Abstract
The emergence of the COVID-19 pandemic has severely affected medical treatment protocols throughout the world. While the pandemic does not affect hand surgeons at first glance, they have a role to play. The purpose of this study was to describe the different measures that have been put in place in response to the COVID-19 pandemic by hand surgeons throughout the world. The survey comprised 47 surgeons working in 34 countries who responded to an online questionnaire. We found that the protocols varied in terms of visitors, health professionals in the operating room, patient waiting areas, wards and emergency rooms. Based on these preliminary findings, an international consensus on hand surgery practices for the current viral pandemic, and future ones, needs to be built rapidly.
Keywords: COVID-19, Hand Surgery, Pandemic, Epidemic, Coronavirus
Résumé
L’émergence de la pandémie à Covid-19 a bouleversé les pratiques médicales dans le monde. À première vue, cette pandémie ne concerne pas les chirurgiens de la main. Pourtant, ils ont un rôle à jouer. Le but de cette étude était de décrire les différentes pratiques mises en œuvre contre la pandémie à Covid-19 à partir du retour d’expérience de 47 chirurgiens de la main exerçant sur tous les continents. Le matériel comprenait 47 chirurgiens de la main exerçant dans 34 pays qui ont répondu à un questionnaire en ligne portant sur les protocoles Covid-19 mis en place. Les résultats ont montré que les pratiques étaient hétérogènes, tant pour les patients, les visiteurs et le personnel soignant au bloc opératoire, en salle de réunion, aux services d’hébergement des patients, au service d’accueil des urgences et en consultations externes. Il nous semble essentiel de définir un consensus international en chirurgie de la main pour lutter contre les pandémies virales actuelles et futures.
Mots clés: Covid_19, Chirurgie de la main, Pandémie, Épidémie, Coronavirus
1. Introduction
The emergence of the COVID-19 pandemic has severely impacted medical practices throughout the world especially those of infectious disease specialists, emergency room personnel, anesthetists, intensivists, virologists, epidemiologists and hygienists. At first glance, the current pandemic does not affect hand surgeons; however, there is evidence that surgeons play a role in the continuation of emergency surgical care, the protection of medical staff and the management of resources [1].
A hand surgeon and an assistant from the Wuhan region were infected on 22nd January 2020 whilst operating on a COVID-19 patient. They self-isolated for 14 days. On the 3rd day, the surgeon showed signs of mild respiratory symptoms that got worse by the 9th day. The COVID-19 diagnosis was confirmed by CT scan and PCR (polymerase chain reaction) testing. Subsequently, the surgeon was admitted to a hospital where he eventually recovered. Review of this case showed that the protective measures in place against COVID-19 had not been followed correctly [2].
The purpose of this study was to describe the different measures that have been put in place in response to the COVID-19 pandemic by hand surgeons throughout the world.
2. Material and methods
The study comprised 47 hand surgeons (level 5 [3]) practicing in 34 different countries (Fig. 1 ). The survey consisted of an online questionnaire filled out between March 23 and 27, 2020. The questionnaire focused on the existing protocols in five key areas: operating theatres, surgeons’ meeting rooms, wards, emergency rooms and external consultations. The results were summarized by describing the key features of the most common protocols used.
Fig. 1.
Geographical distribution of the hand surgeons participating in the study.
3. Results
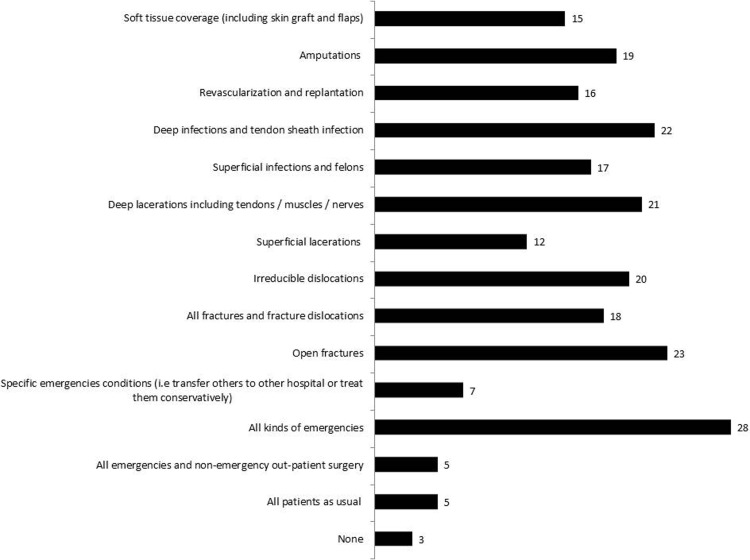
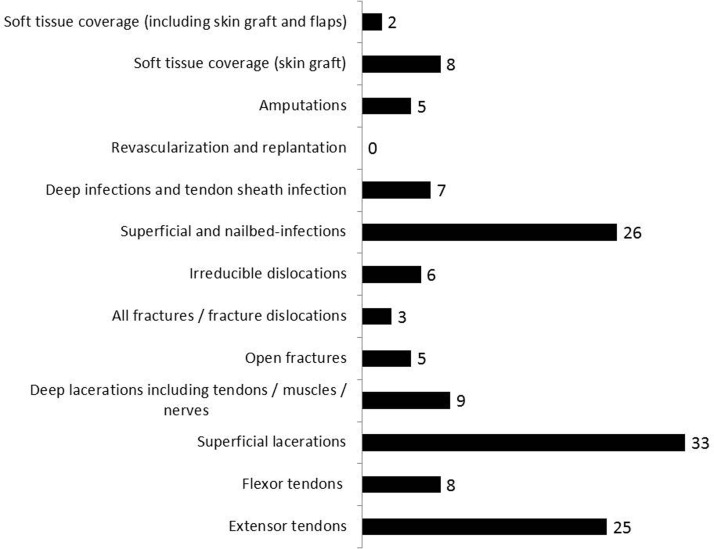
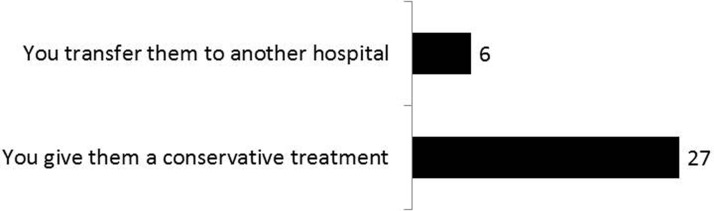
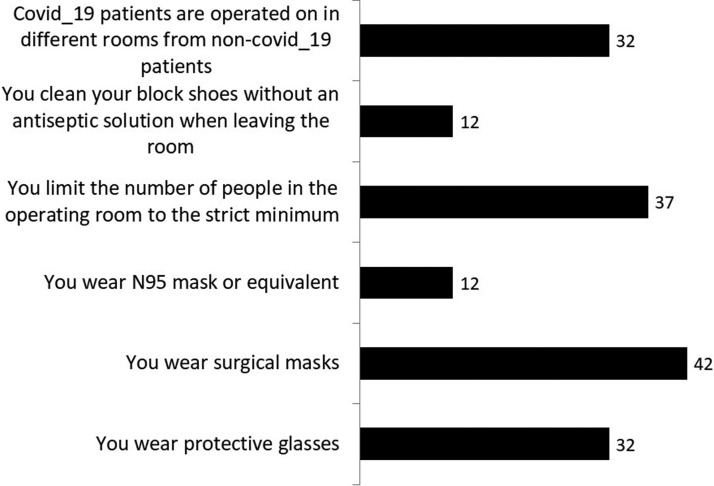
In the operating theatre, 5/47 did not modify the indications for surgery, 3/47 totally stopped performing surgery, and 39/47 modified their practice. Within this last group, 28 operated on emergencies only, whereas 5 continued scheduled surgical activities (Fig. 2 ). Within the group that continued to operate on emergency cases, 38 performed surgery in a small operating theatre on the patients they would normally have operated on in the main theatre (Fig. 3 ). Twenty-seven altered their indications for surgery and proposed conservative treatment (Fig. 4 ). And while 32 surgeons operated on COVID-19 positive patients, these operating theatres were specifically dedicated to COVID-19 patients. The majority wore specific personal protection equipment (PPE); however, the nature of this PPE varied (Fig. 5 ).
Fig. 2.
Question 1: Which patients do you operate on during this COVID-19 pandemic period?
Fig. 3.
Question 2: If you only operate certain emergencies among those that you would have operated in normal times, which ones do you operate outside the operating room in a small emergency room/day surgery center under local anesthesia?
Fig. 4.
Question 3: If you only operate certain emergencies, what do you do with those that you would have operated under normal circumstances and that you do not operate at all?
Fig. 5.
Question 4: In the operating room.
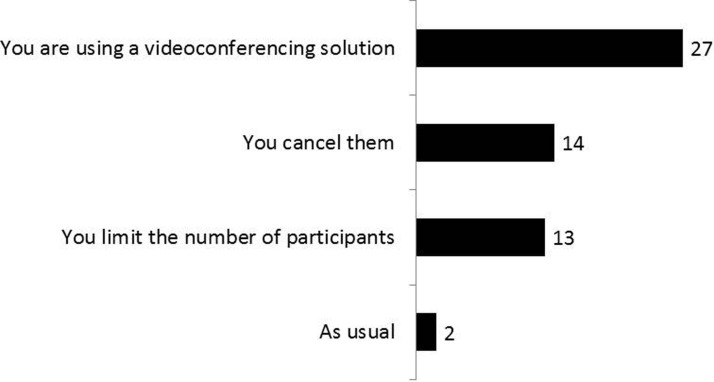
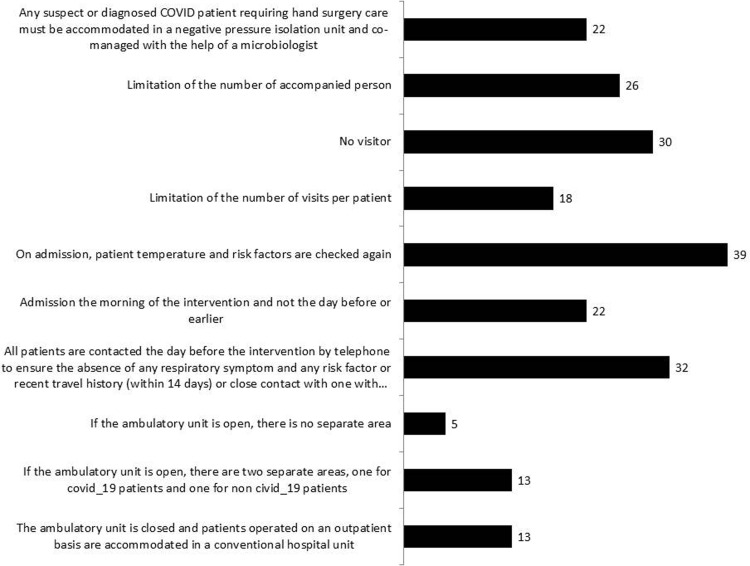
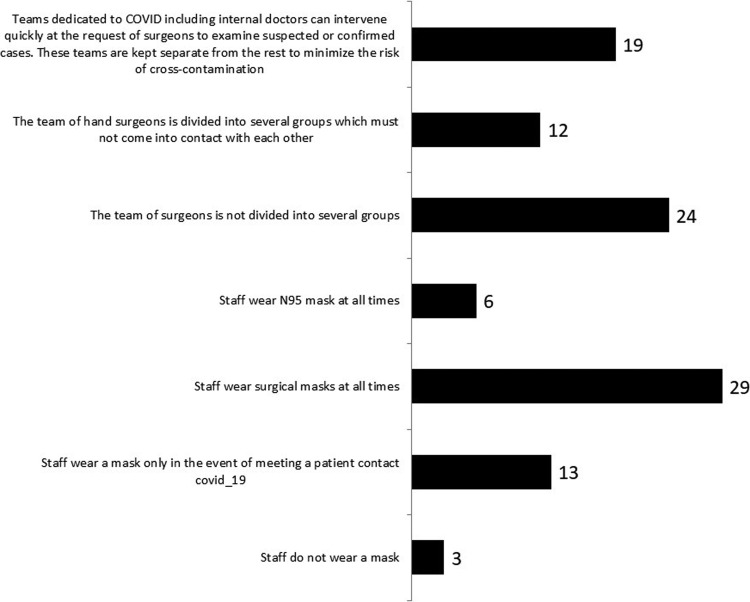
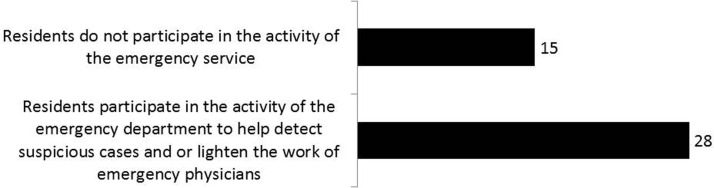
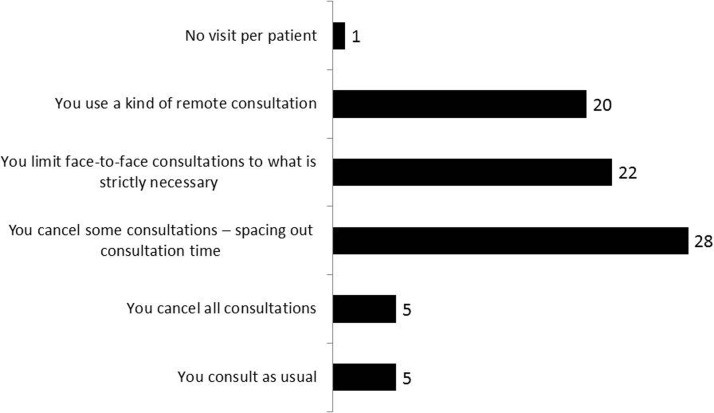
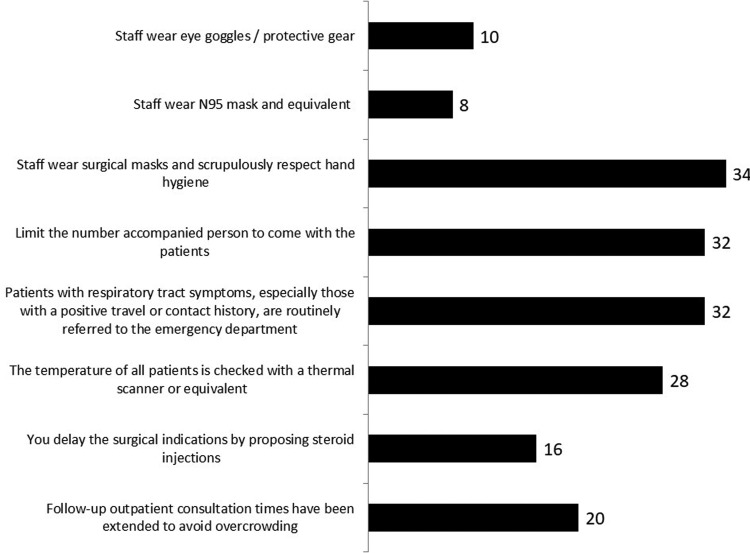
Most surgeons took measures to limit contact in meeting rooms (Fig. 6 ). On the wards, numerous measures were in place to limit transmission of the virus; these applied to patients, visitors and healthcare workers (Fig. 7, Fig. 8 ). In the emergency rooms surveyed, most surgical residents assisted the emergency room staff in screening COVID-19 patients (Fig. 9 ). Consultation practices varied: 5 saw patients as before while 42 modified their practice (Fig. 10 ). Amongst those who continued consultations, the majority took measures to screen patients and used personal protection measures against COVID-19 (Fig. 11 ).
Fig. 6.
Question 5: Staff meetings.
Fig. 7.
Question 6: Organization of hospitalization for patients.
Fig. 8.
Question 7: Organization of hospitalization for staff.
Fig. 9.
Question 8: In the emergency department.
Fig. 10.
Question 9: Organization of outpatient consultations.
Fig. 11.
Question 10: If you continue to consult.
4. Discussion
The management of a viral pandemic necessitates preventative measures to reduce intra-hospital transmission [4]. During surgery, drastic measures were put in place to facilitate the care of patients who are confirmed or suspected of being infected with COVID-19 and reduce the risk of intraoperative transmission to healthcare professionals and other patients. Some hospitals have set protocols related to negative pressure ventilation [5] and more frequent air exchanges as well as limiting the numbers of circulating personnel in the operating theatre [6].
Our study has limitations. The first is that the severity and spread of COVID-19 were not recognized initially. The epidemic in China started in late December 2019 [7] and a pandemic was declared worldwide on 12 March 2020 [8]. Countries that were geographically distant from China lagged in putting into place any counter measures. The second limitation of the study lies in the fact that the severity of the outbreak was not the same in all countries [9]. The third limitation is that different countries took different counter measures, thus explaining the disparity of our survey results.
Our results show that the measures put in place by 47 hand surgeons were not homogeneous. As far as we know, the WHO has not issued any recommendations for the operating theatre related to the COVID-19 pandemic. We feel that the following measures should be implemented strictly:
-
•
all non-urgent surgeries should be deferred to a later date;
-
•
in the operating theatre, all members of the surgical team should comply with exactly the same measures put in place by the infectious diseases department of their respective hospitals;
-
•
all in-person meetings should be cancelled and be replaced by video conferencing;
-
•
the wards should follow the same strict measures;
-
•
office consultations should be deferred or cancelled [10].
If this proves impossible, then the same strict preventative measures should be followed [11].
Given the infection of a hand surgeon in Wuhan [2] and our study's findings, an international consensus is needed on the measures to be taken by hand surgeons during a viral pandemic.
Human and animal rights
The authors declare that the work described has not involved experimentation on humans or animals.
Informed consent and patient details
The authors declare that the work described does not involve patients or volunteers.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
References
- 1.Liang Z.C., Wang W., Murphy D., Hui J.H.P. Novel Coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. 2020;00 doi: 10.2106/JBJS.20.00236. [e1(1-5)d], (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang K., Wang Q., Chen Z. A case of hand surgeon infection of COVID-19 due to exposure to treating a suspect patient. Chinese J Hand Surg. 2020;36 doi: 10.3760/cma.j.cn311653-20200304-00096. (2020-03-08), Available from URL: http://rs.yiigle.com/yufabiao/1184341.htm. [DOI] [Google Scholar]
- 3.Tang J.B., Giddins G. Why and how to report surgeons’ levels of expertise. J Hand Surg Eur. 2016;41:365–366. doi: 10.1177/1753193416641590. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19) Situation Summary. Available from URL: https://www.cdc.gov/coronavirus/2019-ncov/summary.html. (accessed March 2020).
- 5.Ti L.K., Ang L.S., Foong T.W., Ng B.S.W. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020 doi: 10.1007/s12630-020-01617-4. [Epub ahead of print] PubMed PMID: 32144591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y., et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020 doi: 10.1007/s12630-020-01620-9. [Epub ahead of print] Review. PubMed PMID: 32162212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organisation. Announces COVID-19 outbreak a pandemic. Available from URL: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic.
- 8.World Health Organisation 2020c. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel Coronavirus (2019-nCoV). Available from URL: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed 30 January 2020.
- 9.World Health Organization. Coronavirus disease 2019 (COVID 19) Situation Report- 24 March 2020. Available from URL: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200324-sitrep-64-covid-19.pdf?sfvrsn=703b2c40_2. (accessed March 2020).
- 10.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2003539. [Epub ahead of print] PubMed PMID: 32160451. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation. Infection prevention and control during health care when COVID-19 is suspected. Interim Guidance – 19 March 2020. Available from URL: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125.