Abstract
The novel coronavirus 2019 disease (COVID-19) pandemic has placed intense pressure on health care organizations around the world. Among other concerns, there has been an increasing recognition of common and deleterious cardiovascular effects of COVID-19 based on preliminary studies. Furthermore, patients with preexisting cardiac disease are likely to experience a more severe disease course with COVID-19. As case numbers continue to increase exponentially, a surge in the number of patients with new or comorbid cardiovascular disease will translate into more frequent and, in some cases, prolonged rehabilitation needs after acute hospitalization. This report describes the current status of post-discharge cardiac care in Canada and provides suggestions regarding steps that policymakers and health care organizations can take to prepare for the COVID-19 pandemic.
Résumé
La pandémie de maladie à coronavirus 2019 (COVID-19) exerce des pressions intenses sur les organismes de soins de santé de partout dans le monde. Entre autres préoccupations, des études préliminaires rapportent une augmentation de l’observation d’effets cardiovasculaires délétères courants de la COVID-19. En outre, les patients présentant une cardiopathie préexistante sont susceptibles d’être plus durement touchés par la COVID-19. Alors que le nombre de cas continue de croître de manière exponentielle, une hausse soudaine du nombre de patients atteints d’une maladie cardiovasculaire de novo ou concomitante entraînera une augmentation des besoins en matière de services de réadaptation, et, dans certains cas, de services de réadaptation prolongés, après une hospitalisation de courte durée. Le présent rapport décrit la situation actuelle des soins en cardiologie après la sortie de l’hôpital au Canada et propose des mesures que les décideurs et les organismes de soins de santé pourraient prendre pour se préparer dans le contexte de la pandémie de COVID-19.
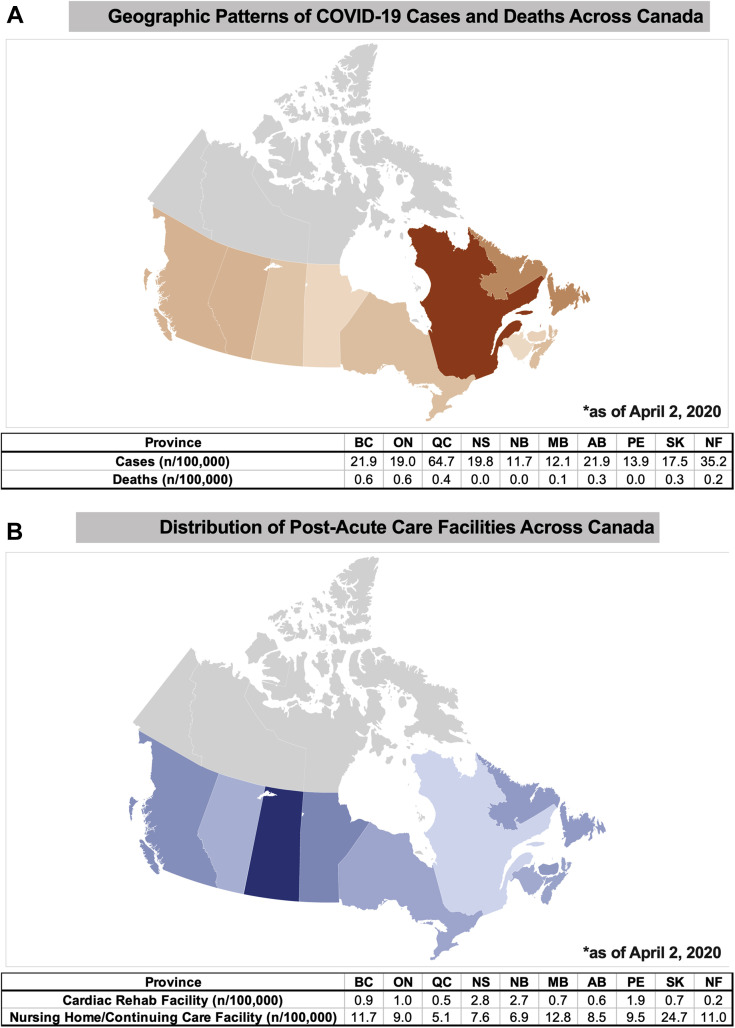
The coronavirus 2019 disease (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, has placed tremendous pressures on health care organizations around the world. As of April 5, 2020, there were 14,018 confirmed cases in Canada spread across the country (Fig. 1 A), with estimates suggesting that 35% to 70% of the Canadian population could eventually become infected.1
Figure 1.
(A) Geographic distribution of COVID-19 cases and deaths per 100,000 population and (B) geographic distribution of post-acute care facilities across Canada per 100,000 population.
Appropriately, much attention to date has focused on addressing the surge of critically ill patients in acute care settings. Less emphasis has been paid to the post-acute health care system capacity to manage numerous cardiac patients after COVID-19, ie, as patients move from hospital to long-term care facilities or home. In Canada, post-acute cardiac care includes outpatient and inpatient cardiac rehabilitation facilities, long-term care hospitals, and nursing homes.
Along with a growing body of knowledge underlying COVID-19, there has been an increased recognition of common and deleterious cardiovascular effects of the novel coronavirus.2 Furthermore, patients with preexisting cardiovascular disease (CVD) are likely to experience a more severe course.2 As case numbers continue to increase exponentially, it is plausible that there will be a massive surge in the number of patients with new or comorbid CVD who will require cardiac rehabilitation after acute care hospitalization.
The objectives of this report are to describe the current status of post-acute cardiac care in Canada and to provide suggestions regarding the steps that policymakers and health care organizations can take to achieve preparedness in this area to reduce care fragmentation in the post-COVID-19 era.
COVID-19 and Cardiovascular Disease
Several reports have noted the incidence and types of adverse cardiovascular events associated with COVID-19. In one early experience from Wuhan, China, arrhythmias were present in 16.7% of hospitalized patients, with 7.2% experiencing acute cardiac injury.3 In a subsequent report, cardiac injury, defined as high-sensitivity troponin I levels above the 99th-percentile upper reference limit, occurred in 19.7% of patients, occurring most frequently among older patients and those with comorbidities.2 The presence of cardiac injury was associated with a more severe disease course and with a higher proportion of patients with acute respiratory distress syndrome, acute kidney injury, and coagulation disorders, compared with patients without cardiac injury.2 Furthermore, cardiac injury was an independent predictor for mortality, with a hazard ratio of 3.41.2 Although this injury does not necessarily indicate myocardial infarction, and its long-term significance remains unknown, the high prevalence and associated mortality has raised significant concern within the cardiovascular community.
In addition to the development of COVID-19–related cardiovascular complications, there are implications of COVID-19 infection on patients with preexisting CVD. In patients with COVID-19, CVD is associated with a higher death rate (13.2%) compared with other comorbidities, including diabetes (9.2%), chronic respiratory disease (8.0%), and cancer (7.6%).4 In general, the development of new cardiac injury or the presence of prior CVD are associated with a more severe disease course.
The pathophysiology of this interaction remains poorly characterized. However, preliminary data suggest that acute inflammation superimposed on preexisting CVD can precipitate cardiac injury, acute coronary syndrome, and myocardial dysfunction and trigger arrhythmias in patients with COVID-19.2 , 3 Given the frequency of cardiac manifestations and injuries, the cardiac rehabilitation system will likely be overwhelmed by an unprecedented number of discharged patients with new or exacerbated CVD.
Post-Acute Cardiac Care in Canada
Canada has a long history of outstanding post-acute cardiac care. Currently, there are ∼ 220 cardiac rehabilitation programs, serving more than 50,000 new patients annually (Fig. 1B). Funding for cardiac rehabilitation varies by provincial and local resources according to their unique population densities and funding structures. Given these differences, along with the geographic diversity of the country, access to cardiac rehabilitation remains variable. Newfoundland has the least access, with 0.2 facilities per 100,000 individuals, while Nova Scotia has the most, with 2.8 per 100,000.
In addition to outpatient cardiac rehabilitation programs, inpatient rehabilitation facilities play a crucial role in supporting the convalescence of patients who no longer require acute care hospitalization. There are 3409 nursing home or continuing care facilities in Canada, with a geographic distribution similar to that of cardiac rehabilitation centers (Fig. 1B).
Although data is limited regarding the proportion of patients with COVID-19 who require post-acute care, historical data from the Canadian Institutes of Health Information Cardiac Care Quality Indicators and Rehabilitation Reports demonstrate that there were 39,438 admissions to inpatient rehabilitation facilities in Canada in the 2018/2019 fiscal year, of which 1331 (3.4%) were cardiac related. Given the associations described between COVID-19 and CVD, we expect that this proportion will increase as patients are discharged from acute care with new or exacerbated cardiac issues.
Potential Burden of COVID-19
As of March 29, 2020, 75.1% of Ontario’s critical care beds were occupied, of which 29.6% were related to confirmed or suspected cases of COVID-19. Several models have been developed to study the potential trajectories of resource use during this pandemic. Although these models focus on acute care resources, they provide a reliable resource to help predict the range of potential impacts on the post-acute care sector as well. Using the total number of inpatient beds, ICU beds, and ventilators in Ontario, the COVID-19 ModCollab5 have examined 3 potential scenarios (Fig. 2 ). In the worst-case scenario, which assumes a growth rate of 33.0% in daily cases (similar to that in Italy), the number of available hospital beds in Ontario could fall to 0 by early to mid-April 2020, without recovery through mid-May. In another scenario, assuming an initial growth rate of 25.0% in daily cases (similar to that initially seen in Ontario) until the of end of March, followed by a 10.7% decrease to account for successful public health measures (school closure, social distancing, testing, and isolation), the maximum impact on inpatient acute hospital care would occur in early April, followed by a sustained recovery. Finally, in a third scenario which assumes an initial 15.0% daily increase, with a similar subsequent 10.7% decrease, the overall impact would be reduced; however, the timing of patient influx to post-acute care would likely be unchanged. The post-acute care sector will play a key role in alleviating pressures on hospitals; however, these facilities and programs themselves will face challenges as they attempt to reduce care fragmentation.
Figure 2.
Model for days until hospital resource depletion due to COVID-19. Adapted from Dr Beate Sander on behalf of the COVID-19 ModCollab5 with permission.
Recommendations for the Current Crisis
In the midst of this global crisis, health care facilities are adapting to deliver care in safer and more efficient ways. Post-acute care facilities will be increasingly challenged by a rising influx of patients with serious and incompletely resolved cardiac problems. Fortunately, as a large country with a significant rural population, Canada has experience with various alternate models for post-acute cardiac care. The maximization of these services to treat patients at home will be an extremely important component of managing resources during the COVID-19 pandemic. To accomplish this, open communication between cardiac rehabilitation centres will be needed for knowledge exchange, allowing centres not currently offering home-based programs to quickly learn from other centres where this practice has been successfully implemented.
In addition, there is a need to maximise mobile health technology to minimise patient and health care personnel exposure to COVID-19. In the context of this pandemic, telehealth technology can be leveraged to reduce the need for in-person care for appropriate patients. Specifically, this technology can be applied to patient follow-up after discharge, to perform remote cardiac monitoring, and to administer cardic rehabilitation curriculums remotely. Digital health interventions, such as the Virtual Care Program from the University of Ottawa Heart Institute (https://pwc.ottawaheart.ca/programs-services/virtual-care), provide services such as self-monitoring tools, reminders, and notifications, as well as peer support groups for those undergoing remote curriculums. Health care systems that will leverage these technologies to manage the upcoming influx of patients could see a reduction in in-person care needs and be in a better position to serve their patients. These technologies will play a particularly important role in filling gaps present in areas with limited access to current cardiac rehabilitation care.
Patient-level factors should also be taken into consideration for the prioritisation of inpatient space. In particular, cognitive impairment, paralysis, and those requiring a ventilator or dialysis are among the factors associated with a greater risk of prolonged inpatient rehabilitation stay. The repurposing of unused buildings, such as hotels, convention halls, clinics, and other spaces, to establish temporary post-acute care settings, where appropriate, could rapidly expand the supply of space, particularly in areas that are currently underserved by post-acute care facilities.
Conclusion
COVID-19 places an unprecedented strain on health care resources in Canada. Given the association of this infection with comorbid cardiac disease and the high rate of new cardiac conditions among infected patients, the post-discharge cardiac rehabilitation sector will be particularly affected. There is a pressing need to address the impact of COVID-19 on post-acute cardiac care. Early preparation and thoughtful planning may help to limit that impact.
An expanded version of this report with additional references is available as Supplementary Material.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 959 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at https://doi.org/10.1016/j.cjca.2020.04.006.
Supplementary Material
References
- 1.Kirkey S. Coronavirus could infect 35 to 70 per cent of Canadians, experts say. National Post, March 10, 2020. https://nationalpost.com/news/canada/coronavirus-could-infect-35-to-70-per-cent-of-canadian-population-experts-say Available at:
- 2.Shi S., Qin M., Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China [e-pub ahead of print]. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.0950 [DOI] [PMC free article] [PubMed]
- 3.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Worldometer Age, sex, existing conditions of COVID-19 cases and deaths: pre-existing medical conditions (comorbidities) https://www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/ Available at:
- 5.COVID-19 ModCollab. Kali Barrett K., Khan Y.A., Mac S. Modeling COVID-19 Healthcare Resource Utilization and Capacity Constraints. COVID-19 ModCollab. https://www.covid-19-mc.ca Available at: Accessed March 31, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.