ratings.
| THHBP | IMC | NH | |
|---|---|---|---|
| Number of CV surgeons | ~30 | <10 | >40 |
| Number of CV beds | ~110 | ~70 | ~630 |
| Number of CV ORs | 6 | 4 | 10 |
| 2013 STS isolated CABG rating* | 97.7 (3 stars) | 97.7 (3 stars) | N/A |
| Number of CABG surgeries | ~200 | ~500 | ~4,000 |
| % of off-pump CABG surgeries | - | - | 75% |
| Average CABG LoS | 4.8 days | 6 days | 7 days |
| (pre-operative stay) | (-) | (1 day) | (2 days) |
CABG, Coronary artery bypass graft surgery; CV, cardiovascular; LoS: length of stay; OR, operating room.
STS developed a comprehensive rating system for the quality of cardiac surgery among hospitals across the US. According to the STS website “about 10-15 percent of all Adult Cardiac Surgery Database participants have been one-star, about 10-15 percent have been three-star, and the remainder have been two-star, or average programs.”
Each hospital primarily applies a distinctive advanced performance management method: specialization of production (THHBP), variation management (IMC), and systems engineering tools such as work flow optimization (NH). During the study period, both US hospitals earned the STS23 top quality rating of 3 stars and ranked in the “lower than expected” mortality tier of the STS CABG outcomes registry. THHBP also attained national distinction on patients’ experience of care. A subsequent study will explore additional approaches to comparing NH’s quality and cost with the two US hospitals.
We previously described our study protocol and details of our application of TDABC 24 to compare hospitals’ direct cost of performing each activity during episodes of inpatient care. TDABC combines two components (Table A.1 in the appendix): a “process map” portraying the sequence and quantity of inputs such as minutes of staff and operating room (OR) time used to produce an output such as a CABG surgery, and a schedule of unit costs incurred for each input, such as the combined average hourly wage and employee benefits cost incurred by a hospital for a senior nurse, or the hourly cost incurred for the physical space and capital equipment in an OR. Using an on-site visiting team composed of US clinicians and management scientists, we collect time and unit-cost information on all clinical and management processes ordinarily applied during an inpatient stay for a specified type of CABG surgery within the cardiovascular department and other hospital units. The examination includes interviews of involved hospital front-line staff and managers, source data such as salary amounts from the hospitals’ payroll systems, and direct observation of time incurred for personnel and space from hospital admission through discharge.
The study does not examine the cost of medication, supplies, and some ancillary services, because standardizing for inter-country differences poses analytic challenges such as judging the equivalence of India’s non-FDA approved disposable surgical supplies and medications to FDA-approved items used in the US. We do not examine indirect costs since they are substantially determined by externally-imposed factors such as the complexity of payment for hospital services and the annual regulatory burden imposed by state and national governments.
To protect the confidentiality of each hospital’s financial information, we index the resulting cost comparison by arbitrarily setting the sum of IMC’s costs to a score of 100. Costs at the other two hospitals are represented in relation to this index. If a comparator’s total indexed costs per CABG are 20% higher than IMC’s, we report the comparator’s cost as 120. If a comparator’s indexed costs are 20% lower than IMC’s, we report the comparator’s cost as 80. Subsequent to indexing, we calculate NH’s cost as a rounded percentage of costs at IMC and THHBP.
To distinguish non-transferable from transferable sources of cost advantage from NH to the two US hospitals, we apply several analytic steps. The first step compares costs based on the local prices that each hospital pays for space and personnel. Since prices for such inputs reflect factors such as prevailing wages in regional labor markets that hospital leaders cannot change, a second step standardizes the cost comparison for this non-transferable source of cost advantage. We arbitrarily assign input prices paid in Salt Lake City by IMC to recalculate total costs for NH and THHBP. A third analytic step neutralizes the impact of inter-hospital differences in “practical capacity” or the number of clinical minutes per year that each personnel type and clinical space is available for work. The rationale for this adjustment is that annual work minutes per employee are also largely shaped by regional labor markets. We apply IMC’s practical capacities to neutralize the comparison for these predominantly non-transferable sources of cost advantage.
After making these two adjustments, we disaggregate the residual inter-hospital cost differences by comparing two components of each hospital’s use of personnel, commonly referred to as labor productivity24. First, we compare the “skill mix” or blend of clinical personnel used by each hospital to care for patients undergoing a CABG. For example, a hospital could excel on skill mix by safely shifting some intra-operative tasks to lower cost personnel, such as using a physician assistant rather than a cardiac surgeon to suture a surgical incision. Second, we compare the average total number of personnel hours dedicated to a CABG case, since a hospital could excel in labor productivity by using fewer total personnel hours per CABG.
Results
Table A.1 and Table OA.1 in the online appendix provides details of TDABC calculations and on-site observations of clinical activity by the US research team. Table II .A displays unsurprising findings from the non-standardized cost comparison—NH’s actual personnel and space costs for patients undergoing CABG are much lower than the two US hospitals: 10% of IMC’s and 6% of THHBP’s. This result aligns with prior international hospital cost comparisons that fail to adjust for the effect of much lower input prices paid by hospitals in low income countries that are not transferable to U.S. hospitals.25 A second analytic step (Table II.B) finds that after applying input prices paid in Salt Lake City by IMC to NH and THHBP, NH’s costs rise to 84% of IMC’s and 55% of THHBP’s. A third analytic step finds that after standardization for practical capacities of personnel and space by applying IMC’s practical capacities (Table II.C), NH retains a cost advantage equal to 93% of IMC’s and 67% of THHBP’s costs.
Table II.
Personnel and space costs indexed to a scale that sets IMC’s total personnel and space costs at 100.
| THHBP | IMC | NH | |
|---|---|---|---|
| A. Unadjusted indexed costs | |||
| Personnel costs | 150 | 87 | 7.4 |
| Space costs | 20 | 13 | 2.2 |
| TOTAL | 170 | 100 | 9.6 |
| NH’s cost as a % of each US hospital | 6% | 10% | |
| B. Indexed costs after applying IMC’s input prices to NH and THHBP | |||
| Personnel costs | 141 | 87 | 76 |
| Space costs | 12 | 13 | 8 |
| TOTAL | 153 | 100 | 84 |
| NH’s cost as a % of each US hospital | 55% | 84% | |
| C. Indexed costs after applying IMC’s prices and practical capacities to NH and THHBP | |||
| Personnel costs | 121 | 87 | 80 |
| Space costs | 17 | 13 | 13 |
| TOTAL | 138 | 100 | 93 |
| NH’s cost as a % of each US hospital | 67% | 93% | |
We display in Table III data used to attribute NH’s residual cost advantage in personnel costs from Table II.C to differences in total personnel minutes used per CABG and skill mix24. Both NH and THHBP use more total personnel minutes than IMC, intra-operatively and postoperatively. In contrast, the two US hospitals use more time (minutes per case) of senior anesthesiologists and senior surgeons than NH. Table III reveals that NH’s combined use of more total personnel hours per CABG and lower skill mix results in a cost that is 8% lower than IMC, the lower cost of the two US hospitals.
Table III.
Intra- and postoperative activity time incurred at each hospital for personnel engaged in caring for patients undergoing CABG surgery
| THHBP |
IMC |
NH |
||||
|---|---|---|---|---|---|---|
| Time (mins) | % of Total Time | Time mins) | % of Total Time | Time (mins) | % of Total Time | |
| (a) Intra-operative activity times for doctors and non-physician providers | ||||||
| Senior anesthesiologist | 330 | 25% | 357 | 30% | 59 | 5% |
| Junior anesthesiologist | - | - | - | - | 328 | 25% |
| Senior surgeon | 378 | 29% | 270 | 23% | 252 | 19% |
| Junior surgeon/fellow | - | - | 284 | 24% | 466 | 36% |
| Mid-level provider (including NP and PA) | 594 | 46% | 279 | 23% | 198 | 15% |
| TOTAL | 1,302 | 1,190 | 1,303 | |||
| (b) Post-operative activity times for nursing and technicians | ||||||
| Post-operative RN | 3,156 | 85% | 2,045 | 69% | 1,407 | 33% |
| Patient care technician | 559 | 15% | 940 | 31% | 2,890 | 67% |
| TOTAL | 3,715 | 2,985 | 4.297 | |||
NP, nurse practitioner; PA, physician assistant; RN, registered nurse.
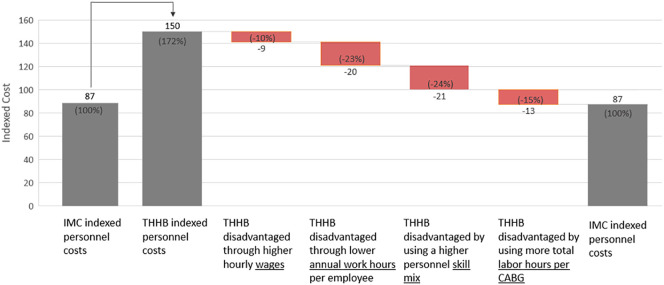
Table IV summarizes results from comparing NH’s personnel costs with IMC’s and THHBP. In Figure 1 , this comparison focuses on the differences between NH and IMC, the lower cost of the two US hospitals. NH is advantaged through lower wages, greater annual work hours for personnel, having a lower skill mix of personnel, but is disadvantaged by using more labor hours per CABG.
Table IV.
Calculating the Personnel Cost Differences Across the Three Hospitals
| IMC vs. THHBP | IMC vs. NH | |
|---|---|---|
| Personnel cost difference (I + II + III) |
87-150 = -63 THHBP’s disadvantage: 72% (-63/87) |
87-7.4 = 79.6 NH’s advantage: 91% (79.6/87) |
| I. Personnel cost difference due to not paying IMC’s wages | 141-150 = -9 THHBP’s disadvantage: 10% (-9/87) |
76-7.4 = 68.6 NH’s advantage: 78% (68.6/87) |
| II. Personnel cost difference due to IMC’s work hours per employee per year | 121-141 = -20 THHBP’s disadvantage: 23% (-20/87) |
80-76 = 4 NH’s advantage: 5% (4/87) |
| III. Personnel cost difference due to different care delivery methods (IIIa + IIIb) |
87-121 = -34 THHBP’s disadvantage: 39% (-34/87) |
87-80 = 7 NH’s advantage: 8% (7/87) |
| IIIa. Personnel cost difference due to use of lower/higher skill mix⁎ | -21 THHBP’s disadvantage: 24% (-21/87) |
29 NH’s advantage: 33% (29/87) |
| IIIb. Personnel cost difference due to use of more/less total labor hours per CABG | -13 THHBP’s disadvantage: 15% (-13/87) |
-22 NH’s disadvantage: 25% (-22/87) |
Figure 1.
Differences in Personnel Costs Between NH And IMC, The Lower Cost Of The Two US Hospitals In The Case Study.
NH’s lower skill mix of personnel makes much greater use of OR technicians and early career physicians and nurses, including student nurses. NH also makes substantial use of unpaid patient family members for support during inpatient convalescence,3 , 4 though its labor savings are substantially offset by the greater time that NH personnel invest in training family members to assist hospital staff during convalescence and to competently care for patients at home after discharge.3 , 4 However, the cost disadvantage that NH incurs by using more total personnel hours per CABG than IMC is more than offset by its use of a much lower skill mix.
Figure 2 summarizes results from comparing NH’s personnel costs between the two US hospitals, IMC and THHBP. THHBP is disadvantaged through higher wages, lower annual work hours for personnel, having a higher skill mix of personnel, and using more labor hours per CABG,
Figure 2.
Differences in Personnel Costs Between THHBP and IMC, the Two US Hospitals.
Discussion
NH’s cost advantage attributable to its lower-cost skill mix corresponds with care delivery methods observed on site. Enabled by its high annual volume of more than 4,000 CABG surgeries, NH customizes the skill mix of its cardiac surgery teams to each patient’s pre- and subsequent peri-operative perceived risk status. US hospitals with much lower volumes of cardiac surgeries cannot afford to deploy skilled senior clinicians to continuously observe lower skilled personnel and participate directly in care only when surgical risk is high or rising.
The US site visiting team observed that NH’s much higher surgical volumes also enable fuller use of costly spaces such as ORs and surgical ICUs. NH schedules at least two elective surgeries per operating room during weekdays and at least one on Saturdays. In the US hospitals, costly OR and surgical ICU spaces more often lay idle during early evenings and weekends. Patients at NH spend two days on average in a low-cost pre-operative hospital unit. The resulting pool of pre-operative patients assures that last-minute surgical cancellations do not waste time of costly clinicians and ORs. NH also controls space costs with a simple, open hospital design and shared patient rooms.
The site visit team at NH observed multiple illustrations of personnel downshifting geared to continuous assessment of peri-operative risk. For example, NH replaces a senior perfusionist with a student perfusionist during its off-pump CABG surgeries, which comprise 75% of NH CABG surgeries. Senior and junior perfusionists overseeing ORs rapidly replace student perfusionists if an off-pump case converts to on-pump case or if other unexpected high-risk events occur. Similarly, a senior anesthesiologist simultaneously monitors operations performed in five glass-windowed operating rooms by standing at the corner of a corridor and intervening quickly if perceived risk of complications rises.
The site visit team observed that NH’s use of detailed protocols for clinical tasks facilitates task downshifting by assigning narrowly-scoped tasks to less skilled personnel. NH’s continuous patient risk stratification, detailed care protocols, and narrowed task assignments for lower-cost personnel illustrate the application of systems engineering tools, long encouraged by the National Academy of Medicine26 and the President’s Council of Advisors on Science and Technology.27 Counter-balancing the transferability of a lower skill mix are valid US hospital and clinician concerns about the more litigious US medical malpractice liability environment.
India’s more permissive hospital and professional licensing regulations facilitate NH’s extensive task downshifting. After postoperative transfer to a floor bed, Indian regulations allow NH to delegate non-professional hospital tasks, such as observation of stable patients, bed linen maintenance, and feeding to patients’ family members under nurse supervision. NH nurses feel such delegation builds family members’ confidence and competence to care for patients after discharge. Patients and their families spend approximately 1200 minutes during the hospital stay being trained by physical therapists, dieticians, and diabetes educators. This is almost three times longer than such interactions at the two US hospitals. Greater engagement of families during postsurgical inpatient convalescence may explain why NH is able to discharge almost all patients directly home and experience a negligible rate of readmissions within 30 days of hospital discharge. Very low posthospital use of post-acute facilities and professionals represents an unmeasured cost advantage for NH relative to US hospitals. In the US, 11% of patients undergoing CABG are discharged to skilled nursing facilities28 and readmissions are not negligible.
Though we excluded the cost of supplies from our analysis, our site visit team observed that NH uses a more restricted menu of surgical supplies than IMC and THHBP. Combined with its scale, standardization of supplies lowers inventory costs and gives NH leverage in price negotiations with suppliers.
We also observe significant differences in patterns of care between the two US hospitals. This comparison illustrates how TDABC-based comparisons can help managers understand and transfer sources of cost-advantage among hospitals enrolled in domestic performance improvement collaboratives or in multi-hospital healthcare organizations. In this case, the higher cost hospital was disadvantaged by higher labor costs, lower productivity (in terms of annual hours work and labor hours per case), and the use of a higher skill mix of personnel in providing services. Financial challenges of the post-COVID-19 environment may encourage US hospitals to conduct more precise cost comparisons to revisit current standard operating procedures governing the use of personnel across the cardiovascular service line. Similar comparisons across hospitals have led to important improvements in clinical quality.29 , 30
Our study is subject to limitations beyond the inherent non-generalizability of case studies. We do not compare costs other than direct costs for personnel and space. Overhead costs are likely to be much higher in the US due to costs imposed by complexities of the US payment, regulatory and external reporting environment. Since the study examines CABG surgeries without complications, findings are not generalizable to CABG procedures resulting in complications or other hospital-based care. Our method for standardizing inter-hospital differences by use of IMC’s input prices does not account for changes in the mix of inputs that THHBP or NH might have made if they were paying the same relative prices for inputs as IMC. Our TDABC approach is partly based on interviews with site personnel to estimate the typical duration of each clinical process. This approach is subject to cognitive and cultural biases that may vary across the three sites. Though NH’s heavy investment of personal time to train patients’ families in postoperative care was included in our analysis, the cost advantage achieved for NH patients due to negligible rates of post-acute care and 30-day readmissions was not included. Lastly, our study does not examine differences between the hospitals in nuanced measures of quality of care, such as short or intermediate-term patient-reported outcomes after hospital discharge using clinical data to adjust for differences in patient risk.
Conclusion
Our case study sheds light on how one modern Indian hospital attains low costs per CABG compared to two well-managed US peers. The full extent of NH’s use of task downshifting is currently unavailable to US hospitals because of state licensing regulations, as well as family expectations about their role in inpatient care. Some bases for NH’s cost advantage could be immediately transferred to US hospitals. These include concentrating high-risk surgeries at hospitals with favorable quality scores and low prices. Harvesting cost advantages from such concentration partly depends on extending elective surgical starts to early evenings and weekends rather than building new hospital capacity. Fulfilling policy-makers’ aspirations to lower payment amounts for care at high-quality hospitals also hinges on whether hospitals pass cost savings from concentration of volume to payers rather than exploit the price negotiating leverage conferred by concentration.
Discovery and adoption of efficiencies also depend on how strongly clinicians and hospital managers are motivated to lower the cost of care. We asked the surgeon-CEO of NH why, after standardizing factors outside of management control, the cost at his hospital is lower than at US peers. He replied that his staff is keenly aware that most of NH’s mostly poor and uninsured patients often “must sell their farms to lie in our beds.” Our US site visit team found NH staff resonated with the CEO’s goal to drive the average total cost of CABG surgery below $1000 within five years.
US health industry executives and personnel may not currently attach the same priority to lowering the financial burden that inefficiencies in care delivery impose on non-affluent Americans via unnecessarily high healthcare prices, insurance premiums and deductibles. Most are likely unaware of secondary effects such as lower wage and job growth for workers in industries other than healthcare.31 To offset inertia, CMS and private sector purchasers of healthcare are encouraging physicians and hospital leaders to deliver the same or better care at lower cost through bundled payment and other forms of value-based purchasing. As public debate continues over whether US hospitals could adapt to a Medicare for All environment,32 estimates of its impact on hospital financial viability should include consideration of potentially transferable opportunities to improve American hospital efficiency such as those illuminated by this case study.
Acknowledgments
The study was supported by the Sue and Dick Levy Fund, an advised fund of the Silicon Valley Community Foundation. Christine Nguyen was also supported by the Stanford University School of Medicine MedScholars Grant and NIH-CATS-CTSA Award TL1 TR001084.
Footnotes
Disclosures. This case study of hospital costs and care delivery methods was exempted from review by the Stanford Institutional Review Board (IRB). It obtained IRB approval at Narayana Health and obtained an IRB quality improvement waiver from the IRB offices used by The Heart Hospital Baylor Plano and Intermountain Medical Center. Two employees at each hospital co-authored the study. Co-author Arnold Milstein is an uncompensated trustee of Intermountain Healthcare, a non-profit organization operating one of the hospitals.
Alternate Contact: Susan Shum-Maxwell – shummax1@stanford.edu
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ahj.2020.04.009.
Appendix A. APPENDIX
Table A.1.
Steps to perform the TDABC analysis of the cost of hospital stays for CABG surgery for each of the three hospitals.
| 1. Select a medical condition and define the care delivery episode; inpatient stay (pre-operative care, intra-operative care, postoperative care, and discharge) for an “average” patient undergoing a first, non-urgent, isolated, multi-vessel CABG surgery without peri-operative complications. | |
| 2. Through onsite observations and interviews, develop process maps with the following principles: | |
| a. Identify each process step in care. | |
| b. Identify the personnel and space (e.g., operating room (OR), intensive care unit (ICU), floor bed) involved for each step. | |
| c. Identify equipment used for each step. | |
| 3. Obtain average time estimates for each process step through interviews and onsite observations. We attempted to interview at least 3 individuals in each personnel category, via a pair of interviewers to minimize interviewer bias. For each process step, we interviewed personnel types performing the step as well as types who would have knowledge of, but not responsibility for, the step to confirm the accuracy of the original estimates. In case of a discrepancy with prior observations or interviews, the causes of this discrepancy were identified, and a consensus estimate was obtained. | |
| 4. Calculate the capacity cost rate (CCR) for each resource: | |
| The expenses attributable to a resource require the calculation of the total cost incurred to make the resource available for patient care. For personnel, this included salary, fringe benefits, administrative support, information technology, and office expenses. For space, this includes annual depreciation, maintenance, operative and housekeeping costs, real estate costs, and the cost value of all equipment in that space. The practical capacity of a resource is the number of clinical minutes that resource is available per year. For personnel, available time only includes direct time available for patients’ care (such as during clinical shifts) and on-call time, but does not include off-duty, vacation and holiday time. For space, available time does not include time when space is unavailable for care due to cleaning and maintenance. | |
| 5. Calculate the total direct personnel and space costs for all resources used over an episode of care by multiplying the total quantity of each resource used in CABG care episodes estimated from the process maps (Step 2) by the resource’s CCR (Step 3). Sum across the resources used at each site. |
Table A.2.
| NH’s 91% advantage in indexed cost of personnel is attributable to three factors: | |
|---|---|
| • Factor I compares NH’s personnel costs inTable II.B andTable II. A – Lower hourly wages in Bangalore than in Salt Lake City confer a 78% cost advantage on NH (76-7.4=68.6, 68.6/87*100=78%) | |
| • Factor II compares NH’s personnel costs inTable II.C and Table II. B – More annual total work hours per employee (practical capacity) in Bangalore than in Salt Lake City confer a 5% cost advantage on NH (80-76=4, 4/87=5%) | |
| • Factor III compares IMC’s personnel cost with NH’s inTable II. C – More productive use of personnel (labor productivity) by NH than by IMC confers an 8% cost advantage on NH(87-80=7, 7/87=8%) is the net result of a 33% cost advantage conferred by NH’s use of a lower personnel skill mix (IIIA, calculated using the formula in Erhun et al. (2015)) and a 25% cost disadvantage conferred by NH’s use of a larger average total amount of personnel hours per CABG (IIIB) |
Appendix B. Supplementary data
Supplementary tables
References
- 1.Richman B.D., Udayakumar K., Mitchell W. Lessons from India in organizational innovation: A tale of two heart hospitals. Health Aff. 2008;27(5):1260–1270. doi: 10.1377/hlthaff.27.5.1260. [DOI] [PubMed] [Google Scholar]
- 2.Govindarajan V., Ramamurti R. Delivering world-class health care, affordably. Harv Bus Rev. 2013;91(11):117–122. [Google Scholar]
- 3.Gupta B., Huckman R.S., Khanna T. Task shifting in surgery: Lessons from an Indian heart hospital. Healthcare. 2015;3(4):245–250. doi: 10.1016/j.hjdsi.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Richman B.D., Schulman K.A. What U.S. hospitals can still learn from India’s private heart hospitals. N Engl J Med Catal. 2017;3 https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0479?casa_token=WC-l0sYt8vkAAAAA:xj11FrN5XWj8O6cMW4osK_kmX0tQnenaRD3ikOWPlH_9uWnGoNrWfNxpzrQ3e9jfO2St0u4rwIYDwokv [Google Scholar]
- 5.Khanna T, Rangan K, Manocaran M. Narayana Hrudayalaya Heart Hospital: Cardiac care for the poor (A). Harvard Bus Case 9-505-078. 2011.
- 6.Rangan VK, Thulasiraj RD. The Aravind Eye Care System: Making sight affordable. September 2007. http://www.hbs.edu/faculty/Pages/item.aspx?num=35648. Accessed April 17, 2015.
- 7.Govindarajan V., Ramamurti R. Harvard Business Review Press; Boston, MA: 2018. Reverse Innovation in Health Care: How to Make Value-Based Delivery Work. [Google Scholar]
- 8.Baker J.J. Aspen Publishers; Gaithersburg, Maryland: 1998. Activity-Based Costing and Activity-Based Management for Health Care. [Google Scholar]
- 9.Capettini R., Chow C.W., McNamee A.H. On the need and opportunities for improving costing and cost management in healthcare organizations. Manag Financ. 1998;24(1):46–59. [Google Scholar]
- 10.Kaplan R.S., Porter M.E. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89(9):46–52. 54, 56-61. [PubMed] [Google Scholar]
- 11.Kaplan R.S., Anderson S.R. Time-driven activity-based costing. Harv Bus Rev. 2004;82:131–138. [PubMed] [Google Scholar]
- 12.Kaplan R.S., Anderson S.R. The innovation of time-driven activity-based costing. J Cost Manag. 2007;21(2):5–15. [Google Scholar]
- 13.Demeere N., Stouthuysen K., Roodhooft F. Time-driven activity-based costing in an outpatient clinic environment: Development, relevance and managerial impact. Health Policy. 2009;92(2-3):296–304. doi: 10.1016/j.healthpol.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 14.French K.E., Albright H.W., Frenzel J.C. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthcare. 2013;1(3-4):136–142. doi: 10.1016/j.hjdsi.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Öker F., Özyapıcı H. A new costing model in hospital management: Time-driven activity-based costing system. Health Care Manag (Frederick). 2013;32(1):23–36. doi: 10.1097/HCM.0b013e31827ed898. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan R.S., Witkowski M., Abbot M. Using time-driven activity-based costing to identify value improvement opportunities in healthcare. J Healthc Manag. 2014;59(6):399–413. [PubMed] [Google Scholar]
- 17.Kaplan A.L., Agarwal N., Setlur N.P. Measuring the cost of care in benign prostatic hyperplasia using time-driven activity-based costing (TDABC) Healthcare. 2015;3(1):43–48. doi: 10.1016/j.hjdsi.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Akhavan S., Ward L., Bozic K.J. Time-driven activity-based costing more accurately reflects costs in arthroplasty surgery. Clin Orthop Relat Res. February 2015 doi: 10.1007/s11999-015-4214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keel G., Savage C., Rafiq M. Time-driven activity-based costing in health care: A systematic review of the literature. Health Policy (New York). 2017;121(7):755–763. doi: 10.1016/j.healthpol.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 20.Tseng P., Kaplan R.S., Richman B.D. Administrative costs associated with physician billing and insurance-related activities at an academic health care system. JAMA. 2018;319(7):691. doi: 10.1001/jama.2017.19148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.About The Joint Commission | Joint Commission. http://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx. Accessed December 17, 2014.
- 22.Who is JCI - Who We Are | Joint Commission International. http://www.jointcommissioninternational.org/about-jci/who-is-jci/. Accessed December 17, 2014.
- 23.The Society of Thoracic Surgeons STS Public Reporting Online. https://publicreporting.sts.org/acsd
- 24.Erhun F., Mistry B., Platchek T. Time-driven activity-based costing of multivessel coronary artery bypass grafting across national boundaries to identify improvement opportunities: Study protocol. BMJ Open. 2015;5(8) doi: 10.1136/bmjopen-2015-008765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Datat S, Rajan M. Flexible Budgets, Direct-Cost Variances, and Management Control. In: Horngren’s Cost Accounting: A Managerial Emphasis. 16th ed. Pearson; 2017.
- 26.National Academy of Engineering and Institute of Medicine. Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC; 2005. 10.17226/11378.
- 27.President’s Council of Advisors on Science and Technology. Report to the President: Better Health Care and Lower Costs: Accelerating Improvement Through Systems Engineering. Washington, DC; 2014.
- 28.Dolansky M.A., Xu F., Zullo M. Post-acute care services received by older adults following a cardiac event: A population-based analysis. J Cardiovasc Nurs. 2010;25(4):342–349. doi: 10.1097/JCN.0b013e3181c9fbca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Connor G.T., Plume S.K., Olmstead E.M. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. JAMA. 1996 Mar 20;275(11):841–846. [PubMed] [Google Scholar]
- 30.Shahian D.M., Jacobs J.P., Edwards F.H. The society of thoracic surgeons national database. Heart. 2013 Oct;99(20):1494–1501. doi: 10.1136/heartjnl-2012-303456. [DOI] [PubMed] [Google Scholar]
- 31.Sood N., Ghosh A., Escarce J.J. Employer-sponsored insurance, health care cost growth, and the economic performance of U.S. industries. Health Serv Res. 2009;44(5p1):1449–1464. doi: 10.1111/j.1475-6773.2009.00985.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schulman K.A., Milstein A. The implications of “Medicare for All” for US hospitals. JAMA. 2019;321(17):1661. doi: 10.1001/jama.2019.3134. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables